Abstract
Purpose
Somatosensory function of the lower limbs is rarely assessed in children with upper motor neuron lesions despite its potential relevance for motor function. We explored consensus regarding somatosensory categories (exteroception, proprioception, interoception, and body awareness), modalities, and outcome measures relevant to lower limb motor function.
Methods
Fifteen international experts with experience of somatosensory function assessment participated in this Delphi study. Surveys of four rounds, conducted online, included questions on the relevance of somatosensory categories and modalities for motor function and on the use of potential outcome measures in clinical practice.
Results
The experts reached consensus on the relevance of six modalities of the categories exteroception, proprioception, and body awareness. Based on their feedback, we formulated three core criteria for somatosensory outcome measures, namely suitability for clinical practice, child-friendliness, and relevance for motor function. None of the nine available outcome measures fulfilled each criterion. The experts also highlighted the importance of using and interpreting the tests in relation to the child’s activity and participation.
Conclusion
There was expert consensus on three categories and six modalities of somatosensory function relevant for lower limb motor function. However, existing outcome measures will need to be adapted for use in paediatric clinical practice.
Consensus was established for the categories and modalities of somatosensory function relevant for lower limb motor function of children with UMN lesion.
Outcome measures should cover tactile function, joint movement and joint position and dynamic position sense, and spatial and structural body representation.
None of the nine existing outcome measures fulfilled the core criteria: feasibility for clinical practice, child-friendliness, and relevance to motor function.
IMPLICATION FOR REHABILITATION
Introduction
The somatosensory system is a part of the sensory nervous system [Citation1,Citation2]. Stimuli are perceived via receptors of the skin, muscles, joints, or connective tissue and are transported via the neural pathways to the central nervous system for further processing [Citation3].
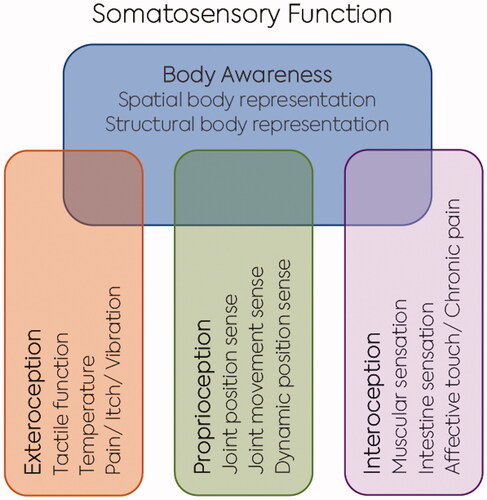
The somatosensory system can be divided in four categories: exteroception, proprioception, interoception, and body awareness (). Exteroception includes the perception of somatosensory stimuli arising from outside the body and includes the modalities touch, vibration, temperature, itch and acute pain. The categories proprioception and interoception include the perception of stimuli arising from inside the body. Proprioception covers the modalities joint position and joint movement sense and dynamic position sense. Interoception includes the modalities muscular sensation, affective touch, intestine sensation, itch, and chronic pain. A further category of somatosensory function is body awareness, which includes the modalities spatial body representation (body schema) and structural body representation (body image) [Citation1].
Figure 1. Categories and modalities of somatosensory function.
Legend: Four categories of somatosensory function (body awareness, proprioception, exteroception, and interoception), with their modalities. Body awareness is influenced by proprioception, extero-, and interoception.
Several studies have identified that somatosensory modalities like the threshold of light touch, vibration, joint movement and position sense, structural and spatial body representation are often impaired in children with an upper motor neuron (UMN) lesion [Citation4–12]. Indeed, diminished somatosensory function is included in the definition as a common impairment in children with cerebral palsy [Citation13]. Further, a lower level of somatosensory function has been shown to negatively affect motor learning and motor function in typically developing children and those with UMN lesions [Citation14,Citation15]. Nevertheless, in practice, therapists do not routinely assess somatosensory function of children with UMN lesions. It has been suggested that this is related to the lack of standardised and validated assessments in these children [Citation16,Citation17]. This also seems to be the case for adults with UMN lesions. Although studies in adults after stroke have demonstrated that body awareness training positively affects balance and activities of daily living [Citation18–21], body awareness assessment and training have not yet been incorporated into routine clinical practice [Citation22,Citation23].
