Abstract
Purpose
Some parents of children with DMD find their role challenging, affecting quality of life. To inform support methods, we aimed to understand the lived experiences of parents and how these interact with disease progression.
Materials and methods
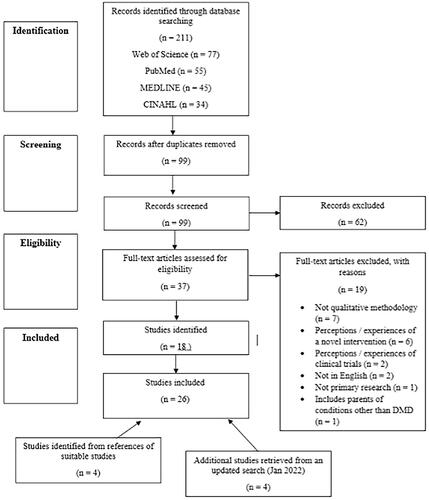
PRISMA informed protocol development. Qualitative and mixed methods studies were included. Four databases were searched and study quality was assessed using a standardised measure. Extracted data were analysed using thematic synthesis.
Results
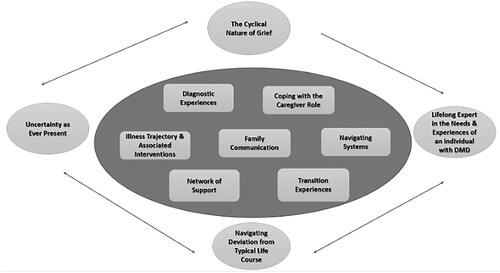
26 studies were included, comprising 362 parents. Seven descriptive themes were apparent: “Diagnostic Experiences”, “Coping with the Caregiver Role”, “Illness Trajectory and Associated Interventions”, “Family Communication”, “Network of Support”, “Navigating Systems” and “Transition Experiences”. Four analytical themes were then derived: “The Cyclical Nature of Grief”, “Lifelong Expert in the Needs and Experiences of an Individual with DMD”, “Navigating Deviation from Typical Life Course” and “Uncertainty as Ever Present”.
Conclusion
The extant evidence suggests that the experience of parenting a child with DMD is often characterised by: a cycle of grief that begins at diagnosis, which runs parallel to the development of expertise in caregiving; within this parents notice deviations from their child’s and their own expected life course and adjust to the emotions and uncertainty that this can bring.
Professionals should be cognisant to the complex grief process associated with DMD, which occurs from diagnosis onwards.
There should be continued support for parents following bereavement.
Peer support groups may also offer parents ways to maintain well-being.
The necessity for parents to function effectively within an uncertain context that induces challenging emotions suggests a role for psychological therapies.
IMPLICATIONS FOR REHABILITATION
Duchenne muscular dystrophy (DMD) is an X chromosome linked progressive neuromuscular condition that occurs in between 10.2 and 12.57 per 100,000 live births [Citation1]. DMD is the result of mutations to the dystrophin gene, which impacts the dystrophin protein and leads to muscle degeneration [Citation1,Citation2]. Although it is possible for females to be affected, DMD predominantly occurs in males, with the first signs becoming apparent around 3 years old and diagnosis typically around 4 years old [Citation2,Citation3]. Disease progression, without steroid treatment, results in young people becoming non-ambulatory and wheelchair reliant by 13 years of age [Citation1,Citation2]. In untreated individuals, following loss of ambulation scoliosis tends to develop and hand and arm movement deteriorates [Citation2,Citation4]. By late adolescence, continual muscle weakening results in cardiomyopathy and respiratory difficulties which, without treatment, are ultimately fatal by the second or third decade of life [Citation1,Citation2]. Those with DMD also often have co-occurring conditions, with a quarter of individuals having an intellectual disability and around 15% presenting with autism spectrum disorder [Citation1,Citation5]. The introduction of the DMD standards of care [Citation5–7] has enhanced professional awareness of the most up to date therapies for DMD, including steroids, surgery, medication, ventilation, and cardiac interventions. With continued improvements in care, the expected lifespan of individuals with DMD has continued to increase and a proportion of people with the condition now live into the fourth and fifth decades [Citation8].
Individuals with DMD are at increased risk of experiencing mental health difficulties, particularly at condition transition points, such as loss of ambulation and initiation of ventilation [Citation5]. However, several studies have shown that quality of life (QoL) for many with DMD is comparable to age matched peers and many report frequently engaging in personally meaningful activities [Citation9–11].
In some instances, DMD may have a detrimental impact on the QoL of parents of individuals with the condition. While the overwhelming majority parents find the experience of parenting in this context highly rewarding [Citation12] and many show high levels of resilience to the stress implicit in caregiving [Citation8], studies have demonstrated that on average parents of those with DMD report lower QoL and elevated anxiety and depression [Citation13,Citation14]. The modified Supportive Care Needs Framework, proposed for parenting needs when children have rare conditions [Citation15], may help understand this phenomenon. This model specifies six support needs of parent caregivers: emotional, practical, physical, psychological, informational and social. Providing care to individuals with DMD can be physically demanding. For example, the requirement to lift the person with DMD can result in pain and injuries for some caregivers [Citation13,Citation14]. Caring for a child with DMD can also have a financial impact. Medical and intervention costs increase with disease progression, and the requirement to take leave from work to provide care can affect income [Citation16,Citation17]. Parenting in this context can also have emotional consequences. Evidence suggests that parents who have stepped back from their career also experience lower emotional well-being [Citation9]. While care procedures can become sources of anxiety, with some parents holding fears that if they do not monitor the ventilation equipment sufficiently they could be responsible for their child’s death [Citation18]. Also, the genetic basis of DMD means that mothers, in particular, can experience guilt for passing the gene to their children as the condition is inherited on the X chromosome [Citation14]. Finally, socially, parents who feel isolated or experience less family cohesiveness may be prone to poorer well-being [Citation19].
This caregiver burden may increase as DMD progresses [Citation20]. Possibly as a result of care demands, such as repositioning during sleep, Nozoe et al. [Citation18] found that caregiver mothers had poorer sleep than controls. Here, sleep quality was particularly poor in mothers of those who had recently commenced non-invasive ventilation. Also, later in the disease course parents may be susceptible to worry about their child’s deteriorating abilities, alongside a reduction in time for their own rest or social outlets [Citation21].
It is important again to recognise that, while challenging, most parents find their role rewarding. Indeed, a recent survey showed that 82% were unwilling to transfer caregiving duties to someone else [Citation14]. Yet, it is clear that caregiving can, in cases, have an impact on parents' QoL and mood, which perhaps increases as their child’s physical health deteriorates. Qualitative studies may provide deeper insights into the quality of parental experiences. This can help us understand with more nuance what factors contribute to QoL and mood, and therefore, how to support parents who are undertaking this important and valuable role. Two previous systematic reviews have collated qualitative studies examining specific aspects of caregiving in DMD. Landfeldt et al. [Citation13] analysed all quantitative and qualitative studies on caregiver burden in DMD. The resulting narrative synthesis, of mostly quantitative studies, suggested that caregiving burden is negatively associated with a range of outcomes, from QoL, sleep, family function and mood to work productivity. A further narrative review by Glover et al. [Citation8] specifically considered resilience in caregivers of those with DMD and suggested that resilience is a common feature of the parental experience and it is influenced by coping methods and social support. Neither review was positioned to characterise the broader experience of parents of individuals with DMD, nor was a qualitative synthesis undertaken. An examination of the wider extant qualitative literature of parental experiences may be helpful for providing a more complete picture of parenting in this context. This may provide an understanding of a wider range of opportunities to support parents. Therefore, the present systematic review set out to apply a detailed qualitative synthesis methodology to all existing qualitative literature detailing the experiences of parents of individuals with DMD. The specific research questions addressed by this review were:
What is the lived experienced of being a parent to an individual with DMD?
