Abstract
Purpose
Exoskeleton use by people with complete spinal cord injury (SCI) in daily life is challenging. To optimize daily exoskeleton use, a better understanding of the purpose of use and the accompanying improvements are needed. The perspective of experienced exoskeleton users could guide design improvements.
Methods
Face-to-face semi-structured interviews were held with 13 people with SCI with exoskeleton experience. Interviews were audio-taped, transcribed, and analysed thematically.
Results
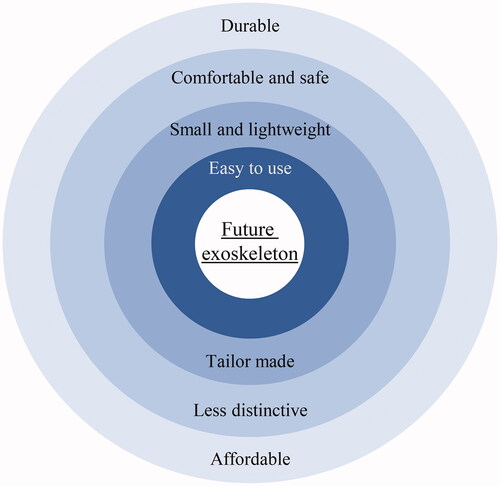
Participants expressed three future purposes of exoskeleton use: for daily activities (e.g., stair climbing), exercise (e.g., staying healthy), and social interaction (e.g., standing at parties). Exoskeleton use during daily activities was the ultimate goal. Therefore, the future exoskeleton should be: easy to use, small and lightweight, tailor made, safe, comfortable, less distinctive, durable, and affordable. Improving the ease of use was relevant for all purposes, for all participants. The other suggestions for improvement varied depending on the purpose of use and the participant.
Conclusion
Increasingly more advanced improvements are needed to transition from an exercise purpose to social interaction, and ultimately use during daily activities. In the current study, detailed suggestions for improvements have been made. Only when multiple of these suggestions are adjusted, can the exoskeleton be used to its full potential.
The use of an exoskeleton by people with a complete spinal cord injury in daily life is still in its infancy.
To optimize daily exoskeleton use, a better understanding of the purpose of use and exoskeleton improvements is needed.
More advanced improvements to future exoskeletons are needed to make a transition from use as an exercise device to use during social interaction and daily activities.
Improving the ease of use of future exoskeletons is considered a priority by experienced users, followed by making the exoskeleton small, lightweight, and tailor made.
IMPLICATIONS FOR REHABILITATION
Introduction
Spinal cord injury (SCI) is characterized by damage of the spinal cord that leads to (partial) loss of sensory, motor, and autonomic functions below the lesion [Citation1]. A motor complete SCI is characterized by paralysis of the muscles below the lesion level and, thus, recovery of walking capacity is unlikely, resulting in a lifetime reliance on a wheelchair [Citation2,Citation3]. Further, people with SCI are also at risk for the occurrence of secondary health complications, such as bladder and bowel disorders, pressure ulcers, spasticity, and pain [Citation4,Citation5], which are associated with a lower quality of life [Citation5]. Recently, wearable exoskeletons (such as the ReWalk™, Ekso™, and Indego® exoskeleton) have appeared on the consumer market [Citation6,Citation7]. In the clinical setting, wearable exoskeletons are mainly used for training purposes and to enhance health benefits in people with complete SCI. The health benefits include less spasticity [Citation8,Citation9], improved bowel function [Citation10], and improved overall quality of life [Citation8]. However, to preserve these health benefits, regular exoskeleton use is necessary. One approach to facilitate regular exoskeleton use is to ensure that wearable exoskeleton can be used at home and in the community.
Little is known about the use and experienced benefits of exoskeleton use in the community. To our knowledge, two studies investigated community exoskeleton use, namely in a community-based gym [Citation11] or in and around the home [Citation12]. In both studies, the exoskeleton was mainly used for exercise purposes [Citation11,Citation12]. Participants also emphasized the usefulness of an exoskeleton for social interaction, for instance, because it enables them to stand upright and look people in the eyes instead of the waist [Citation11,Citation12]. The exoskeleton was rarely used to facilitate functional mobility during daily activities [Citation12]. Study participants reported physical and psychosocial benefits after using the exoskeleton for ∼10 weeks [Citation12] or one year [Citation11]. They experienced less spasticity, less pain, better wound healing, improved bowel function, and improved mental well-being and increased energy to (socially) interact at eye level [Citation11,Citation12]. Although there seem to be physical and psychosocial benefits for exoskeleton users, it is unclear which barriers exoskeleton users experience in the home and community setting.