As assessments are time-consuming and can be burdensome for children, knowing which modalities are most important for lower limb function and motor learning is essential. Another consideration is feasibility in clinical practice [Citation23]. Therefore, it is crucial to identify the tests that significantly impact motor learning and influence an individual child’s rehabilitation planning (tailored therapy). Clark et al. highlighted in their Delphi study on general tests used to assess paediatric lower limb neurological impairment that more therapy time should be spent on assessing tactile function [Citation24]. Additionally, they recommended that therapists should assess a range of somatosensory modalities and adapt the test procedures to the needs of the children [Citation24].
To date, most of the research on somatosensory outcome measures has focused on the upper limbs, particularly on stereognosis and tactile function relevant for fine motor skills of the hand [Citation11,Citation25–28]. However, other somatosensory modalities may also influence motor function of the lower limbs, like walking. For example, results of recent studies have suggested that reduced joint position and movement sense, as well as tactile function are associated with walking ability [Citation9,Citation29,Citation30]. These studies investigated tactile function with monofilament measurements, two-point discrimination, vibration, and joint position sense.
There is currently no agreement about the categories and modalities that should be covered when assessing impairments in somatosensory function relevant for lower limb motor function in children with UMN lesions. Consequently, consensus does not exist on which outcome measures should be used.
In this study, we used the Delphi approach to explore expert consensus on which categories, modalities, and assessments are considered relevant when assessing lower limb somatosensory function. The Delphi approach is a method of structuring group communication between experts in which individual participants provide feedback on a particular issue [Citation31]. It eliminates potential sources of conflict because participants are anonymous and it provides an opportunity to revise individual views in response to group trends. In short, the Delphi approach effectively seeks consensus on unanswered questions [Citation32]. For example, the Delphi approach has been used to identify relevant categories (i.e., based on the International Classification of Functioning, Disability and Health—Children and Adolescents Version) and core sets of exercise outcome measures for children with UMN lesions [Citation33,Citation34]. A core set can be applied to clinical practice as a toolbox of outcome measures [Citation35]. A toolbox contains outcome measures and allows clinicians to select the appropriate assessments to evaluate the aspects relevant for the clinical reasoning process of an individual child [Citation35].
Therefore, this project aims through the identification of expert consensus to (a) identify the categories and modalities of somatosensory function that should be considered for inclusion in an expanded toolbox of outcome measures that assess lower limb somatosensory function in children with UMN lesions, and (b) explore the recommendations of experts for the implementation of these outcome measures in clinical practice.
Method
Study design
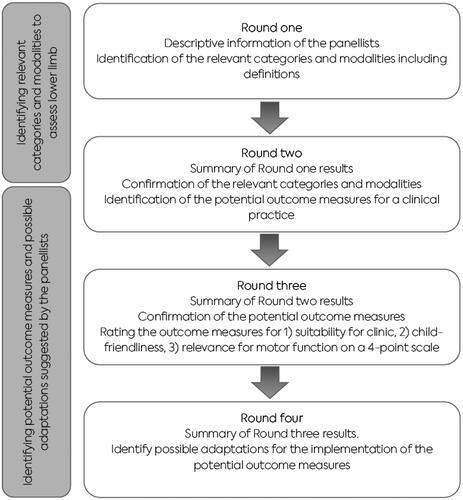
We applied a Delphi survey method with online surveys. We performed four survey rounds (). Each round was open for one month. One week before the deadline, participants received a reminder. Rounds one to three allowed panellists to explain their answers and recommend somatosensory function categories, modalities, or assessments not listed in the survey.
Figure 2. Process of the Delphi approach.
Legend: Four rounds of the Delphi process for identifying and reaching consensus on the relevant categories, and modalities of potential outcome measures to assess lower limb somatosensory function.
