Abstract
Purpose
Children with cerebral palsy (CP) are at risk of cognitive impairments and need to be cognitively assessed to allow for individualized interventions, if applicable. Therefore, a systematic protocol for the follow-up of cognition in children with CP, CPCog, with assessments offered at five/six and 12/13 years of age, was developed. This report presents and discusses assessment practices in Sweden and Norway following the introduction of CPCog and a quality improvement project in Norway aimed at increasing the number of children offered cognitive assessments.
Materials and methods
A questionnaire investigating assessment practices was sent to pediatric habilitation centers in Sweden and Norway. In Norway, the habilitation centers also participated in a quality improvement project aimed at increasing adherence to the CPCog protocol.
Results
Of the respondents, 64–70% report that they assess cognition in children with all degrees of motor impairment, and 70–80% assess at the ages recommended in CPCog. Following the quality improvement project in Norway, the percentage of children assessed increased from 34 to 62%.
Conclusions
The findings illustrate that the provision of information is not sufficient to change practice. Implementation of new re/habilitation procedures is aided by targeting health care practices individually.
Children with cerebral palsy (CP) have increased risk of cognitive impairments that require intervention.
Assessments of cognition should be offered to all children with CP because the nature of cognitive impairments may vary.
Introducing a follow-up protocol of how and when to perform cognitive assessments is a step towards ensuring equal access to the services for all children with CP.
A quality improvement project might be a viable method for implementing a protocol into everyday clinical practice.
Implications for rehabilitation
Introduction
Cerebral palsy (CP) is a neurodevelopmental movement disability caused by a congenital or early acquired brain injury, which results in activity limitations [Citation1]. Although the CP diagnosis is based on motor impairments, difficulties with sensation, perception, communication and cognition are frequent and can vastly affect daily functioning [Citation2–5]. Epidemiological studies based on national CP registries indicate that 30–40% of children with CP have an intelligence quotient below 70, and impairments in visual-spatial cognition and executive functioning are frequent across CP subtypes [Citation2,Citation4,Citation6,Citation7]. However, although most children with CP have IQ scores in the normal range, cognitive functioning in children with CP varies considerably from profound intellectual disability to giftedness [Citation8].
The increased risk of cognitive impairments and the consequences these impairments might have on the academic functioning and socio-emotional well-being of children with CP prompted psychologists in the Scandinavian countries to develop a protocol for the follow-up of cognition, the CPCog [Citation9]. In the protocol it is recommended that, at a minimum, an assessment of cognition is offered all children with CP at five/six and 12/13 years of age. The assessment should include a test of intelligence, as well as assessments of visual-spatial perception and executive functioning. When intellectual disability is suspected, evaluation of adaptive functioning is recommended. To assess intelligence, it is recommended to use the Wechsler Preschool and Primary Scale of Intelligence (WPPSI) [Citation10, Citation11] at five/six years of age and the Wechsler Intelligence Scale for Children (WISC) [Citation12, Citation13] at 12/13 years of age. It should also be noted that the Wechsler tests are the only standardized measures of intelligence with local norms available in the Scandinavian countries. In addition, the Beery-Buktenica Developmental Test of Visual-Motor Integration (VMI) [Citation14] is recommended for assessing visual-motor integration. Furthermore, to assess executive and adaptive functioning, it is recommended to use the Behavior Rating Inventory of Executive Function (BRIEF) [Citation15, Citation16] and the Vineland Adaptive Behavior Scales [Citation17, Citation18] questionnaires, respectively. The recommended instruments are all frequently used in the Scandinavian countries [Citation9] and all reportedly have good psychometric properties in a Scandinavian context, i.e., showing good to excellent internal consistency and test-retest reliability [Citation19–22].
CP registries and the systematic follow-up of motor functions of individuals with CP are well established in Sweden and Norway. In 1994, the Swedish Cerebral Palsy Follow-Up Program (CPUP) was established in parts of the country. Later, in 2005, the CPUP became a national quality registry for CP, in which families in all of Sweden can participate. Data in the CPUP are collected at local habilitation centers, consisting of approximately 150 public and private centers across the 21 healthcare regions [Citation23]. Upon registration in the CPUP, parents/caregivers are informed that their child's data can be used for research purposes and that they may opt out at any time. All Swedish healthcare regions currently participate in CPUP [Citation24], and more than 95% of children with CP have joined the CPUP [Citation25].
In Norway, all children with CP have the right to be treated at one of the 21 nationwide habilitation centers. The systematic follow-up of motor function of children with CP started in 2006. With written caregiver consent, data are registered by the habilitation centers in the Norwegian Quality and Surveillance Registry for Cerebral Palsy (NorCP). The NorCP comprises over 93% of children with CP in Norway born from the year 2002 onwards [Citation26].