A few studies examined possible barriers and/or improvements of an exoskeleton to optimize its use. Reported areas of improvement were safety [Citation13–17], ease of use (including the need of a buddy [Citation13–15,Citation18], need of upper extremity support [Citation14,Citation18,Citation19], walking speed [Citation13,Citation15–18], donning [Citation13–18], transportability [Citation14,Citation17,Citation19], and energy demand [Citation15]), costs [Citation15–17], comfort [Citation16–18], reactions of others [Citation17], and appearance [Citation17]. However, these suggested improvements are from researchers and individuals with no exoskeleton use experience [Citation13–16,Citation18,Citation19]. More importantly, it was concluded that there is an important gap between the expectations of non-exoskeleton users with SCI and what can be done with existing exoskeletons in the community [Citation17]. The needs and wishes for the future exoskeleton from the perspective of people with complete SCI with community-based exoskeleton experience are still unclear. In addition, the various barriers people with complete SCI may experience when using the exoskeleton may vary depending on the purpose of its use (e.g., the need for a buddy might be a barrier for functional daily use, but not for social interaction at an eye-level).
To optimize the use of exoskeletons in daily life by people with complete SCI, a better understanding of the purpose of use and accompanying improvements from the perspective of exoskeleton users are needed. The perspective of experienced users with complete SCI provides an important contribution to the improvement of future exoskeletons. These insights can inform future exoskeletons designs, and ultimately, can help to optimize community-based exoskeleton use. Therefore, the main research questions of this qualitative study were (1) for which purpose(s) would (potential) exoskeleton users like to use the exoskeleton in the future and (2) which improvements are needed to the current exoskeleton to facilitate these desired purpose(s) of use?
Methods
A qualitative study design involving in-depth semi-structured interviews with thematic analysis was chosen to address the research questions. Ethical research codes, such as the confidentiality of participants' identity, taking permission for the audio recording of the interview, and the right to withdraw from the study, were followed. All participants received information about the purpose, methods, and ethical rights, and all of them gave written informed consent in accordance with the Declaration of Helsinki before the start of the interview. The medical ethics committee of Arnhem-Nijmegen determined that this study met the requirements for exemption from the Medical Ethics Committee review under the Dutch Medical Research Involving Human Subjects (2019-5637). The study was approved by the internal review board of the Sint Maartenskliniek.
Population and recruitment
Adult people in the chronic phase (>6 months) after a motor complete SCI (American Spinal Injury Association Impairment Scale (AIS) (A or B) who used a wearable exoskeleton both in the clinical setting and community-setting and had proficiency in the Dutch language were eligible. Participants were selected via purposive sampling [Citation20]. In the Netherlands, exoskeletons are not reimbursed or delivered as assistive technologies for community use. Hence, Dutch people who have community-based exoskeleton experience are either people who purchased their own exoskeleton (through crowdfunding) or who participated in a research project. Eligible people who participated in our previous exoskeleton study (2016-2418 [Citation12]) and who gave consent to be contacted for a follow-up study were approached. These people have experienced exoskeleton users who had completed a clinical training period of ∼8 weeks (±24 training sessions) [Citation12] and had used the ReWalk™ exoskeleton in the home and community setting. The amount of community use by these people ranged from 3 to 15 days [Citation12]. In addition to those who had exoskeleton experience in a community setting through participation in our previous study [Citation12], people in the Netherlands who purchased their own exoskeleton were contacted to participate. In total, three people (including one participant from our previous study [Citation12]) had purchased their own ReWalk™ exoskeleton through crowdfunding and, thus, had ample community exoskeleton experience. To our knowledge, this was the entire population of Dutch people with complete SCI who used an exoskeleton in the home and in the community setting. Potential participants were first approached by an e-mail containing the information letter. If they had no objections, they were contacted by telephone after one week of reflection and, if they wanted to participate, to schedule an interview appointment.
Data collection
Single face-to-face interviews were held at the participant’s home or at the rehabilitation clinic, according to the preference of the participant. The interview guide consisted of six semi-structured open-end questions. Two sensitizing questions related to the participant’s past exoskeleton experience, followed by four main theme questions [Citation21] specific to the research questions. (1) Could you describe the first day you used the exoskeleton at home or outside the clinic? (2) Could you describe the last time you used the exoskeleton at home or outside the clinic? (3) Suppose you would use the exoskeleton every day, for example, like putting in your contact lenses every morning or wearing your glasses, what should the exoskeleton look like to you? (4) For which activities would you like to use the exoskeleton? What would the purpose of exoskeleton use be? (5) Which changes to the current exoskeleton are needed for that purpose? (6) Looking back at the exoskeleton you used, what do you think are the most important changes that are needed? In addition, probing questions [Citation21] were asked to gain more details. All questions were open-ended, as such questions tend to yield richer data than closed questions [Citation21,Citation22].