Participants
To be eligible to participate as a panel member, researchers were required to have published at least one paper related to somatosensory function assessments in the target population. During the recruitment process, authors and co-authors (researchers) of relevant publications were identified and contacted first. These researchers were then asked to recommend clinical experts experienced with somatosensory function assessments, and at least five years of clinical experience working with children with UMN lesions. The lead author (PM) contacted the possible panellists and clinical experts by e-mail and provided them with the study information pack. All experts, i.e., researchers and clinicians who agreed to participate, received a link to the Jisc online survey tool (https://www.onlinesurveys.ac.uk). According to the guidelines for Delphi studies, the aim was to include at least 15 researchers and clinical experts [Citation36].
Procedure and analysis
In the first survey round, we provided panellists with a list of four somatosensory categories and corresponding modalities: (a) exteroception, which includes the modalities tactile function, temperature, pain, itch, and vibration (b) proprioception, which includes the modalities joint position sense, joint movement sense, and dynamic position sense, (c) interoception, which includes the modalities muscular sensation, affective touch, intestine sensation, and chronic pain, and finally (d) body awareness, which includes the modalities spatial, and structural body representation. We provided definitions and description of the categories and modalities in the survey (Supplementary material S1). Panellists were asked to state whether or not they agreed that one should use at least one outcome measure of each category and modality in clinical practice to assess somatosensory function in children with UMN lesions, taking into account the relevance to lower limb motor function. Each question had three options; “I agree,” “I disagree,” “I am not sure,” and panellists were invited to explain their answer using a free text box if they wished to do so. The frequency of each answer option was calculated and this informed the level of agreement. We defined the following levels of agreement as consensus for the relevance of the somatosensory categories and modalities to lower limb motor function:
An agreement level of 75% was needed to definitely include a specific category or modality: [numbers of agree/(numbers of agree + numbers of disagree + numbers of unsure)] ≥ 0.75 [Citation37].
If the number of unsure responses differentiated between below or above 75% agreement, i.e., [numbers of agree/(numbers of agree + numbers of disagree + numbers of unsure)] < 0.75, but [numbers of agree/(numbers of agree + numbers of disagree)] ≥ 0.75, the question was reformulated and the option “I do not feel qualified” was added in the next round.
Categories and modalities with lower agreement were excluded; i.e., [numbers of agree/(numbers of agree + numbers of disagree)] < 0.75.
Finally, we asked panellists to suggest further categories or modalities relevant to assessing lower limb somatosensory function in the last question of the first survey round.
In the second survey round, we shared the results of the first round with the experts. In this round, we also included the response option “I do not feel qualified to answer this question.” This adjustment made it possible to distinguish between unclearly formulated questions and a lack of expertise of the panellist for a specific item. Finally, the second survey included a list of somatosensory function measures for each modality (). The list was based on a systematic literature review on the psychometric properties of lower somatosensory function assessments in children with UMN lesions [Citation38], and the additional outcome measures mentioned by the panellists in round two. The question in this survey round was: “Would you include the following outcome measure in assessing somatosensory function in children/youths with UMN lesions, as they are related to lower limb function?” Panellists could choose between “I agree,” “I disagree,” “I am not sure,” or “I do not feel qualified to answer this question” with the option to explain their answer. Again, the panellists were asked if they would add additional outcome measures to the presented list.
Table 1. Overview of outcome measures listed in the second Delphi round survey. The list is based on our previous systematic review [Citation38].
In the third survey round, we presented the results of the second survey to the panellists. In addition, two authors (PM, MvdL) independently identified themes with an affinity diagram from the free-text comments provided by the experts in the first two rounds, with the final themes agreed upon through discussion. These themes were presented to the panellists and also informed the formulation of the questions in this round. The free text comments also highlighted three criteria which are critical for the application of outcome measures in practice. These criteria were:
Clinical suitability (e.g., time required, costs, material, procedure, evaluation, and interpretation of test results).
Child-friendliness (e.g., suitability for children aged 5 to 18 years).
Relevance for daily-life lower limb motor function (e.g., standing, balance, and walking).