Prior to the introduction of the CPCog, there were no national recommendations for how and when to assess cognition, and not all registered cognition data were based on standardized and normed tests [Citation27]. In Sweden, the CPUP began registering cognition data in accordance with CPCog in 2015. According to the 2020 CPUP annual report [Citation25], there has been a year-by-year increase in the number of cognitive assessments. By the end of 2020, a total of 296 children in the targeted ages were assessed [Citation28]. In Norway, CPCog was introduced in 2013 [Citation29]. Prior to the CPCog, a study published in 2008 [27], based on data from 374 children with a diagnosis of CP born between 1996 and 1998, showed that 29% had undergone cognitive testing. Five years after the introduction of CPCog in 2018, 34% of 1,614 children with CP born between 2002 and 2013 were recorded with a CPCog protocol in NorCP [Citation30]. Moreover, the percentage of children assessed with a standardized test of intelligence at each habilitation center varied between 9% and 54% [Citation30].
The variability between centers and the slow rate of implementation of CPCog was somewhat surprising. In a survey of the 21 Norwegian pediatric habilitation centers in 2012 (prior to the development of the protocol), 15 of the 16 centers that responded expressed favorable attitudes towards having a systematic protocol for the follow-up of cognition [Citation9]. The slow implementation rate was a concern from a health service perspective, as it is the official policy in the Scandinavian countries that all citizens should have equal access to the same services [Citation31]. Furthermore, the slow implementation rate could not be ascribed to difficulties administering the recommended instruments as the recommended instruments are well-known among psychologists in Scandinavia. In addition, studies have shown that it is possible to assess 62% of children with CP using standardized tests [Citation32]. When the assessment is adapted to accommodate for speech and motor impairments by allowing other response modalities than pointing with a finger, as many as 80–90% can be assessed with those tasks from the CPCog-battery which have a multiple-choice format and require only pointing as response mode, e.g., Matrix Reasoning from the WISC and Visual perception from the VMI [Citation8]. For this reason, feedback from the pediatric habilitation centers was collected to better understand the centers' experiences with the implementation of CPCog, and to make an effort to increase the number of children being offered cognitive assessments in line with CPCog.
The aim of the current study is therefore as follows: 1) to explore facilitators and barriers to the implementation of CPCog in pediatric habilitation centers in both Sweden and Norway and 2) to investigate if it is possible to increase the number of children with CP assessed in line with CPCog via a clinical quality improvement project.
Method
To investigate the first aim of the study, a survey was sent to psychologists and managers who work at habilitation centers in Sweden and Norway. To investigate the second aim, a clinical quality improvement project was carried out in Norway in 2019–2020 [Citation33]. The methodology for the survey and the quality improvement project will be presented separately.
Implementation of CPCog in Sweden and Norway (aim 1)
Instrument
A questionnaire was developed to capture information about the CPCog implementation process. The Swedish and Norwegian questionnaires were similar but not identical, as they were adapted for each respective country. The respondents were asked about their awareness and use of the CPCog protocol, how many children with CP they typically assessed per year at their center, characteristics of the children who were offered assessments (e.g., age and gross motor function as classified by the Gross Motor Function Classification System [Citation34]), whether they had routines for disseminating the results following assessment to preschools/schools, and whether they offered any systematic interventions (e.g., support groups for children with CP, parental support groups or courses in augmentative and alternative communication (AAC)). Some open-ended items were also included.
Procedure
Participation in the project was based upon informed consent. In the information letter accompanying the questionnaires, the psychologists and habilitation managers were encouraged to answer the questionnaires independently of each other. We approached the following two groups as they have complementary perspectives offering important information: managers to get an overview regarding allocation of resources at their habilitation center, and psychologists to get an insight into details concerning cognitive assessments.
We aimed to include only pediatric habilitation centers that offer services to children with CP in Sweden and all pediatric habilitation centers in Norway. In Sweden, centers which only offered services to children with specific diagnoses that did not include CP, such as autism spectrum disorders, were excluded from this study. In Norway, all centers offer services to children with CP and therefore all centers were approached. An illustration of the inclusion process can be found in .
Figure 1. Inclusion of participants (psychologists and managers) from Swedish and Norwegian habilitation centers.
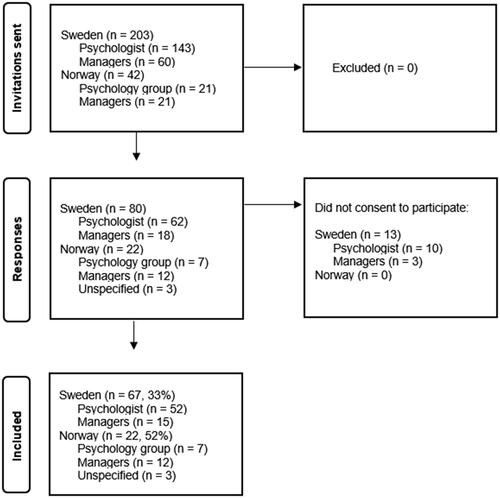
In Sweden, questionnaires were sent via email and administered through REDCap®, which is a secure web application for online surveys. Data collection occurred from December 2020 to February 2021, where 143 psychologists working in pediatric habilitation centers were invited to participate, of which 62 replied. Of these psychologists, 52 (36% response rate) agreed to participate. Sixty questionnaires were sent out to managers of pediatric habilitation centers, of which 18 replied. Of these, 15 agreed to participate (25% response rate). The psychologists at the habilitation centers were asked to fill out the questionnaire individually, meaning that some centers may be represented by multiple psychologists.
