Abstract
Purpose
To determine the efficacy of the “Training for Occupational health physicians To Involve Significant others” (TOTIS) e-learning module for improving occupational health physicians’ (OHPs) knowledge, attitudes, and self-efficacy regarding involving significant others in the return-to-work process.
Materials and methods
A randomized controlled trial with 87 OHPs, involving an intervention group and a wait-listed control group. Between-group differences in knowledge, attitude, and self-efficacy outcomes, and retention of effects were assessed using ANOVA and paired t-tests. Reactions to the e-learning module were analyzed with descriptive statistics and thematic analysis.
Results
We found moderate to large effects on OHPs’ knowledge (p < 0.001, ηp2 = 0.202), attitudes (p = 0.003, ηp2 = 0.098), and self-efficacy (p < 0.001, ηp2 = 0.237), with retention of all changes at 10-week follow-up. OHPs graded the e-learning module with a mean score of 7.9 out of 10 (SD = 1.11) and indicated that the module increased their awareness of the role of significant others and encouraged them to address this more often.
Conclusions
The TOTIS e-learning module and accompanying materials are valuable resources for OHPs to learn how significant others influence work outcomes of workers with chronic diseases and to manage their involvement in the re-integration process.
Trial registration
This study is registered in the Netherlands Trial Register under trial number NL8744; https://www.trialregister.nl/trial/8744.
The TOTIS e-learning module is the first evidence-based training to improve the knowledge, attitudes, and self-efficacy of occupational health physicians with regard to involving significant others in the re-integration process of workers with chronic diseases.
The e-learning module and accompanying tools can increase the awareness of occupational health physicians about the role of significant others and encourage them to address the role of significant others in the re-integration process of sick-listed workers.
It could be beneficial to expand on the e-learning module with a face-to-face training program involving group interaction, peer discussion, and skills development.
Implications for rehabilitation
Introduction
Significant others (such as partners, family members, or friends) can play an important role in how workers cope with the consequences of a chronic disease, thereby influencing their work and health outcomes [Citation1–5]. Prior research suggests that significant others can meaningfully support workers with chronic diseases in work re-integration after sickness absence, both in daily life and during consultations with occupational health physicians (OHPs) [Citation6–8]. For example, their involvement in occupational health care can be helpful in reducing anxiety in workers, recalling information, and providing extra information to the OHP. Moreover, involving significant others in decision-making and re-integration plans can enhance support and promote helpful behaviors from significant others, and facilitate effective communication and joint problem solving between workers and their significant others. These benefits of significant other involvement could in turn lead to better health, personal relationships, and work outcomes [Citation1,Citation9–11].
Despite the potential benefits of involving significant others in the return-to-work process of sick-listed workers with chronic diseases, it is currently not common practice for OHPs to do so [Citation7]. This can in part be explained by a lack of self-efficacy on the part of OHPs to assess and respond to the cognitions (i.e., illness perceptions, work-related beliefs and expectations) and behaviors of significant others related to work outcomes, highlighting one barrier to successfully implementing significant other involvement in occupational health care [Citation7]. Other studies have found that involving significant others in occupational health care can present additional challenges and that OHPs may find it difficult to involve significant others in care [Citation6–8]. For example, the presence of a significant other could negatively affect the interaction between the worker and OHP or could lead to significant others being involved in ways that may threaten a worker’s autonomy.
To effectively involve significant others in the work re-integration process of workers with chronic diseases, OHPs require the necessary knowledge and skills to (i) identify in which situations the involvement of significant others is called for and the best ways to involve them, (ii) assess how significant others affect the worker’s recovery and return to work, and (iii) facilitate support, effective communication, and successful coping of workers and their significant others. While several clinical and multidisciplinary guidelines advise health professionals to involve significant others in treatments and care [Citation12–21], guidance and training for OHPs on how to manage significant other involvement and what this should entail is generally lacking.
For this reason, we developed the e-learning module “Training for Occupational Health Physicians to Involve Significant Others” (TOTIS) to educate OHPs on how they can best address the role of significant others and manage their involvement in the return-to-work process of workers with chronic diseases. In this study, we focused on the evaluation of this newly developed e-learning module among a sample of Dutch OHPs who were involved in supporting sick-listed workers with chronic diseases to return to work. More specifically, we aimed to determine the efficacy of the TOTIS e-learning module in improving OHPs’ knowledge, attitudes, and self-efficacy with regard to involving significant others in the return-to-work process. We hypothesized that the e-learning module would have positive effects on all three outcomes. In addition, we explored OHPs’ responses to and satisfaction with the e-learning module.
Materials and methods
Design
This study was a non-blinded randomized controlled trial (RCT), with an intervention and a wait-listed control group. In this RCT, we aimed to determine the efficacy of the e-learning module in improving OHPs’ knowledge, attitudes, and self-efficacy (i.e., confidence in their own knowledge and skills) with regard to addressing the role of significant others in the return-to-work process of sick-listed workers with chronic diseases. We were interested in the absolute effects of the e-learning module and therefore wanted to compare OHPs receiving access to the e-learning module with OHPs in an inactive control condition (i.e., not receiving access to the e-learning module). As gaining access to the e-learning module and receiving continuing education points were considered to be important incentives for OHPs to participate in this study, we decided upon a wait-list control group. While it would have been interesting to also determine the relative effects of the e-learning module using an active control condition, this was not feasible in this study because there was no suitable alternative intervention available. In addition to determining the efficacy of the e-learning module, we explored OHPs’ responses to and satisfaction with the e-learning module.