How do parenting experiences interact with the age of the individual with DMD or disease progression?
Materials and methods
Search strategy and study selection criteria
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [Citation22] and the Enhancing Transparency in Reporting the Synthesis of Qualitative Research (ENTREQ) [Citation23] guidelines were followed in the completion of this review. The protocol was pre-registered on Prospero (registration number is CRD42020197303). The SPIDER tool [Citation24] informed the inclusion and exclusion criteria and the search strategy, which are summarised below:
Inclusion:
Sample: Parents performing a caregiving role for an adult or child with DMD
Phenomenon of Interest: Parents’ experiences of parenting an individual with DMD
Design: Qualitative and mixed method studies where it is possible to identify the quotations of parents. Any qualitative data collection technique is appropriate e.g. interview or focus group.
Evaluation: Qualitative analysis
Research type: Primary research studies published in a peer reviewed journal in the English language. Only studies published since the year 2000 due to DMD care advances.
Exclusion criteria:
Phenomenon of Interest: Parents’ experiences of parenting individuals with conditions other than DMD. For example, parents’ experiences of a novel intervention or parents’ perceptions regarding taking part in clinical trials.
Design: Qualitative and mixed methods studies that include parents of those with DMD alongside parents of those with other conditions.
Research type: Review articles were not included. Grey literature was not searched
The search strategy is outlined in and a summary is provided below:
Table 1. Search strategy.
“Parent*” OR “caregiver” OR “mother” OR “father” AND “Duchenne Muscular Dystrophy” AND “interview*” OR “focus group*” OR “qualitative” OR “mixed method*” OR “experience*” OR “understand*” OR “attitude” OR “feel*” OR “view” OR “opinion” OR “perce*” OR “belie*”.
This search strategy was initially carried out in November 2020 in four databases: Web of Science, PubMed, MEDLINE and CINAHL. Reference lists of included studies were searched to identify additional relevant studies. We repeated the search again in January 2022.
Study selection
The titles of the articles retrieved from searches were screened by the first author CMD and duplicates were disregarded. CMD subsequently screened the article titles and abstracts to determine their eligibility, in line with the inclusion and exclusion criteria, and excluded ineligible studies. In cases where it was unclear whether a study was eligible based on the title and abstract, CMD retrieved the full text. Where it remained unclear whether a study met the inclusion/exclusion criteria the full text was reviewed independently by a second researcher (CDG) and the two researchers then met to make a decision. shows how this process was recorded as a PRISMA flowchart.
Quality assessment
The ten-item Critical Appraisal Skills Programme Checklist (CASP; see Appendix A) [Citation25] for qualitative research was used to evaluate the quality of each of the studies included in the review. To enhance the reliability and validity of ratings and reduce systematic errors in rating, the first stage of quality assessment involved independent rating of a proportion of the initial 22 included studies (25%; n = 6) by two researchers, CMD and a second reviewer (AH). Initially interrater agreement, determined through a Cohen’s kappa calculation, was κ = .76. CMD and AH met to discuss and resolve differences in their independent ratings and following this κ = .94. Subsequently, CMD rated the remainder of the papers. CASP ratings for all papers are outlined in . Studies were not excluded due to their results on the quality assessment.
Table 2. CASP quality assessment [Citation26].
Data extraction
A standard data extraction form was applied to all included studies. The following information was extracted: title, author(s), year of study, country of study, study aims, number of participants, type of participants (e.g. mothers or fathers) and mean age or range, mean age or range of the individuals being parented and study methodology and analysis. Data labelled findings of results, which included results reported in the abstract and the entire section of the paper labelled results or findings, were extracted for the thematic synthesis. To help ensure no systematic errors in data extraction for a subset of the studies from the initial search (25%; n = 6) AH independently extracted the data using the form. CMD and AH then met to discuss discrepancies in the data extraction, and CMD alone extracted the remainder.
Data synthesis
Thematic synthesis [Citation52] was deemed the most appropriate analytic technique, for two reasons. First, we expected the studies to differ in terms of epistemology and methodology, and thematic synthesis can construct themes from varied methodologies [Citation53]. Second, it is argued that parsimonious presentation of results as themes provides accessibility to practitioners developing interventions [Citation53].
The process of thematic synthesis involved entering data into NVIVO [Citation54]. CMD then coded this data line by line. CDG, a research clinical psychologist with experience working with muscular dystrophy, reviewed a subset of the coding. From these initial codes, inductive descriptive themes were devised, as a result of code prominence and frequency. The final stage of analysis involved the development of inductive analytical themes, which were more in-depth than the descriptive themes and answered the review questions. The research team, CMD, CDG and RMQ, a Neuromuscular Consultant with specialist expertise in DMD, then met to examine the analytical themes. Here themes and supporting quotations were reviewed and alternative possibilities explored amongst the team. Data extracted from studies returned in the updated search were integrated into the descriptive and analytic themes.
Results
Summary of findings
As shown in and , 22 studies were initially included in the review, with 4 added following the updated search in January 2022 [Citation26,Citation40,Citation46,Citation48]. Giving a total of 26 studies included in the review. Publication dates ranged from 2004 until 2021. The largest number of studies (N = 8) were from the UK, with five from the USA, five from Canada, two from Japan and one from each of the following countries: Australia, Brazil, Norway, the Netherlands, India and Jordan. Across the papers, there were 362 parents. The exact breakdown of numbers of mothers and fathers was not always reported. However, as is common, mothers were more frequently represented in the cohorts. The majority of studies collected data via semi-structured interviews. The most common analytic technique reported was thematic analysis, which was applied in 13 of the studies, followed by grounded theory which was applied in four studies. Of note, three papers did not indicate the analytic methods applied.
Table 3. Summary of included studies.
Quality assessment
As shown in overall, quality ratings were high. Yet, due to the importance placed on considering the relationship between participants and the researcher in qualitative research, it is noteworthy that this was only clearly outlined in nine of the studies (Criterion 6 “Adequate consideration of researcher-participant relationships”). More recent studies were more likely to consider the relationship between the participants and researcher. There were some concerns about the reporting of data analysis methods (Criterion 8, “Data analysis rigorous”) and ethical considerations (Criterion 7, “Adequate consideration of ethical issues”) in a minority of studies.
Descriptive themes
The seven descriptive themes identified are outlined below and represented in the centre of . In line with ENTREQ [Citation23] participant quotations and author interpretations were differentiated with participant quotations bold and author interpretations italic.