Ratings were made on a 4-point ordinal scale with the following options: “high,” “somewhat high,” “somewhat low,” and “low.” Respondents also had the option to choose “I do not feel qualified to answer this question.” We defined consensus slightly differently for the third round. Consensus was reached when 75% of the panellists or more selected “high” or “somewhat high.” In addition, the experts were asked if they had any direct experience with this outcome measure, either using the same or an alternative protocol. Finally, the details on the test procedures, the outcomes, necessary equipment, costs, and evidence on relationship with activity or motor function were presented to the panellists in the survey for each outcome measure with the information from the corresponding literature, see reference list in the Supplementary Material (S2).
In the fourth round, the panellists’ ratings for each of the three criteria for each outcome measure were presented. Finally, the experts were invited to add recommendations for implementing these measures in clinical practice.
Ethical considerations
This study received ethical approval from the research ethics committee of Queen Margaret University, Edinburgh (UK). All panellists ticked a box indicating their consent to participate in the study, and all answers were collected anonymously.
Results
Participants
Twenty-four authors of a peer-reviewed study on somatosensory function in children with UMN (“researchers”) were invited to participate in the expert panel. Nine agreed to participate, nine declined, and six did not respond. All nine researchers who agreed to participate recommended colleagues who were clinicians, researchers, or both. These persons were subsequently invited to participate.
Finally, 20 experts agreed to participate in the Delphi process. Seventeen completed the first survey, and 16 the second survey. One person asked to withdraw after the second round due to time constraints. The characteristics of the panellists are shown in .
Table 2. Characteristics of the panellists (n = 15).
Results of the survey rounds
In the first round, all experts agreed that there was no need to add any categories for assessing the somatosensory function of the lower limbs other than the four categories listed. There was consensus that at least one outcome measure representing the category exteroception (88% agreement) and one representing proprioception (94% agreement) should be included into the toolbox. For the category of body awareness, the agreement was 71%, thus, a consensus was not reached. For the category interoception, the agreement was low at 47%. The experts reached consensus on the following modalities: tactile function (94%), joint movement sense (94%), joint position sense (88%), dynamic position sense (75%), and spatial body representation (88%). Two panellists recommended including additional modalities; for body awareness, mental rotation of body parts, and for proprioception, the sense of force.
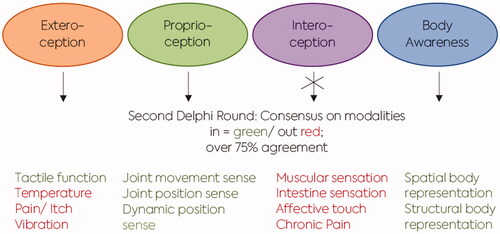
In the second round, the questions on including at least one outcome measure into the toolbox of the modality of body awareness and interoception were rephrased due to the high numbers of unsure answers in round 1. While agreement was reached to include outcome measures for the two modalities of body awareness, panellists did not agree on including modalities representing interoception.
In summary, the following modalities reached consensus for inclusion as a potential outcome measure in the toolbox; tactile function, joint movement and position sense, dynamic position sense, spatial and structural body representation (). Five themes emerged from the affinity diagram derived from the free-text comments. These were (a) the importance of the definitions of the relevant categories and modalities; (b) the need for instrumented tests of somatosensory function and that such tests must be suitable for application in the clinical practice; (c) the influence of the child’s cognitive level and age on the results; (d) the relevance to activity and participation of the outcome measures that should be applied in clinical practice; and (e) the importance of measuring somatosensory function of the trunk. Out of these five themes, three criteria were defined for the third survey. These were (1) the suitability for clinical practice, (2) child-friendliness, and (3) relevance for motor function. The definitions for each category and modality were shared with the panellists in the previous rounds. We further added the question whether the panellists would include an assessment of somatosensory function of the trunk.
Figure 3. Summary of the results from the first and second Delphi rounds.
Legend: Outcomes of the first and second rounds of identifying categories and modalities of somatosensory outcome measures of three categories and six modalities (green) reached consensus to be relevant for motor function. The modalities highlighted in red were excluded.