In Norway, the questionnaires were mailed to all 21 pediatric habilitation centers in April 2018. Each habilitation center received two questionnaires: one for the manager and one for the psychologists. The psychologists were asked to respond as a group (i.e., one response representing all psychologist in a habilitation center), in order to extract the full extent of practices at that specific center. The respondents were asked to indicate whether they were replying as a manager or a group of psychologists. A total of 42 questionnaires were sent and 22 replied (52% response rate), representing at least 12 of the 21 habilitation centers (some respondents chose to not indicate their habilitation center). Of those who chose to indicate their profession, 12 were managers and seven were psychologists.
The Norwegian national quality improvement project (aim 2)
Aims and methodology
The aim of the quality improvement project was to increase the number of children with CP being offered cognitive assessments in line with CPCog recommendations. The specific aims were 1) to have 65% of all children with CP registered in the NorCP cognitively assessed and the CPCog protocol recorded in the NorCP by the end of 2019, and 2) 85% by the end of 2020. The consent used for participation in NorCP also served as consent for the quality improvement project.
The invitation to participate in the quality improvement project was extended to all 21 pediatric habilitation centers, so that all children with CP could be reached. The services the children received differed marginally between centers, and the methodology needed to accommodate for this. The project therefore followed recommendations from the Breakthrough Series. The Breakthrough Series offers a model for how to cooperate on improvement of health services when it is known what needs to be changed and how these changes can be achieved [Citation35]. This model is particularly suitable for services that are offered at different geographical locations, but have similar responsibilities and mandate, and where there is variability in performance among health care sites. This was the case in Norway regarding assessment of cognition of children with CP. The Breakthrough Series model further describes how collaboration towards a common goal may include a variety of local adaptations and sub-goals. The methodology details six prerequisites for implementing such a project [Citation36], which were fulfilled when the project commenced (see ).
Table 1. Prerequisites for implementing a project according to the Breakthrough model of cooperation for improvement of health services and status in Norwegian national quality improvement project prior to launch of project.
Procedure and monitoring of progress
The project began February 1st, 2019 and ended December 31st, 2020. It consisted of three national meetings in 2019 and take-home assignments to be worked at by the local habilitation centers in between the meetings.
The national meetings included lectures and group discussions about the project progression. Lecture topics included the development and rationale of the CPCog, information about the NorCP and the methodology outlined in the Breakthrough series model. The lecture topics also included areas of specific relevance for psychologists working with children with CP, such as cognitive functioning, mental health issues, assessment instruments, family support, and materials for preschools/schools about CP from the Norwegian CP Association.
In line with the Breakthrough methodology, each pediatric habilitation center worked on the project locally. This ensured that the measures taken to reach the overarching national goal – which was to increase the number of children with CP assessed with tests of cognition – were appropriate for and adapted to local conditions. The psychologists, in cooperation with the local multidisciplinary team, formulated targets and procedures most suitable to increase the number of children with CP offered assessments, developed plans to reach those targets and monitored progression. A one-page summary of the targets and procedures were submitted to the project leaders ahead of the national meetings. These summaries were used for sharing ideas and success stories between the habilitation centers.
The monitoring of results was conducted through a quality indicator, i.e., the percentage of children with CP assessed with a test of cognition, which NorCP reports to the Norwegian Advisory Unit for Medical Quality Registries [Citation37]. The quality indicator is publicly available (see https://www.skde.no/kvalitetsregistre/alle/sykehus?indicator = nerve), is regularly updated and shows percentage assessed at each habilitation center as well as nationally.
Analyses
Descriptive statistics were used to analyze the questionnaires in Sweden and Norway. In Sweden, the statistics feature in REDCap® was used. In Norway, all statistical analyses were performed using IBM SPSS version 25. The Norwegian Quality Improvement Project data, i.e., percentage of children with CP assessed, were obtained from NorCP in a non-identifiable aggregated format.
Ethics
In Sweden, ethical approval was granted by the Swedish Ethical Review Authority, Stockholm, Sweden (dnr. 2020-04930). In Norway, ethical approval for the study was granted by the data protection officer at Oslo University Hospital (#2017/13706) and the Regional Committee for Medical and Health Research Ethics (#2018/1870).
Results
The results from the survey and the quality improvement project are presented independently.
Implementation of CPCog in Sweden and Norway (aim 1)
The 52 Swedish psychologists who participated in the survey represented 18 of the 21 healthcare regions in Sweden. Fifty of the 52 psychologists (96%) stated that they assess cognition in children with CP. The majority of these assessments were in line with the age recommendations in CPCog (see ). The majority (43 of 52, 83%) stated that they had a routine for cognitively assessing children with CP, and 85% had heard of CPCog, but only 36% followed it. Reasons for not following CPCog included insufficient time and resources, lacking directives from the management, and insufficient knowledge of guidelines (see ). The vast majority (96%) reported providing guidance and recommendations following cognitive assessments, including group meetings of children and adolescents with CP, training regarding AAC, support groups for parents, and referrals to other healthcare providers.