Interviews were conducted by the first author (Ph.D. candidate, trained interviewer), with whom all participants were familiar from the previous study where she was the main researcher and contact point for the participants [Citation12]. No other participants or researchers were present during the interview. As a sensitizer, each interview started with a short videoclip (±1 min) in which the participant saw him/herself walk in the exoskeleton. For participants who participated in our previous study [Citation12], this videoclip consisted of the participant’s final clinical training session with the exoskeleton before 2 weeks of community use (video recorded as part of the previous study and written informed consent was given for use) [Citation12,Citation23]. For the other participants, the sensitizer consisted of video material they uploaded to YouTube themselves. Each interview was audio-recorded and transcribed verbatim for data analysis. During and after each interview, field notes were made. The duration of the interviews varied between 30 and 90 min (median of 68 min). To ensure complete and transparent reporting, the Consolidated Criteria for Reporting Qualitative Research (COREQ) checklist was used [Citation24]. An overview of the interview instructions and interview guide can be found in the Supplementary Material.
Data analysis
Data collection and data analysis were alternated and repetitively reflected upon by two researchers (RvD and JV). Analysis of the data was done in an iterative process using thematic analysis [Citation25,Citation26]. In line with thematic analysis, the transcripts were first to read several times for familiarization with the data [Citation25,Citation26]. Subsequently, the coding of the transcripts was done in three steps: open, axial, and selective coding [Citation25,Citation26]. Initial open coding was performed by the first author, with labelling segments of the transcript close to the phrasing of the participant. Thereafter, codes were refined throughout the analysis and categorized into themes (axial coding). The first and second authors constantly compared [Citation26], repetitively reflected on [Citation25,Citation27], and adjusted the axial codes. From the axial codes, the core themes and relations between themes were identified (selective coding). The core themes were shaped through theoretical sensitisation [Citation12,Citation14,Citation16,Citation28]. The number and phrasing of the core themes were carefully determined through ongoing reflexive dialogue [Citation25] between the researchers. Memos were written and used during the analysis to help the researchers keep track of and reflect upon decisions made [Citation26]. To help interpret the findings, the field notes [Citation26] (from during and after the interview) were used. Data saturation was assumed if no new axial codes emerged from the analysis of the last two interviews. To make sure the core themes were grounded in the data [Citation25,Citation29] and to ensure confirmability [Citation27], the final results were discussed with the first, second, and last author and adjusted if necessary, until consensus was reached. The software program ATLAS.ti was used to code the data and write the memos. To ensure confidentiality, codes (P1gender_high/lowSCI, P2gender_high/lowSCI, etc.) were used instead of the participants’ names when indicating from whom a quote originated. In these codes, high SCI refers to an injury level between thoracic 1 and 6 (Th1-6) and low SCI between Th7 and Lumbar 1.
Results
Participants
Thirteen out of the 16 contacted people participated in the study. Reasons for not participating were self-reported lack of sufficient community-based exoskeleton experience (n = 1), and limited time to participate (n = 2). A summary of the characteristics of the thirteen participants is given in . In addition to community-based ReWalk™ experience, six participants also had experience with another exoskeleton: the Indego® exoskeleton in a clinical setting (n = 4, ±3 years ago) and/or a research exoskeleton (i.e., March or Symbitron) in a lab setting (n = 4, ±1.5 years ago). The time between the last community-based exoskeleton use and the interview ranged between 1 day and 4 years (median of 2 years).
Table 1. Characteristics of people with community-based exoskeleton experience who participated in the study.
Purpose of exoskeleton use
Three future purposes of exoskeleton use were mentioned in the interviews, namely for daily activities, exercise, and social interaction. provides an overview of the purposes of use with exemplary citations. The use during daily activities and for exercise was addressed in the interviews of all participants. Most participants wanted to use the future exoskeleton during daily life activities in which they now used the wheelchair, such as grocery shopping or driving a car. Some people even expressed a desire to ultimately use the exoskeleton in a way that they could forget about their complete SCI but did not consider this a realistic option of future use. Participants also mentioned that they were interested in using the exoskeleton as an exercise device to stay fit and to stimulate health benefits. Furthermore, the use of the exoskeleton for social interaction (e.g., go to the pub, join in a group chat at a party with bar tables, or play with their children) was mentioned in almost all interviews. Some participants emphasized that for exercise and social interaction you do not need to purchase your own exoskeleton, but could share an exoskeleton with others as well.
Table 2. Purpose of exoskeleton use with exemplary citations.
Motives for exoskeleton use
In addition to the purposes of future exoskeleton use, three motives for exoskeleton use were clearly described in the interviews, namely societal importance, preserving autonomy, and fun. A few participants mentioned that for them, a motivation for exoskeleton use was the societal importance for further development.
P12male_lowSCI: “[Using the exoskeleton] may prevent a burn-out or depression, something like that. […] People will do more things which will… will make it easier for some people to work. I think people can then contribute more to society at large, some he, it does depend on your lesion.”
P5female_lowSCI: “I think it’s something that’s still in its infancy, that needs to be developed further. […]. I think we should all do our bit to make that happen […] it may actually be something that will be covered by health insurance in the future. Mainly for people who’ve recently suffered a spinal cord injury, I should think.”