In the third round, the panel members rated the three criteria, i.e., the suitability for clinical practice, child-friendliness, and relevance for motor function of the outcome measures listed in the survey (see Supplementary material S2 for the details of the outcome measures). shows the number of experts who rated the criteria as high or somewhat high for each of these outcome measures. None of the outcome measures reached the consensus of 75% for all of the three criteria. Agreement was reached on (1) suitability for the use in clinical practice for registration of light touch and perception of movement direction (Fugl-Meyer Assessment), and localisation of tactile input on the lower limb; (2) suitability considering child-friendliness was only found for the registration of light touch (Fugl-Meyer Assessment); and finally, (3) relevance on motor function only for the dynamic joint position sense.
Table 3. Third round: Rating of currently available lower limb somatosensory outcome measures.
The experts were also asked whether they would recommend including somatosensory function outcome measure of the trunk into the toolbox. This question was added as a result of the free-text comments. Only four of the 15 panellists (27%) would include a somatosensory trunk outcome measure into the toolbox. Nevertheless, they all stated that the functioning of the trunk as a core part of the body is essential for movement and activity.
Experience with the outcome measures varied among panellists. Panellists reported experience with assessing tactile functions for the following modalities; registration of light touch (Fugl-Meyer Assessment, n = 5; monofilament test n = 3), and aesthesiometer (n = 7). Seven panellists reported to have experience in the application of the following proprioception measures: joint position and joint movement sense with motion sensors, joint movement sense (Fugl-Meyer Assessment), and dynamic joint position sense. Seven panellists had experience assessing body awareness with the outcome measure for localisation of tactile input on a body part illustration, and four had experiences assessing a tactile input directly on the lower limb.
In the fourth round, the panellists were invited to add any recommendations for implementation of these measures in clinical practice (see ). One recommendation was that the application and documentation of the outcome measures should be easily implemented and not time-consuming to perform (e.g., as an App). This was also important to improve the child-friendliness of the outcome measures, where additional requirements were that the measures should be easy to understand and fun for the child. The panellists also highlighted the need for validated outcome measures, and a standardised protocol with clear instructions. Concerning the relevance of the somatosensory function outcome measures for activity, the panellists considered that the tests should relate to the overall rehabilitation goal of the child and be incorporated within and used as part of the clinical reasoning process ().
Table 4. Expert’s recommendations for the implementation of the outcome measures in clinical practice.
Discussion
This Delphi study aimed to explore consensus on which lower limb somatosensory categories, modalities, and outcome measures are relevant for lower limb motor function in children with UMN lesions. In addition, we aimed to explore the recommendations of experts for implementing the available outcome measures in clinical practice. The experts reached consensus that outcome measures should cover the categories exteroception, proprioception, and body awareness. In addition, the experts agreed that the modalities of tactile function, joint position sense, joint movement sense, dynamic position sense, structural and spatial body representation should be assessed in children with UMN lesions.
Nine outcome measures for these six modalities were then scored for the three criteria of (1) suitability for use in clinical practice, (2) child-friendliness, and (3) relevance to motor function. While some assessments appear practical, appropriate for children, or relevant to activity and participation, none of the outcome measures achieved 75% or greater agreement (high or somewhat high) for all three criteria. For example, light-touch registration, assessed with the Fugl-Meyer Assessment, achieved high agreement for use in clinical practice and child-friendliness but low relevance for activity. In contrast, measuring dynamic joint position sense yielded high agreement for relevance to activity, but its use in clinical practice and child-friendliness was rated as low. These latter results were similar to the consensus on body awareness modalities. Outcome measures that are easy and quick to perform, and do not require specialised equipment, such as the Fugl-Meyer Assessments for assessing light touch and joint movement sense, are easily implementable in clinical practice. They can often be completed in a short time, and therefore the child-friendliness is likely high. Nevertheless, the low agreement for relevance for activity could be related to the low level of evidence regarding the relevance of these somatosensory functions for motor activities. These findings are well in line with those from Clark et al. [Citation24]. They reported various barriers for applying lower limb neurological examinations in children, including the limited standardisation and the lack of age-specific adjustments that would improve the child-friendliness [Citation24]. Further barriers may include global mental function, communication, or the child’s ability to stay concentrated. They and we can conclude that a lot of work still needs to be done to develop valid outcome measures that are more child-friendly and suitable for clinical practice.