Figure 2. Reasons listed by Swedish psychologists as why the CPCog was not followed (N = 24).
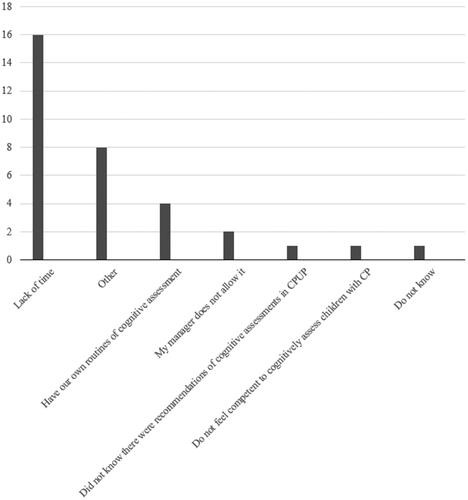
Table 2. Reported assessment practices and adherence to the CPCog protocol in pediatric habilitation centers in Sweden (N = 203 respondents; psychologists and managers) and Norway (N = 22 respondents; centers), number and percentage reported for each question.a
The 15 Swedish habilitation managers who completed the questionnaire represented 10 of the 21 healthcare regions. Of the managers, only 73% (11 of 15) reported that their centers offered cognitive assessment of children with CP. The main reasons for not offering assessments were lack of time and lack of psychologists to carry out the assessments. In contrast to the psychologists, the managers reported that the majority of assessments were offered at five/six years of age and less frequently at 12/13 years of age (see ). Similar to the psychologists, 87% had heard of CPCog and only 36% reported that they had started registering results in CPUP.
In Sweden, 65% reported that they assess less than ten children annually and only one respondent, a psychologist, reported assessing cognition in more than 15 children with CP annually (see and ). Adherence to CPCog was reported to be somewhat higher by those who reported assessing cognition in six to ten children with CP annually than in those who reported assessing five or less (52% versus 37%), but otherwise there are few differences that could be related to number of children assessed annually (see ).
Table 3. Number of children assessed annually with a cognitive test at a Swedish pediatric habilitation center, presented in relation to groups reported assessed (age and Gross Motor Function Classification System level), and the center’s knowledge of and adherence to the CPCog protocol, as reported by psychologist and managers.
In Norway, the survey was administered before the quality improvement project began. Of the respondents, including both psychologists and managers, 82% had heard about CPCog and 59% reported adherence to it (see ). There was consistency in responses across items, as those who reported following the CPCog protocol also reported that they assessed children at the recommended ages and sent assessment results to the NorCP. Of the 20 responses detailing assessment practices, 35% reported assessing less than 10, 35% between 10 and 15, and 30% assessed more than 15 children with CP annually (see and ). Assessment at the recommended ages in CPCog and reported adherence to the CPCog protocol was highest in centers assessing more than 10 children annually (see ). Reasons for not reporting data to NorCP were lack of time and not being aware that data should be registered.
Table 4. Number of children assessed annually with a cognitive test at a Norwegian pediatric habilitation centers (N = 20 centers), presented in relation to groups reported assessed (age and Gross Motor Function Classification System levels), and the centers’ knowledge about and adherence to the CPCog protocol.
In addition to reporting current assessment practices, the respondents were also encouraged to provide feedback as to how CPCog could be improved. Suggestions included more accessible research reports in Scandinavian languages on the benefits of cognitive assessments for children with CP, improved collaboration among psychologists concerning their experiences with CPCog, recommendations for assessments of nonverbal skills, and clearer guidelines concerning what information should be registered and when. The majority of comments were made by Swedish psychologists.
The Norwegian national quality improvement project (aim 2)
All 21 pediatric habilitation centers in Norway chose to participate in the project, comprising 62 professionals from all over the country. Representatives from all the centers were present at all three national gatherings, and all worked on implementing procedures locally to increase number of children being given cognitive assessments. Of the 21 participating centers, 15 sent their development plans with locally adapted targets and procedures to the project group.
Before the project commenced, 34% of the children registered in NorCP had been assessed. The overall percentage of children registered in NorCP who were assessed with a standardized test of cognition increased throughout 2019. By December 2020, 62% (948 of 1537) children born between the years 2002 and 2014 had been assessed [Citation26] (see ). The increase in mean percentage of children assessed in the years from CPCog was introduced (2013–2018) compared to after initiation of the quality improvement project in in 2019 was statistically significant, t(5) = −5.6, p = .00.
Figure 3. Percentage of children with cerebral palsy in the Norwegian Quality and Surveillance Registry for Cerebral Palsy recorded as having been cognitively assessed, as registered from 2013 to 2020.
