Abstract
Purpose
People with severe intellectual disabilities are often supported during mealtimes. However, little information exists about how they and care staff co-ordinate their mealtime behaviours.
Method
Four people with severe intellectual disabilities and 12 members of care staff participated in this research. Video data were collected from two services for people with intellectual disabilities. Approximately 30 eating or drinking interactions were filmed, totalling approximately 9.5 h of footage. This footage was analysed using conversation analysis (CA). Ethnographic notes were made. CA is a fine-grained systematic approach which allows examination of how mealtimes are achieved, looking closely at verbal and non-verbal behaviours.
Results
Results show how people with severe intellectual disabilities can demonstrate whether they are ready, or not, for a mouthful of food or drink despite their limited language abilities. Ways in which readiness and unreadiness were demonstrated are outlined and staff responses are also considered.
Conclusions
There are wider implications for self-determination among people with severe intellectual disabilities. Examples provided suggest that people with severe intellectual disabilities can, and do, make decisions about how fast they eat and when they prefer to complete other activities. Respecting these decisions, carers better support the autonomy of individuals with severe intellectual disabilities.
Impacts for rehabilitation
People with severe intellectual disabilities often need support in eating and drinking.
People with severe intellectual disabilities use a variety of verbal and non-verbal resources to show when they are ready and when they are not.
Decisions made by people with severe intellectual disabilities relating to mealtimes should be acknowledged and respected.
Allowing people with severe intellectual disabilities to steer mealtime activities promotes agency and self-determination.
Introduction
When a person with severe intellectual disabilities (SID) is supported to eat or drink orally (as opposed to through a tube), this action is by definition co-achieved. The person with intellectual disabilities cannot be a passive participant as they need at least to open their mouth and swallow. However, research into how people with SID and those supporting them co-ordinate mealtime behaviours is limited. This paper is an in-depth, qualitative examination of how people with SID and care workers coordinate their behaviours in feeding/eating interactions, paying particular attention to how people who receive assistance with eating use non-verbal behaviours to exert some control over the process, and how care workers respond to these behaviours.
People with severe intellectual disabilities and dysphagia
People with SID often have difficulties transporting food to their mouth and may also have dysphagia [Citation1]. Dysphagia refers to difficulties in swallowing and carries potentially life-threatening health risks such as choking [Citation2–5]. Guidance about supporting those with dysphagia, including those with intellectual disabilities, relates mostly to dysphagia management, with less attention paid to communication [Citation6]. In an evaluation of compliance with guidance on dysphagia provided by speech and language therapists, Chadwick et al. [Citation7] found higher levels of compliance with practical guidance such as the use of equipment, changing food consistency and physical positioning, and lower levels for guidance relating to support, prompting, socialising, and ensuring that a bolus had been swallowed. They suggest that this may be because advice on the latter was more abstract than practical advice on the former. In contrast, Charpentier et al. [Citation8] noted that when support was given by parents in a home setting to people with intellectual disabilities and dysphagia, advice about pacing and communication was more likely to be followed.
People with severe disabilities and mealtime interactions
Research into mealtime communication involving people with SID indicates that the focus of care staff is on getting the job of eating/drinking done, whereas other more social elements such as being playful or engaging in simple chat are often not viewed as a priority [Citation9–11]. Robertson et al. [Citation1] suggest that limited interactivity may carry psychosocial risks such as reduced choice and enjoyment of food, and Harding and Cockrill [Citation12] emphasized the need to manage both health and emotional risks, one of which is the possibility of disempowerment when a person with intellectual disabilities feels unable to control their consumption of food and drink. Ball et al. [Citation13] suggest that more emphasis on improving the social and interactional aspects of mealtimes may enhance the experience and enjoyment of them by people with intellectual disabilities.
In some ways, psychological and social risks are related to medical risks for those with complex eating and drinking needs. Harding and Halai [Citation6] suggest that if interaction is effective at mealtimes, then risks relating to swallowing are reduced. These authors point out that it is important to try to establish how people with limited communication signal that they are ready for food or drink. If a carer can understand from the behaviour of the person with SID that they still have a mouthful of food, they may wait before offering more and thus prevent a harmful gagging or choking response.
Schwier and Stuart [Citation14] suggest that waiting for a person with intellectual disabilities to signal that they are ready for the next mouthful also puts them in control of the pace of the interaction, which is likely to have positive psychological and emotional benefits. Self-determination, the capacity to act in one’s own life with agency, is widely recognized as important to psychological wellbeing [Citation15], and UK government policy since the white paper Valuing People [Citation16] has required services to ensure that people with intellectual disabilities have as much choice and control over their own lives as possible. Although the focus in policy documents is often on the “large” life decisions, such as where to live, self-determination is also about smaller decisions and actions during everyday activities, such as when to go to bed, who to sit next to, and how quickly to eat. However, how people with SID exert agency in the small activities of life is not widely researched [Citation17–19].
Conversation analysis and mealtime interactions
This study uses conversation analysis (CA) to examine mealtime interactions. CA provides a systematic approach to examine how social action is co-achieved. One of the benefits of using this approach is that it ensures that the behaviours of the person with SID are considered, something that has largely been neglected to date. CA also allows examination of how care staff behave during mealtime interactions, and how the two interactants respond to each other over a sequence of turns. One of the underlying principles of CA is that participants in a “conversation” are considered “to mutually orient to, and collaborate to achieve, orderly and meaningful communication” (p.1[Citation20]).
CA has been used to examine the sequential order of non-verbal interactions both in children [Citation21] and adults with intellectual disabilities (e.g., Finlay et al. [Citation18]) among others. There is also a growing body of work which uses CA to examine the communicative and social aspects of family mealtime interactions (e.g., see literature [Citation22,Citation23]). Particularly relevant for this paper, conversation analytic research has examined how requests can be made non-verbally among non-disabled people [Citation24]. For example, when playing cards, a player holds out an object (their hand of cards) for another to take from. When preparing potatoes, a person who has peeled a potato places it in a meaningful position (i.e., on the chopping board) for another person to cut, and when collecting plates after a meal a person reaches out for an object (the plate) that the other person controls. Pointing is also an important way to indicate requesting actions non-verbally. All of these examples are joint activities where the non-verbal request allows for the activity to continue. Rossi [Citation24] concludes that most non-verbal requests occur in circumstances which are based upon highly structured joint activities. Supported mealtime interactions are exactly that and therefore allow for such “requests” (although we have chosen to avoid this terminology, as explained later) to occur.
Previous research also demonstrates that non-verbal presentations of objects can act as offers [Citation25]. In many of the mealtime sequences we describe below, the staff member prepares a spoon of food and puts it in a particular position near the person with SID. Using the term “offer” in these cases may suggest that the staff member was the first person to initiate the feeding/eating sequence. However, this was not always the case as some presentations of food by workers were initiated by people with SID signalling that they were ready to eat. Schwier and Stewart [Citation14] suggest that such signals include looking at the person supporting them or opening the mouth. These behaviours might sometimes be referred to as “requests”.