Participants
To be eligible for participation in this study, OHPs had to be proficient in written Dutch and be a registered OHP. In the Netherlands, two types of OHPs are involved in occupational health care: occupational physicians and insurance physicians. Occupational physicians are generally involved in the first two years of sick leave, during which time they provide support and guidance to help employees retain or return to work. In the Netherlands, insurance physicians can work in either the public or private sector. Most work in the public sector and are mainly involved in claim disability assessment after two years of sick leave, although some are also involved in supporting employees to retain or return to work. Insurance physicians who work in the private sector (medical advisors) are involved in the return-to-work processes of self-employed workers. For this study, we included only OHPs whose work tasks included providing support and guidance to sick-listed workers with chronic diseases to help them return to work. Thus, OHPs who were only involved in claim disability assessment were excluded from participation. No other exclusion criteria were applied.
Participants were recruited through (1) the Netherlands School of Public and Occupational Health (NSPOH), (2) the Dutch Association of Occupational Medicine (NVAB), (3) the Dutch Association for Insurance Medicine (NVVG), (4) the Dutch Association of Medical Advisers in Private Insurance (GAV), (5) Arbo Unie (a nationally operating occupational health service), and (6) the Dutch Social Security Institute: the Institute for Employee Benefits Schemes (UWV). An invitation to participate was sent by email to all occupational and insurance physicians (working in either the public or private sector) in these databases. In this email, a short description was given about the study and eligibility criteria. In addition, a link was included to a webpage of the NSPOH with more detailed written information about the study and the registration form to sign up. In addition, the contact information of the researchers was provided to enable potential participants to ask questions or request additional information.
Procedure
All data was collected electronically without direct contact with or interference from the researchers. At the start of the RCT, all participants completed a baseline questionnaire (week 0). Using random sampling in SPSS, the main researcher (NS) allocated OHPs who had completed the baseline questionnaire to either the intervention group or the control group (1:1 ratio). We stratified randomization with regard to profession (i.e., occupational physician vs insurance physician) to ensure a well-balanced representation of the different professions between groups. To prepare for randomization, separate databases were created for respectively occupational physicians and insurance physicians. While the researcher performing the random sampling procedure did have access to the baseline data, the datasets used for randomization did not contain any data other than participants’ name, contact information, and occupation.
After randomization, the NSPOH gave the intervention group access to the e-learning module through a dedicated website link, while the control group was wait-listed for four weeks (week 1–4). After the 4-week trial period, a follow-up questionnaire was disseminated to both the intervention and control group (week 5). Participants in the wait-listed control group were automatically given access to the e-learning module after they completed the follow-up questionnaire. To determine retention of the effects of the e-learning module, the intervention group was asked to complete the follow-up questionnaire for a second time ten weeks after the 4-week trial period. In addition to these questionnaires, participants in both groups were asked to fill out an evaluation form after completing the e-learning module.
To minimize attrition due to missing values, we checked the baseline and follow-up data for missing data. Two weeks after the first notification that participants could complete one of the questionnaires, reminders were sent to participants who had not yet responded. In addition, in cases where a questionnaire was only partially completed, a reminder was sent to the participant to complete the remaining items. In addition to these precautions, participants had to fully complete the baseline questionnaire, the follow-up questionnaire(s), and the evaluation form to qualify for accreditation for participating in this study.
This study was approved by the Central Ethics Review Committee (CTc) of the University Medical Center Groningen (CTc UMCG 202000077) and is registered in the Netherlands Trial Register (NL8744).
Intervention
The TOTIS e-learning module was developed to educate OHPs on how they can best address the role of significant others and manage their involvement in the return-to-work process of sick-listed workers with chronic diseases. The e-learning module aimed to improve OHPs’ knowledge on: (1) how significant others can influence the work participation of workers with chronic diseases, (2) the role of coping of workers and their significant others in the recovery and work re-integration processes, (3) the concepts “illness perceptions” and “dyadic coping” and their relevance for re-integration, (4) how OHPs can assess illness perceptions and coping strategies in workers and significant others, and (5) how OHPs can facilitate helpful illness perceptions, adequate coping and communication among workers and significant others, and how OHPs can intervene on factors that may hinder recovery and re-integration.
The e-learning module consisted of five parts: (1) when and how to address the role of significant others; (2) coping and re-integration; (3) the role of dyadic coping; (4) the role of illness perceptions; and (5) summary of key messages and best-practice recommendations. Content within each part was focused on delivering essential knowledge and translating that knowledge into practical skills (i.e., the “know” and “do” for best-practice in involving significant others). The first four parts included interactive components, such as videos or vignettes in combination with multiple-choice questions. The content was in part based on the results of our previous studies which sought to gain insight into: the relevant cognitive-behavioral factors of significant others associated with work outcomes of workers with chronic diseases [Citation1], OHPs’ current practices [Citation7], and stakeholders’ views on involving significant others in occupational health care [Citation6,Citation7]. The content was additionally based on research of current practices with regard to involving significant others in related professional domains and available literature on the topics addressed within the e-learning module. The e-learning module was accompanied by a conversation tool, which included: (1) a reference book containing an overview of the key messages and practical advice from the e-learning module, (2) validated questionnaires with which OHPs could gain insight into illness perceptions and coping of workers and their significant others, (3) a conversation leaflet that was developed to facilitate communication between workers and significant others, and (4) ten leaflets about different chronic diseases that were developed to promote adequate illness perceptions. More detailed information about the development of the e-learning module is provided in Supplementary material.