The use of the exoskeleton was frequently compared to wheelchair use, which is something this population uses daily. For example, some participants stressed that they are completely autonomous with their wheelchair and that this level of independence is something they also wanted to pursue with the future exoskeleton, especially during daily activities.
P2female_lowSCI: “Independence. I think that's the biggest one. I’m now too dependent on someone else or on devices, for safety, weight [heaviness of the exoskeleton], all the things I can’t do myself, over which I’ve no control now. Yes, independence. Not needing help with anything. That’s it basically.”
P10female_highSCI: “That buddy is also a deal with the Rewalk […] I find it annoying that I have to wait until someone has time to walk with me. But when it comes to the exercise purpose, I find that less, a lesser obstacle than when it comes to doing the shopping or just doing your household [daily activities purpose]. Then indeed the first must is having that buddy gone.”
Contrary to wheelchair use, the motive for exoskeleton use was sometimes referred to as “for fun,” in which fun was an end in itself.
P7female_highSCI: “Well. it has to be fun. That it becomes less therapeutic. Sure, it will never be exactly the walking you were used to [before the injury], but I do think that it’s very close, that you can just go for a nice stroll around the block.”
Improvements of exoskeleton
To optimize the future exoskeleton, different improvements were suggested. Experienced exoskeleton users mentioned that their future exoskeleton should be easy to use, small and lightweight, tailor made, safe, comfortable, less distinctive, durable, and affordable (). The innermost circle (i.e., easy to use) of represents the desired improvement that was relevant for all purposes of use, for all participants. The circles further to the edge, represent improvements that are more person-dependent or dependent on the purpose of use. More detailed information regarding how the order of the circles of improvement was established can be found in the Supplementary Material. In the next sections, the different suggestions for improvement will be discussed.
Figure 1. Inductive themes for exoskeleton improvements that could optimize the future exoskeleton according to people with a complete spinal cord injury with community-based exoskeleton experience. The inner circles of improvement are less purpose- and person-dependent than the outer circles. This means that the innermost circle was relevant for many purposes of use and supported by many participants (i.e., mentioned by all participants in a similar fashion). The circles closer to the edge represent improvements that are more dependent on the purpose of use (i.e., relevant for less purposes) and/or more person-dependent (i.e., mentioned by only a few participants with more diverse opinions).
First circle: easy to use
Regardless of the purpose of the future exoskeleton, all participants mentioned that the future exoskeleton should be easier to use. Therefore, participants were advised to improve the remote-control watch, balance, step and speed adjustments, and donning and doffing of the exoskeleton. Improvements to the remote-control watch were mentioned most frequently, for instance improving readability in sunlight and/or changing control options. Suggested control options were via speech or via touch (e.g., touching the thigh to walk and touching the bottom to sit down). Some participants suggested to relocate the control to the crutches, as long as the crutches are needed for balance support. This crutch-control would preferably include a small screen on which different speeds, step heights, and step frequencies could be selected. In addition, participants mentioned that keeping balance with the exoskeleton (especially in stance) required much physical and mental effort. To be able to focus on other things, such as a conversation or use of kitchen utensils, balance improvements in the future exoskeleton were desired.
P11male_lowSCI: “What’s essential in that suit [=exoskeleton]? What can still be improved? Well, first of all, the balance. Not having to use crutches anymore is the most important thing. […] That you don’t constantly need to keep your balance; the suit should do that for you. That’s what I think is crucial. Suppose I could walk the way I am doing now, but could keep my balance without needing crutches. That would immediately be a real functional improvement.”
Step and speed adjustments were desired so that the exoskeleton could be used more broadly.
P9male_lowSCI: “It should have gears, like in a car. Or let’s take a bike as an example. Let’s say you have one, two, three positions and that the third position is the highest gear. This gear allows you to, for example, take a big step, or increase your pace. That works perfectly for outdoors. Position two would then be something just in between. And position one would reduce the length of your steps and their frequency. Then I think it could be used functionally in a home situation indoors.”
In addition, some participants expressed the wish to don and doff the exoskeleton, without needing several preparations: P10female_highSCI: “You also have to bring something [a stool] on which you put it [the exoskeleton], to be able to don it there.” and P6female_lowSCI. “I don’t want to spend more time putting it on than that I’m actually using it.”
Second circle: small, lightweight, and tailor made
The improvements in the second circle were mostly related to transporting the exoskeleton and adjusting the hardware to the body of the user. Participants acknowledged that they could not lift and transport the exoskeleton (in a convenient way) by themselves, due to the weight and the physical dimensions. This hampered exoskeleton uses considerably during daily activities, but also to socially interact.
P8male_highSCI: “But maybe it will make a difference when carrying it to and from the car. If I can move it myself, for example, in three sections instead of one big awkward lump for which I would need someone else to help me. […] It wouldn’t be so heavy then. Maybe it’ll save some space. That would make me independent. I’d be very happy, even if it did take me five minutes longer to put it on.”