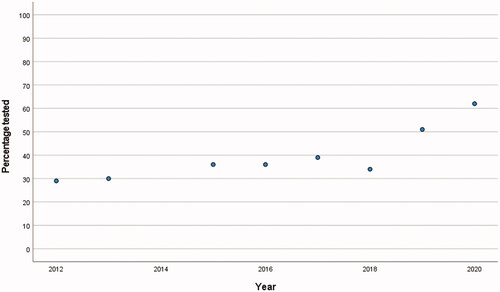
The aim to have 65% of children with CP cognitively assessed and reported to the NorCP by 2019 and 85% by 2020 nationally in Norway was not reached. However, the percentage of children born between the years 2010 and 2014 who were assessed, ranged from 66% to 84% as of December 31, 2020 (see ), indicating an increase in line with the project aim for the younger cohorts of children. Furthermore, all centers improved their practices in that the percentage of children assessed with a standardized test of intelligence increased from a range of 9 − 54% to a range of 25 − 84% by December 31, 2020 [Citation26].
Figure 4. Percentage of children with cerebral palsy in the Norwegian Quality and Surveillance Registry for Cerebral Palsy recorded with at least one cognitive assessment with a standardized measure per birth year as of December 31, 2020.
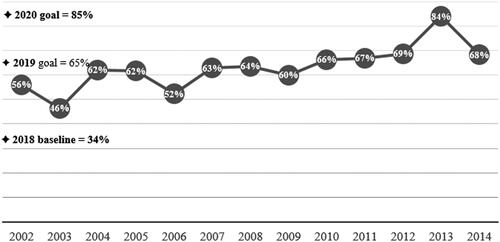
Although the overall percentage of children with CP cognitively assessed by each center continued to vary greatly, 11 of the 21 habilitation centers reached the 2019 goal with more than 65% assessed.
Discussion
The initiative to develop the CPCog protocol came from user organizations in Scandinavia [Citation9], underscoring the importance of offering cognitive assessments from a family perspective. As shown through the data of this questionnaire-based study, variabilities are significant in assessment practices for children with CP both in Sweden and Norway. Such variabilities are problematic, because they hinder equal access to services. In the Scandinavian countries, equal access to health services is an articulated political goal [Citation38]. Prior to the Norwegian quality improvement project, data registered in NorCP illustrated that access to cognitive assessments varied greatly throughout the country [Citation30]. The large variability among the centers in assessment practices, and the reported lack of time, was reflected in the number of children with CP being offered cognitive assessments at each respective habilitation center.
In both countries, a majority reported assessing fewer than 15 children annually. This number reflects that although CP is the leading cause of physical disability in children [Citation3], the demographics of Sweden and Norway contribute to few children per regional habilitation center. For example in Norway, a prevalence rate of 2 per 1,000 gives 150 children with CP per birth year, implying that, on average, 7 children should be served by each of the 21 habilitation centers. This low number of children means that many psychologists working at habilitation centers do not get the experience of performing repeated cognitive assessments with a variety of children with CP. This could impact the quality of assessments offered, perhaps in particular for those children considered most challenging to assess, namely children with the most severe speech and motor impairments [Citation39].
There is no national authority over the pediatric habilitation centers in either Sweden or Norway. The implementation of and adherence to CPCog rely on each habilitation center to recognize the advantages of such a protocol, as well as parents giving consent to assessments. It also requires knowledge that although CP is a motor disability, the underlying brain injury may also cause specific cognitive impairments, even if it does not cause intellectual disability. This group therefore needs to be prioritized for assessment by psychologists in order to enable appropriate interventions. Raising awareness of these factors, as was done through the Norwegian quality improvement project, has proven valuable in improving assessment practices in Norway.
Through the Norwegian quality improvement project, the percentage of children with CP registered in NorCP who had been tested increased significantly, from 34% prior to project start to 62% by the end of 2019. These figures include only children assessed with standardized tests, and not children with an evaluation of cognitive functioning based solely on clinical opinion. However, even with the improvement following the quality improvement project, there are still considerable differences between habilitation centers in Norway. Differences in the size of habilitation centers, numbers of patients with CP, and access to qualified personnel may explain some of the key differences in implementation of and adherence to CPCog. Since children with CP with the most severe speech and motor impairments are considered to be the most challenging to assess, it is possible that these groups sometimes miss out on assessments and important interventions as well as the assistance required [Citation2]. Previous studies have shown that cognitive skills can be masked by limitations of movement and motor control [Citation6]. Thus, underuse of assessments for subsets of children with CP, mainly those those at GMFCS levels IV–V and MACS levels IV–V, may also lead to false assumptions about cognitive abilities, less targeted therapeutic interventions and implementation of sub-optimal assistive technologies. It is therefore promising that a majority of respondents from both Sweden and Norway reported assessing children at all GMFCS levels. However, the CPCog protocol should be expanded to include a more precise description of how cognitive assessments for these children should be conducted, as it can help mitigate discrepancies in care.
The main goal of the Norwegian quality improvement project was to support a continued increase in the percentage of children being assessed from 65% by the end of 2019 to 85% by the end of 2020. Unfortunately, this goal was not fully met; by the end of 2020, 62% of children with CP had been assessed nationally. The main reasons the goals of 65% and 85% were not reached, were due to the lower percentages of cognitive assessments in the older cohorts born during the years 2002–2006 (for children born before 2006, only 57% were assessed by the end of 2020). These children were older than the recommended assessment ages in CPCog (assessments recommended at a minimum at five/six and 12/13 years of age), as they were aged 14–18 in 2020. Furthermore, as the Norwegian CP follow-up program was not national until 2006, many of the habilitation centers chose to include only children born 2006 onwards [Citation38].