In a small pilot study, an independent group of evaluators (1 OHP and 3 public health researchers) was engaged to evaluate the e-learning module. Each evaluator was given online access to the e-learning module. While going through the module, evaluators could directly add free-text comments and recommendations. In addition, they completed a short evaluation survey with questions regarding the appropriateness of the content and the general appearance and functionality of the e-learning module. If one or more aspects were rated neutrally or negatively, evaluators were asked to provide additional information that could be used to improve these aspects. The evaluators were positive about the content, general appearance and functionality of the e-learning module and indicated that no major changes were needed. Based on the free-text comments and the responses to the evaluation survey, we made some minor textual changes to the e-learning module to improve the readability of certain sentences. The final version of the module was assessed for educational quality by the Dutch Social Medicine to Accreditation Bureau (ABSG) and accredited for 1.5 continuing education points for license re-registration of occupational health physicians.
Outcome measures
We measured knowledge with a knowledge test consisting of 20 multiple choice items based on the content and learning objectives of the e-learning module. More specifically, the knowledge test was designed to measure: (1) OHPs’ knowledge of the cognitive and behavioral processes underlying the influence of significant others and considerations to make regarding the involvement of significant others in occupational health care and (2) the OHPs’ ability to assess when and how they can best gain insight into the influence of significant others and involve them in the re-integration process. The knowledge test consisted of different types of questions (i.e., true-false, scenario based, and matching questions). For instance, several factual questions were included about the concepts “illness perceptions” and “dyadic coping”. In other questions, OHPs had to choose the best course of action for an OHP in a specific scenario or match descriptions of illness perceptions or the coping mechanisms of workers and significant others with the corresponding illness perception domain or type of dyadic coping. Each correct answer was scored as “1” and each incorrect answer was scored as “0”. For each measurement, we calculated a sum score for each participant.
We measured attitudes towards involving significant others with 11 items measured on a 6-point Likert scale. Items were derived from a scale designed to identify healthcare providers’ attitudes to family involvement during routine adult critical care [Citation22]. Since the items from this scale were originally designed to measure attitudes about family involvement during routine adult critical care, we adapted the items to better reflect on significant other involvement in the occupational health care context. For instance, the item “I support patient wishes for family members to be present during daily patient care” was changed to “I support wishes of a worker for a significant other to be present during consultations.” For each measurement, we calculated a mean score for participants who had answered at least nine of the ten items, with a higher score representing a more positive attitude towards significant other involvement in occupational health care. The internal consistency of the construct was good, with a Cronbach's alpha ranging from 0.80 to 0.87 across measurements.
We measured self-efficacy with regard to involving significant others with 15 items measured on a 5-point Likert scale. Items were derived from the questions on self-reported knowledge and clinical skills used by Fary et al. [Citation23]. Since these items were originally designed to measure physiotherapists’ self-reported knowledge and clinical skills in managing people with rheumatoid arthritis, we adapted the items to reflect on the knowledge and skills targeted in the TOTIS e-learning module. For example, OHPs were asked to answer the question: “How confident do you feel in your skills to explore dyadic coping processes of workers and significant others?” For each measurement, we calculated a mean score for participants who had answered at least 14 of the 15 items, with a higher score representing a higher degree of self-efficacy with regard to involving significant others in occupational health care. The internal consistency of the construct was good, with a Cronbach's alpha ranging from 0.86 to 0.96.
We measured responses to and satisfaction with the e-learning module with an evaluation form consisting of 13 items, which participants were asked to fill out after completing the e-learning module. Ten items were measured on a 5-point Likert scale, ranging from strongly agree to strongly disagree, including questions on participants’ overall impressions of the content, the organization and structure of the e-learning module, and its perceived usefulness. In one item, participants were asked to grade the e-learning module on a 10-point rating scale. In two open questions, participants were asked to indicate what they appreciated most and what they appreciated least about the e-learning module.
Sociodemographic measures
At baseline, we collected descriptive information of the OHPs (age, gender, profession, employment status, years in practice, and organization size).
Sample size
A priori sample size calculations for a parallel, 2-arm RCT using G*Power software [Citation24] determined that a sample size of 128 would be sufficient to detect an effect size of 0.5 with a power of 80% and a 2-tailed alpha of 0.05. An estimated effect size of 0.5 was considered reasonable based on established recommendations [Citation25]. Estimating an attrition rate of approximately 25% based on prior studies among occupational and insurance physicians [Citation26–31], we aimed to include 160 OHPs.
Data analysis
We analyzed the quantitative data using SPSS version 26 [Citation32]. We used descriptive statistics (i.e., frequencies, percentages, means, standard deviations) to describe the study sample. Differences in baseline characteristics were tested with t-tests for continuous variables and chi-square tests for categorical variables. Analyses were conducted per-protocol, excluding the OHPs for whom no outcome data was available. We also performed intention-to-treat analyses using the last observation carried forward approach, thereby including the OHPs lost to follow-up (17 in the intervention group, and 8 in the control group), but this had no influence on the results. Because this study was an efficacy trial, in which we were interested in the effects of the intervention on OHPs in a specific controlled setting, rather than an effectiveness study carried out in real practice, we chose to present the results of the per-protocol analyses only. We assessed between-group differences in knowledge, attitude, and self-efficacy outcomes using an analysis of variance (ANOVA), applying a significance level of 0.05. In addition, Partial Eta Squared effect sizes were calculated. Following the recommendations of Cohen [Citation33], effects sizes of ηp2 = 0.01, ηp2 = 0.06, and ηp2 = 0.14 were considered to be respectively small, medium and large in magnitudes. In these analyses, we used mean change scores of the three outcomes, which were calculated for each participant by subtracting the mean score of the baseline measurement from the mean score of the follow-up measurement after the 4-week trial period. We used paired t-tests to evaluate retention of changes in knowledge, attitude, and self-efficacy between the first and second follow-up measurements of participants in the intervention group. We used descriptive statistics and thematic analysis to analyze the OHPs’ responses to and satisfaction with the TOTIS e-learning module.