We use the term “demonstrations of readiness” rather than “offers” and “requests” because it is a neutral term and acknowledges the co-operative nature of the activity. Also, readiness can be demonstrated at varying levels of intensity. Although some behaviours may look like requests and offers, others may be more ambiguous (e.g., gaze), while others might look more like pre-expansion sequences [Citation26] (a sequence which occurs before, and lays the groundwork for, a base sequence [Citation27]). The use of the more inclusive and neutral label of “readiness” in this paper accommodates this ambiguity and allows for a greater degree of flexibility and more nuanced interpretation of the data where those involved have limited communicative ability. Because of the differing abilities of the participants, the ways in which they demonstrate readiness to staff, and the ways in which staff demonstrate readiness to them, differ. However, the actions that these behaviours achieve appear to follow a similar sequential pattern.
In summary, this article offers an in-depth qualitative examination of how supported feeding/eating interactions occur in care settings. It illustrates how people with SID and support workers co-ordinate their behaviours, how those being supported signal that they are ready or not, and thus exert agency over their consumption, and how supporters respond to these signals. By closely examining the different behaviours used by staff during mealtimes, we also identify those which are effective and those which are less so, with a view to illuminate and inform best practice.
Methods
Setting
Data were collected at two services for people with intellectual disabilities (Langley and Daisy Way - names have been changed). Langley, a day centre, catered for approximately 40 service-users with severe to mild intellectual disabilities. Daisy Way, a residential centre, provided support for seven adults with severe intellectual disabilities.
Participants
Five adults with severe intellectual disabilities (one woman, four men) and 12 members of care staff (four women, eight men) participated in the research. The mean age of participants with severe intellectual disabilities was 37.6 years (range 31–48). Three had no verbal abilities, one could use only a small number of words/phrases, whereas one could use a greater number of phrases but his verbal abilities were declining and he had a significant delay in his verbal responses. Although five participants with SID were recruited, one of them did not eat orally, instead using a PEG (Percutaneous Endoscopic Gastrostomy), a tube which goes directly into the stomach through the abdominal wall. The other four all required physical assistance to move food from the table to their mouth. The number of years experience of the care staff was from 15+ years to less than a year.
Ethics
The UK Social Care Research Ethics Committee granted ethical approval for this research. Approval was also given by the Research Governance Boards from the relevant local authorities. Consent and data collection procedures were consistent with the Mental Capacity Act [Citation28] and included numerous checks before and during recording for signs of distress or dissatisfaction on the part of the participants. Pseudonyms have been used throughout.
Procedure
One of the authors (CN) visited the two services repeatedly over approximately one year. During this time CN collected 40 h of video recordings of everyday interactions comprising activities such as music sessions, physiotherapy, and meals. Thirty interactions involving eating or drinking were recorded, and involved 4 service-users and 12 staff members (totalling approximately 9.5 h of video).
The majority of these interactions were filmed during lunch, but some footage includes people having drinks or jelly in the mornings/afternoons. The videos varied in length, from some short drinking interactions lasting 2 min for a single drink, to approximately 40 min of footage capturing lunch, dessert, and a drink.
To supplement the recordings, ethnographic notes were made and ad hoc interviews with care staff regarding particular behaviours that were observed were carried out. Ethnographic notes describing written institutional guidelines relevant to the behaviour of support staff were used in a limited way [Citation29]. In extract 5, we have noted that Jake has a health condition that all staff are aware of and are encouraged to monitor. In extract 8, we note that the behaviour of the supporter runs counter to the written institutional guidelines for supporting Jake, and that he is a new member of staff. Although we do not assert that these are definite reasons for the supporter’s behaviour in each instance, we note them as relevant contextual factors in understanding the eating/feeding activities we are interested in. For this paper, the video footage was watched, catalogued, and analysed with a focus on how mouthfuls were co-achieved. A bottom-up conversational analysis approach was taken [Citation20]. Although it was possible to transcribe the extract using multimodal conventions (such as Mondada’s [Citation30]), we opted for the slightly more readable Jeffersonian-style transcription [Citation31] to make the article more accessible for practitioner readers. Close attention was paid to the behaviours and sequential organisation which constituted successful and unsuccessful delivery and acceptance of food on spoons.
A note on conversation analysis terminology
CA considers that social actions occur in interactions sequentially, where interactional turns are relevant to the turns that preceded and those that will follow [Citation27]. The simplest example of sequential organisation in “conversation” is the adjacency pair [Citation26,Citation32]. Adjacency pairs are pairs of conversational turns which occur next to one another, each produced by a different person [Citation33]. Each pair has a first pair part (FPP), produced by the first person, and a second pair part (SPP), produced by the second.
If the FPP is a demonstration of readiness by person 1, then the SPP could be either a demonstration of readiness or unreadiness by person 2. An SPP that aligns with the course of action of the FPP is referred to in CA as preferred, and SPPs that do not are dispreferred. Preference here does not refer to the psychological motives or desires of the second person but to a course of action which aligns with that suggested by the first. When one person demonstrates their readiness to the other (e.g., a worker bringing a spoon of food near the person with SID’s mouth), then the preferred SPP would be for the other person to demonstrate they too are ready (attending, willing and able), for example by opening their mouth. This would align with the intended course of action (of a mouthful being achieved) of the FPP.
Analysis
Sequences involving a preferred response
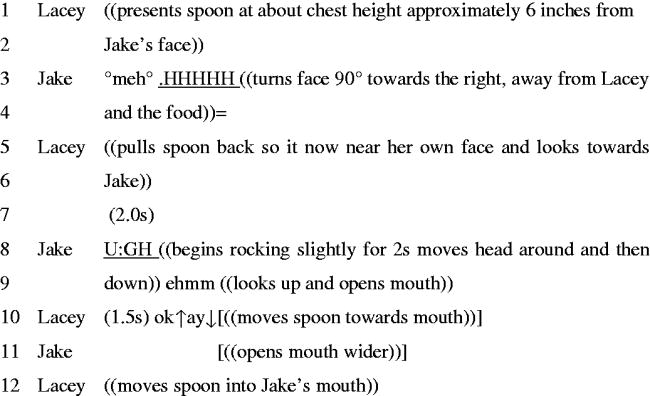
We identified a base sequence with preferred responses, in which mouthfuls were achieved in a straightforward way with the minimum of turns. These either involved the worker or the person with disabilities taking the first turn with a display of readiness, and the other person responding with their own display of readiness (a preferred SPP). In extract 1, Jake, a man with severe intellectual disabilities, is having lunch in the dining room. Lacey, a member of care staff, is supporting him.