P9male_lowSCI: “It is quite a bulky thing to carry around [….] The volume could be a barrier when you would want to take it with you to walk somewhere else. So suppose you're at home and you're walking here in the neighborhood. I’m with my spouse or a close friend and we want to go somewhere. Then the volume could be a problem.”
In addition, participants mentioned that, especially due to the crutches, you need a lot of space. Therefore, some participants noted that their (wheelchair-friendly) house was too cramped for exoskeleton use during daily in-home activities. A minority of the participants expressed the desire for an exoskeleton that is exactly tailored to their body but can also be adjusted to different people, in case you want to share an exoskeleton.
P7female_highSCI: “Normally you have enough space but now it feels mega small, because with that suit [=exoskeleton] and those crutches you’re a bit like a big robot stomping around the house. It’s not very pleasant. I hope that in the future they’ll be able to develop suits that are as compact as possible, so that you can easily use [them] at home. It would be really great if I could do more things standing or walking.”
Third circle: safe, comfortable, and less distinctive
Opinions on improving safety were diverse. Some participants considered the safety of the exoskeleton as very important and even something that—if not guaranteed—would lead to disuse, while others felt that using the exoskeleton was safe and the risks were similar to that of other activities.
P5female_highSCI “Improvements that would make me use it regularly to move about? Well, most certainly an emergency stop. […] Suppose getting up doesn’t go well… if you could just press something in your crutches if things start to go wrong, and you’d be able to get back in the right position and slowly lower it, so that you go back to base [the sitting position], if I had had those options I think it would have been less scary for me.”
P4female_highSCI “In the end there is one thing you don't want and that is falling.”
P9male_lowSCI: “Yes, you can fall, but you can also fall over in your wheelchair, you know. There’s no danger of that. Zero, nil, nothing! It may happen that your crutch slips when you’re walking somewhere and that it bounces a bit, but so what? If I go handcycling, another road users may not see me and I may get hit by a car, but that’s a risk I’m willing to take.”
Participants who desired an exoskeleton that could be worn all day during daily activities or in social situations, such as the pub, mentioned that it should be comfortable to wear and that, for example, a battery on your back would be inconvenient to sit comfortably (anywhere). Some participants expressed that the ultimate level of comfort would be not feeling or noticing you’re wearing an exoskeleton during all daily activities or while sitting in the wheelchair.
P11male_lowSCI: “It’s just a hassle with that thing. You’re completely constricted, even when sitting. You can’t really move well in it. So I could sit in the pub in it, but I wouldn’t feel very relaxed.”
P3male_lowSCI: “That you don't even think about can I take that thing with me. That that thing is so intertwined with you, that would be the best thing…. I would maybe take a shower standing up if I could…. […] That you can just wear the suit in bed, so to speak. That you don't notice that you have it on. That you just wake up, that you think of oh run upstairs.”
P10female_highSCI: “That you just put it on in the morning and keep it on all day. Of course, that would be totally super. That you might sit in your wheelchair with it, and do bits in your wheelchair. And when you want to get up you can just stand up. That would be the ultimate vision of the future. That you just put it on like a pair of pants and keep it on all day. And also get into your car with it without a wheelchair.”
Although most participants focused more on the functionality of the exoskeleton, some participants expressed the wish to make the exoskeleton’s appearance as close to normal as possible, so that they don’t attract (extra) attention in social situations (e.g., less visible and less noisy).
P1male_highSCI: “That it [the walking pattern] looks natural. So that people don’t think you’re some kind of robot. I think you could easily do this with the latest software.”
P9male_lowSCI: “If you have a suit [exoskeleton] like that and you go to a party, you are more an attraction. And I think a suit is for you to walk in, not to be seen in. At least that's how I see it. […] If there would be a party with forty people present, and I walk in wearing a suit like that, then forty people's eyes are on that suit. But it wasn't about the suit, it was about the party.”
Fourth circle: affordable and durable
Most participants indicated that the current exoskeletons are too expensive with respect to what it is currently capable of. Therefore, almost all participants focused on improvements to its functionality (not its affordability). However, a minority mentioned that not all improvements were necessary and one participant pointed out that the exoskeleton should have fewer functionalities so that it could be marketed cheaper and become accessible to a larger group.
P1male_highSCI: “I think you first need to focus on affordability and, of course, functionality, particularly if you want to stimulate further development. After all, it’s a very specific target group.”
In addition, only a few participants mentioned improvements in the durability of the exoskeleton.
P13male_highSCI “Then [to be able to walk in the rain] you need to make it waterproof. So, for example, the bearings need to be well sealed, and you need to use corrosion-resistant material. Like mobile phones. All mobile phones are water resistant nowadays… So that means a backpack… but that will all drive up the price.”