Results
illustrates the participant flow through the RCT, consistent with the CONSORT criteria [Citation34]. A total of 87 OHPs completed both the baseline questionnaire and the follow-up questionnaire after the 4-week trial period. At baseline, the intervention and control groups were similar with regard to demographic and work characteristics: the majority being occupational physicians working in paid employment and having at least 16 years of work experience. More detailed demographic information of the participants in both groups is provided in . There were no differences in baseline characteristics between participants remaining in the final study sample and participants who were lost to follow-up.
Figure 1. CONSORT flow chart of participants through randomized controlled trial. TOTIS: Training for Occupational Health Physicians to Involve Significant Others.
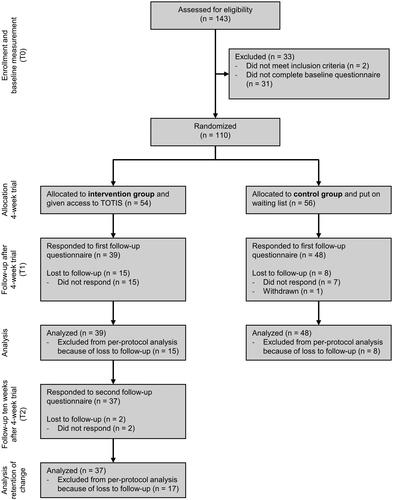
Table 1. Baseline characteristics of participating occupational health physicians.
Representativeness of the sample
About seventy percent of participants in this study was occupational physician and indicated to have at least 16 years of work experience, which is comparable to the general population of OHPs (occupational physicians and insurance physicians) in the Netherlands [Citation35]. The percentage of participants between the age of 55 and 64 years (38 and 62 percent for respectively female and male OHPs) is also comparable to the general OHP population (57 and 45 percent for female and male OHPs). However, a relatively high percentage of OHPs in our study was female (55.2% in our study vs. 37.7% in the general OHP population).
RCT outcomes
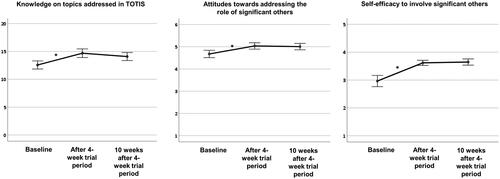
We observed statistically significant between-group differences at the end of the 4-week trial (). The magnitude of positive change in outcomes scores in the intervention group was significantly greater than in the control group for knowledge on topics addressed in TOTIS (F(1, 85) = 21.51, p < 0.001, ηp2 = 0.202), attitudes towards involving significant others (F(1, 85) = 9.25, p = 0.003, ηp2 = 0.098), and self-efficacy with regard to involving significant others (F(1, 85) = 26.38, p < 0.001, ηp2 = 0.237). Partial Eta Squared effect sizes for these differences ranged from 0.098 to 0.237, representing moderate to large effects [Citation33].
Table 2. Between-group differences in knowledge, attitudes, and self-efficacy.
The assumption of normality was violated in the control group for both attitudes and self-efficacy with regard to involving significant others, due to two and one significant outliers respectively. As this could have biased the results, we performed additional analyses excluding these outliers. However, the results for both attitudes (F(1, 83) = 9.18, p = 0.003, ηp2 = 0.100) and self-efficacy (F(1, 84) = 26.48, p < 0.001, ηp2 = 0.240) remained similar to those of the primary analyses.
Thirty-seven participants of the intervention group (94.9%) completed the second follow-up questionnaire ten weeks after the 4-week trial period and were included in the retention of change analyses. illustrates the changes over time for the outcome variables. There were no statistically significant within-group differences between the follow-up after the 4-week trial period and the follow-up ten weeks after the 4-week trial period for knowledge (t(36) = 1.33, p = 0.192), attitudes (t(36) = 0.39, p = 0.700) or self-efficacy with regard to involving significant others (t(36)= −0.45, p = 0.653).
Figure 2. Changes over time for the outcome variables for participants in the intervention group (n = 37). *Statistically significant differences (p < 0.05); TOTIS: Training for Occupational Health Physicians to Involve Significant Others.
Responses to and satisfaction with the e-learning module
A total of 63 OHPs (72.4%) completed the evaluation form after finishing the TOTIS e-learning module. Satisfaction with the e-learning module was high (). OHPs graded the e-learning module with a mean score of 7.9 on a 10-point scale (SD = 1.11), with 60 participants (95.2%) giving a rating of seven or higher.
Figure 3. Occupational health physicians' evaluation of the TOTIS e-learning module. TOTIS: Training for Occupational Health Physicians to Involve Significant Others.
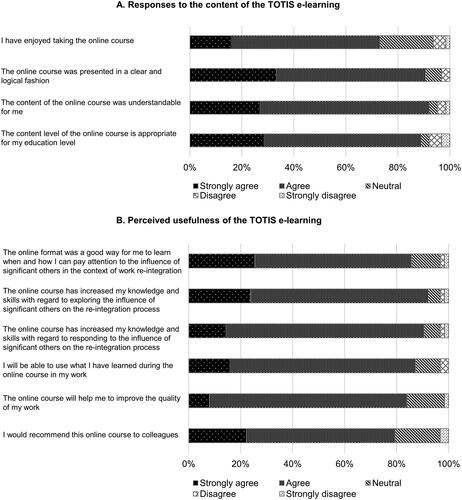
In an open response question, OHPs indicated appreciating various aspects of the TOTIS e-learning module. They considered the subject addressed in the e-learning module to be topical, interesting, and inspiring, and valued the theoretical information and knowledge they gained about the different topics addressed in the e-learning module (e.g., coping strategies, dyadic coping, illness perceptions, and assessment and intervention options). Many OHPs also appreciated the practical advice, tips, accompanying materials, and applicability for occupational health practice. They indicated that the e-learning module increased their awareness, helped them to gain new insights into the role of significant others and encouraged them to address this topic more often. OHPs also valued the different ways that the learning material was offered (e.g., text, videos, animations, examples, practice material, schematics). Finally, some OHPs indicated appreciating the convenience of being able to follow the e-learning module in their own preferred timing, location, and speed.