Extract 1
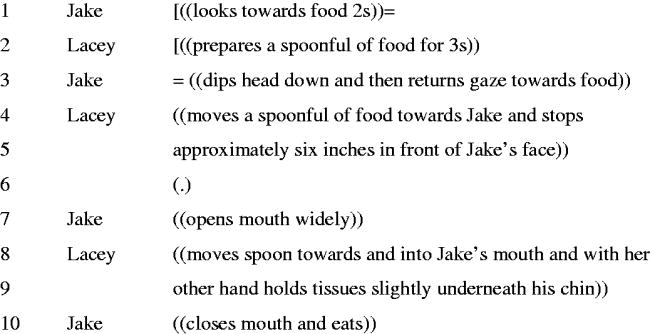
In lines 1 and 3, while Lacey is preparing a spoon of food, Jake looks at the spoon. It is unclear whether Lacey notices this, but her presentation of the full spoon in a particular position (in line 4), namely at eye level, slightly to the right of Jake’s mouth, demonstrates that Lacey is ready. In line 7, Jake responds by opening his mouth. It is clear that both parties are ready to co-complete the mouthful and the actions that follow allow this to be achieved.
Extract 2 shows another non-verbal example of a mouthful being co-achieved. In this example, Jenny, a woman with severe intellectual disabilities, and Tom, a member of care staff, are together with CN, one of the researchers. Andrew, a man with mild-moderate difficulties, who is verbally fluent, is also sitting close by. Although there is some talk in this extract, it is not directed towards Jenny. Andrew is asking Tom if he has seen a TV programme earlier in the week. Our focus, however, is on the interaction between Jenny and Tom.
Extract 2
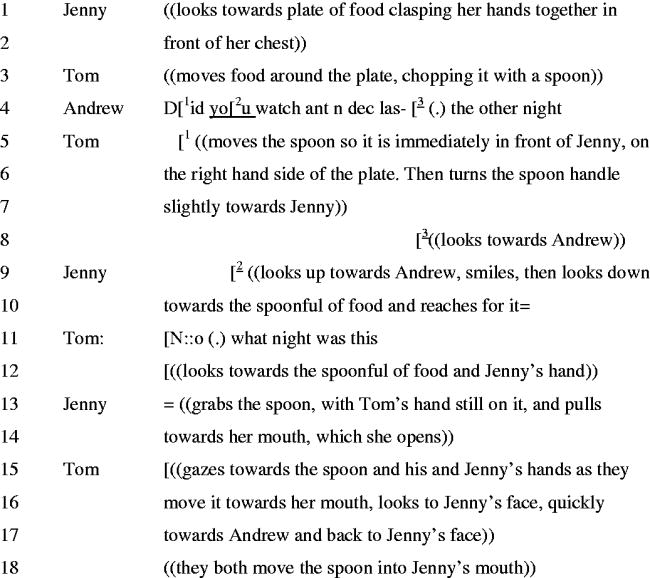
Tom’s presentation of the spoon on the right hand side of Jenny’s plate with the handle facing towards her, demonstrates that he is ready to assist Jenny to take the next mouthful (lines 5–7). In lines 9–10, Jenny then demonstrates her readiness. She does so first by reaching for the spoon. Once her hand is on the spoon, Tom provides hand-over-hand support to help Jenny move the spoon to her mouth, which she opens.
These examples are relatively straightforward. They demonstrate Pomerantz’s [Citation34] principle that when one person’s FPP, here a staff demonstration of readiness, is responded to with a preferred SPP (here, a service-user’s demonstration of readiness), the interactions can be sequentially simple. It should also be noted that in both cases the person with SID had looked at the food before the worker positioned the full spoon: this might have been a FPP if the worker had noticed the gaze and treated it as a signal of readiness.
Extract 3 shows a person with SID, Jenny, initiating the eating sequence. Again, the interaction is relatively straightforward. Jenny is sitting in her wheelchair at a round table in the dining hall of Langley Way. Thomas, a member of care staff, is sitting on her right-hand side.
Extract 3
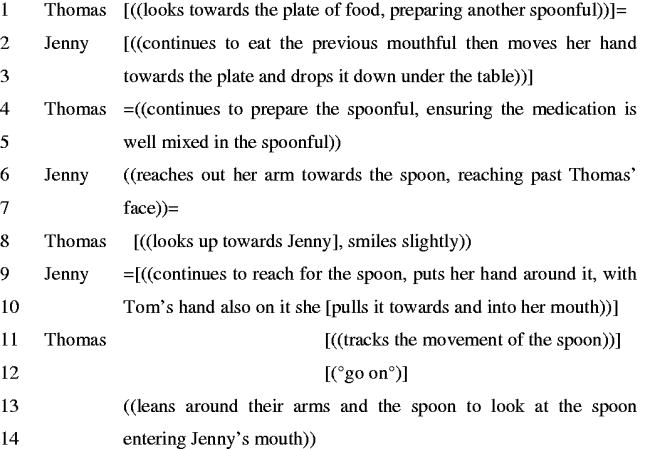
Although Thomas has not presented the spoon to Jenny, he has put food onto the spoon in lines 1 and 4. Before he has time to present the spoon to her, Jenny reaches for and grabs it in lines 6 and 9. Thomas, who acknowledges this by looking towards Jenny and smiling (in line 8), allows the mouthful sequence to continue by not resisting Jenny’s behaviours and provides a verbal go-ahead in line 12.
Sequences involving dispreferred responses
When responses are dispreferred (i.e., when the response to one person’s display of readiness is not a display of readiness by the other), the sequence involves additional interactional work. Extract 4 involves Jake, a man with SID, and Luke, a support worker. Jake is sitting in a chair in the dining hall. Luke is sitting to Jake’s right.
Extract 4
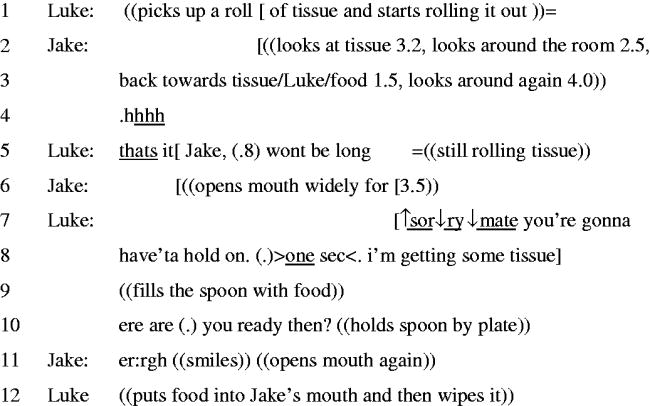
In this extract, Luke and Jake are not ready at the same time. In lines 1 and 5, Luke is otherwise engaged in preparing tissue to use while supporting Jake during lunch. Jake’s use of gaze in line 3 could be seen as an initiation of the activity (see Filipi [Citation21] for examples of how pre-verbal toddlers use gaze to initiate engagement). However, Luke does not respond until Jake’s outbreath in line 4. In line 5, Luke addresses Jake verbally, acknowledging the delay by saying “won’t be long.” After this, Jake clearly demonstrates his readiness by opening his mouth wide (line 6). In line 7, Luke again acknowledges Jake’s display of readiness, this time with an apology and an explanation of why he is not producing the spoon of food.
