Abstract
Purpose
To assess the change in individual outcomes for people with disability and complex needs after moving into newly built, individualised apartments in the community.
Methods
People with disability (neurological disorder or cerebral palsy) and complex needs (n = 15, aged 18–65 years) completed quantitative self-report measures over two time-points (pre-move and 6–24 months post-move). Pre-move living arrangements included group homes, residential aged care, private rentals, and living with parents. Post-move living arrangements were individualised apartments built for people with disability. Health, wellbeing, community integration, and support needs were compared across pre- and post-move timepoints.
Results
Paired sample t-tests showed significant improvements consistent with large effects in wellbeing (p = 0.031, Eta2=0.29) and community integration (p = 0.008, Eta2=0.41), particularly home integration, and a trend towards improved health (p = 0.077, Eta2=0.21). A Wilcoxon signed rank test demonstrated a trend towards reduced support needs (z= −1.941, p = 0.052) consistent with a medium effect (r = 0.35) and an average decrease of 2.4 support hours per participant per day.
Conclusions
Well-located housing with appropriate design, technology and support provision makes a positive contribution to wellbeing, community integration, and health for people with complex disability.
People with disability who move into individualised apartments experience significant positive change in health, wellbeing, and participation.
Findings highlight the benefits of housing that foster independence and enable personal choice and control.
Evidence suggests that investment in appropriately designed and well-located housing has positive outcomes for people with disability.
Evidence collected within this outcome framework has the potential to ensure models of housing and support that are responsive to the diverse and changing needs of people with disability.
Implications for rehabilitation
Introduction
Adequate housing is universally viewed as one of the most basic human needs. Our home and living arrangements have a strong influence on our quality of life [Citation1–3]. Indeed, a considerable body of literature affirms the links between housing, health outcomes, and quality of life for people with disability [Citation4]. Despite demonstration of these links, a substantial number of people with significant disabilities and complex needs (e.g., intellectual disability, brain injury, spinal cord injury, multiple sclerosis, and cerebral palsy) are denied access to their own home and have limited choice in housing and living arrangements [Citation5,Citation6]. The World Health Organisation [Citation7] describes complex needs as resulting from functional impairment which has substantial impact on a person’s independence in one or more mobility, self-care, domestic life, or self-management activities.
Group homes are currently the predominant model of housing and support for adults with disability and complex needs [Citation8]. In this model of housing up to six people with disability are co-located in a single residence; they have little or no say in where they live, who they live with, and are often separated from the community, with few opportunities for community engagement and participation [Citation4,Citation6] Limited consideration is given to the social compatibility between residents; individuals with challenging behaviours are often placed in group homes with four or five other people [Citation9]. Although group homes aim to resemble suburban homes, the structure of residents' daily lives is largely determined by staff rosters, routines, and priorities. In the group home model, residents are commonly treated as service users or recipients of care [Citation4,Citation10], and therefore no inherent drivers exist to foster independence and reduce paid supports over time [Citation11].
Many people with disability currently living in group homes have similar profiles and capacity for independent living to people in less restricted living arrangements [Citation11]. However, many individuals are living in housing that was not designed to be adaptable for people with disability. In this situation, inadequate design and limitations concerning modifying the environment can prohibit effective home participation, diminish personal choice and control, and increase support needs to complete daily tasks [Citation12]
In recognition of the potential negative outcomes of group homes, there is currently a strong international focus on the provision of suitable housing for people with disability and maintaining people’s right to choose where and how they live [Citation4,Citation13]. Worldwide, housing for people with disability is moving away from group homes towards individualised models of housing. These individualised models prioritise individuals’ rights to exercise choice and control over decisions that affect their lives across multiple domains [Citation14]. They aim to allow choice over both smaller decisions about everyday living (e.g., sleep and wake times, meal content, etc.) as well as more complex decisions (e.g., where and with whom they live, type of support, who provides support) [Citation14]. The living arrangements are life stage appropriate and personalised based on individuals needs and preferences [Citation15], thus the way they are implemented can vary substantially from person to person [Citation16].
Despite the move towards individualised models of housing, there is a paucity of research that investigates the outcomes of this housing on the residents [Citation11]. However, the results of this small number of existing studies affirm that meeting an individual’s housing needs and preferences is foundational to positive outcomes in major life areas [Citation11]. Studies have found that individualised housing has range of favourable outcomes for people with disability including increased self-determination, autonomy, home and community participation and choice [Citation17–19]. People with disability who live in individualised housing can also experience improvements in functional skills, mood, and social relationships [Citation20–22]. Reduced challenging behaviour has also been associated with living in individualised housing [Citation20] Smart home and communications technology incorporated into contemporary housing alone has enormous potential to increase independence and autonomy and reduce support costs [Citation23].