Discussion
In this qualitative study, experienced exoskeleton users expressed three future purposes of exoskeleton use: for exercise, social interaction, and daily activities. Using the current exoskeleton for exercise is already possible [Citation12,Citation30,Citation31] and only a few improvements to make it easier to use were desired for this purpose. To facilitate social interaction, besides easier to use, the exoskeleton should also be small and lightweight, tailored to the person, and for some people less distinctive. For the ultimate purpose of future exoskeleton use, namely during daily activities, the most improvements were needed.
The extent of improvements needed for daily activities varied between participants, possibly reflecting participants who kept their answers closer to nowadays reality (i.e., feasible with the current technological knowledge) and participants who were willing/dared to describe their ultimate future exoskeleton. For instance, improvements to the comfort level varied from improving seating comfort in a (wheel)chair to a level where one becomes intertwined with the exoskeleton (i.e., wearing it in bed and while showering). A similar embodiment process has been described in people becoming en-wheeled with a (sports)wheelchair [Citation32,Citation33]. Although participants who described their ultimate exoskeleton may have given unrealistic answers from a designer’s perspective, there is great value in these answers because they provide insight into what is ultimately pursued. The discrepancy between what is ultimately pursued and what is possible with the current exoskeleton technology is important information for clinicians to manage expectations regarding exoskeleton use in daily life. Exoskeleton use during daily activities was often discussed in the context of participants' current, wheelchair-bound, execution of daily activities. Contrary to wheelchair use, the motive for exoskeleton use was also referred to as “for fun.” Something that was not stated by the participants about their everyday wheelchair, was only considered an assistive device for transportation from one place to the other.
Although we (partly) found similar areas of improvement as in previous studies, the relevance and content of these areas of improvement sometimes differed. A previous survey study concluded that safety, affordability, ease of use, and comfort were considered the most important areas of improvement [Citation16]. The relevance of improving the ease of use was supported by our findings (i.e., inner circle in ). However, we found that the other areas of improvement mentioned in the survey study (i.e., safety, affordability, and comfort) [Citation16], were more purpose- and person-dependent. This suggests that these areas of improvement are less relevant to be improved first. Especially for safety, the relatively low relevance of improvement found in the current study was not expected from both a clinical and a design perspective. In addition, the content within an area of improvement sometimes differed from previous findings. For example, the current study revealed specific improvements to the remote control watch (e.g., readability) to make the exoskeleton easier to use, instead of the earlier reported improvements to the comprehensive concept of ‘ease of use’ of the exoskeleton [Citation13–18]. In addition, being able to adjust the speed (i.e., accelerate and decelerate) while using the exoskeleton in various situations was desired, instead of maximizing the speed of the exoskeleton itself [Citation13,Citation15–18]. Also, a reduction in the number of preparations needed before exoskeleton use (e.g., placing the exoskeleton on a stool) was desired, whereas, once these preparations were made, the previously indicated concern with donning and doffing the exoskeleton [Citation13–18] was not an issue according to our participants. These detailed, yet very important, improvements have hardly been discussed in previous studies.
The discrepancy compared to previous studies could be attributed to the distinct enrolled (patient) populations. The suggested improvements in previous studies are from researchers and individuals who have not used the exoskeleton [Citation13–19]. Only people with exoskeleton experience (outside the clinical setting) will be able to mention detailed, yet very important, improvements for home and community use, such as to the remote control watch. In addition, all participants involved in this study can be seen as “early adopters,” meaning that they were already willing to use these not yet fully developed exoskeletons. Moreover, they were able to use these exoskeletons in their current form in the community, suggesting that they were motor competent. However, it is important to keep in mind that the needs and requirements of these competent early adopters, may differ from the ultimate target group of the exoskeleton (i.e., the general complete SCI population). Nevertheless, also in these early adopters, multiple improvements were mentioned before the technology will become mainstream for a larger population.
To target a larger population, the transferability of the results to different patient populations (e.g., incomplete SCI) is important. The three purposes of exoskeleton use expressed by people with complete SCI in this study (i.e., exercise, social interaction, and daily use), could be of interest for people with incomplete SCI as well [Citation17]. For instance, similar daily activities (e.g., taking a shower or grocery shopping) and social interactions (e.g., playing with their kids) have been reported by novice people with incomplete SCI [Citation17] and are confirmed by our experienced exoskeleton users with complete SCI. For people with incomplete SCI an additional major purpose of the use is expected, namely gait re-training with the goal of improving walking without an exoskeleton. Whilst our study participants did not consider gait re-training a realistic option for them, the wish for this purpose of use was reported by people with an incomplete SCI [Citation17]. Indeed, several studies have shown that people with incomplete SCI can improve their walking speed and walking distance through exoskeleton training [Citation34–37] and that these improvements can be transferred to walking without an exoskeleton [Citation35,Citation38]. An important exoskeleton improvement to facilitate gait re-training is that the guidance force of the exoskeleton can be adjusted to meet the (gait) capacity of the user. This is currently possible with the Ekso bionics™ [Citation39] and Indego® [Citation40] exoskeleton, but not with the ReWalk™ [Citation41] exoskeleton.