Here is an example of why we have used the term “display of readiness.” Although Jake’s behaviours during this extract could be interpreted as either requests or complaints, it could also be argued that Jake is simply anticipating the next mouthful. This would, however, still be demonstrating Jake’s readiness even if his actions were not designed for Luke to notice. Jake’s more subtle behaviours (in lines 3 and 4) appear to prompt Luke to demonstrate his understanding of Jake’s behaviour and treat the situation as a complainable one [Citation35], and Luke’s speech in line 5 orients to the delay. When Jake opens his mouth in line 6, his readiness to continue with the course of action is clear. However, Luke’s response in line 7 clearly marks that his response is dispreferred [Citation26]: he provides Jake with an apology, [SORRY MATE], a request that Jake waits and an indication of how long that will be [you’re gonna hav’ta hold on (.) one sec], and an account as to why that is the case [I’m getting some tissue] (lines 7–8). Examples of Jake and others opening their mouth, demonstrating readiness for the next mouthful, occurred several times during the mealtime interactions we recorded. They were not always responded to by staff. Often this seemed to be due to the staff member’s gaze being elsewhere while completing other mealtime-related tasks, meaning that the displays of readiness from the person with SID, at times, appeared to go unnoticed by the staff member.
Coordinating the speed at which a person takes mouthfuls requires both participants in the interaction to display readiness and to monitor the other’s behaviour. When a support worker demonstrates they are ready, for example by holding a spoon of food near the person’s mouth, the person with SID might not be ready for a mouthful for a variety of reasons: they may still have food in their mouth, they may be having trouble swallowing, they may be tired, they may feel nauseous or they may be concentrating on something else, for example. Supporters responded by (1) temporarily withdrawing the spoon, (2) leaving the spoon in position and providing verbal encouragement, (3) offering the food in a more insistent way.
Temporary withdrawal of food
In this extract, Lacey and Jake are in the dining room sitting opposite one another. Lacey responds to Jake’s demonstration of unreadiness by withdrawing the food.
Extract 5
Lacey positions the spoon about 6 inches from Jake’s face. Jake demonstrates his unreadiness in line 3, including a loud, pronounced inbreath suggesting that he may have difficulty breathing and/or swallowing. Jake has a condition which means he may stop breathing at any time so this is a particular risk to him. He also turns away, prompting Lacey to retract the spoon (line 5) and her offer of food. She then looks at him and waits (line 6–7). Finally, in line 9, Jake demonstrates he is ready by moving his head back around to face Lacey and opening his mouth. Lacey shows she understands this as meaning he is ready by saying “okay” and moving the spoon towards him. Jake upgrades his readiness by opening his mouth wider before he receives the mouthful.
In some cases, the behaviour of the person with SID might be ambiguous, leading the supporter to continue, upgrade or repeat an offer of food. In this case, a person might offer a clearer display of unreadiness. An example of this involved Jake, a man with SID, and Luke, a support worker. Luke was trying to feed Jake milkshake from a plastic cup in the dining room. Luke was sitting opposite to him, slightly to his left.
Extract 6
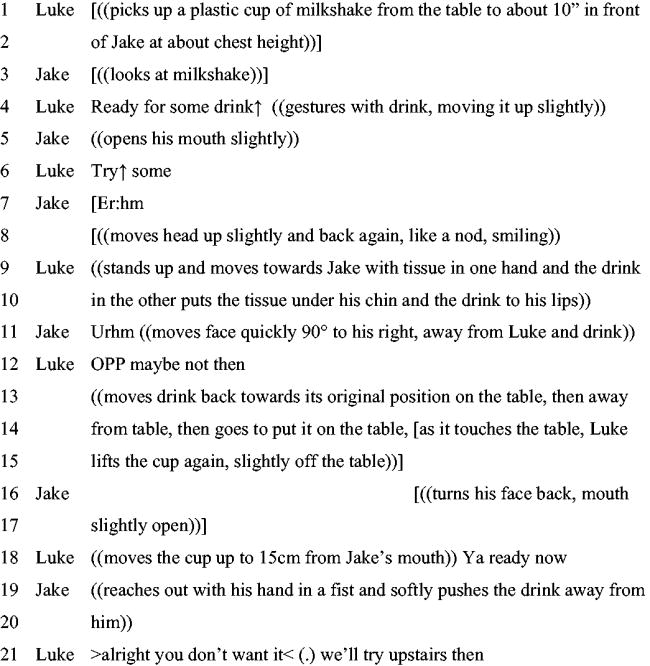
In this example, Jake’s early actions are ambiguous. His gaze towards the drink in line 3 could be perceived as a demonstration of readiness and his slightly open mouth in line 5 would also support this. Yet after Luke’s demonstration of readiness in line 6, Jake vocalises again and moves away from the drink, suggesting he is not ready. Luke then withdraws the drink moving it back towards the table. In line 16, Jake’s turn of his head back towards Luke and the drink could, again, be perceived as a potential act of readiness. Luke responds to this by providing the drink once again to Jake in line 18, but this time Jake’s response is upgraded. He physically pushes the drink away (line 19). Luke treats this as a clear rejection (“>alright you don’t want it< (.)” and offers a possible solution (“We’ll try upstairs then”) - line 21.
Continuing to offer food with further encouragement
In extract 7, taken from the same mealtime recording as extract 5, Lacey continues to offer the food in the face of Jake’s apparent unreadiness.
Extract 7
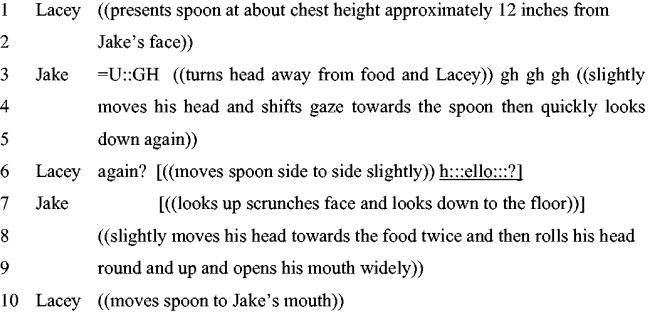
Here, Jake demonstrates that he is not ready for the next mouthful using his voice, facial expression, gaze and head position. He vocalises and turns away from the food (line 3), he scrunches up his face, which staff may understand to be a negative reaction, and he looks at the floor (line 7). Only in line 9 does he indicate readiness by opening his mouth. Throughout the extract, Lacey leaves the spoon in the position she originally put it in line 1. By not withdrawing the spoon, she is able to demonstrate her readiness throughout while she waits for Jake. She also tries to encourage a demonstration of readiness in line 6, both verbally and by “jiggling” the spoon. These behaviours appear to be in response to Jake’s shift of gaze toward the spoon in line 4 which is potentially a subtle sign of readiness. However, in line 7, Jake appears unready again (he looks down to the floor). The non-withdrawal of the spoon allows him the opportunity to be able to decide when he is ready for the mouthful, which he does in line 9 by opening his mouth.