Many countries around the world have signed and ratified the United Nations Convention on the Rights of Persons with Disabilities (UNCRPD). Reflecting the principles of the UNCRPD, many governments have introduced individualised funding programs that aim to provide increased choice and control in the lives of people with disability [Citation24]. There has been a rise of specific funding allocated to specialist disability housing which endeavours to provide suitable, affordable housing for people with disability [Citation25]. As a result, an increasing number of people with disability are choosing to move into the individualised housing options now becoming available to them [Citation6]. Given these policy developments and shift in the disability sector towards more individualised housing models, it is critical to understand the outcomes associated with individualised housing. Existing literature investigating the outcomes associated with individualised housing is dominated by studies pertaining to intellectual disability, with substantially less research focusing on individuals with acquired complex disability such as brain injury, spinal injury, multiple sclerosis, or cerebral palsy [Citation4]. Therefore, the aim of the current study was to investigate the change in outcomes for people with disability and complex needs who move into individualised housing with appropriate design, support, technology, and location. Specifically, it was expected that participants would experience improvements in individual outcomes (health, wellbeing, community participation, and support needs) after moving into an individualised housing option, when compared to their prior living arrangement.
Methods
Design
This study is part of a larger mixed-methods research project designed to systematically evaluate individual experiences and outcomes of moving to and living in newly built, individualised models of housing for people with a disability over a 3-year period. The larger study has been designed to enable definitive statistical testing and constructivist qualitative evaluation of outcomes for participants as a group and within specific subgroups. Subgroups will be defined by variables that capture important considerations for ongoing developments in the sector including individual, housing, and support factors. The overall evolution and contribution of factors that predict the outcomes of living in new Specialist Disability Accommodation (SDA) housing for people with disability will be evaluated using multilevel modelling with data collected across a three-year period. Potential predictors of outcome operate at three levels: the level of the person, the SDA housing option, and the paid support delivery level. Designated outcomes in the larger study include subjective lived experience, health, wellbeing, community participation, autonomy, care and needs level, and support hours with economic impact tracked longitudinally as a function of budgetary impacts, direct economic impacts, and economic value of welfare impacts. The proposed sample size of 250–300 participants will include people with physical, sensory, or cognitive disability such as intellectual disability and acquired neurological disorders (brain injury, spinal cord injury, and progressive disorders) with complex needs as defined by SDA policy.
The current study presents a subset of results on three primary self-report outcome measures collected at two time-points (time 1: pre-move and time 2: 6–24 months post-move). Data collection took place between June 2019 and July 2021. These standardised outcome measures assessed the three personal outcome domains of health, wellbeing, and community integration. In line with published evidence suggesting individualised housing can have favourable outcomes for people with disability, we hypothesised significant positive changes for the group from pre- to post-move on each of these measures. A fourth measure was used to explore change in the level of support required by each participant in daily life. Given little if any direct evidence about support needs across living environments has been published, we did not make a directional hypothesis in relation to this variable.
Setting
To investigate the effectiveness of individualised models of housing, participants moving into apartments funded through the National Disability Insurance Scheme (NDIS) in Australia were recruited to the study. The NDIS is an individualised funding arrangement for people with disability that was implemented in Australia in 2013. Currently, just over 500 000 people with disability are receiving funding from the NDIS [Citation26]. Based on a social insurance model, the NDIS provides funding to eligible people with a “permanent and significant” disability for a range of supports, including mobility equipment, home modifications, community participation activities, and daily support needs [Citation27]. The NDIS also provides housing payments for people with disability and complex care needs who require housing specifically designed to maximise independence or improve the efficiency of the delivery of person-to-person support. This housing payment, intended to meet capital costs, is called Specialist Disability Accommodation (SDA) funding. Only 6% (30 000) of NDIS participants with the highest support needs are eligible for SDA [Citation28]. Non-capital costs, such as day-to-day support and services are funded separately under the NDIS. SDA-funded housing enables individuals to transition from a range of living environments including group homes, residential aged care (RAC), and living with ageing parents to more contemporary models of housing designed for people with disability.
The implementation of SDA policy [Citation29] in Australia in 2016 has seen a significant increase in new apartments for people with disability. In June 2021, there were 1950 dwellings enrolled with the NDIA as new build SDA [Citation26]. Of these dwellings, 875 were apartments. A further 806 SDA apartments are under construction across Australia, delivering housing for a further 860 NDIS participants with the highest support needs. Most of these dwellings are single occupancy [Citation30]. These apartments are funded on the premise that well-located housing with appropriate design, technology, and support provision will allow for better quality of life, increased independence, and reduced lifetime care costs for people with disability and complex care needs.
Participants
Study selection criteria required participants to be over 18 years of age with a disability (acquired neurological disorder or cerebral palsy) and complex needs. Participants were not excluded due to the severity of disability or cognitive disability as a result of an acquired neurological disorder. All participants were required to be able to independently agree to participate and have adequate communication skills. Adequate communication skills included the use of different modalities or strategies of communication such as verbal or written communication, verbal prompts, repetition, and rephrasing of information or use of augmentative communication devices [Citation31]. Study selection criteria also stipulated that participants either: (1) were granted SDA funding and awaiting their move into SDA or (2) had recently moved into their new SDA funded apartment.