In a second open response question, OHPs reported what they found least valuable about the TOTIS e-learning module. Some OHPs indicated that they needed time to get used to the online format and that it was easy to miss information, for example due to clicking through the e-learning module too quickly or missing a hyperlink to additional information. Moreover, some OHPs experienced technical issues (e.g., having to repeat parts of the e-learning module due to their progress not being saved correctly or not being able to find the additional material in the learning portal). Furthermore, due to the online format, OHPs missed opportunities to practice with the accompanying materials (e.g., questionnaires), further develop new skills, have peer discussions, ask questions, and receive feedback. Furthermore, some OHPs felt that the e-learning module was too theoretical, indicated that the terminology used in the e-learning module (e.g., dyadic coping) was less useful, and expressed concerns about the applicability in occupational health practice.
Discussion
This study aimed to determine the efficacy of the TOTIS e-learning module with respect to improving knowledge, attitudes, and self-efficacy of OHPs with regard to involving significant others in the return-to-work process of sick-listed workers with chronic diseases. The results of this study show that the OHPs who completed the e-learning module significantly improved on all three outcome measures compared to OHPs who did not have access to the e-learning module, and that these effects remained significant at a 10-week follow-up. Moreover, the e-learning module was positively evaluated by OHPs. Participants indicated that the e-learning module increased their awareness about the role of significant others, helped them to gain new insights into this topic and encouraged them to address the topic more often. In addition, they appreciated the practical advice and tips given in the e-learning module and the accompanying materials. Some OHPs reported difficulties with navigating the e-learning module without inadvertently skipping parts and with technical issues in monitoring their progress. Some OHPs also indicated missing the opportunity to practice with the accompanying materials, to discuss the learning material with their peers, to receive feedback from a trainer, or to further develop new skills.
To the best of our knowledge, this is the first study to evaluate an e-learning module on involving significant others in health care, thereby limiting the possibilities to compare our findings with other studies. However, various prior studies on e-learning programs have shown that online learning can be an effective method to enhance knowledge, attitudes, and self-efficacy among health care professionals [Citation28,Citation36–39]. In many theoretical models, knowledge, attitudes, and self-efficacy are seen as powerful determinants of behavioral change [Citation40,Citation41], which is supported by prior research on determinants of various types of physician behaviors (i.e., communication behaviors, counselling practices, referrals to specialized services, and prescribing behaviors) [Citation42–47]. In a survey study among OHPs, we found that a lack of self-efficacy of OHPs was significantly associated with their assessment of cognitions and behaviors of significant others related to work outcomes of workers with chronic diseases [Citation7]. In addition, we found that negative attitudes towards significant other involvement could also partially explain why some OHPs often pay little attention to the influence of significant others and why OHPs decide to not involve significant others in the re-integration process [Citation7]. Intervening on these behavioral determinants of OHPs by means of the TOTIS e-learning module may lead to them more often addressing the role of significant others in occupational health care. This is consistent with the OHPs’ responses that the e-learning module encouraged them to address this topic more often.
The reported benefits and limitations of the e-learning module format are also found in other studies on internet-based resources for continuing medical education. Consistent with our findings, various studies have shown that e-learning programs can be an effective method for enhancing the knowledge, attitudes, and self-efficacy of health care professionals [Citation28,Citation36–39]. Furthermore, similar to what the OHPs indicated in this study, other studies have highlighted that flexibility with regard to the location, time, and pace of learning is an important advantage of e-learning modules compared to face-to-face training programs [Citation36,Citation37,Citation39]. Finally, prior studies confirm our findings that navigation issues, technical difficulties, lack of interaction with the trainer and peers, and need for a component of face-to-face teaching are potential disadvantages of an e-learning module [Citation36,Citation38,Citation39,Citation48,Citation49].
Strengths and limitations
This study has several strengths. First, the randomized controlled design with follow-up is considered to be the gold standard in assessing intervention efficacy and minimizes confounding factors, as well as allocation and selection bias. Moreover, as all answers were electronically recorded, there was no risk of an outcome assessment bias. In addition, while no standardized instruments were available to measure attitudes and self-efficacy with regard to involving significant others, we derived our items from existing questionnaires and both constructs had good internal reliability across the three measurements.