In both extracts 5 and 7, Lacey demonstrates the importance of waiting for Jake to be in a position where he is able, attending, and willing to demonstrate his readiness. In contrast, the next extract shows a different and less successful approach by a support worker.
Supporter offering food in a more insistent way
Before this extract, Jake was brought to an almost empty dining room and left alone for 10 min, while Elvis, a relatively new care worker, prepared the food and became distracted by other tasks. During the wait, Jake’s mood appeared to change markedly. When he entered the room, he was smiling, rocking softly and lightly vocalising, but by the end of the wait he was rocking heavily, biting his hand, making louder and longer vocalisations (similar to screams) and thrashing about in his wheelchair. Others, including CN, attended to Jake and his behaviours became calmer. Elvis then returned and continued to prepare for the meal. In this extract, we see Elvis behave in ways that do not adhere to the centre’s guidelines for supporting Jake, which state that staff should not follow his face with food if he turns away, and that staff should wait to “re-offer” food if Jake refuses. The guidelines also suggest that he should not be taken to the dining hall long before his food is ready as “he does not like to wait for his food.” The extract below includes the first mouthful Jake had of his lunch.
Extract 8
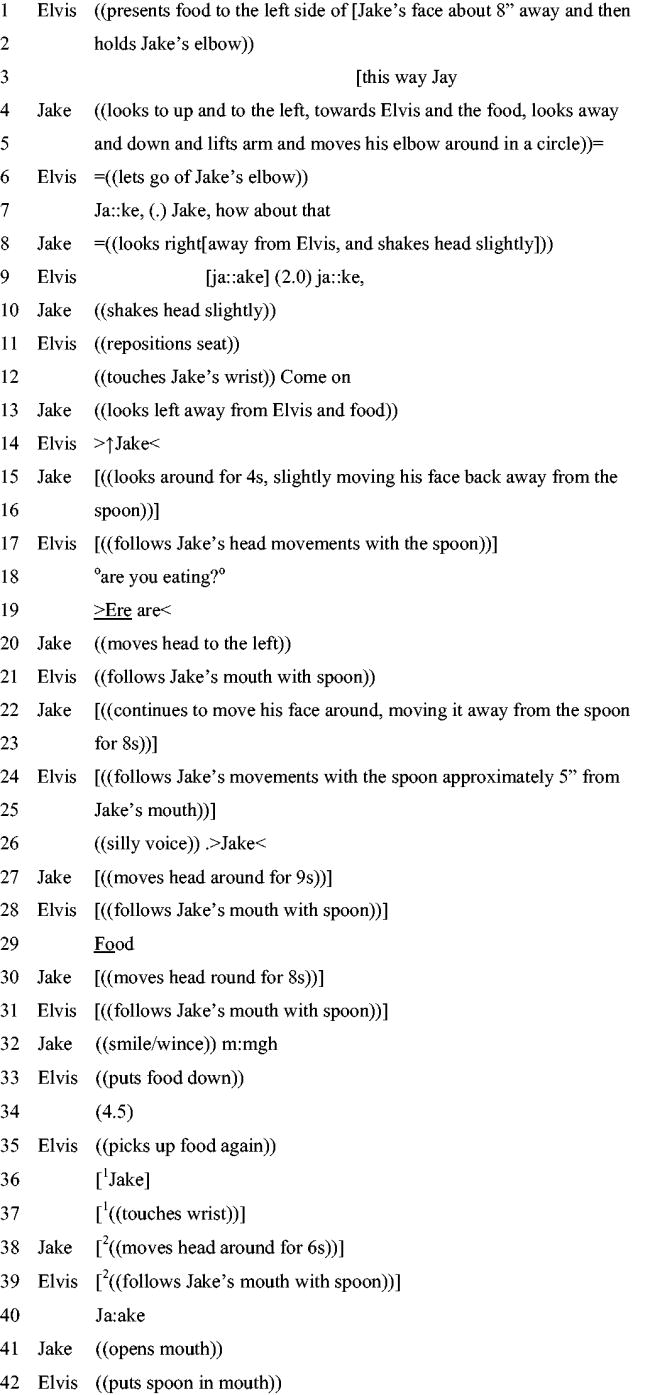
In this extended example, Jake demonstrates his unreadiness in various ways: by not opening his mouth, averting his gaze (lines 4–5 and 13), resisting physical touch (line 5), and moving his face away from the spoon. Elvis continues to encourage him to eat despite these signs, using verbal prompts, touch, and by following Jake’s head movements with the spoon. His talk is clearly designed to encourage Jake’s demonstration of readiness: he uses Jake’s name nine times in this short interaction, says “come on,” and his speech is often animated, a technique often used with infants and people with intellectual disabilities [Citation36]. Finally, in line 33, Elvis accepts Jake’s unreadiness, puts the spoon down and waits for a moment. It is not until line 41 that Jake accepts the spoon by opening his mouth.
Although some of these strategies have been used in other examples in this paper, this extract looks very different because of the sheer number of demonstrations and the lack of time and space Elvis allows between demonstrating his own readiness and seeking such a demonstration from Jake.
The reason Jake is unready is unclear. We cannot say from the data whether he is withholding his readiness as a protest about having been left in the dining room, because he is experiencing emotions which interfere with a desire to eat or interact, because he would prefer to be supported by another member of staff, because he is not actually hungry and is only eating because of the constant, strong encouragement to do so, or for some other reason. Although Jake finishes the rest of his meal, Elvis and Jake are generally not well synchronised, and many of the mouthful sequences look similar to this one. The extract below (which occurs later in the meal) shows a slightly different outcome. Before the transcript begins, Elvis uses the same responses as above. Jake makes some low vocalisations and lets a quantity of saliva escape from his mouth, which Elvis wipes away with a paper towel. Then Elvis continues to offer the spoon.
Extract 9
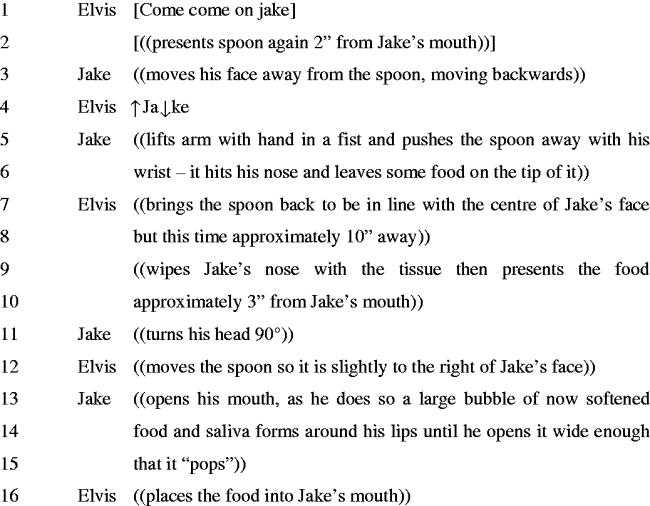
Here, Jake first demonstrates unreadiness by moving his face away from the spoon (line 3) and then upgrading it by using his hand to push the food away (line 5). Elvis continues to encourage him by moving the food back towards his mouth. When Jake does open his mouth (line 13), it is clear that he has been breaking down food, which is still visible in his mouth. A clue that this might be the case is that saliva had come out of his mouth moments before this extract. Surprisingly, instead of providing Jake with more time, or perhaps offering him a drink, Elvis puts the food in his mouth (line 16). In the data set as a whole, staff presented food when service-users still had food in their mouths more often than expected.