Although 62% is somewhat lower than what was aimed for, taking into account that the Covid-19 pandemic reached Norway in March 2020, with somewhat restricted access to health care services, it is to be considered promising that the percentage did not decrease during the year 2020. This might be interpreted as a sign of consolidation of the CPCog protocol. It implies that children previously not assessed, such as those turning five/six years of age in the year 2020, were assessed during the year 2020, despite the pandemic.
Clinical implications
Cognition may affect the daily functioning of the child as well as the family dynamics to a larger extent than the actual motor impairments. However, given the high degree of variability in cognitive abilities in children with CP [Citation40–42], cognitive assessment is a necessary first step towards elucidating about the interventions that might be needed for the individual with CP. This is also reflected in the practices reported by the psychologists of both countries, as almost all reported that assessments were followed-up by guidance and suggestions for interventions.
Previous studies have indicated that certain cognitive impairments, such as visual-spatial difficulties, can become more apparent as children with CP grow older and demands of education and life in general increase [Citation43–45]. In addition, several studies have shown that cognition is an important predictor for participation in social and leisure activities for children with CP [Citation46–48]. Research has also established that children with CP are at higher risk of developing mental health issues [Citation49–51]. Early discovery of cognitive impairments in order to facilitate appropriate interventions and services is an important factor for increasing participation in social and leisure activities. Increased participation may also help prevent children with CP from developing secondary mental health issues, resulting in better developmental outcomes and higher quality of life. Thus, there is a need for multiple assessments over time. The responses from psychologists in both Sweden and Norway reflected the need for multiple assessments throughout a child’s development. As such, the tendency observed from the survey results, particularly in Sweden and to somewhat lesser degree in Norway, suggesting that assessments are prioritized at earlier ages (i.e., five/six years of age) over later ages (i.e., 12/13 years of age), is of some concern.
Variations in the proportion of children being offered cognitive assessment between the pediatric habilitation centers was noted in the present study. This implies that further work is needed in order to secure equality of services. Furthermore, when comparing results from Sweden and Norway it would seem that launching a protocol without accompanying measures taken to translate that into clinical practice, is not sufficient. Given the success of the Norwegian national quality improvement project, we recommend that a similar approach should be considered to increase the implementation of a cognitive assessment protocol in other countries.
Limitations
There are many similarities between the Swedish and Norwegian societies. Such similarities include the belief that all citizens should have equal access to healthcare. However, differences in how the services are organized mean that Sweden and Norway may not be directly comparable in terms of why CPCog has been implemented at such differing rates.
With regard to the questionnaires, it is a limitation that we had some missing responses to the Norwegian questionnaire. It is also a limitation that due to the organization of the services in Sweden, where there is – to the best of our knowledge – no national overview of habilitation centers serving children with CP, we were not able to estimate the percentage of habilitation centers in Sweden that participated in this study. Limitations which apply to all studies with a survey design, i.e., that respondents were mainly those who have a particular interest in the field, can also not be disregarded.
With regards to the data presented from Norway, one limitation is that NorCP may not have complete cognition data for all children with CP, as some pediatric habilitation centers in Norway may perform cognitive assessments for children with CP without reporting it to NorCP. It may also the case in Sweden. Furthermore, although parents/guardians of only 14 of approximately 3,000 eligible children for registration in NorCP (≈0.5%) declined being included in the registry, some may opt out from participating in CPCog despite agreeing to inclusion in NorCP. It is also possible that some might only agree to participation in CPCog at five/six years but not at 12/13 years since they are free to opt out at any time point.
For the data from Sweden, the issue of missing data is likely a larger limitation, as there is currently no available registry data on how many of the eligible children whose parents/guardians have been offered to participate in CPCog follow-up and have declined.
As the focus is on service delivery and implementing changes in health care provisions, we are not able to report data on the cognitive functioning of the children with CP assessed. However, in future publications this will be possible to do, and it will then also be possible to investigate whether there are specific subgroups of children with CP not assessed.
Conclusion
This study has shown that implementing a protocol for cognitive assessments in children with CP is not only feasible, but an important step towards ensuring equal access to services. The findings suggests that it is possible to increase adherence to a protocol through targeted projects, though such projects require time and resources.
Disclosure statement
No potential competing interest was reported by the author(s).
Additional information
Funding
References
- Rosenbaum P, Paneth N, Leviton A, et al. A report: the definition and classification of cerebral palsy april 2006. Dev Med Child Neurol Suppl. 2007;109(Suppl 109):8–14.
- Stadskleiv K. Cognitive functioning in children with cerebral palsy. Dev Med Child Neurol. 2020;62(3):283–289.
- Pakula AT, Braun KVN, Yeargin-Allsopp M. Cerebral palsy: classification and epidemiology. Phys Med Rehabil Clin N Am. 2009;20(3):425–452.