For the two tactile function outcome measures, the monofilaments for detecting light touch and the two-point discrimination test, consensus was not achieved on any of the three criteria. Panellists commented in their free-text statements that these assessments may be of value to use in the rehabilitation for some children in clinical practice, such as children after acquired brain injury or spinal lesions. We assume that evaluating light touch is used more as a measure of somatosensory recovery in these patient groups. Particularly for patients with spinal cord injury, segmental changes in light touch are part of the International Standard for Neurological Classification of Spinal Cord Injury (ISNCSCI) [Citation37].
The panellists agreed that modalities of body awareness (spatial and structural body representation) should be included in assessing somatosensory function in these children. This agrees with the Delphi study by Clark et al., in which experts also recommended these two modalities in the neurologic examination of the paediatric lower limb [Citation24]. However, to date, no standardised protocols are available to assess these modalities. Overall, the findings of the current study indicate that the majority of the assessments of somatosensory function currently available needs to be adapted for routine use within paediatric clinical practice. Our results might also be of interest for other paediatric and adult patient groups. For example, children with developmental coordination disorders (DCD) can show similar sensorimotor impairments as children with UMN lesions, including reduced somatosensory function, especially proprioception [Citation41,Citation42].
Methodological limitations
One methodological consideration is the relatively small number of panellists, which also reflects the relatively small number of articles published in the field of assessing somatosensory function in children with UMN lesions [Citation17]. In addition, some of the panellists did not work with all of the currently available somatosensory function assessments. This reflects that standardised tests to assess somatosensory functions are rarely applied in routine clinical practice [Citation17]. This lack of standardly applied tests is supported by multiple experts’ comments in our Delphi study such as: “it is fine to have tests, they need to be standardised and valid”; “I feel all of these are important and under assessed”; “Just to say I do not regularly use all of these (outcome measures) but feel we should.”
Further, for some modalities, there is currently no instrument available, and these modalities are therefore not explicitly tested. For example, although joint movement sense can be assessed with the sensory scale of the Fugl-Meyer Assessment, panellists commented that they would prefer an instrument with sensors that accurately measures changes that are relevant to motor function. Devices to assess joint movement sense are currently available for research purposes but are not yet accessible for routine clinical practice [Citation13].
However, the currently available measures need to be adapted, especially in relation to their suitability for clinical practice and child-friendliness. Further, the view of the expert panellists indicated that a clear link to motor functions and the treatment goal must be evident to justify using the somatosensory outcome measure.
Finally, future directions of research should include the perceptions of children and families in relation to modalities of somatosensory function that they would consider meaningful to assess. In particular, families could be involved in helping to decide which outcome measures are perceived as feasible and child-friendly and, if not, how they need to be adapted to achieve this.
Conclusion
This study explored the expert consensus regarding the categories and modalities, and finally the outcome measures to be included in a toolbox assessing lower limb somatosensory function in children with UMN lesions. The currently available measures need to be adapted, especially concerning their suitability for clinical practice and child-friendliness. Based on statements from the panellists, the assessments should be relevant for activity and participation and finally their application should result in a benefit for the child and the treatment process.
2021_Supplementary_S2.docx
Download MS Word (46.2 KB)2021_Supplementary_S1.docx
Download MS Word (36.3 KB)Acknowledgment
We highly appreciate the panel members for their participation and valuable feedback; Prof. Liana Palermo, Anastasia Zarkou PT, PhD, Prof. Dr. Eugene Rameckers, Dr. Margret Mayston, Beverly Cusick PT, MS, Rashelle Hoffman PT, PhD, Jenny Carroll PT, Susanne Loew PT, Kirsten Ursem PT, Dr. Arturo Nuara, Ria Cuppers, PT MSc, Pieter Meyns, PhD, Béatrice Marth, PT MAS, and Heather Holgate OT MAS, Rolf Noergaard, PT.