Figure 2. Diagram representing the relationship between the themes evident in the analysis. Note. The four analytical themes have been placed around the outside of the figure. The arrows demonstrate the cyclical relationship between these analytical themes. The seven descriptive themes have been placed in the centre. Each descriptive theme is equally related to the other descriptive themes as important facets of the experience of being a parent of an individual with DMD.
Diagnostic experiences
Experiences of the DMD diagnostic process were described across studies [Citation26,Citation28,Citation37–39,Citation42,Citation43,Citation47–49]. Often parents had initial concerns about their child’s health, but had such concerns dismissed “he was about 3½ or 4 years old and he was not keeping up with other kids…The paediatrician told us we were just worrying” [Citation28,p.287]. At times this dismissal alleviated parents’ concerns and they felt a sense reassurance for a short time [Citation38,Citation49]. Yet when the child’s symptoms remained, parents felt the need to consult multiple professionals in the hope that someone would take their concerns seriously [Citation28,Citation38,Citation49]. This journey involved “false reassurance” [Citation49,p.1296], which ultimately resulted in “diagnostic delay” [Citation38,p.151]. When a diagnosis was received, many parents were unhappy with the delivery, “I would think that a doctor would actually take the time to call and maybe throw a little bit of psychology into it” [Citation28,p.289], which made accepting this life-changing condition more difficult [Citation39]. Parents often experienced a period of “grief” [Citation42,p.107] following the diagnosis and needed time to come to terms with the “loss of the idealized son” [Citation37,p.3086]. “Other caregivers described a general feeling of “enormous sadness” at their son’s diagnosis” [Citation48,p.6].
Coping with the caregiver role
Within this theme a deviation from parents’ expectations of “normal parenting” is emphasised [Citation28,Citation29,Citation39,Citation42,Citation43,Citation45,Citation47,Citation50,Citation51] alongside the “multiple physical demands” [Citation45,p.9]. that are implicit in caregiving. Parents described how they “adjusted” [Citation51,p.749] to the caregiving demands, where they were also required to perform typical parenting tasks – “muscular dystrophy– related stressors occur in the context of ordinary life stressors that would be experienced in the course of parenting any child” [Citation29,p.136]. Parents “described how the strain of constant lifting and carrying had resulted in them experiencing back problems, including sciatica, back ache and muscle spasms” [Citation48,p.5].
Whether a parent accepts the role of primary caregiver or supporting caregiver, the gender of the parent appeared to influence experiences [Citation26]. One mother stated: “Always, I have put my needs aside …any time. I moved house for my son, drifted from job to job” [Citation51,p.749]. Studies showed that caregiving was allocated in line with traditional gender roles with mothers “more likely to focus on day-to-day care of the affected child” [Citation39,p.1227] and fathers more likely to get involved in activities such as fundraising [Citation39], with one study a notable exception [Citation43]. Yet even when the traditional gender division of care was apparent, given the demands of caring for their child, fathers were also required to be active beyond the traditional father role. For fathers, this meant ensuring the family had sufficient knowledge of the condition, supporting mothers with the physically demanding caregiving tasks and taking an active role in planning for future support needs [Citation26,Citation37,Citation39,Citation45,Citation46]. One study indicated how an increase in the individual with DMD’s weight can increase physical demands [Citation46]. One father stated “I have come to realize my great importance in taking care of my child, and his mother and I have reached a state of balance and the distribution of roles between us” [Citation26,p.7].
A present moment focus is adopted by many parents, thereby ensuring that they do not become overwhelmed with caregiving demands [Citation27,Citation29,Citation30,Citation39,Citation41,Citation42,Citation45] “We get through by taking each day as it comes, and whatever problems arise, we deal with them when they arise” [Citation27,p.1199]. Parents discussed a range of other coping mechanisms that helped [Citation29,Citation30,Citation32,Citation37,Citation39,Citation42] but interestingly maladaptive coping strategies were only explicitly discussed in three studies [Citation30,Citation32,Citation48]. It was reported that “In a small number of cases, parents had become depressed, developed anxiety or resorted to alcohol or drug use as a way of coping” [Citation30,p.189]. Another study indicated that “Some caregivers reported that they had needed to take time off sick for physical and mental health issues that had arisen due to their son’s DMD” [Citation48,p.7].
Illness trajectory and associated interventions
Progression of DMD was discussed by many parents [Citation26,Citation27,Citation29,Citation32,Citation36,Citation37,Citation39–48,Citation50]. They were aware of the individual’s “deteriorating condition” [Citation36,p.76] and discussed the “functional losses” [Citation37,p.3086], both through experience “because of the progression of DMD, the boys are helpless in all their self-care activities, and Bob’s role as the caregiver entails doing all these things for them” [Citation43,p.87] or anticipation that their son would eventually move towards this stage, “We’ve been on this plateau phase with [names son] … I’m now turning more of my thoughts and attention to [names son] because he’s now deteriorating” [Citation32,p.488]. Other parents noted that their child struggles with progression, “I know his symptoms are drastically progressing since last 6 months. And he is never ready to accept this and creating numerous issues at home” [Citation40,p.148].
For many parents, the end of ambulation signified a significant point in the progress of the condition [Citation29,Citation39,Citation41,Citation42,Citation47], which often led to the realisation that “a lot of your issues medically that come up occur after the walking stops” [Citation29,p.137]. One study noted that “The unavoidable use of glucocorticoids, along with mobility deterioration both contributed to the boys’ weight increasing” [Citation46,p.5]. Parents also support their children with treatment decisions and often must decide whether an intervention should be accepted or continued “We never put our son on prednisone. We were more concerned about quality of life, and didn’t like the possible side-effects” [Citation47,p.391]. On the other hand, parents discussed the benefits of their child accepting certain interventions, “…with [ataluren] it’s like having a new lease of life, it’s like he’s been given an extra chance, he’s been given a few more years of walking…” [Citation48,p.9].
Family communication
Family communication was not openly discussed in all studies yet, where it was, it was regarded as imperative in child and family “coping with DMD” [Citation39,p.1228]. “…Where there does not exist open communication between the partners about the emotional aspects of the illness” [Citation45,p.12] there can be misunderstanding, which impacts parents’ ability to cope with the caregiving role. Communication about the condition with the individual with DMD was deemed “the most important thing” [Citation41,p.538] and communication with siblings was important but on occasions overlooked or avoided “I don’t think we’ve ever really talked about what it’s like for them to be the siblings of a DMD child” [Citation44,p.7]. It was noted that the distress caused by diagnosis can lead families to talk to each other more often [Citation26]. Families seemed to have “rules” [Citation39,p.1230] regarding DMD communication, resulting in either honesty or the withholding of condition related information [Citation27,Citation29,Citation31,Citation39,Citation41,Citation44].
Interestingly, it was noted that DMD “was the only condition where affected children were usually given less information than their siblings” [Citation39,p.1228]. One parent reported that they “Never wish to talk about the progression of illness with child” with DMD [Citation40,p.148]. Often, with both siblings and individuals with DMD, parents indicated that decisions to disclose disease related information were influenced by the age or perceived maturity of the children [Citation29,Citation39,Citation41,Citation44,Citation50]. It was suggested that genetics was a topic that parents were more likely to discuss with siblings than individuals with DMD [Citation31,Citation44]. Yet, genetics seemed to be a particularly difficult topic to discuss and this may partially be attributed to feelings of guilt as DMD carrier [Citation39,Citation47].