Although participants in the current study were particularly experienced with the ReWalk™ exoskeleton, we expect that for people with complete SCI the purposes of use, areas of improvement, and to a large extent, the relevance of the improvements are generalisable to other wearable exoskeletons that rely on upper extremity support. Caution applies to the remote control watch and the ‘small and lightweight’-suggestion because these aspects differ between the most commonly used exoskeletons (i.e., ReWalk™, Indego®, and Ekso bionics™) [Citation39–41].
Strengths and limitations
A strength of the current study is that almost the entire population of Dutch people with a complete SCI who used an exoskeleton in the home and in the community setting were interviewed and that data saturation was met. However, this population consisted of a limited number of selected and young people and the community exoskeleton use was relatively long ago for some participants, which could have led to recall bias. To recall memories, and, thus, minimize the recall bias, a video of the participant's own ReWalk™ exoskeleton use was shown before the interview.
Conclusion
Experienced exoskeleton users expressed three future purposes of exoskeleton use: for daily activities, exercise, and social interaction. Increasingly more advanced improvements of future exoskeletons are needed to transition from an exercise purpose to social interaction, and ultimately use during daily activities. In the current study, detailed suggestions for improvements from experienced exoskeleton users have been made. Only when multiple of these suggestions are adjusted, the exoskeleton can be used to its full potential. We want to encourage future researchers to collaborate with exoskeleton designers to attain the ultimate goal of shifting the role of the exoskeleton user from being a ‘passenger’ to being a ‘pilot’ so that the exoskeleton becomes a device usable in everyday life. Only when experienced users can test new developments, the true benefits of these developments can be assessed.
Supplementary_Table_1.docx
Download MS Word (53.8 KB)Supplementary_material_Interview_guide.docx
Download MS Word (34.6 KB)Disclosure statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Additional information
Funding
References
- Nas K, Yazmalar L, Şah V, et al. Rehabilitation of spinal cord injuries. World J Orthop. 2015;6(1):8–16.
- Burns AS, Marino RJ, Flanders AE, et al. Clinical diagnosis and prognosis following spinal cord injury. Handb Clin Neurol. 2012;109:47-62.
- Kay ED, Deutsch A, Wuermser LA. Predicting walking at discharge from inpatient rehabilitation after a traumatic spinal cord injury. Arch Phys Med Rehabil. 2007;88(6):745–750.
- Jensen MP, Truitt AR, Schomer KG, et al. Frequency and age effects of secondary health conditions in individuals with spinal cord injury: a scoping review. Spinal Cord. 2013;51(12):882–892.
- Adriaansen JJE, Ruijs LEM, van Koppenhagen CF, et al. Secondary health conditions and quality of life in persons living with spinal cord injury for at least ten years. J Rehabil Med. 2016;48(10):853–860.
- Shi D, Zhang W, Zhang W, et al. A review on lower limb rehabilitation exoskeleton robots. Chinese J Mech Eng. 2019;32(1):1–11.
- Lajeunesse V, Vincent C, Routhier F, et al. Exoskeletons’ design and usefulness evidence according to a systematic review of lower limb exoskeletons used for functional mobility by people with spinal cord injury. Disabil Rehabil Assist Technol. 2015;3107:1–13.
- Baunsgaard C, Nissen U, Brust A, et al. Exoskeleton gait training after spinal cord injury: an exploratory study on secondary health conditions. J Rehabil Med. 2018;50(9):806–813.
- Miller LE, Zimmermann AK, Herbert WG. Clinical effectiveness and safety of powered exoskeleton-assisted walking in patients with spinal cord injury: systematic review with meta-analysis. MDER. 2016;22:455–466.
- Chun A, Asselin PK, Knezevic S, et al. Changes in bowel function following exoskeletal-assisted walking in persons with spinal cord injury: an observational pilot study. Spinal Cord. 2020;58(4):459–466.
- Cahill A, Ginley OM, Bertrand C, et al. Gym-based exoskeleton walking: a preliminary exploration of non-ambulatory end-user perspectives. Disabil Health J. 2018;11(3):478–485.
- van Dijsseldonk RB, van Nes IJW, Geurts ACH, et al. Exoskeleton home and community use in people with complete spinal cord injury. Sci Rep. 2020;10(1):1–8.
- Gorgey AS. Robotic exoskeletons: the current pros and cons. World J Orthop. 2018;9(9):112–119.
- Kandilakis C, Sasso-Lance E. Exoskeletons for personal use after spinal cord injury. Arch Phys Med Rehabil 2021;102(2):331–337.