A limitation of this study is that our final sample size was smaller than intended based on the sample size calculation. One explanation for the lower inclusion rate is the higher workload of Dutch OHPs during the COVID-19 pandemic [Citation50], which may have limited their ability and willingness to participate in research. The COVID-19 pandemic and increased workload might also have resulted in more attrition during this study, especially among participants in the intervention group who had less incentive to complete the follow-up questionnaires as this was not a requirement for them to gain access to the e-learning module. On the other hand, many continuing education activities were cancelled due to the pandemic and opportunities to gain sufficient continuing education points were limited, which might have increased retention of participating OHPs in both the intervention and control group. While no data is available on whether the pandemic has otherwise influenced OHPs’ responses to the e-learning module, we do not expect this to be the case. Although the sample size was sufficient to detect statistically significant effects, a larger study sample would have resulted in more precise estimates of the effects. Furthermore, it is possible that the use of a wait-list control group has resulted in artificially inflated estimates of the effects of the e-learning module, as this is a known issue with a wait-list control design in RCTs [Citation51]. While participating OHPs in the control group were not instructed to refrain from seeking information about involving significant others, it is possible that knowing they would gain access to the e-learning module after the follow-up questionnaire decreased their natural information-seeking behavior [Citation51]. However, we do not expect that a control condition in which OHPs did not gain access to the e-learning after the trial period would have resulted in smaller effects, as lack of time can be an important barrier for OHPs to seek evidence-based information [Citation52,Citation53] and not much information on this topic is easily available for OHPs. Another limitation of this study is that differential retention occurred across conditions, with the control group having better retention than the intervention group. The larger retention in the control group may have been due to the promise that they would receive access to the e-learning module and accompanying tools at the end of the trial, whereas the intervention group already had access during the trial period. Furthermore, as mentioned before, the higher workload of OHPs during the COVID-19 pandemic might have caused higher attrition rates, especially in the intervention group as they had less incentive to complete the follow-up questionnaires since they had already received access to the e-learning module during the 4-week trial period. However, we do not expect that this biased the findings as we found no differences in baseline characteristics between the participants remaining in the final study sample and those who dropped out. Another limitation is that some selection bias seems to have occurred, possibly limiting the generalizability of our study findings. More specifically, compared to the total population of OHPs in the Netherlands, a relatively high percentage of OHPs was female (55.2% in our study vs. 37.7% in the general OHP population). In addition, it is possible that OHPs who already perceived the inclusion of significant others in the return-to-work process to be of value and who were therefore more likely to actually include significant others were more inclined to participate in this study. While it is uncertain whether such a selection has occurred and whether this has biased the results, it is possible that OHPs with less positive perceptions about the inclusion of significant others in the return-to-work process would benefit more from the e-learning module than OHPs who already have positive perceptions about this to start with.
Implications for occupational health practice and future research
The current study shows that the TOTIS e-learning module and the accompanying tools are an effective resource to educate OHPs on how they can best address the role of significant others and manage their involvement in the return-to-work process of sick-listed workers with chronic diseases. Making the e-learning module readily available, for example through educational institutes offering continuing medical education for OHPs, is an important next step. Considering the moderate to large effects of the e-learning module on the three behavioral determinants and the ease and low cost with which it can be implemented, we believe that it would be worthwhile to broadly implement the e-learning module as continued medical education for OHPs. It might also be beneficial to expand on the e-learning module with a face-to-face training program involving group interaction, peer discussion, and skills development (for example, through role-playing exercises).
This study was a first step in evaluating the TOTIS e-learning module by focusing on changes in the three behavioral determinants knowledge, attitude, and self-efficacy of OHPs. Future research is needed to investigate whether these changes actually affected the behavior of OHPs in identifying cases in which the involvement of significant others could be helpful and managing this involvement over the course of the re-integration process. Whether such behavioral changes among OHPs lead to better recovery and sustained return to work for workers with chronic diseases should likewise be examined. Furthermore, in addition to OHPs, other professionals involved in work re-integration might also be able play an important role in the context of significant other involvement in occupational health care. For instance, OHPs might be able to delegate or reallocate tasks surrounding the assessment of the influence of significant others and their involvement in the re-integration process to a job coach, case manager, labor expert, occupational psychologist, or occupational health nurse. The topics addressed in the module are therefore also relevant to other professionals who provide support and guidance to help workers retain or return to work. Therefore, further research is needed to examine the generalizability of the e-learning training module beyond OHPs. A first step in this will be taken in a project that has recently started, in which we will further develop and evaluate the e-learning module for labor experts. Furthermore, future research could focus on translation and validation of the e-learning module and accompanying materials in different countries and settings. An English version of the e-learning module is currently being developed. However, differences in context should be taken into account in translation and implementation of the e-learning module and accompanying materials in different countries and settings.
Conclusion
Our findings indicate that the TOTIS e-learning module and accompanying materials are valuable resources for OHPs to learn about how significant others influence return to work of workers with chronic diseases and to manage their involvement in the re-integration process. Moreover, the e-learning module can increase OHPs’ awareness about the influence of significant others on workers’ coping, recovery, and work outcomes, and encourage them to address this topic more often in their daily practice. Future research should determine whether the e-learning module affects actual significant other involvement by OHPs and whether this in turn leads to better worker outcomes.
Ethical approval
This study was approved by the Central Ethics Review Committee (CTc) of the University Medical Center Groningen (CTc UMCG 202000077).
Informed consent
Informed consent was obtained from all participants in the study.
Author contributions
All authors contributed to the conception and design of the study. NS and HdV developed the questionnaires and invitation letter; SB and MH reviewed the content. NS performed the data collection, data analyses, and drafted the manuscript. All authors have contributed to critical revision of the main intellectual content of the manuscript and have approved the final version.
Online_resource_1.docx
Download MS Word (48.6 KB)Acknowledgements
We thank Puck Winnubst for her contribution to the development of the TOTIS e-learning module. We would also like to thank the Netherlands School of Public and Occupational Health for their contribution to the recruitment of participants and data collection. Furthermore, we would like to thank dr. Tialda Hoekstra for her methodological advice. Finally, we thank all occupational health physicians who participated in this study.
Disclosure statement
Drs. Snippen, Dr. de Vries, and Prof. dr. Brouwer received grants from Instituut Gak to conduct the study; Professor dr. Hagedoorn has nothing to disclose. No potential conflict of interest was reported by the author(s).
Data availability statement
The dataset generated and/or analyzed during the current study is not publicly available, but is available from the corresponding author upon reasonable request. In addition, the e-learning module and accompanying materials are available from the corresponding author upon reasonable request for translation and validation in other countries and settings.