Disclosure statement
The authors alone are responsible for the content and writing of the paper. The authors declare no conflict of interest. This work was in part sponsored by a grant from the Anna Müller Grocholski Foundation, which was not involved in study design, data collection, data analysis, and manuscript preparation, and publication decisions.
Additional information
Funding
References
- de Haan EHF, Dijkerman HC. Somatosensation in the brain: a theoretical re-evaluation and a new model. Trends Cogn Sci. 2020;24(7):529–542.
- Hall J. Guyton and hall textbook of medical physiology. 13. Philadelphia: Elsevier; 2016.
- Kurz MJ, Heinrichs-Graham E, Becker KM, et al. The magnitude of the somatosensory cortical activity is related to the mobility and strength impairments seen in children with cerebral palsy. J Neurophysiol. 2015;113(9):3143–3150.
- Choi J, Vining E, Mori S, et al. Sensorimotor function and sensorimotor tracts after hemispherectomy. Neuropsychologia. 2010;48(5):1192–1199.
- de Bode S, Fritz S, Mathern GW. Cerebral hemispherectomy: sensory scores before and after intensive mobility training. Brain Dev. 2012;34(8):625–631.
- Corti C, Poggi G, Massimino M, et al. Visual perception and spatial transformation of the body in children and adolescents with brain tumor. Neuropsychologia. 2018;120:124–136.
- Fontes PL, Cruz T, Souto DO, et al. Body representation in children with hemiplegic cerebral palsy. Child Neuropsychol. 2017;23(7):838–863.
- Nuara A, Papangelo P, Avanzini P, et al. Body representation in children with unilateral cerebral palsy. Front Psychol. 2019;10:354.
- Zarkou A, Lee SCK, Prosser LA, et al. Foot and ankle somatosensory deficits affect balance and motor function in children with cerebral palsy. Front Hum Neurosci. 2020;14:45–12.
- Damiano DL, Wingert JR, Stanley CJ, et al. Contribution of hip joint proprioception to static and dynamic balance in cerebral palsy: a case control study. J NeuroEngineering Rehabil. 2013;10(1):57.
- Wingert J, Burton H, Sinclair R, et al. Tactile sensory abilities in cerebral palsy: deficits in roughness and object discrimination. Dev Med Child Neurol. 2008;50(11):832–838.
- Wingert J, Burton H, Sinclair R, et al. Joint-position sense and kinesthesia in cerebral palsy. Arch Phys Med Rehabil. 2009;90(3):447–453.
- Rosenbaum P, Paneth N, Leviton A, et al. A report: the definition and classification of cerebral palsy. Dev Med Child Neurol. 2006;49:8–14.
- Robert MMT, Guberek R, Sveistrup H, et al. Motor learning in children with hemiplegic cerebral palsy and the role of sensation in short-term motor training of goal-directed reaching. Dev Med Child Neurol. 2013;55(12):1121–1128.
- Brownell CA, Zerwas S, Ramani GB. “So big”: the development of body self-awareness in toddlers. Child Dev. 2007;78(5):1426–1440.
- Auld M, Boyd R, Moseley G, et al. Tactile assessment in children with cerebral palsy: a clinimetric review. Phys Occup Ther Pediatr. 2011;31(4):413–439.
- Walmsley C, Taylor S, Parkins T, et al. What is the current practice of therapists in the measurement of somatosensation in children with cerebral palsy and other neurological disorders? Aust Occup Ther J. 2018;65(2):89–97.
- Lindvall MA, Anderzén Carlsson A, Forsberg A. Basic body awareness therapy for patients with stroke: experiences among participating patients and physiotherapists. J Bodyw Mov Ther. 2016;20(1):83–89.
- Ahn S-N. Differences in body awareness and its effects on balance function and independence in activities of daily living for stroke. J Phys Ther Sci. 2018;30(11):1386–1389.
- Zimmermann-Schlatter A, Schuster C, Puhan MA, et al. Efficacy of motor imagery in post-stroke rehabilitation: a systematic review. J NeuroEngineering Rehabil. 2008;5(1):8.
- Dickstein R, Levy S, Shefi S, et al. Motor imagery group practice for gait rehabilitation in individuals with post-stroke hemiparesis: a pilot study. NeuroRehabilitation. 2014;34(2):267–276.