This study reports the outcomes of the first 15 participants (see ) from the larger research project. These participants had all moved into Metropolitan SDA funded apartments and completed data collection over the first two time points (time 1: pre-move and time 2: 6–24 months post-move). All participants were fluent in English and five participants were from culturally diverse backgrounds (Aboriginal or Torres Strait Islander = 2, South Asian = 2, Polynesian = 1). All participants in this study had high support needs and SDA in their NDIS plan. Only 6% of NDIS participants with the highest support needs are eligible for SDA. All participants relied on a form of disability pension as a source of income. Participants' pre-move living arrangements spanned a variety of environments, including group homes, residential aged care (RAC), vulnerable housing, private rentals, and living with parents. The present withdrawal rate for the overall project is 5%, and 18.5% of participants have been lost to follow up over the 3 year time period.
Table 1. Participant characteristics (n = 15).
All participants moved into one of a small number of SDA apartments (e.g., 6–12) peppered throughout a larger private residential development (e.g., more than 70 apartments) located near accessible public transport and other community amenities. The apartments incorporate best practice accessible design as they are tailored to the needs of people with disability by incorporating appropriate technology and design features. Technological features in these apartments include devices or systems that automate home-based activities and allow their users to complete tasks, control their environment, communicate with others, or monitor their safety. For example, doors, lights, and heating might be controlled by a user’s voice or a device [Citation23]. The design of the apartments incorporates accessible features such as wide door frames, no steps, hoists and bathrooms and kitchens that are designed to be used by people who are sitting or standing [Citation30]. The residential developments also include one additional apartment to be used as a base for 24-h onsite support staff. This arrangement enables people with high support needs to live in their own apartment, while also being co-located to facilitate access to on-site support. Participants represent a range of pre- and post-move support arrangements. For example, some participants had all of their disability support provided by the on-site shared support provider. Others utilised some on-site shared support and utilised another disability support provider for their 1:1 support or directly employed workers to provide 1:1 support.
Procedure
Institutional approval to conduct this study was obtained from the La Trobe University Human Ethics Committee prior to its commencement. Recruitment was supported through a partnership with housing and community service providers. Adults who had secured an individualised housing option were informed about the research project by a staff member from the service provider. If the potential participant expressed an interest in or willingness to participate in the study, and agreed to be contacted by the research team, the participant's preferred means of contact was passed on to the research team. After informed consent was obtained, an interview was arranged.
Data collection consisted of structured interviews with administration of several quantitative outcome measures (overall health, wellbeing, community integration, and level of support). Interviews were completed by skilled research assistants with extensive clinical experience working with people with complex needs and communication difficulties. Research assistants were independent of housing and service providers. If data collection was unable to be completed before the participant moved, outcome measures were completed retrospectively. Retrospective data collection was completed for six of the 15 participants. For these participants, data were quality checked by a researcher independent of the data collection. Transcripts were examined to ensure interviewers provided appropriate framing to participants regarding the context of their responses (i.e., please think back to before you moved home and answer the following questions as if you were still living at X). In this small data set, two people were not included because the data were deemed not to be retrospective. It was confirmed by the research assistant responsible for data collection that the included participants provided information that was aligned with their retrospective living situation.
Data collection was conducted either face-to-face in the participant’s home, or via video conferencing. Data collection was completed as part of a larger study (with measures additional to those reported here) and in total took approximately 1–1.5 h per participant. Participants were given the choice to complete the study over one or multiple sessions. For participants who were unable to complete the measures or who required assistance to participate in the interview, a close other was present to assist as required. One of the participants used a communication aid to complete the interview. All interviews were recorded using a digital recording device.
Outcome measures
Three primary outcome measures were used to assess the impact of change in living environment across a range of personal life domains. Overall health was measured using the visual analogue scale (EQ-VAS) component of the EuroQol-5-dimension descriptive system (EQ-5D) [Citation32–34]. The EQ-VAS is a brief and cognitively undemanding, self-reported rating of overall health. The EQ-VAS has been found to be an acceptable measure of generic health independent of the EQ-5D [Citation34].
Wellbeing was measured using the Warwick-Edinburgh Mental Well-Being Scale (WEMWBS) [Citation35,Citation36]. The WEMWBS is a 14-item scale which assesses key concepts of mental well-being such as positive affect, satisfaction with interpersonal relationships, and positive functioning. WEMWBS scores show a broadly normal distribution. Thus, it captures the full spectrum of positive mental health without floor or ceiling effects and is well suited to monitoring trends over time and evaluating the effects of interventions [Citation36].
The Community Integration Questionnaire – Revised (CIQ-R) [Citation37] was used to assess community integration. The CIQ-R has a total of 18 items across four subscales. The Home Integration Subscale measures active participation around the home; the Social Integration Subscale measures interpersonal relations and participation in activities outside the home; the Productivity Subscale measures employment, education, and volunteer activities; and the Electronic Social Networking Subscale measures participation in electronic social networking (ESN) activities.
The Care and Needs Scale (CANS) [Citation38] was used to explore the impact of change in living environment on participants’ support needs. The CANS is an eight-category scale that measures the type and extent of support needed in daily life [Citation38]. Scores represent one of eight levels of support, ranging from no support (i.e., level 0 – “Can live in the community, totally independently”) to mid-range (level 4 – “Can be left alone for part of the day and over-night”), through to very high support needs (level 7 – “Cannot be left alone”).