Network of support
Parents performing a caregiving role for an individual with DMD described that engaging a large support network was a way of protecting their well-being [Citation29,Citation30,Citation32–34,Citation36,Citation39,Citation41–45,Citation48–51]. Parents spoke of the benefits of support groups for DMD, feeling connected with the DMD world via social media and developing connections with other parents: “A group on Facebook is valuable for us. It’s a closed group for parents and children with DMD and it’s ingenious” [Citation41,p.538]. Although some parents were less comfortable with the aforementioned types of support: “One mother endorsed that initially it was overwhelming to see kids who were in wheelchairs” [Citation44,p.7]. Yet the main narratives involved finding such supports helpful for normalising parental experiences and for creating mutual support networks: “It does make you feel quite nice to think you’ve passed on some information and helped someone” [Citation32,p.488]. Additionally, groups provided parents with social opportunities for their children with DMD [Citation29,Citation34,Citation36,Citation41,Citation45,Citation50]. Informal support including “emotional support from family and friends” [Citation42,p.108] was highly valued.
Despite the focus on interpersonal support, financial support was also described within the narratives – given the need to pay for interventions, equipment, and external caregivers in some healthcare systems [Citation29,Citation33,Citation41,Citation43,Citation45,Citation49,Citation51]. One parent reported, “We have always tided over difficulties with monetary support from a colleague from a Christian group. I was frantic to raise my son, care for my son” [Citation51,p.749]. This was further supported by a study indicating that access to palliative care support was dependent upon the availability of sufficient funds [Citation40].
Navigating systems
Parents of those with DMD must navigate many systems, including the medical and education systems, in order to cater for the needs of the individual with DMD [Citation26–30,Citation33–36,Citation38,Citation39,Citation41–44,Citation46,Citation47,Citation49,Citation50]. Many parents commented on unhelpful experiences and interactions with professionals, often attributed to a lack of DMD knowledge: “The experience with the health care providers was just terrifying and horrible. We felt we knew more than the doctors” [Citation28,p.287]. Yet, positive experiences with professionals labelled “good chemistry” [Citation41,p.537] were also discussed, in particular those related to a team or multidisciplinary approach [Citation28,Citation30,Citation41,Citation42].
Many parents felt the need to engage in a process of self-education “by reading about DMD, while some studied the latest research and attended international conferences” [Citation41,p.537]. The acquisition of knowledge aided parents in “advocating” [Citation28,p.287] for individuals with DMD [Citation28,Citation29,Citation33,Citation36,Citation39,Citation41,Citation47,Citation50]. Such advocacy allowed parents to promote an awareness of their children’s needs beyond DMD – noting that professionals at times would attribute all the individual’s difficulties to the DMD. For example “parents reported having to fight for assessment and diagnosis even though their sons presented with literacy difficulties” [Citation33,p.279]. Parents were pleased by the introduction of legislation and guidelines to support individuals with DMD in navigating systems [Citation33], yet concurrently, were not convinced that professionals were always implementing such guidance – reporting “few examples of structured transition planning as required by legislation” [Citation27,p.1196].
Transition experiences
Transition experiences demonstrates how parents draw upon the skills learned in earlier years and navigate systems to support the transition of the individual with DMD to adulthood [Citation27,Citation29,Citation33,Citation36,Citation40,Citation41,Citation49–51]. Yet, parents still find transitions a challenge, “Transitions are a most difficult process– each stage we breakdown” [Citation40,p.148].
Parents described an active role in supporting decisions around further education training and employment. For example, “focusing now on things that he is good at …” [Citation29,p.136] was described as promoting a positive outlook for the parent and individual. Yet, some parents described a less active role and do “not see a good enough reason to put pressure on their sons to work harder, stay at college or think about work” [Citation27,p.1198]. The young people were also transitioning to adult services and the “timing” [Citation36,p.76] was viewed as optimal for some parents – believing “it was high time to leave that scene[pediatrics] behind ’’ [Citation36,p.76]; whereas some parents had concerns about changing services, given the deteriorating health of the individual [Citation36,Citation41].
With their increasing maturity, parents recognised the importance of the individual with DMD taking the lead role in organising their lives to meet their own needs [Citation33,Citation42,Citation51]. One parent encouraged her son to “Arrange your helpers by yourself if necessary. Think by yourself and you can handle it” [Citation50,p.91]. Throughout their lives parents are involved in future planning for the individual with DMD and this becomes increasingly important as parents age [Citation27,Citation29,Citation49]. At this point, parents may have to consider increasing assistance from external caregivers [Citation36,Citation41,Citation45], with the recognition that “providing full care should be slowly transferred” [Citation50,p.89]. Another form of future planning is the consideration of palliative care [Citation40].
Analytical themes
Four analytical themes, represented on the outside of , were derived from the descriptive themes and capture parental experiences across the stages of disease progression. Theme one, “The Cyclical Nature of Grief” commences at diagnosis and becomes salient at illness deterioration points, remaining a part of parents’ experience after their child has died. Theme two “Lifelong Expert in the Needs and Experiences of an Individual with DMD” commences following diagnosis and continues throughout the individual’s life. Theme three, “Navigating Deviation from the Typical Life Course” becomes more apparent with increasing age and disease progression. Theme 4, “Uncertainty as Ever Present,” involves reflections on the challenges of planning for an uncertain future given the dialectic between terminal nature of the condition and the ever-increasing life expectancies for people with DMD.
The cyclical nature of grief
Grief was apparent as an inseparable aspect of parenting an individual with DMD. Across studies parents reported shock at diagnosis [Citation26,Citation32,Citation37,Citation39,Citation41,Citation42,Citation47,Citation48] and within this state of grief, denial and anger were apparent “I was angry. I passed through denial but got stuck in anger for a long time” [Citation47,p.390]. Guilt was also expressed due to the genetic nature of the condition [Citation39,Citation47]. Some parents hoped for “an external miracle, or cure” [Citation42,p.108], and the realisation that the condition was not going away had a detrimental impact on the mood of some parents, illustrated by the notion that “everything went dark” [Citation41,p.536]. Yet, with “acceptance,” p.487 of the condition, an understanding of DMD may become “incorporated into daily life” [Citation42,p.109] and grief may decline.
Grief reached heightened states at disease progression points. For example it was outlined that when mobility aides were introduced it was “a signal for illness deterioration and a re-awakening of the feelings experienced at diagnosis” [Citation30,p.186]. Grief may rise prior to bereavement and thus can be linked to the individual’s increasing dependency with age and the idea that parents sometimes “wait for death” [Citation41,p.538]. The intensity of grief increases when the individual dies but the parent’s identity as a DMD caregiver remains, and therefore parents may seek support by continual involvement with other parents of individuals with DMD [Citation32].