- Ehrsson HH, Spence C, Passingham RE. That’s my hand! activity in premotor cortex reflects feeling of ownership of a limb. Science. 2004;305(5685):875–877.
- Busse M, Tyson SF. How many body locations need to be tested when assessing sensation after stroke? An investigation of redundancy in the rivermead assessment of somatosensory performance. Clin Rehabil. 2009;23(1):91–95.
- Clark R, Baque E, Wells C, et al. Perceived barriers, enablers and modifications to tests assessing pediatric lower limb neurological impairment: an international Delphi survey. Phys Ther. 2021;101(3):1–11.
- Clayton K, Fleming JM, Copley J. Behavioral responses to tactile stimuli in children with cerebral palsy. Phys Occup Ther Pediatr. 2003;23(1):43–62.
- Cooper J, Majnemer A, Rosenblatt B, et al. The determination of sensory deficits in children with hemiplegic cerebral palsy. J Child Neurol. 1995;10(4):300–309.
- Goble DJ, Hurvitz EEA, Brown SSH. Deficits in the ability to use proprioceptive feedback in children with hemiplegic cerebral palsy. Int J Rehabil Res. 2009;32(3):267–269.
- Sanger T, Kukke S. Abnormalities of tactile sensory function in children with dystonic and diplegic cerebral palsy. J Child Neurol. 2007;22(3):289–293.
- Uzun Akkaya K, Elbasan B. An investigation of the effect of the lower extremity sensation on gait in children with cerebral palsy. Gait Posture. 2021;85:25–30.
- Asano D, Morioka S. Associations between tactile localization and motor function in children with motor deficits. Int J Dev Disabil. 2017;64(2):113–119.
- McMillan SS, King M, Tully MP. How to use the nominal group and delphi techniques. Int J Clin Pharm. 2016;38(3):655–662.
- Bayley EW, MacLean SL, Desy P, et al. ENA’s delphi study on national research priorities for emergency nurses in the United States. J Emerg Nurs. 2004;30(1):12–21.
- Schiariti V, Klassen AF, Cieza A, et al. Comparing contents of outcome measures in cerebral palsy using the international classification of functioning (ICF-CY): a systematic review. Eur J Paediatr Neurol. 2014;18(1):1–12.
- Verschuren O, Ketelaar M, Keefer D, et al. Identification of a core set of exercise tests for children and adolescents with cerebral palsy: a Delphi survey of researchers and clinicians. Dev Med Child Neurol. 2011;53:449–456.
- Wright FV, Majnemer A. The concept of a toolbox of outcome measures for children with cerebral palsy: Why, what, and how to use? J Child Neurol. 2014;29(8):1055–1065.
- Keeney S, Hasson F, Mckenna H. The Delphi Technique in Nursing and Health Research; 2010.
- Schuld C, Franz S, Brüggemann K, et al. International standards for neurological classification of spinal cord injury: impact of the revised worksheet (revision 02/13) on classification performance. J Spinal Cord Med. 2016;39(5):504–512.
- Marsico P, Meier L, van der Linden M, et al. Psychometric properties of lower limb somatosensory function and body AwarenessOutcome measures in children with upper MotorNeuron lesions: a systematic review. Dev Neurorehabil. 2021;25(5):1–14.
- Mclaughlin JF, Felix SD, Nowbar S, et al. Lower extremity sensory function in children with cerebral palsy. Pediatr Rehabil. 2005;8(1):45–52.
- Portnoy S, Maayan C, Tsenter J, et al. Characteristics of ataxic gait in familial dysautonomia patients. PLoS One. 2018;13(4):e0196599–14.
- Chen FC, Pan CY, Chu CH, et al. Joint position sense of lower extremities is impaired and correlated with balance function in children with developmental coordination disorder. J Rehabil Med. 2020;52(8):jrm00088.
- Verbecque E, Johnson C, Rameckers E, et al. Balance control in individuals with developmental coordination disorder: a systematic review and meta-analysis. Gait Posture. 2021;83:268–279.