The primary outcome measures used in the evaluation have high reliability (internal consistency, test–retest, inter-rater coefficients >0.7), validity (construct, convergent, and/or predictive), established sensitivity to change in adults with disability and normative (population level) data. Australian population level data were available for the CIQ-R [Citation37] and the EQ-VAS [Citation39]. We used UK data for the WEMWBS [Citation35]. Although the EQ-VAS uses a single visual analogue scale rating, it has been found to be consistently responsive to change in longitudinal studies [Citation40–42] during follow-up periods and across pre- versus post-intervention comparisons.
Data analysis
The overall hypotheses guiding analysis of the data were that significant improvements would be demonstrated on post-move scores as compared with pre-move scores on measures of health, wellbeing, and community integration. Given these hypotheses were directional, in the context of a small sample, we specified incremental alpha designations with the two-tailed alpha level p < 0.10 as being indicative of a trend towards significance: ^p < 0.10 (trend towards significance); *p < 0.05 (significant); **p < 0.01 (significant). Inclusion of the p < 0.10 trend alpha level enabled us to use the two-tailed test to explore significant change (p < 0.05) in the positive direction with the same power (and an equal probability of a type I error) as a one-tailed test [Citation43]. Where a significant change or a trend towards a significant change was demonstrated, Eta2 was used to index the magnitude of the effect for each comparison. The guidelines proposed by Cohen [Citation44,p.284–287] for interpreting the value were applied: 0.01 small effect, 0.06 moderate effect, and 0.14 large effect. Paired sample t-tests were conducted to compare overall health, wellbeing, and community integration outcomes at pre-move and post-move. We also compared the observed change for each participant against the reliable change index for each measure to evaluate whether the magnitude of the change made by the individual represented reliable or clinically significant change (better or worse) not explained by measurement error.
With respect to the CIQ-R subscales (home integration – HI, social integration – SI, ESN, and productivity – Prod), we planned to conduct exploratory post hoc pre- versus post-move comparisons, if statistical significance was demonstrated on the total CIQ-R score. These post hoc comparisons were planned to provide preliminary insight into the pattern of change across these constructs and the contribution of each to post-move community integration change within this small sample of participants. We applied a Bonferroni adjustment for multiple comparisons (p = 0.05/4) yielding an alpha level of 0.0125 for these four post hoc comparisons. Given little if any direct investigation of support needs across living environments has been published, we did not make a directional hypothesis in relation to this variable. A Wilcoxon signed rank test, the non-parametric alternative to the paired t-test, was conducted to compare change in level of support from pre-move to post-move [Citation45,Citation46] and a two-tailed alpha level of 0.05 was applied. Finally, bivariate correlations (Pearson’s r) were used to explore the potential influence of time living in a new SDA apartment (weeks post move) on outcome (post move scores on measures of health, wellbeing and community integration). We hypothesised positive correlations with one-tailed significance set at an alpha level of 0.05.
Results
Pre- and post-move descriptive statistics, statistical comparison indices and effect size results on the three primary outcome measures are provided in . As can be seen in (panel A), change in overall health scores at post-move compared to pre-move demonstrated a trend towards improvement (p = 0.077) consistent with a large effect (Eta2=0.21). At post-move, health scores for nine of the 15 participants (60%) had moved in a positive direction and seven of these participants displayed reliable and clinically significant improvement (see ). Scores for two participants showed no change, four participants showed a reduction in scores at post-move and two of these participants demonstrated reliable and clinically significant deterioration. Wellbeing scores showed significant improvement at post-move compared to pre-move (p = 0.031), and this change was consistent with a large effect (Eta2=0.29) (see , panel B). As a group, pre-move wellbeing was 1.36 standard deviations below the population mean and improved to being within one standard deviation (–0.7 SD) of the population mean. The total wellbeing ratings of 10/15 participants had moved in a positive direction and three of these demonstrated reliable and clinically significant improvement. The scores from pre- to post-move did not show reliable change for the remaining five participants.
Figure 1. Mean health, wellbeing, and community integration scores (panels A–C, respectively) at pre- and post-move (bars represent standard deviation). Higher scores indicate more positive outcomes.
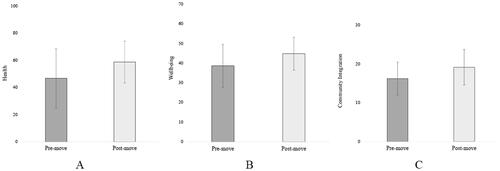
Table 2. Pre vs. post move comparisons: health, wellbeing, and community integration (paired sample t-tests; n = 15).
Table 3. Reliable change analysis for EQ-VAS, WEMWBS, and CIQ-R (n = 15).