Supporter taking advantage of a person’s mouth opening
In some instances, the supporter placed food in a person’s open mouth when it was not clear they had opened their mouth for that purpose. The next example involves Patrick, a service-user who uses talk. He has limited verbal communication skills but one of his utterances is “OH NI:CE” which he uses to show he likes or enjoys something. He also enjoys proto-conversations, non-verbal turn-taking interactions that have some of the features of a conversation without formal language. Here, Patrick is in his wheelchair and Jose (the support worker) is sitting on a chair at an angle to him. This extract involves Patrick’s first and second mouthfuls of food at this mealtime.
Extract 10
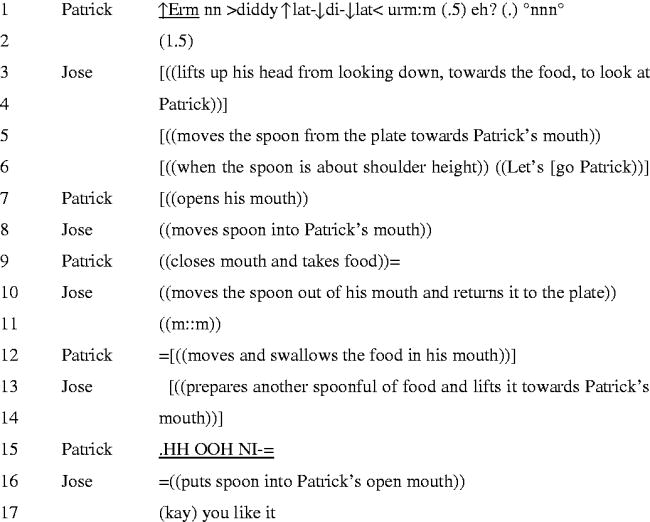
This extract starts with Patrick vocalising in an animated way in line 1, which does not appear to be responded to directly by Jose. The mouthful sequence from lines 3 to 11 is fairly straightforward, and both parties demonstrate readiness to the other, Jose by shifting his gaze towards Patrick, movement of the spoon and providing a verbal prompt (lines 3-6) and Patrick by opening his mouth in line 7. His gaze is also directed towards Jose throughout.
However, Patrick appears unready in the second mouthful sequence. In line 15, Patrick takes a sharp, loud inbreath and utters “OOH NI-“ before he is cut off by Jose placing a spoonful of food into his mouth. Whether Patrick was trying to say “OH NI::CE” to the taste of the first mouthful, or the upcoming arrival of the second, he is clearly enjoying the food and does not react in a negative way to the spoonful of food being put into his mouth. Nevertheless, being part-way through an unfinished utterance strongly indicates that he was not deliberately demonstrating his readiness in line 15. Here it is important to note the difference between being physically and mentally prepared. The person with SID could be considered physically ready when their mouth is open, as it is then possible to put food in their mouth. However, this does not necessarily mean that they are mentally prepared for the next mouthful. As this extract exemplifies, people with SID who need assistance at mealtimes are more than just their bodies and should not be reduced to such. Attention should be paid to the intention behind a person opening their mouth during a mealtime and these intentions respected, promoting dignity and autonomy.
Patrick’s initiations in line 1 and line 15 are ignored, and shortly after the end of the transcript Patrick starts to cough. It could be argued that, had Jose responded to Patrick’s attempts to be social then the mealtime may have been slower paced and this potentially could have been avoided.
Extract 11 also involves a service-user being fed when they had their mouth open for a reason other than eating. Elvis, the same care worker as in extracts 8 and 9, is sitting on Simon’s right and is mainly trying to control any potentially problematic behaviours such as self-slapping. Saheb is sitting on Simon’s left and is mainly providing the prepared spoonfuls of food. They are all in the dining room.
Extract 11
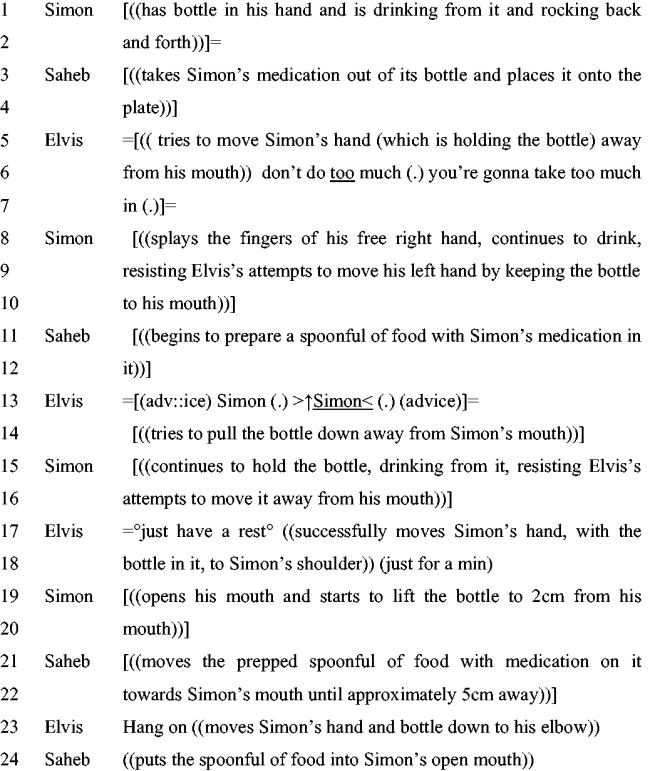
At the beginning of Extract 11, Simon has his own bottle and is in control of how and when he drinks. In lines 5–7, Elvis encourages Simon to stop drinking, seemingly concerned about the rate at which he is consuming the drink. He does this by trying to move the bottle and by using Simon’s name, directives, and other verbal prompts (lines 5–7, 13–14, 17–18). Simon resists this by splaying his fingers, not moving the bottle away from his mouth, and trying to put it back when it is finally moved (lines 8–10, 15–16, 19–20). In line 19, Simon moves the bottle back to his face and opens his mouth. It is clear he is trying to drink. However, at the same time Saheb also moves a spoonful of food very close to Simon’s mouth (line 21–22). Elvis then moves Simon’s hand (and the drink) away from his face (line 23), allowing Saheb to place the food into Simon’s open mouth (line 24).