- Palermo AE, Maher JL, Baunsgaard CB, et al. Clinician-focused overview of bionic exoskeleton use after spinal cord injury. Top Spinal Cord Inj Rehabil. 2017;23(3):234–244.
- Wolff J, Parker C, Borisoff J, et al. A survey of stakeholder perspectives on a proposed combined exoskeleton-wheelchair technology. J Neuroeng Rehab. 2014;11:1–10.
- Lajeunesse V, Routhier F, Vincent C, et al. Perspectives of individuals with incomplete spinal cord injury concerning the usability of lower limb exoskeletons: an exploratory study. TAD. 2018;30(1–2):63–76.
- van Silfhout L, Hosman AJF, van de Meent H, et al. Design recommendations for exoskeletons: perspectives of individuals with spinal cord injury. J Spinal Cord Med. 2021. DOI:10.1080/10790268.2021.1926177
- Fritz H, Patzer D, Galen SS. Robotic exoskeletons for reengaging in everyday activities: promises, pitfalls, and opportunities. Disabil Rehabil. 2019;41(5):560–563.
- Robinson OC. Sampling in interview-based qualitative research: a theoretical and practical guide. Qual Res Psychol. 2014;11(1):25–41.
- Kallio H, Pietilä AM, Johnson M, et al. Systematic methodological review: developing a framework for a qualitative semi-structured interview guide. J Adv Nurs. 2016;72(12):2954–2965.
- Turner DW. Qualitative interview design: a practical guide for novice investigators. Qual Rep. 2010;15:754–760.
- van Dijsseldonk RB, Rijken H, van Nes IJW, et al. A framework for measuring the progress in exoskeleton skills in people with complete spinal cord injury. Front Neurosci. 2017;11:699–612.
- Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–357.
- Braun V, Clarke V. Qualitative research in psychology using thematic analysis in psychology using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
- Tuckett AG. Applying thematic analysis theory to practice: a researcher's experience. Contemp Nurse. 2005;19(1–2):75–87.
- Kalu FA, Bwalya JC. What makes qualitative research good research? An exploratory analysis of critical elements. IJSSR. 2017;5(2):43–56.
- Demers L, Weiss-Lambrou R, Ska B. The Quebec user evaluation of satisfaction with assistive technology (QUEST 2.0): an overview and recent progress. TAD. 2002;14(3):101–105.
- Boeije H. Analysis in qualitative research. Boom Lemma; 2012.
- Kolakowsky-Hayner SA. Safety and feasibility of using the Ekso™ bionic exoskeleton to aid ambulation after spinal cord injury. J Spine. 2013;4:1–8.
- Gagnon DH, Escalona MJ, Vermette M, et al. Locomotor training using an overground robotic exoskeleton in long-term manual wheelchair users with a chronic spinal cord injury living in the community: lessons learned from a feasibility study in terms of recruitment, attendance, learnability, performa. J Neuroeng Rehab. 2018;15:1–12.
- Papadimitriou C. Becoming en-wheeled: the situated accomplishment of re-embodiment as a wheelchair user after spinal cord injury. Disabil Soc. 2008;23(7):691–704.
- Monforte J, Smith B, Pérez-Samaniego V. ‘It's not a part of me, but it is what it is’: the struggle of becoming en-wheeled after spinal cord injury. Disabil Rehabil. 2021;43(17):2447–2453.
- Benson I, Hart K, Tussler D, et al. Lower-limb exoskeletons for individuals with chronic spinal cord injury: findings from a feasibility study. Clin Rehabil. 2016;30(1):73–84.
- Grasmücke D, et al. Against the odds: what to expect in rehabilitation of chronic spinal cord injury with a neurologically controlled hybrid assistive limb exoskeleton. A subgroup analysis of 55 patients according to age and lesion level. Neurosurg Focus. 2017;42:1–9.
- Khan AS, Livingstone DC, Hurd CL, et al. Retraining walking over ground in a powered exoskeleton after spinal cord injury: a prospective cohort study to examine functional gains and neuroplasticity. J Neuroeng Rehab. 2019;16:1–17.
- Kubota S, Nakata Y, Eguchi K, et al. Feasibility of rehabilitation training with a newly developed wearable robot for patients with limited mobility. Arch Phys Med Rehabil. 2013;94(6):1080–1087.
- Baunsgaard CB, Nissen UV, Brust AK, et al. Gait training after spinal cord injury: safety, feasibility and gait function following 8 weeks of training with the exoskeletons from Ekso bionics article. Spinal Cord. 2017;56:106–116.
- Food and Drug Administration. Ekso™ and Ekso GT™ – K143690; 2016.
- Food and Drug Administration. Indego® – K173530; 2018 [cited 2019 Oct 10]. p. 1–12. Available from: https://www.accessdata.fda.gov/cdrh_docs/pdf17/K173530.pdf
- Food and Drug Administration. ReWalk™ P6.0 – K200032; 2020. p. 1–6