Overall community integration total scores showed a large positive effect (Eta2=0.41) with the group mean showing a significant increase at post-move compared to pre-move (p = 0.008) (see , panel C). One subscale within the CIQ-R, HI, showed significant improvement at post move (p = 0.004), with a large effect (Eta2=0.41). Mean scores on the remaining three subscales increased but did not demonstrate statistically significant change. Overall, the pre-move group mean of the community integration total score was 1.28 standard deviations below the population mean and improved to being within 1 standard deviation (–0.7 SD) of the population mean. Total community integration scores had moved in a positive direction for 73% (11/15) of the participants and this improvement represented a reliable and clinically significant change for five participants and no participants showed reliable deterioration.
Across the three primary outcome measures, eight participants showed reliable improvement on at least one measure, two on two measures and three on all three measures. In addition, bivariate correlation analyses showed that scores on all three measures improved with increasing time post-move. These correlations were commensurate with small to medium effects but did not reach statistical significance (see ). While a trend towards reduced support needs was evident, this change in support level from pre- to post-move (Z= −1.941, p = 0.052) approached but did not each significance. It was however consistent with a medium effect (r = 0.35). At post-move, CANS support level remained the same for five participants indicating that support needs had not changed. For eight participants, the level decreased at post-move indicating reduced support needs and for the remaining two participants the level increased reflecting higher support needs. No participant had a change in support level that exceeded a single level change. These changes in support level reflect an overall reduction in daily support hours for the group of 15 participants. The average support hours per participant at pre-move was 19 h per day; the average support hours per participant at post-move was 16.6 h per day. This change represents an average decrease of 2.4 support hours per participant per day.
Table 4. Correlation of post-move outcome scores with time post-move (weeks) (n = 15).
Discussion
Affordable and accessible housing is foundational to social and economic participation and maximising the independence of people with disability. Traditionally, government funded housing for people with disability has tended to be separate from the community and congregated with other people with disability [Citation6]. Findings of this study support the premise [Citation4] that moving away from housing that is congregated and segregated to individualised housing and living arrangements can result in better outcomes for people with disability. In Australia, SDA policy and payments within the NDIS were designed to create a market of housing for people with disability that maximises the independence of tenants and improves the efficiency of support delivery. The current results provide preliminary evidence regarding the potential of contemporary housing in meeting the aims of SDA policy by improving the lives of tenants and maximising independence. Results also have international implications, as an increasing number of jurisdictions dedicate specific funds to specialist disability housing [Citation25].
Despite the small and heterogeneous sample in this preliminary study, statistically significant improvements consistent with large positive effects were demonstrated in the wellbeing, and community integration of tenants at post-move compared with pre-move. A positive trend commensurate with a large effect was also evident on health post-move. Scores on these three measures also improved with increasing time post move. Although these correlations did not reach statistical significance, it is encouraging to see that they corresponded with small to medium effects despite the small sample size. A trend towards a reduction in level of support needed by tenants’ post-move compared to pre-move was also shown. These results demonstrate the positive personal outcomes that can be experienced by people with disability when they have the opportunity to move into individualised housing that reflects their will and preferences. The findings also strengthen the contemporary evidence base underpinning the social importance of residential environments as significant determinants of health, wellbeing, and community integration [Citation1–3].
The magnitude of the change in overall subjective health ratings is a particularly promising finding that was not only evident at the group level but also at the individual level. Nine participants (60%) self-rated their health more positively at the post-move time point and for seven participants (47%) the change towards “the best health you can imagine” was consistent with reliable and clinically significant improvement. Improvements in subjective health suggest that overall lifetime care costs are likely to reduce for this group [Citation48,Citation49]. This finding alone has important implications for future health related cost utility analyses of the longitudinal impact of change in living environment for people with disability.
Positive change in subjective wellbeing, including psychological functioning, sense of self, and future focussed optimism, was a significant finding following the change of living environment for this group. Prior to the move, the mean wellbeing of the group was clearly outside the typical range for the general population. Post-move their level of wellbeing moved to a range typical of their non-disabled peers. Again, it is noteworthy that the total wellbeing ratings of two-thirds of the participants had moved in a positive direction with three participants showing reliable and clinically significant improvement and no participant showing negative change beyond that anticipated through measurement error. This finding echoes previous research that has found emotional functioning to improve for people with intellectual disability after moving into individualised housing [Citation20]. The change in wellbeing found in the current study is an early indicator that individualised housing, in particular SDA apartments, can enable people with severe disabilities to fulfil some of their aspirations to live an ordinary life and to feel more optimistic about their future.
Not only did health and wellbeing improve for this group of tenants, but they also had a greater level of community integration post-move compared to pre-move. This statistically significant change reflected a large positive effect for the group and positive change post-move for 11 (73%) of the 15 participants. Five participants demonstrated reliable and clinically significant improvement, and none showed reliable decline. The Home Integration Subscale of the CIQ-R showed participants were significantly more active in the operation of their home including activities such as meal preparation and grocery shopping. These changes in home-based activities reflect that after moving into their apartments, participants were more involved in everyday life compared to their pre-move living situation. This outcome was expected as participants had moved from environments that largely did not foster independence to a built environment designed to maximise independence. Indeed, previous research has found that residents with intellectual disability living semi-independently or independently, participate in significantly more domestic tasks, such as household cleaning, cooking, shopping, and related tasks, compared to those living in family and staffed homes [Citation50,Citation51]. These findings indicate that living in individualised housing allows people with disability to live more like their non-disabled peers in their homes.