Discussion
The extracts presented here show that the people with SID in this study are able to demonstrate whether or not they are ready for a mouthful of food or drink despite their limited language abilities. Readiness was demonstrated in a number of ways, including eye gaze towards food and/or the staff member, opening the mouth, and reaching for feeding equipment. More generally, stopping other activities and a lack of behaviours demonstrating unreadiness could also signal readiness. In some cases, these behaviours were ambiguous and staff misinterpreted them, indicating the importance of supporters being flexible in their approach.
Lack of readiness was demonstrated by averted gaze, moving the face away from the staff member and food, facial expressions, body position and posture, vocalisations, pushing the food away, engaging in other courses of action, and involuntary actions such as difficulties breathing or swallowing. A lack of readiness behaviours could also demonstrate unreadiness.
The level to which a person may demonstrate their readiness or unreadiness can vary within a single interaction. This is demonstrated in extract 6 where Jake first simply turns away from the food before pushing it away with his hand. Knowing that a person has the ability to upgrade a response may encourage staff not to abandon the interaction in ambiguous situations. However, the use of persistence by staff in the face of ambiguity requires them to respond appropriately to upgraded behaviours, which was not always the case in the interactions reported in this article.
Staff members demonstrated readiness by preparing a spoonful of food and placing it in a relevant position, providing verbal and physical prompts, and orienting their eye gaze towards the service-user and the food/drink. Staff tried to encourage service-user demonstrations of readiness with gaze, use of names, touching the service-user, verbal directives and encouragement, and movement of the spoon. If the person with SID still did not produce a display of readiness (opening their mouth), there were four different staff responses: (1) withdraw the spoon, (2) leave the spoon in position and encourage verbally, (3) use the spoon to seek a demonstration of readiness by, for example, following head movements away from the food, and (4) take advantage of the service-user’s open mouth if it is open for another reason.
Options 3 and 4 seem the least desirable responses. Without providing the service-user with time or space for their unready state to change, such behaviours could lead to coercion. Withdrawing the spoon or leaving it in position both appear to be appropriate responses to service-user unreadiness. Which is used seems to depend, at least to some extent, on the circumstances of the service-user unreadiness. Leaving the spoon in position allows for a continued demonstration of readiness and gives the service-user more control in the interaction as they do not have to re-elicit the staff member’s demonstration. However, withdrawal tended to be used when there was a medical risk, such as a participant coughing or having difficulty breathing or swallowing.
Sometimes the two participants’ courses of action were not aligned because they were trying to do different things. This was the case for the examples presented under option 4, where the member of staff takes advantage of the service-user’s open mouth. Here, the institutional goal to feed the person is given precedence over self-determination. Placing food in the mouth of a person who is talking supports the finding from previous research that sometimes little attention is given to the two-way interaction of mealtimes, with the focus on getting the job done [Citation9,Citation10].
It has been suggested that if communication relating to eating and drinking is effective during mealtimes then risks relating to swallowing are reduced [Citation6,Citation37]. In addition, Chadwick et al. [Citation7] noted that several dysphagia guidelines suggest that those supporting mealtimes should wait for cues from the person with dysphagia that they are ready for the next mouthful. However, many of those guidelines do not outline what these cues might be, and few real-life detailed examples of feeding/eating interactions have been analysed in the literature. This paper provides examples of readiness cues and demonstrates how communication and interactional co-ordination are important aspects of dysphagia management. If staff are alert to the ways by which service-users demonstrate that they are not ready for a new spoonful of food, perhaps because they are still eating the food from the previous mouthful, then the pacing of the mealtime can be adjusted, and instances of swallowing difficulties and associated problems reduced.
Some of the behaviours exhibited by staff members in this paper did not conform to the particular service-user’s mealtime guidelines which were available in the services. This may reflect insufficient training, insufficient paid time set aside for staff to be fully conversant with the guidelines, lack of communication in the service or lack of access to the guidance. In one service in the current study, files were kept in the offices of senior management, which made it more difficult for staff to quickly refresh their memory on the best way to support a particular person.
There are wider implications for self-determination among people with SID. Not only do we provide several examples here of support workers failing to respect the clear expressions of those they are helping, but the examples also show that people with SID can and do make decisions about when and how fast to eat, and when they prefer to do other activities such as speaking and drinking, even during mealtimes. These small, mundane acts of self-determination are often neglected by measurement scales and policy which often concentrate on the larger and more obvious decisions in a person’s life.
Although it can be difficult to assess the extent to which the behaviours of people with SID are intentional, the choices they express in this article at least appear to demonstrate decision-making abilities. The DSM-5 (2013) states that people with severe intellectual disabilities “cannot make responsible decisions regarding well-being of self or others” (p.36). However, deciding not to open your mouth for another mouthful of food while you are still eating looks like a responsible decision (although the precise meaning of the term “responsible decision” is open to debate). Many of the extracts presented offer examples of interactions that suggest that people with SID can make decisions and that at times these decisions are not treated as legitimate.
There were some examples of social activity occurring at mealtimes. However, the evidence from the footage was similar to previous research [Citation9,Citation10,Citation14] in that the focus of staff was on getting the task done and not on creating a two-way, social, mealtime interaction. Furthermore, as demonstrated in Extract 10, social initiations were sometimes ignored. In this example, when the participant opened their mouth to talk, food was placed inside it. This stark example demonstrates that at times very little attention is given to the social elements of mealtimes.
We believe it is important not to assume that staff members who may have exhibited less than perfect practice always do so, or are ill-meaning. In fact, many of the staff members clearly cared about the service-users and spent their own time and money to further support them. Examples include visiting the service-users in hospital in the staff member’s own time and buying objects, such as light up toys, out of their own money. The staff were brave to allow their practice to be examined in minute detail and when thinking about how to improve practice, responsibility should not only fall on individual staff members. Level of training, staffing numbers, and the ethos of the centre are just three examples of institutional factors that may have an influence on interactions such as those reported in this paper.
Suggestions for further research include examining how successful staff view specific mealtime interactions and asking them to reflect and comment on their own practice. This, alongside the analysis presented within this article, could help to form the basis of staff training relating to supporting people with SID at mealtimes. In addition, further attention should be paid to the communicative resources people with SID use to repair interactions. The term “repair”, which is used in conversation analysis [Citation26], basically refers to how people overcome problems communicating with each other. As noted within the analysis, at times staff members did not attend to the open mouth of the person they were supporting. Topics such as how do people with SID respond to this, whether and how they try to repair the interaction, if so how and when are they successful in doing so, require further research. However, these issues are unfortunately outside the scope of this paper.
Conclusion
People with SID can show they are ready for a mouthful of food or drink by looking towards food or the person supporting them, reaching for feeding equipment, opening their mouth, ceasing incompatible behaviours or not demonstrating unreadiness. Individuals can display lack of readiness by moving their face away from the staff member or the food, pushing away the food, averting gaze, certain individual body positions, facial expressions, postures, and vocalisations, or engaging in other courses of action. Difficulties breathing or swallowing and/or a lack of readiness behaviours can also signal unreadiness.