- Himmelmann K, Beckung E, Hagberg G, et al. Gross and fine motor function and accompanying impairments in cerebral palsy. Dev Med Child Neurol. 2006;48(6):417–423.
- Påhlman M, Gillberg C, Himmelmann K. One‐third of school‐aged children with cerebral palsy have neuropsychiatric impairments in a population‐based study. Acta Paediatr. 2019;108(11):2048–2055.
- Sigurdardottir S, Eiriksdottir A, Gunnarsdottir E, et al. Cognitive profile in young icelandic children with cerebral palsy. Dev Med Child Neurol. 2008;50(5):357–362.
- Hollung SJ, Vik T, Lydersen S, et al. Decreasing prevalence and severity of cerebral palsy in Norway among children born 1999 to 2010 concomitant with improvements in perinatal health. Eur J Paediatr Neurol. 2018;22(5):814–821.
- Stadskleiv K, Jahnsen R, Andersen GL, et al. Neuropsychological profiles of children with cerebral palsy. Dev Neurorehabil. 2018;21(2):108–120.
- Bøttcher L, Stadskleiv K, Berntsen T, et al. Systematic cognitive monitoring of children with cerebral palsy–the development of an assessment and follow-up protocol. Scand J Disab Res. 2016;18(4):304–315.
- Wechsler D. Wechsler preschool and primary scale of intelligence. 4th ed. Swedish version. Bromma: Pearson Assessment; 2014.
- Wechsler D. Wechsler preschool and primary scale of intelligence. 4th ed. Norwegian version. Bromma: Pearson Assessment; 2015.
- Wechsler D. Wechsler intelligence scale for children. 5th ed. Norwegian version. Bromma: Pearson Assessment; 2017.
- Wechsler D. Wechsler intelligence scale for children. 5th ed. Swedish version. Bromma: Pearson Assessment; 2016.
- Beery KE, Beery NA. The Beery-Buktenica developmental test of Visual-Motor integration. London: Pearson Assessment; 2010.
- Gioia GA, Isquith PK, Guy SC, et al. Behavior rating inventory of executive function. 2nd ed. Norwegian version Stockholm. Sweden: Hogrefe; 2018.
- Gioia GA, Isquith PK, Guy SC, et al. Behaviour rating inventory of executive function. 2nd ed. Swedish version. Stockholm, Sweden: Hogrefe; 2017.
- Sparrow SS, Cicchetti DV, Balla DA. Vindeland adaptive behavior scales. 2nd ed. Swedish version. Bromma, Sweden: Pearson Assessment; 2012.
- Sparrow SS, Cicchetti DV, Balla DA. Vineland adaptive behaviour scales. 2nd ed. Norwegian version. Bromma, Sweden: Pearson Assessment; 2012.
- Brøndbo PH, Egeland J. Måleegenskaper ved den norske versjonen av wechsler intelligence scale for children, fifth edition (WISC-V) [measurement characteristics of the norwegian version of wechsler intelligence scale for children, fifth edition (WISC-V)]. Psyk Test Barn. 2019;5:1–11.
- Heyerdahl S, Eikeseth S. Måleegenskaper ved den norske versjonen av vineland adaptive behavior scales [measurement characteristics of the norwegian version of vineland adaptive behavior scales]. Psyk Test Barn. 2014;2:1–11.
- Køhn K, Halvorsen M. Måleegenskaper ved den norske versjonen av behavior rating inventory of executive function (BRIEF), lærerversjon [measurement characteristics of the norwegian version of behavior rating inventory of executive function (BRIEF), teacher form]. Psyk Test Barn. 2020;5(1):1–11.
- Sørensen L, Hysing M. Måleegenskaper ved den norske versjonen av Behavior Rating Inventory of Executive Function (BRIEF), foreldreversjon [Measurement characteristics of the Norwegian verson of Behaviour Rating Inventory of Executive Function (BRIEF), parent form] 2014. p. 1–10.
- Visser L, Ruiter SA, van der Meulen BF, et al. Accommodating the Bayley-III for motor and/or visual impairment: a comparative pilot study. Pediatr Phys Ther. 2014;26(1):57–67.
- Alriksson-Schmidt A, Arner M, Westbom L, et al. A combined surveillance program and quality register improves management of childhood disability. Disabil Rehabil. 2017;39(8):830–836.
- CPUP Uppföljningsprogram för cerebral parese. Årsrapport 2020 [Annual report 2020]. 2020.
- Andersen GL, Hollung SJ, Klevberg GL, et al. Norsk kvalitets- og oppfølgingsregister for cerebral parese Årsrapport for 2020 med forbedringstiltak [Norwegian Quality and Surveillance Registry for Cerebral Palsy Annual Report for 2020 with improvement measures] 2021.
- Andersen GL, Irgens LM, Haagaas I, et al. Cerebral palsy in Norway: prevalence, subtypes and severity. Eur J Paediatr Neurol. 2008;12(1):4–13.
- Alriksson-Schmidt AI. CPCog update online webinar. The cerebral palsy follow-up programme (CPUP), Sweden and NorCP. Norway; 2021.