Lifelong expert in the needs and experiences of an individual with DMD
Following diagnosis parents described commencing a journey where they become “specialists” [Citation51,p.749] not only in the caregiving role and the needs of the individual, but also experts in the individual’s experiences, as a result of the extremely close relationship the parent and child develop [Citation26,Citation28,Citation29,Citation35,Citation39,Citation41,Citation42,Citation45–48,Citation50]. “In providing constant care, a special bond is created between mother and child, and the mother becomes acutely aware of her child’s suffering and limitations” [Citation45,p.9]. This quotation illustrates why it can be difficult for the parent to separate aspects of his or her individual identity from that of DMD caregiver. As the young person ages and isolation increases, parents increasingly see themselves as their child’s prime source of comfort: “You have to fulfil every moment of her day and make her a life because there’s nobody else there to make it for her …" [Citation45,p.10]. At the same time, parents reported “…social isolation generally related to avoiding certain social situations that were difficult because of their son’s DMD” [Citation48,p.7].
With increasing age and disease progression parents described becoming experts in the increasingly “complex” [Citation51,p.749] caregiving tasks “to prevent their son from contracting pneumonia, ileus, and/or bedsores” [Citation50,p.90]. The increasing demands make caregiving challenging. Yet, as the role of caregiver is integral to their identity, they described great difficulty trusting anyone else in managing the interventions and equipment [Citation50,Citation51]. Where external caregivers became necessary, parents continued to remain involved, often to ensure that caregivers were adequately trained and performing the role in a way that the expert deemed as optimal: “Teaching the aides all of these things is my duty. When we get an untrained recruit, I have to teach him everything” [Citation50,p.88].
Navigating deviation from typical life course
As the disease progresses, parents notice their own and their child’s life course deviate from what they may have expected [Citation26,Citation29,Citation34–37,Citation41,Citation42,Citation45,Citation47,Citation50,Citation51]. When the child is young, parents expect the child to be dependent. However, when dependence increases with age it can lead parents to feel a sense of frustration that their child’s life course differs from the norm: “It is unreal that for others life goes upwards and then it starts going the wrong way for my boy” [Citation41,p.537]. Some parents indicated that they would like their child to develop skills for independence but there is confusion regarding how to do this “you become more dependent but you’re an adult and you want to become more independent but how do you do that?’’ [Citation36,p.77]. On the other hand, some parents found that interventions prolonged independence, “…He can be left alone for you know hours and hours, I can go out for instance from say 9am until 5 pm and [son] will cope perfectly fine at home without me or anyone here …” [Citation48,p.9].
Yet, on occasions parents described resistance to their children engaging in the typical developmental tasks, such as college and independent living [Citation50], due to their own worries, encouraging what was described as “prolonged derivative dependency” [Citation51,p.746]. As the child becomes older “outside contacts become fewer” [Citation45,p.10], the young person is becoming increasingly isolated at what should be a highly social time in their life. Furthermore, “as the boys became older and the need for help increased, the offers of services, medical and other follow up became fewer and key professionals disappeared” [Citation41,p.538], which illustrates that some parents may feel more isolated later in their journey.
Parents also described noticing deviations from their own expected/typical life course, mourning for the loss of the independence that they hoped would come after raising a child to adulthood. This is illustrated by the following quotation “Regular, middle-aged parents may experience life independent of children… They may also think, “I can enjoy my senior life.” But…we, parents with disabled children, can’t think so” [Citation51,p.749].
Uncertainty as ever present
From the point of diagnosis, parents described awareness of the terminal nature of DMD and awareness regarding the uncertainty of when death will occur [Citation26–30,Citation32,Citation37,Citation39–42,Citation45,Citation48–50]. While, in the past, parents could have expected their child to live to their teens, in recent years – with improvements in treatment – life expectancy has continued to increase considerably. This has meant that “families have had to revise their expectations” [Citation27,p.1197]. Some parents adapted to this uncertainty by changing “aspirations” [Citation30,p.189] and “optimizing the time together; doing ‘normal’ family activities while the child is still capable” [Citation45,p.10]. Parents proactively engaged in planning and preparing for the future [Citation27,Citation29], with one parent noting that her son spoke “about what he’d be doing when he was 40 and I firmly believe that you need to encourage that. So, I follow his lead” [Citation27,p.1198]. “Hope” [Citation42,p.111], was deemed essential in coping, “That’s the hope that I can go and get for my own strength, but also maybe for J.’s future that will certainly end with death” [Citation42,p.111].
Despite the hope and resilience of the parents in the quotations outlined above, the precarious situation and death remained present and was in some cases avoided in communication [Citation29,Citation39] with families indicating “that they are selective in sharing information, most notably concerning mortality of DMD” [Citation44,p.6]. With increasing age and deteriorating health “parents live with a sense of impending crisis because their son cannot live without a mechanical ventilator and care” [Citation50,p.90]. Parents described struggling with the “considerable rupture in the expected course of life, which presupposes that the death of parents will precede that of children” [Citation37,p.3086]. Also, as parents experienced deteriorating health themselves there was worry regarding what would happen to their child if they, the parent, were to die [Citation51]. Simultaneously, parents also have to take a role in “preparing for death” [Citation45,p.10] for their child and this involves considerations such as palliative care [Citation40]. As caring has been such an integral part of their lives, their occupation and social life, uncertainty arises regarding how life will be without their child [Citation32,Citation37,Citation41]. On occasions great support was received from fellow parents after a bereavement and thus parents may find a new role in “wanting to help other parents during these emotional times” [Citation32,p.488].
Discussion
The seven descriptive themes common across the 26 studies included in this qualitative synthesis highlight the breadth of experiences and challenges implicit in parenting in this context, characterised by: “Diagnostic Experiences”, “Coping with the Caregiver Role”, “Illness Trajectory and Associated Interventions”, “Family Communication”, “Network of Support”, “Navigating Systems” and “Transition Experiences”. The four higher order analytical themes outline the complexity of parental emotional responses and how they interact with disease progression. A type of grief process often begins at diagnosis and re-emerges at key mobility and symptom transition points and beyond the life of the child (“The Cyclical Nature of Grief”). Over time parents become experts in needs of their child (“Lifelong Expert in the Needs and Experiences of an Individual with DMD”). This process also involves coping with the emotions concomitant to their emerging awareness of the deviations from their child’s and own expected life course (“Navigating Deviation from Typical Life Course”) and the uncertainty regarding their child’s lifespan (“Uncertainty as Ever Present”).
The descriptive themes and to some extent in the analytical themes map onto those proposed in the modified Supportive Care Needs Framework for parents of children with rare conditions [Citation15]. This suggests that such a framework is relevant to understanding the experiences of parents of children with DMD. Practical and emotional needs were apparent within “Coping with the Caregiver Role” and “Navigating Systems”. Informational needs were particularly evident in the latter where, when navigating educational and healthcare systems for their children, parents noticed that professionals often lacked knowledge regarding DMD. Some parents struggle in the caregiving role without social support as evidenced in “Network of Support” and “Lifelong Expert in the Needs and Experiences of an Individual with DMD”. As caregiving becomes an increasingly significant part of their identity, socialising can be impacted. Finally, the emotional and psychological needs were apparent throughout – particularly within the themes of “Diagnostic Experiences”, “Illness Trajectory and Associated Interventions”, “Family Communication” and “Transition Experiences”.