The remaining three subscales of the CIQ-R did not show significant changes in a positive or negative direction. Two of these subscales primarily reflect participation in activities outside the home. Thus, this lack of significant change could be expected given the severity of disability in this cohort and the fact that most participants were still settling into their new apartment and neighbourhood. Further, it is important to note that post-move data collection took place during COVID-19 pandemic restrictions for 11 participants. Decline in productivity and little improvement in SI, both of which are measured by frequency of activities outside the home environment, may well be associated with these COVID-19 social restrictions. In this context, the increase in ESN activity consistent with a moderate effect may also reflect increased reliance on electronic devices by participants during this period. Moreover, the positive changes in health, wellbeing, and community integration, particularly HI outcomes for the group are substantial when considered alongside the negative impact the COVID-19 pandemic has been found to have on life domains of people with disability including fewer opportunities to participate in the community [Citation52] and negative impact on wellbeing [Citation50,Citation51].
Overall group data demonstrated a measurable reduction in the level of support needed post-move compared to pre-move. This reduction likely parallels the group’s increased participation in HI activities. Both these findings are unsurprising given that participants moved to a built environment that was designed to maximise independence, increase privacy and dignity, and reduce reliance on paid support. Support needs were reduced for the majority (53%) of participants. For the remaining participants, their needs either did not change (33%) or increased marginally (13%). Together these changes represent an average decrease of 2.4 support hours per participant per day. Longer term follow-up is required to understand how tenants’ support levels change beyond the period of adjustment to their new environment.
Finally, the preliminary findings of this study demonstrate that the outcome framework utilised in the current research project has the capacity to reliably monitor changes in function and support domains valued by people with disability and complex needs. The framework is well-suited to provide a rigorous evidence base to further tailor models of housing and support to ensure that they are responsive to the diverse and changing needs of people with disability. This study has allowed us to test, pilot and refine the outcome framework and thus establish its feasibility and acceptability in the context of the everyday lives of people with disability and complex needs.
Strengths and limitations
This preliminary evaluation of the individual outcomes of people with disability and complex needs after moving into newly built, individualised apartments in mainstream developments has both limitations and strengths. Clearly the sample size is small and brings with it associated limitations of compromised power and generalisability of the findings. While pre-move participants were living in diverse environments, we emphasise that the current results pertain to one type of individualised housing environment (apartments integrated into new mainstream housing with availability of on-site support) for participants who qualified for SDA funding within the rules of the Australian NDIS. In addition, we undertook the current preliminary analysis to explore outcomes for these participants and to establish the sensitivity and feasibility of our selected measures for indexing change in this population. Across our analyses, we report not only levels of statistical significance for pre- and post-move comparisons but also associated effect size. Group based data were also augmented by individual comparisons using reliable change indices that consider the potential impact of measurement error within our selected assessments. Taken together these methodological aspects of the study strengthen the interpretability of these preliminary findings. While the results reported here relate to quantitative measures, the larger outcome framework is multimethod and includes pre- and post-move semi-structured interviews. Transcripts are analysed using a constructivist grounded theory approach using open and focussed coding to identify emergent themes and relations between them [Citation53]. This qualitative analysis is currently underway, and we anticipate it will provide rich understanding of the process of moving to and living in individualised housing at the level of personal experience.
Implications and future research
Typically, traditional disability service systems have not afforded people the basic right to choose where they live or who they live with. The results of this study support the proposition that some people with disability who are given the opportunity to choose to live in individualised housing options have potential for more independent living, increased wellbeing and community participation. In the next phase of this research, we will scale up data collection and include contemporary housing options beyond SDA apartments. With a larger sample, we will have the capacity to predict the trajectory of individuals and subgroups of people with diverse disability types. Using data from this larger study, we will be able to compare subgroups and determine who is most likely to flourish in different models of housing and support or who might have different needs and require a more tailored response. As the number of participants is scaled up, this framework will provide an evidence base regarding the specific impact of the built form, technology and support provided and enable further investigation of cost effectiveness and cost utility metrics from both a services and social perspective. There will also be scope to identify opportunities to intervene and provide additional capacity building to improve the outcomes of tenants with specific needs. The outcomes framework will help maximise the benefits of contemporary models of housing by building a comprehensive evidence base that captures change over time and increases transparency and accountability within the sector.