- Jahnsen R, Elkjaer S, Myklebust G. Cerebral Parese Oppfølgingsprogram. Årsrapport. Status 31.12.2013 [Cerebral Palsy Follow-up Program. Yearly report. Status December 31st, 2013]. Oslo University Hospital; 2014. https://oslo-universitetssykehus.no/avdelinger/Documents/CPOP%20arsrapport%202013.pdf
- Andersen GL, Hollung SJ, Vik T. Cerebral pareseregisteret i Norge: Årsrapport for 2018 med forbedringstiltak [The Norwegian Cerebral palsy registry: Annual report for 2018 with improvement measures] 2019.
- Alriksson-Schmidt AI, Jeglinsky I, Jonsdottir G, et al. Living life with cerebral palsy? A description of the social safety nets for individuals with cerebral palsy in the nordic countries. Scand J Public Health. 2021;49(6):653–665.
- Sherwell S, Reid SM, Reddihough DS, et al. Measuring intellectual ability in children with cerebral palsy: Can we do better? Res Dev Disabil. 2014;35(10):2558–2567.
- Stadskleiv K, Andersen GL, Hollung SJ. Kvalitetsforbedringsprosjekt: Økt andel barn med cerebral parese som tilbys kognitiv utredning [Quality improvement project: Increased number of children with cerebral palsy offered cognitive assessment]. Nasjonalt Servicemiljø for Medisinske Kvalitetsregistre 2020.
- Palisano R, Rosenbaum P, Walter S, et al. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol. 1997;39(4):214–223.
- Institute for Healthcare Improvement. The breakthrough series: IHI's collaborative model for achieving breaktrhough improvement. Boston (MA): Institute for Healthcare Improvement; 2003.
- Kilo CM. A framework for collaborative improvement: lessons from the institute for healthcare improvement's breakthrough series. Qual Manag Health Care. 1998;6(4):1–13.
- Peny-Dahlstrand M, Gosman-Hedström G, Krumlinde-Sundholm L. Are there cross-cultural differences of ADL ability in children measured with the assessment of motor and process skills (AMPS)? Scand J Occup Ther. 2012;19(1):26–32.
- Holm S, Liss P-E, Norheim OF. Access to health care in the scandinavian countries: ethical aspects. Health Care Anal. 1999;7(4):321–330.
- Kurmanaviciute R, Stadskleiv K. Assessment of verbal comprehension and non-verbal reasoning when standard response mode is challenging: a comparison of different response modes and an exploration of their clinical usefulness. Cogent Psychology. 2017;4(1):1275416.
- Geytenbeek JJM, Vermeulen RJ, Becher JG, et al. Comprehension of spoken language in non‐speaking children with severe cerebral palsy: an explorative study on associations with motor type and disabilities. Dev Med Child Neurol. 2015;57(3):294–300.
- Ballester-Plané J, Laporta-Hoyos O, Macaya A, et al. Cognitive functioning in dyskinetic cerebral palsy: Its relation to motor function, communication and epilepsy. Eur J Paediatr Neurol. 2018;22(1):102–112.
- Reid SM, Meehan EM, Arnup SJ, et al. Intellectual disability in cerebral palsy: a population-based retrospective study. Dev Med Child Neurol. 2018;60(7):687–694.
- Ego A, Lidzba K, Brovedani P, et al. Visual–perceptual impairment in children with cerebral palsy: a systematic review. Dev Med Child Neurol. 2015;57:46–51.
- Levine SC, Kraus R, Alexander E, et al. IQ decline following early unilateral brain injury: a longitudinal study. Brain Cogn. 2005;59(2):114–123.
- Pirila S, van der Meere J, Korhonen P, et al. A retrospective neurocognitive study in children with spastic diplegia. Dev Neuropsychol. 2004;26(3):679–690.
- Amini M, Saneii SH, Pashmdarfard M. Factors affecting social participation of iranian children with cerebral palsy. Occup Ther Health Care. 2018;32(3):290–305.
- Vila-Nova F, Oliveira R, Cordovil R. Participation in leisure activities by portuguese children with cerebral palsy. Percept Mot Skills. 2020;127(6):1051–1067.
- Bult MK, Verschuren O, Jongmans MJ, et al. What influences participation in leisure activities of children and youth with physical disabilities? A systematic review. Res Dev Disabil. 2011;32(5):1521–1529.
- Bjorgaas HM, Elgen IB, Hysing M. Trajectories of psychiatric disorders in a cohort of children with cerebral palsy across four years. Disabil Health J. 2021;14(1):100992.
- Bjorgaas HM, Hysing M, Elgen IB. Psychiatric disorders among children with cerebral palsy at school starting age. Res Dev Disabil. 2012;33(4):1287–1293.
- Downs J, Blackmore AM, Epstein A, Cerebral Palsy Mental Health Group, et al. The prevalence of mental health disorders and symptoms in children and adolescents with cerebral palsy: a systematic review and Meta-analysis. Dev Med Child Neurol. 2018;60(1):30–38.