Additionally, and perhaps more specific to DMD, the present review identified that an ongoing grief response is often part of parents’ experience (“The Cyclical Nature of Grief”). However, grief does not appear to follow a ‘typical’ linear progression as described in staged models of grief [Citation55]. Instead, the fluctuating conceptualisation of grief within the Rollercoaster Model of the Bereaved Caregiver [Citation56] appears more appropriate. Parents of those with DMD often communicated that grief begins at diagnosis, then recurs at key time points throughout the disease course –particularly at transition points, and obviously beyond the death of their child. This may explain parents’ continued desire for support from other parents of individuals with DMD, even after bereavement [Citation27].
“Lifelong Expert in the Needs and Experiences of an Individual with DMD” demonstrates how over time, and with the involvement in increasingly complex and often life-preserving tasks, the caregiver role becomes more demanding and can become incorporated as an important part of the parent’s identity. “Navigating Deviation from Typical Life Course” illustrates the conflicts parents’ experience when comparing their child’s and their own position in life with their expectations or the functioning of peers. These disparities between expectation and experience become more pronounced with increasing age and illness deterioration. When parents rate the QoL of their child with DMD, they often rate it as poorer than the affected person themselves [Citation10,Citation57,Citation58]. The present study helps us understand this finding. Parents’ ratings may be influenced by an awareness of the obstacles their child faces in comparison to typically developing peers or perhaps by their own emotional experiences, especially grief and worries about the future [Citation58].
The final analytical theme “Uncertainty as Ever Present” demonstrates the challenges parents face when planning for the future with their child’s ever-changing needs. Therefore, quantitative findings regarding greater prevalence of depression and, particularly, anxiety, amongst parents of individuals with DMD are not surprising when considered alongside this theme [Citation13,Citation59]. The precarity of their child’s health and uncertain future means that uncertainty must be tolerated. This may be compounded by the responsibilities of the caregiver role. For example, where parents indicated difficulty sleeping due to fears that not monitoring their son’s ventilation equipment could result in death [Citation18]. On the other hand, there is variation between parents, with some coping well within this uncertain context, having developed a tolerance of uncertainty and resilience [Citation8].
Clinical implications
There are differences in QoL and well-being across parents of individuals with DMD. It seems that most find caregiving rewarding [Citation12] and many will retain good well-being and will not require or want additional support. However, others find the burden of care challenging, and a proportion struggle with low or anxious mood. In outlining the psychological complexity of the parenting role in DMD, the present review provides clues as to how or where support can be provided to parents of individuals with DMD.
“The Cyclical Nature of Grief” fits with the Rollercoaster Model of the Bereaved Caregiver [Citation56]. This should inform healthcare professional’s interactions with parents. It may be helpful to validate parents’ natural emotional responses – to notice that a range of responses to their son’s situation are expected and it’s normal for these to fluctuate. Additionally, this review highlights that grief continues after death and therefore allows the recommendation that parents should continue to access interventions following the death of their child. Engagement with Parent support groups seemed to be experienced as helpful for QoL. Thus, the provision of such groups would be beneficial throughout the parenting journey [Citation32].
Furthermore, given the psychological complexity of the experience of parenting in this context and the emotional impact, there is a potential role for common psychological interventions such as Cognitive Behavioural Therapy (CBT) [Citation60], Acceptance and Commitment Therapy (ACT) [Citation61,Citation62] or mindfulness-based approaches, amongst others. CBT and ACT have been shown to be effective in helping parents of children with chronic conditions [Citation61]. However, specifically in supporting parents of individuals with DMD, we are aware of only one case study, where a CBT approach was shown to be helpful in reducing anxiety and depression in a parent caregiver [Citation63]. Irrespective of psychological or other intervention approaches the present systematic review suggests a few key areas where therapists and healthcare professionals should focus their energies. For example, the theme of “Uncertainty as Ever Present” shows how parents of individuals with DMD often experience anxiety in the face of uncertainty around disease progression [Citation64]. Techniques within CBT specifically target intolerance of uncertainty by helping individuals to challenge positive beliefs about worry, cognitive avoidance and negative problem orientation [Citation64]. Acceptance or mindfulness techniques may also help parents develop their ability to stay present even when they are experiencing understandable anxiety [Citation65]. Being present to and accepting of the discomfort that comes with conversations about disease progression or when making plans for death or dying, may, in instances, mean that individuals within a family unit can have more open and honest conversations that better prepare them for the future. Indeed, in one theme, open communication within the family was described as helpful for maintaining parental well-being. Thus, parents could be encouraged to explore whether honest discussions within the whole family unit, including siblings – for example, regarding the emotional impact of caregiving or concerns regarding genetics [Citation44]– might be effective for well-being.
Future multidisciplinary interventions for parental wellbeing should consider including the above adaptations. Future research is required to see if these adaptations to multidisciplinary interventions are acceptable to parents or if these lead to increased engagement or efficacy for improving parental well-being and reducing distress.
Limitations of literature base
Several of the included studies had methodological weaknesses. Epistemology refers to the theoretical stance adopted when undertaking qualitative research and it aligns with analytical technique [Citation66]. Yet half of the studies included in this review did not acknowledge epistemology nor indicate any theory guiding their qualitative approach. Additionally, three studies failed to indicate the qualitative analytic technique used.
Linked to epistemology is reflexivity, which refers to the researcher’s acknowledgement of the impact their role had on the research findings, which aids trustworthiness [Citation67]. Despite the integral nature of reflexivity in qualitative research [Citation67], CASP ratings showed that only 9 of the 26 studies gave adequate consideration to the researcher-participant relationship, with the majority of studies not acknowledging the relationship at all. The researchers who conducted many of the included studies did not explicitly outline how their own personal experiences, beliefs and prejudices may have impacted data interpretation. It is possible that such biases may have led to the current study over or underrepresenting certain parental experiences, thereby ultimately impacting the content of the resultant themes. Yet, we expect that the large number of studies included in the review (N = 26), alongside the consideration of reviewer reflexivity in our own analysis, offered some protection against the detrimental impact of this methodological weakness in the literature on the review findings.
Although, a significant number of fathers were included in these studies, as is common with much literature on parental experience, their voices are underrepresented. Similarly, the majority of included studies are from English-speaking or European countries, and none are from Africa. Thus the findings of the present review may not entirely generalise to parents in other cultures, or to countries where limited health or social care provision makes it challenging to access support networks. Therefore– future research into parents’ experiences in other countries is now needed.
There are some possible weaknesses in the methods of this review. While extraction, quality assessment and analysis involved several researchers, title and abstract screening were only conducted by one researcher – making it possible that eligible studies may have been missed. An iterative process informed the development of each resultant theme. However, undertaking independent coding in the earlier stages of the analysis would have led to greater certainty in the reliability of initial codes. The descriptive and analytic themes were delineated from detailed analysis of the data-set derived from the initial 22 studies. The four studies that emerged from the updated search [Citation26,Citation40,Citation46,Citation48] were integrated at a later stage and had less influence on theme construction.