Support workers in this study showed they are ready by preparing a spoonful of food and placing it position, turning their gaze towards the person and the food/drink, and/or making prompts. When the person with SID did not show readiness behaviours, support staff encouraged their production with use of names and other verbal directives and encouragements, gaze, touch, and movement of the spoon. If the person with SID still did not respond to these, there were two positive response types by the supporter: withdraw the spoon, or leave it in position and give further verbal encouragement. Two types of responses were less respectful of the autonomy of the service-user: using the spoon to follow the person’s head movements and putting the food in the person’s mouth when they had opened it for another reason. This study demonstrates how the autonomy of a person with SID is displayed in small moment-to-moment behaviours, and how attention to, and respect for, these behaviours is important for the promotion of self-determination.
Acknowledgements
The authors thank Anglia Ruskin University who provided the funding for this project. Also, our unreserved thanks are given to the centres that accommodated this research and to all the participants involved. The authors thanks are also given to the editor and anonymous reviewers for their insightful feedback, which has helped strengthen the paper.
Disclosure statement
No potential conflict of interest was reported by the authors.
Data availability statement
Research data are not shared. Participant confidentiality could not be protected if video data are shared because individuals could be visually identified.
Additional information
Funding
References
- Robertson J, Chadwick D, Baines S, et al. Prevalence of dysphagia in people with intellectual disability: a systematic review. Intellect Dev Disabil. 2017;55(6):377–391.
- Glover G, Williams R, Heslop P, et al. Mortality in people with intellectual disabilities in England. J Intellect Disabil Res. 2017;61(1):62–74.
- Helfrich-Miller KR, Rector KL, Straka JA. Dysphagia: its treatment in the profoundly retarded patient with cerebral palsy. Arch Phys Med Rehabil. 1986;67(8):520–525.
- Samuels R, Chadwick DD. Predictors of asphyxiation risk in adults with intellectual disabilities and dysphagia. J Intellect Disabil Res. 2006;50(Pt 5):362–370.
- Kennedy M, McCombie L, Dawes P, et al. Nutritional support for patients with intellectual disability and nutrition/dysphagia disorders in community care. J Intellect Disabil Res. 1997;41(5):430–436.
- Harding C, Halai V. Providing dysphagia training for carers of children who have profound and multiple learning disabilities. Br J Learn Disabil. 2009;55(108):33–47.
- Chadwick DD, Jolliffe J, Goldbart J. Adherence to eating and drinking guidelines for adults with intellectual disabilities and dysphagia. Am J Mental Retard. 2003;108(3):202–211.
- Charpentier A, Morgan S, Harding C. A service evaluation of parent adherence with dysphagia management therapy guidelines: reports from family carers supporting children with complex needs in Greece. Disabil. 2018;42(3):1–8.
- Bailey DB, Jr Harms T, Clifford RM. Social and educational aspects of mealtimes for handicapped and nonhandicapped preschoolers. Early Child Spec Educ. 1983;3(2):19–32.
- Ferm U, Ahlsén E, Björck-åkesson E. Conversational topics between a child with complex communication needs and her caregiver at mealtime. Augment Altern Commun. 2005;121(1):19–41.
- Harding C, Wade C, Harrison K. Communication between children and carers during mealtimes. J Res Spec Educ Needs. 2013;13(4):242–250.
- Harding C, Cockerill H. Managing eating and drinking difficulties (dysphagia) with children who have learning disabilities: what is effective? Clin Child Psychol Psychiatry. 2015;20(3):395–405.
- Ball SL, Panter SG, Redley M, et al. The extent and nature of need for mealtime support among adults with intellectual disabilities. J Intellect Disabil Res. 2012;56(4):382–401.
- Schwier KM, Stewart ES. Breaking bread, nourishing connections: people with and without disabilities together at mealtime. Michigan: Brookes Pub; 2005.
- Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. 2000;55(1):68–78.
- Department of Health. Valuing people: a new strategy for learning disability for the 21st century. A White Paper. London: HMSO; 2001.
- Antaki C, Finlay WML, Walton C, et al. Offering choices to people with intellectual disabilities; an interactional study. J Intellect Disabil Res. 2008;52(12):1165–1175.
- Finlay WML, Antaki C, Walton C. Saying no to the staff: an analysis of refusals in a home for people with severe communication difficulties. Sociol Health Illn. 2008;30(1):55–75.
- Nicholson C, Finlay WML, Stagg S. Forms of resistance in people with severe and profound intellectual disabilities. Sociol Health Illn. 2021;43:642–659.
- Hutchby I, Wooffitt R. Conversation analysis. Cambridge (UK): Polity; 2008.
- Filipi A. Toddler and parent interaction: the organisation of gaze, pointing and vocalisation. (Vol. 192) Pragmatics and beyond new series. Amsterdam: John Benjamins Publishing; 2009.
- Kent A. Compliance, resistance and incipient compliance when responding to directives. Discourse Stud. 2012;14(6):711–730.
- Jenkins L, Hepburn A. Children’s sensations as interactional phenomena: a conversation analysis of children’s expressions of pain and discomfort. Qual Res Psychol. 2015;12(4):472–491.
- Rossi G. When do people not use language to make requests. Request Soc Interact. 2014;26:303–334.
- Lerner GH, Zimmerman DH. Action and the appearance of action in the conduct of very young children. In LeBaron DG, Mandelbaum J, editors. Studies in language and social interaction. Mahwah (NJ): Erlbaum; 2003. p.441–457.
- Schegloff EA. Sequence organization in interaction. Volume 1: a primer in conversation analysis. Cambridge: Cambridge University Press; 2007.
- Stivers T. Sequence organization. In Sidnell J, Stivers T, editors. The handbook of conversation analysis. Sussex: Wiley-Blackwell; 2014. p.191–209.
- Mental Capacity Act. London: The Stationery Office; 2005.
- Maynard DW. Ethnography and conversation analysis. In: Hesse-Biber SN, Leavy P, editors. Emergent methods in social research. 2006. p. 55–94.
- Mondada L. Multiple temporalities of language and body in interaction: challenges for transcribing multimodality. Res Lang Soc Interact. 2018;51(1):85–106.
- Jefferson G. Glossary of transcript symbols. Conversation analysis: studies from the first generation. Amsterdam: John Benjamins; 2004. 13–31.
- Sacks H. 1967. The search for help: no one to turn to. In Schneidman E, editor. Essays in self-destruction. New York (NY): Science House;1967. p.203–223.
- Schegloff EA, Sacks H. Opening up closings. Semiotica. 1973;8(4):289–327.
- Pomerantz A. Agreeing and disagreeing with assessments: some features of preferred/dispreferred turn shaped. In Atkinson JM & Hertiage J, editors. Structures of social action: studies in conversation analysis. Cambridge: Cambridge University Press; 1984. p.57–101.
- Schegloff EA. On complainability. Soc Probl. 2005;52(4):449–476.
- Nind M, Hewitt D. A practical guide to intensive interaction. Kidderminster: BILD Publications. 2001.
- Mathisen B. Dysphagia and early language development. Aust Commun Q. 2001;3(1):7–9.