Conclusions
The traditional disability service system in Australia has not afforded people the basic right to choose where they live or who they live with. Organisations throughout Australia, including the National Disability Insurance Agency (NDIA), are breaking down barriers and supporting people with disability to exercise their right to choose where and with whom they live [Citation54]. The ongoing development of individualised models will enable the Australian Government to work towards fulfilling the obligations it has signed up to in the Convention of the Rights of Persons with Disabilities regarding maintaining people’s rights to choose where they live [Citation6]. The findings of this study support the premise that well-located housing with appropriate design, technology, and support provision can make a significant contribution to improved health, wellbeing, increased independence, and reduced lifetime care costs for people with disability and complex care needs. While this study reports outcomes for only a small group of participants, it does provide preliminary evidence to support the intent of the SDA policy introduced in Australia in 2016 which was designed to secure investment in new disability housing to foster independence, enable effective delivery of support and reduce the long-term liability of government. In addition, it is worth noting that positive changes occurred for this group of participants when the majority (73%) were also negotiating the negative social and emotional consequences of COVID-19 and associated restrictions without increases in disability payments or specific disability services. More broadly, these findings offer preliminary support for the worldwide development and implementation of personalised budgets that includes funding allocated to specialist disability housing, as well as the investment in individualised models of housing for people with disability.
Acknowledgements
We would like to thank the many people who contributed to this research, including all the primary research participants and close others who generously provided their time to complete the study. We would like to thank Jacqui Naismith, Donna Wakim, Liz Williams, Elizabeth Beadle, Margaret Johnston, Anna Ewan, Sophie Moore, Megan Topping, and Ella-Rose Minter for their valuable contribution to the project.
Disclosure statement
The authors report no conflicts of interest.
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
References
- Veitch JA. Investigating and influencing how buildings affect health: interdisciplinary endeavours. Can Psychol. 2008;49(4):281–288.
- Kyle T, Dunn JR. Effects of housing circumstances on health, quality of life and healthcare use for people with severe mental illness: a review. Health Soc Care Community. 2008;16(1):1–15.
- Kavanagh AM, Aitken Z, Baker E, et al. Housing tenure and affordability and mental health following disability acquisition in adulthood. Soc Sci Med. 2016;151:225–232.
- Oliver S, Gosden-Kaye EZ, Winkler D, et al. The outcomes of individualized housing for people with disability and complex needs: a scoping review. Disabil Rehabil. 2020;1–15.
- Australian Institute of Health and Welfare. Current and future demand for specialist disability services. Canberra: AIHW; 2007.
- Wiesel I. Housing for people with intellectual disabilities and the National Disability Insurance Scheme reforms. Res Pract Intellect Dev Disabil. 2015;2(1):45–55.
- World Health Organization. World Health Organization International Classification of Functioning, Disability and Health. Geneva; 2001.
- Beadle-Brown J, Mansell J, Kozma A. Deinstitutionalization in intellectual disabilities. Curr Opin Psychiatry. 2007;20(5):437–442.
- Wiesel I. Allocating homes for people with intellectual disability: needs, mix and choice. Soc Pol Admin. 2011;45(3):280–298.
- Keogh F. Disability and mental health in Ireland: searching out good practice. Mullingar, Ireland: Genio; 2009.
- Independent Advisory Council to the NDIS. Pathway to contemporary options of housing and support. Canberra; 2018.
- Wiesel I. Living with disability in inaccessible housing: social, health and economic impacts. Melbourne: University of Melbourne; 2020.
- Habitat UN. The right to adequate housing fact sheet no. 21/Rev. 1. Geneva: UN; 2009.
- Bigby C, Douglas J. Supported decision making. Choice, preference, and disability. Cham: Springer International Publishing; 2020. p. 45–66.
- Connellan J. Commentary on housing for people with intellectual disabilities and the National Disability Insurance Scheme reforms (Wiesel, 2015). Res Pract Intellect Dev Disabil. 2015;2(1):56–59.
- Taleporos G, Craig D, Brown M, et al. Housing and support for younger people with disabilities transitioning to independent living: elements for success in the design and implementation of disability care Australia, a National Disability Insurance Scheme. Melbourne (VIC): Youth Disability Advocacy Service; 2013.
- Bigby C, Bould E, Beadle-Brown J. Comparing costs and outcomes of supported living with group homes in Australia. J Intellect Dev Disabil. 2018;43(3):295–307.
- Tichá R, Charlie Lakin K, Larson SA, et al. Correlates of everyday choice and support-related choice for 8,892 randomly sampled adults with intellectual and developmental disabilities in 19 states. Intellect Dev Disabil. 2012;50(6):486–504.
- Wehmeyer M, Bolding N. Enhanced self-determination of adults with intellectual disability as an outcome of moving to community-based work or living environments. J Intellect Disabil Res. 2001;45(Pt 5):371–383.
- Marlow E, Walker N. Does supported living work for people with severe intellectual disabilities? Adv Ment Health Intellect Disabil. 2015;9(6):338–351.
- McConkey R, Kelly F, Craig S, et al. Irish persons with intellectual disability moving from family care to residential accommodation in a period of austerity. J Appl Res Intellect Disabil. 2018;31(5):833–839.
- McConkey R, Bunting B, Keogh F, et al. The impact on social relationships of moving from congregated settings to personalized accommodation. J Intellect Disabil. 2019;23(2):149–159.
- Jamwal R, Callaway L, Ackerl J, et al. Electronic assistive technology used by people with acquired brain injury in shared supported accommodation: implications for occupational therapy. Br J Occup Ther. 2017;80(2):89–98.