Finally, the themes identified in this analysis represented the downstream impact of a child’s DMD symptoms on common parental experiences. Thus, the analysis was not designed to test whether the presence or severity of certain specific DMD symptoms leads to a different parental experience. It possible that common behavioural symptoms, such as those that come along with autism, intellectual disability [Citation68] could impact on parental experience in specific ways – for example, causing greater parental distress or requiring greater external support. Therefore, to enable better support to parents of children experiencing behavioural symptoms, future qualitative research should explore how parents cope with these specific symptoms.
Conclusion
This systematic review synthesised data from 26 studies with qualitative findings, collating and analysing the experiences of 362 parents of individuals with DMD. The lived experience of parenting an individual with DMD results in a journey beginning at diagnosis where parents experience an ongoing cycle of grief, whist at the same time becoming an expert in the caregiving role. Parents must navigate a deviation from the typical life course for themselves and their children, whilst continually adjusting to uncertainty regarding their child’s future. Support for parents might include provision of peer support groups, promoting present moment coping, increasing tolerance of uncertainty and support directed towards the non-linear process of grief.
Disclosure statement
The authors report no conflicts of interest specific to this work.
Additional information
Funding
References
- Andrews JG, Wahl RA. Duchenne and Becker muscular dystrophy in adolescents: current perspectives. Adolesc Health Med Ther. 2018;9:53–63.
- Ryder S, Leadley R, Armstrong N, et al. The burden, epidemiology, costs and treatment for Duchenne muscular dystrophy: an evidence review. Orphanet J Rare Dis. 2017;12(1):1–21.
- Uttley L, Carlton J, Woods HB, et al. A review of quality of life themes in Duchenne muscular dystrophy for patients and carers. Health Qual Life Outcomes. 2018;16(1):1–16.
- Otto C, Steffensen BF, Højberg A-L, et al. Predictors of health-related quality of life in boys with Duchenne muscular dystrophy from six European countries. J Neurol. 2017;264(4):709–723.
- Birnkrant DJ, Bushby K, Bann CM, et al. Diagnosis and management of Duchenne muscular dystrophy, part 3: primary care, emergency management, psychosocial care, and transitions of care across the lifespan. Lancet Neurol. 2018;17(5):445–455.
- Bushby K, Finkel R, Birnkrant DJ, et al. Diagnosis and management of Duchenne muscular dystrophy, part 2: implementation of multidisciplinary care. Lancet Neurol. 2010;9(2):177–189.
- Bushby K, Finkel R, Birnkrant DJ, et al. Diagnosis and management of Duchenne muscular dystrophy, part 1: diagnosis, and pharmacological and psychosocial management. Lancet Neurol. 2010;9(1):77–93.
- Glover S, Hendron J, Taylor B, et al. Understanding carer resilience in Duchenne muscular dystrophy: a systematic narrative review. Chronic Illn. 2020;16(2):87–103.
- Baiardini I, Minetti C, Bonifacino S, et al. Quality of life in Duchenne muscular dystrophy: the subjective impact on children and parents. J Child Neurol. 2011;26(6):707–713.
- Opstal SH, Jansen M, van Alfen N, et al. Health-related quality of life and its relation to disease severity in boys with Duchenne muscular dystrophy: satisfied boys, worrying parents-a case-control study. J Child Neurol. 2014;29(11):1486–1495.
- Graham CD, Rose MR. What explains high life satisfaction in men living with Duchenne muscular dystrophy? A preliminary study to inform psychological intervention. Muscle Nerve. 2017;56(1):163–166.
- Pangalila RF, van den Bos GA, Stam HJ, et al. Subjective caregiver burden of parents of adults with Duchenne muscular dystrophy. Disabil Rehabil. 2012;34(12):988–996.
- Landfeldt E, Edström J, Buccella F, et al. Duchenne muscular dystrophy and caregiver burden: a systematic review. Dev Med Child Neurol. 2018;60(10):987–996.
- Landfeldt E, Lindgren P, Bell CF, et al. Quantifying the burden of caregiving in Duchenne muscular dystrophy. J Neurol. 2016;263(5):906–915.
- Pelentsov LJ, Laws TA, Esterman AJ. The supportive care needs of parents caring for a child with a rare disease: a scoping review. Disabil Health J. 2015;8(4):475–491.
- Schreiber-Katz O, Klug C, Thiele S, et al. Comparative cost of illness analysis and assessment of health care burden of Duchenne and Becker muscular dystrophies in Germany. Orphanet J Rare Dis. 2014;9(1):1–13.
- Landfeldt E, Lindgren P, Bell CF, et al. The burden of Duchenne muscular dystrophy: an international, cross-sectional study. Neurology. 2014;83(6):529–536.
- Nozoe KT, Polesel DN, Moreira GA, et al. Sleep quality of mother-caregivers of Duchenne muscular dystrophy patients. Sleep Breath. 2016;20(1):129–134.
- Raina P, O’Donnell M, Schwellnus H, et al. Caregiving process and caregiver burden: conceptual models to guide research and practice. BMC Pediatr. 2004;4(1):1–13.
- de Moura M, Wutzki HC, Voos MC, et al. Is functional dependence of Duchenne muscular dystrophy patients determinant of the quality of life and burden of their caregivers? Arq Neuropsiquiatr. 2015;73:52–57.
- Liang R, Chan SHS, Ho FKW, et al. Health-related quality of life in Chinese boys with Duchenne muscular dystrophy and their families. J Child Health Care. 2019;23(3):495–506.
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and Meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–341.
- Tong A, Flemming K, McInnes E, et al. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol. 2012;12(1):181–188.
- Cooke A, Smith D, Booth A. Beyond PICO: the SPIDER tool for qualitative evidence synthesis. Qual Health Res. 2012;22(10):1435–1443.
- Programme CAS. CASP qualitative checklist. [online]. 2018. Available from: https://casp-uk.net/casp-tools-checklists/
- Obeidat HM, Al Hadid LA, Al-Sagarat AY, et al. Lived experience of Jordanian parents having a child with Duchenne muscular dystrophy. J Pediatr Nurs. 2021;57:5–10.
- Abbott D, Carpenter J. ‘Wasting precious time’: young men with Duchenne muscular dystrophy negotiate the transition to adulthood. Disabil Soci. 2014;29(8):1192–1205.
- Bendixen RM, Houtrow A. Parental reflections on the diagnostic process for Duchenne muscular dystrophy: a qualitative study. J Pediatr Health Care. 2017;31(3):285–292.
- Erby LH, Rushton C, Geller G. “My son is still walking”: stages of receptivity to discussions of advance care planning among parents of sons with Duchenne muscular dystrophy. Semin Pediatr Neurol. 2006;13(2):132–140.
- Garralda ME, Muntoni F, Cunniff A, et al. Knee-ankle-foot orthosis in children with duchenne muscular dystrophy: user views and adjustment. Eur J Paediatr Neurol. 2006;10(4):186–191.
- Hayes B, Hassed S, Chaloner JL, et al. Duchenne muscular dystrophy: a survey of perspectives on carrier testing and communication within the family. J Genet Couns. 2016;25(3):443–453.