Additional information
Funding
References
- Snippen NC, Vries H d, Burg-Vermeulen S V D, et al. Influence of significant others on work participation of individuals with chronic diseases: a systematic review. BMJ Open. 2019;9(1):e021742–13.
- Rosland A-MM, Heisler M, Piette JD. The impact of family behaviors and communication patterns on chronic illness outcomes: a systematic review. J Behav Med. 2012;35(2):221–239.
- Deek H, Hamilton S, Brown N, FAMILY Project Investigators, et al. Family-centred approaches to healthcare interventions in chronic diseases in adults: a quantitative systematic review. J Adv Nurs. 2016;72(5):968–979.
- Badr H, Acitelli LK. Re-thinking dyadic coping in the context of chronic illness. Curr Opin Psychol. 2017;13:44–48.
- Checton MG, Magsamen-Conrad K, Venetis MK, et al. A dyadic approach: applying a developmental-conceptual model to couples coping with chronic illness. Health Educ Behav. 2015;42(2):257–267.
- Snippen NC, de Vries HJ, Bosma A, et al. Workers’ views on involving significant others in occupational health services. A focus group study. Disabil Rehabil. 2021;:1–12.
- Snippen NC, de Vries HJ, de Wit M, et al. Assessing significant others’ cognitions and behavioral responses in occupational health care for workers with a chronic disease. Disabil Rehabil. 2020;43(19):1–14.
- Sharp RJ, Hobson J. Patient and physician views of accompanied consultations in occupational health. Occup Med. 2016;66(8):643–648.
- Lamore K, Montalescot L, Untas A. Treatment decision-making in chronic diseases: What are the family members’ roles, needs and attitudes? A systematic review. Patient Educ Couns. 2017;100(12):2172–2181.
- Wolff JL, Roter DL. Family presence in routine medical visits: a meta-analytical review. Soc Sci Med. 2011;72(6):823–831.
- Baucom DH, Porter LS, Kirby JS, et al. Psychosocial issues confronting young women with breast cancer. Breast Dis. 2005;23:103–113.
- Vooijs M, van der Heide I, Leensen MCJ, et al. Richtlijn Chronisch Zieken en Werk [Guideline ’the chronically ill and work’]. Amsterdam; 2016. Available from: https://www.psynip.nl/wp-content/uploads/2017/03/Richtlijn_chronisch_zieken_en_werk_2016.pdf.
- Scottish Intercollegiate Guidelines Network (SIGN). Management of chronic pain. A national clinical guideline. Sign; 2019. Available from: https://www.sign.ac.uk/media/1108/sign136_2019.pdf.
- Scottish Intercollegiate Guidelines Network (SIGN). Brain injury rehabilitation in adults. A national clinical guideline; 2013. Available from: http://www.sign.ac.uk/assets/sign130.pdf.
- National Institute for Health and Care Excellence (NICE). Stroke rehabilitation in adults. Clinical guideline [CG162]; 2013. Available from: https://www.nice.org.uk/guidance/qs2/resources/stroke-in-adults-pdf-58292707525%0Ahttps://www.nice.org.uk/guidance/cg162.
- National Institute for Health and Clinical Excellence (NICE). Depression in adults: recognition and management. Clinical guideline [CG90]; 2009. Available from: https://www.nice.org.uk/guidance/cg90/resources/depression-in-adults-recognition-and-management-975742636741.
- National Institute for Health and Clinical Excellence (NICE). Rehabilitation after critical illness. Clinical guideline [CG83]; 2009. Available from: https://www.nice.org.uk/guidance/cg83/resources/rehabilitation-after-critical-illness-in-adults-pdf-975687209413.
- van Dijk JL, Bekedam MA, Brouwer W, et al. Richtlijn Ischemische Hartziekten [Guideline ischemic heart disease]. Utrecht; 2007 [cited 2019 Feb 21]. Available from: www.nvab-online.nl.
- National Institute for Health and Care Excellence. Workplace health: long-term sickness absence and capability to work. NICE guideline [NG146]; 2019. Available from: https://www.nice.org.uk/guidance/ng146.
- Scottish Intercollegiate Guidelines Network (SIGN). Cardiac rehabilitation. A national clinical guideline. Edinburgh: Scottish Intercollegiate Guidelines Network; 2017. Available from: sign.ac.uk/media/1047/sign150.pdf.
- Scottish Intercollegiate Guidelines Network (SIGN). Management of epithelial ovarian cancer. A national clinical guideline. Edinburgh: Scottish Intercollegiate Guidelines Network; 2018. Available from: https://www.sign.ac.uk/media/1073/sign135_oct2018.pdf.
- Al Mutair A, Plummer V, Paul O’Brien A, et al. Attitudes of healthcare providers towards family involvement and presence in adult critical care units in Saudi Arabia: a quantitative study. J Clin Nurs. 2014;23(5–6):744–755.
- Fary RE, Slater H, Chua J, et al. Policy-into-practice for rheumatoid arthritis: randomized controlled trial and cohort study of e-learning targeting improved physiotherapy management. Arthritis Care Res 2015;67(7):913–922.
- Erdfelder E, FAul F, Buchner A, et al. Statistical power analyses using G*power 3.1: Tests for correlation and regression analyses. Behav Res Methods. 2009;41(4):1149–1160.
- Field A. Discovering statistics using SPSS 2nd ed. London: SAGE Publications; 2005.
- Zwerver F, Schellart AJM, Knol DL, et al. An implementation strategy to improve the guideline adherence of insurance physicians: an experiment in a controlled setting. Implement Sci. 2011;6:131.
- Zwerver F, Schellart AJM, Anema JR, et al. Changes in insurance physicians’ attitudes, self-efficacy, intention, and knowledge and skills regarding the guidelines for depression, following an implementation strategy. J Occup Rehabil. 2013;23(1):148–156.