- Lord JOHN, Hutchison P. Individualised support and funding: building blocks for capacity building and inclusion related papers. Disabil Soc. 2003;18(1):71–107.
- Tøssebro J. Scandinavian disability policy: from deinstitutionalisation to non-discrimination and beyond. Alter. 2016;10(2):111–123.
- National Disability Insurance Agency. NDIS quarterly report to disability ministers – Q4 2020–2021. Australia; 2021.
- Foster M, Henman P, Tilse C, et al. Reasonable and necessary’ care: the challenge of operationalising the NDIS policy principle in allocating disability care in Australia. Aust J Soc Issues. 2016;51(1):27–46.
- National Disability Insurance Agency. National Disability Insurance Scheme Act. Canberra; 2020.
- Robert S. National Disability Insurance Scheme (Specialist Disability Accommodation) Rules 2020. Australia: Government Australia; 2020.
- Aimers N, Wellecke C, Winkler D, et al. Specialist Disability Accommodation supply in Australia. Melbourne: Summer Foundation; 2021.
- Douglas JM. Conceptualizing self and maintaining social connection following severe traumatic brain injury. Brain Inj. 2013;27(1):60–74.
- Chen P, Lin K-C, Liing R-J, et al. Validity, responsiveness, and minimal clinically important difference of EQ-5D-5L in stroke patients undergoing rehabilitation. Qual Life Res. 2016;25(6):1585–1596.
- van Reenen M, Janssen B. EQ-5D-5L user guide: basic information on how to use the EQ-5D-5L instrument. Rotterdam: EuroQol Research Foundation; 2015.
- Feng Y, Parkin D, Devlin NJ. Assessing the performance of the EQ-VAS in the NHS PROMs programme. Qual Life Res. 2014;23(3):977–989.
- Tennant R, Hiller L, Fishwick R, et al. The Warwick-Edinburgh Mental Well-Being Scale (WEMWBS): development and UK validation. Health Qual Life Outcomes. 2007;5:63.
- Stewart-Brown S, Janmohamed K. Warwick-Edinburgh Mental Well-Being Scale (WEMWBS). User guide. Version 1. NHS Health Scotland, University of Warwick and University of Edinburgh; 2008.
- Callaway L, Winkler D, Tippett A, et al. The Community Integration Questionnaire – Revised: Australian normative data and measurement of electronic social networking. Aust Occup Ther J. 2016;63(3):143–153.
- Tate R. Manual for the Care and Needs Scale (CANS). Unpublished manuscript, Rehabilitation Studies Unit, University of Sydney Revised Version. Vol. 1; 2011.
- McCaffrey N, Kaambwa B, Currow DC, et al. Health-related quality of life measured using the EQ-5D–5L: South Australian population norms. Health Qual Life Outcomes. 2016;14(1):1–12.
- Hunger M, Sabariego C, Stollenwerk B, et al. Validity, reliability and responsiveness of the EQ-5D in German stroke patients undergoing rehabilitation. Qual Life Res. 2012;21(7):1205–1216.
- Kainz A, Meisinger C, Linseisen J, et al. Changes of health-related quality of life within the first year after stroke – results from a prospective stroke cohort study. Front Neurol. 2021;12:1746.
- Pickard SA, Johnson JA, Feeny DH. Responsiveness of generic health-related quality of life measures in stroke. Qual Life Res. 2005;14(1):207–219.
- Frost J. Hypothesis testing: an intuitive guide for making data driven decisions. State College (PA): Statistics by Jim Publishing; 2020.
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. New York (NY): Routledge; 1988.
- Siegel S. Nonparametric statistics for the behavioral sciences. New York: McGraw-Hill; 1956.
- Wilcoxon F. Individual comparisons by ranking methods. Biometrics. 1945;1(6):80–83.
- Chiu C, Wilcher K, Jones A. Perceived COVID-19 impacts on stress, resilience, and mental health among people with multiple sclerosis: a longitudinal prospective study. J Rehabil. 2021;87(1):80–87.
- Parkin D, Devlin N. Is there a case for using visual analogue scale valuations in cost–utility analysis? Health Econ. 2006;15(7):653–664.
- Maas AIR, Menon DK, Adelson PD, et al. Traumatic brain injury: integrated approaches to improve prevention, clinical care, and research. Lancet Neurol. 2017;16(12):987–1048.
- Felce D, Perry J, Kerr M. A comparison of activity levels among adults with intellectual disabilities living in family homes and out-of-family placements. J Appl Res Intellect Disabil. 2011;24(5):421–426.
- Gardner JF, Carran DT. Attainment of personal outcomes by people with developmental disabilities. Ment Retard. 2005;43(3):157–174.
- Lee B, Mangadu T, Tansey TN, et al. The intermediary role of loneliness in the relationship between COVID-19 stress and maladaptive coping among people with disabilities and chronic health conditions. J Rehabil. 2021;87(1):33–39.
- Charmaz K. Constructing grounded theory: a practical guide through qualitative analysis. London: Sage; 2006.
- NDIA. A home for living: Specialist Disability Accommodation Innovation Plan. Report no. DA0426; 2018.