- Hodges L, Dibb B. Social comparison within self-help groups: views of parents of children with Duchenne muscular dystrophy. J Health Psychol. 2010;15(4):483–492.
- Hoskin J. Aspiration, austerity and ableism: to what extent are the 2014 SEND reforms supporting young people with a life-limiting impairment and their families to get the lives they want? Br J Spec Educ. 2019;46(3):265–291.
- Houwen-van Opstal SLS, van den Elzen YMEM, Jansen M, et al. Facilitators and barriers to wearing hand orthoses by adults with duchenne muscular dystrophy: a mixed methods study design. J Neuromuscul Dis. 2020;7(4):467–475.
- Hunt A, Carter B, Abbott J, et al. Pain experience, expression and coping in boys and young men with Duchenne Muscular Dystrophy - a pilot study using mixed methods. Eur J Paediatr Neurol. 2016;20(4):630–638.
- Lindsay S, McAdam L, Mahendiran T. Enablers and barriers of men with Duchenne muscular dystrophy transitioning from an adult clinic within a pediatric hospital. Disabil Health J. 2017;10(1):73–79.
- Lucca SAd, Petean EBL. Fatherhood: experiences of fathers of boys diagnosed with Duchenne Muscular Dystrophy. Cien Saude Colet. 2016;21(10):3081–3089.
- Parsons EP, Clarke AJ, Bradley DM. Developmental progress in Duchenne muscular dystrophy: lessons for earlier detection. Eur J Paediatr Neurol. 2004;8(3):145–153.
- Plumridge G, Metcalfe A, Coad J, et al. Family communication about genetic risk information: particular issues for Duchenne muscular dystrophy. Am J Med Genet A. 2010;152A(5):1225–1232.
- Sadasivan A, Warrier MG, Polavarapu K, et al. Palliative care in Duchenne muscular dystrophy: a study on parents’ understanding. Indian J Palliat Care. 2021;27(1):146–151.
- Saetrang T, Bjørk IT, Capjon H, et al. Parent-child communication and timing of interventions are challenges in the Duchenne muscular dystrophy care. Acta Paediatr. 2019;108(3):535–540.
- Samson A, Tomiak E, Dimillo J, et al. The lived experience of hope among parents of a child with Duchenne muscular dystrophy: perceiving the human being beyond the illness. Chronic Illn. 2009;5(2):103–114.
- Segal R. Occupations and identity in the life of a primary caregiving father. J Occup Sci. 2005;12(2):82–90.
- Sulmonte LA, Bisordi K, Ulm E, et al. Open communication of Duchenne muscular dystrophy facilitates disclosure process by parents to unaffected siblings. J Genet Couns. 2021;30(1):246–256.
- Tomiak EM, Samson A, Miles SA, et al. Gender‐specific differences in the psychosocial adjustment of parents of a child with duchenne muscular dystrophy (DMD)‐Two points of view for a shared experience. Qual Res J. 2007;7(2):2–21.
- Walker M, Mistry B, Amin R, et al. A qualitative exploration of the priorities and experiences of children with Duchenne muscular dystrophy, their parents, and healthcare professionals around weight management. Disabil Rehabil. 2021;1–9.
- Webb C. Parents’ perspectives on coping with Duchenne muscular dystrophy. Child Care Health Dev. 2005;31(4):385–396.
- Williams K, Davidson I, Rance M, et al. A qualitative study on the impact of caring for an ambulatory individual with nonsense mutation Duchenne muscular dystrophy. J Patient Rep Outcomes. 2021;5(1):71.
- Wong SH, McClaren BJ, Archibald AD, et al. A mixed methods study of age at diagnosis and diagnostic odyssey for Duchenne muscular dystrophy. Eur J Hum Genet. 2015;23(10):1294–1300.
- Yamaguchi M, Suzuki M. Becoming a back-up carer: parenting sons with Duchenne muscular dystrophy transitioning into adulthood. Neuromuscul Disord. 2015;25(1):85–93.
- Yamaguchi M, Sonoda E, Suzuki M. The experience of parents of adult sons with Duchenne muscular dystrophy regarding their prolonged roles as primary caregivers: a serial qualitative study. Disabil Rehabil. 2019;41(7):746–752.
- Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008;8(1):45–10.
- Booth A, Noyes J, Flemming K, et al. Structured methodology review identified seven (RETREAT) criteria for selecting qualitative evidence synthesis approaches. J Clin Epidemiol. 2018;99:41–52.
- Castleberry A. NVivo 10 [software program]. Version 10. QSR International; 2012. AJPE. 2014;78(1):25.
- Stroebe M, Schut H, Boerner K. Cautioning health-care professionals: bereaved persons are misguided through the stages of grief. Omega (Westport). 2017;74(4):455–473.
- Moorhouse M, O’Connor M. The rollercoaster model of the bereaved caregiver. Progress in Palliative Care. 2021;29(6):320–326.
- Gocheva V, Schmidt S, Orsini A-L, et al. Association between health-related quality of life and motor function in ambulant and nonambulant Duchenne muscular dystrophy patients. J Child Neurol. 2019;34(14):873–885.
- Wei Y, Speechley KN, Zou G, et al. The relationship between quality of life and health-related quality of life in young males with Duchenne muscular dystrophy . Dev Med Child Neurol. 2017;59(11):1152–1157.
- Landfeldt E, Lindgren P, Bell CF, et al. Health-related quality of life in patients with Duchenne muscular dystrophy: a multinational, cross-sectional study . Dev Med Child Neurol. 2016;58(5):508–515.
- Beck AT. Cognitive therapy: past, present, and future. J Consult Clin Psychol. 1993;61(2):194–198.
- Graham CD, Gouick J, Krahé C, et al. A systematic review of the use of Acceptance and Commitment Therapy (ACT) in chronic disease and long-term conditions. Clin Psychol Rev. 2016;46:46–58.
- Hayes SC, Strosahl KD, Wilson KG. Acceptance and commitment therapy: the process and practice of mindful change. New York: Guilford Press; 2011.
- Birdsey N. CBT for anxiety related to parenting a child with a life-limiting neuromuscular condition: a single case study. Clin Case Stud. 2021;20(2):129–146.
- Dugas MJ, Freeston MH, Ladouceur R. Intolerance of uncertainty and problem orientation in worry. Cogn Ther Res. 1997;21(6):593–606.
- Hayes SC, Hofmann SG. Process-based CBT: the science and core clinical competencies of cognitive behavioral therapy. Oakland (CA): New Harbinger Publications; 2018.
- Carter SM, Little M. Justifying knowledge, justifying method, taking action: epistemologies, methodologies, and methods in qualitative research. Qual Health Res. 2007;17(10):1316–1328.
- Newton BJ, Rothlingova Z, Gutteridge R, et al. No room for reflexivity? Critical reflections following a systematic review of qualitative research. J Health Psychol. 2012;17(6):866–885.
- Darmahkasih AJ, Rybalsky I, Tian C, et al. Neurodevelopmental, behavioral, and emotional symptoms common in Duchenne muscular dystrophy. Muscle Nerve. 2020;61(4):466–474.