- Hugenholtz NIR, De Croon EM, Smits PB, et al. Effectiveness of e-learning in continuing medical education for occupational physicians. Occup Med. 2008;58(5):370–372.
- Kok R, Hoving JL, Smits PBA, et al. A clinically integrated post-graduate training programme in Evidence-Based medicine versus ‘no intervention’ for improving disability evaluations: a cluster randomised clinical trial. PLOS One. 2013;8(3):e57256.
- van Beurden KM, Brouwers EPM, Joosen MCW, et al. Effectiveness of an intervention to enhance occupational physicians’ guideline adherence on sickness absence duration in workers with common mental disorders: a cluster-Randomized controlled trial. J Occup Rehabil. 2017;27(4):559–567.
- Heselmans A, Donceel P, Aertgeerts B, et al. The attitude of Flemish occupational health physicians toward evidence-based occupational health and clinical practice guidelines. Int Arch Occup Environ Health. 2010;83(2):201–208.
- IBM Corp. IBM SP SS Statistics for Windows, Version 26.0. Armonk, NY: IBM Corp. 2019.
- Richardson JTE. Eta squared and partial eta squared as measures of effect size in educational research. Educ Res Rev. 2011;6(2):135–147.
- Schulz KF, Altman DG, Moher D, CONSORT Group CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ. 2010;11:32–38.
- Capaciteitsorgaan. Capaciteitsplan 2021–2024. Deelrapport 4. Sociaal Geneeskundigen. Utrecht; 2019. Available from: https://capaciteitsorgaan.nl/app/uploads/2019/12/Capacitietsplan-2021-2024-Deelrapport-4-SG.pdf.
- Rouleau G, Gagnon MP, Côté J, et al. Effects of e-learning in a continuing education context on nursing care: systematic review of systematic qualitative, quantitative, and mixed-studies reviews. J Med Internet Res. 2019;21(10):e15118.
- Nesterowicz K, Librowski T, Edelbring S. Validating e-learning in continuing pharmacy education: User acceptance and knowledge change. BMC Med Educ. 2014;14(1):7.
- Vaona A, Banzi R, Kh K, et al. E-learning for health professionals. Cochrane Databse Syst Rev. 2018;1:1–79.
- Regmi K, Jones L. A systematic review of the factors - enablers and barriers – affecting e-learning in health sciences education. BMC Med Educ. 2020;20(1):1–18.
- Perkins MB, Jensen PS, Jaccard J, et al. Applying theory-driven approaches to understanding and modifying clinicians’ behavior: what do we know? PS. 2007;58(3):342–348.
- Godin G, Bélanger-Gravel A, Eccles M, et al. Healthcare professionals’ intentions and behaviours: a systematic review of studies based on social cognitive theories. Implement Sci. 2008;3:36.
- Burglehaus MJ, Smith LA, Sheps SB, et al. Physicians and breastfeeding: beliefs, knowledge, self-efficacy and counselling practices. Can J Public Health. 1997;88(6):383–387.
- Spagnolo J, Vasiliadis H-M, Berbiche D, et al. The influence of primary care physicians’ mental health knowledge, attitudes and self-efficacy on referrals to specialised services: findings from a longitudinal pilot trial. BJPsych Open. 2020;6(6):1–8.
- Schellart AJM, Zwerver F, Anema JR, et al. Relationships between the intention to use guidelines, behaviour of insurance physicians and their determinants. BMC Health Serv Res. 2013;13:400.
- Ponnet K, Wouters E, Van Hal G, et al. Determinants of physicians prescribing behaviour of methylphenidate for cognitive enhancement. Psychol Health Med. 2014;19(3):286–295.
- Ghaffarifar S, Ghofranipour F, Ahmadi F, et al. The causal relationship between interns’ knowledge and self-efficacy and their value in predicting the interns’ communication behavior with patients. Int J Community Based Nurs Midwifery. 2015;3(4):263–271.
- Pittet D, Simon A, Hugonnet S, et al. Hand hygiene among physicians: performance, beliefs, and perceptions. Ann Intern Med. 2004;141(1):1–8.
- Childs S, Blenkinsopp E, Hall A, et al. Effective e-learning for health professionals and students–barriers and their solutions. A systematic review of the literature–findings from the HeXL project. Health Information & Libraries J. 2005;22(s2):20–32.
- Noesgaard SS, Ørngreen R. The effectiveness of e-learning: an explorative and integrative review of the definitions, methodologies and factors that promote e-learning effectiveness. Electron J e-Learning. 2015;13:278–290.
- Steenbeek R. LAD vragenlijstonderzoek gezond en veilig werken tijdens en na de COVID-19 uitbraak [LAD questionnaire working healthy and safely during and after the COVID-19 outbreak]. Utrecht: Landelijke Vereniging van Artsen in Dienstverband (LAD); 2020. Available from: https://www.lad.nl/wpcontent/uploads/2020/10/Rapportage-LAD-vragenlijstonderzoek-Gezond-en-Veilig-werkentijdens-en-na-COVID-19-DEF.pdf
- Mohr DC, Spring B, Freedland KE, et al. The selection and design of control conditions for randomized controlled trials of psychological interventions. Psychother Psychosom. 2009;78(5):275–284.
- Schaafsma F, Hulshof C, Van Dijk F, et al. Information demands of occupational health physicians and their attitude towards evidence-based medicine. Scand J Work Environ Health. 2004;30(4):327–330.
- Upton D, Stephens D, Williams B, et al. Critical review introduction occupational therapists’ attitudes, knowledge, and implementation of evidence-based practice: a systematic review of published research. Br J Occup Ther. 2014;77(1):24–38.
