Abstract
Purpose
Physical activity (PA) levels in older care home residents are low. This has detrimental effects on health. Little is known about the nature of interventions to increase physical activity in this population.
Methods
A scoping review to: (1) identify and describe interventions to increase PA in older care home residents, and (2) describe the extent to which interventions address care home context, systemised by social–ecological models. We systematically searched databases for peer-reviewed intervention studies to increase PA in older people resident in care homes. Data were extracted using the template for intervention description and replication (TIDieR) and mapped against a social–ecological framework to locate the intervention focus.
Results
The 19 included studies consisted of interventions tested in randomised or quasi-experimental trial designs. Interventions consisted of single or multiple components and predominantly addressed individual resident level factors (such as muscle strength) rather than broader social and environmental aspects of context. Interventions were not all fully described. For most interventions a distinct theoretical foundation was not identified. Interventions were mostly delivered by health professionals and research staff external to care homes.
Conclusions
Future interventions should address contextual care home factors and should be clearly described according to intervention description guidance.
Physical activity holds promise as an effective means of improving health and function in older care home residents, but physical activity levels in this population are low.
Several reasons beyond the individual resident but related to care home contextual factors may explain low PA in care homes
To date, contextual factors influencing PA in care homes have been poorly addressed in interventions.
Wider care home context (social, cultural, and environmental factors) must be considered in future interventions.
Implications for rehabilitation
Introduction
Care homes provide accommodation, personal care and support, and/or onsite nursing care for people who can no longer live independently in their own homes [Citation1]. Admission to a care home is often associated with further functional and health decline and associated adverse outcomes such as increased mortality and reduced quality of life [Citation2]. Importantly, care home residents’ engagement in physical activity (PA)—defined as “any bodily movement produced by skeletal muscle that requires energy expenditure” [Citation3]—has consistently been shown to be low [Citation4–7]. Estimates for PA levels range from 79% [Citation5] to 92% [Citation4] of daytime hours spent physically inactive.
Evidence from systematic reviews indicates that low levels of PA are associated with a high risk of adverse outcomes in care home residents with pressure sores, joint contractures, decreased cardiovascular function, and urinary infections all reported [Citation8]. However, it is increasingly recognised that multimorbidity alone does not account for declines in health and function of older adults [Citation9]. Consequently, sarcopenia—defined as the progressive loss of muscle mass and function [Citation10]—has been identified as an important muscle disorder that is a powerful predictor of adverse health outcomes in older people, independent of clinical disease [Citation11–13]. The prevalence of sarcopenia in the care home population is estimated to be as high as 85% [Citation14], with physical inactivity identified as a major risk factor for the development of sarcopenia [Citation15].
Crucially, low levels of PA are associated with the development of frailty [Citation16]. There are generally two ways of defining frailty; the phenotype model [Citation13] and the deficit accumulation model [Citation17]. The phenotype model defines physical frailty as reduced reserve capacity which can be expressed as weight loss, exhaustion, weakness, slowness, and reduced physical activity [Citation13]. The deficit accumulation model is defined more broadly as an increased risk of adverse outcomes as a result of older peoples’ reduced ability to respond to stress because of the accumulation of multiple deficits [Citation17,Citation18]. As such, frailty can be assessed by considering an individual’s morbidities, extent of physical frailty, and dependence in activities of daily living [Citation17,Citation19]. Given this broad definition, the vulnerability of older care home residents to developing frailty [Citation20], and the association between low PA and frailty [Citation16], it is therefore important to explore ways of increasing PA levels in care home residents.
As well as physical benefits of PA, wider psychosocial benefits are also reported in terms of slowing cognitive decline [Citation21] and improvements in behaviour, mood, and sleep [Citation22–24]. Systematic review evidence of interventions to increase PA reports short and medium term improvements in clinically relevant outcomes in older people with depression [Citation25]. In addition, PA has been shown to mitigate impairment in domains of cognition, and psychological health in older people with mild cognitive impairment and dementia [Citation26,Citation27], and is therefore recommended for older people across a range of settings, including in care homes [Citation26].
Several reasons beyond the individual resident but related to care home contextual factors may explain low PA in care homes [Citation28]. First, organisational culture in care homes may influence PA. Organisational culture in care homes is often defined by rules, procedures, and entrenched social norms [Citation29] and may leave little room for latitude or spontaneity, thus reducing PA opportunity [Citation30]. Care home staff may not adopt standalone interventions that aim to increase levels of PA for reasons that include perceived risk to the resident, low belief in their utility, insufficient training and support, workload concerns, and high staff turnover [Citation31]. Changes to work practices are often short-lived because staff often revert to previous habits [Citation31,Citation32]. Pervasive care home routines and negative attitudes to PA among staff and residents may negate an emphasis on promoting PA [Citation33]; however, recent evidence suggests that with carefully designed interventions, it is possible to effect behaviour change among care home staff [Citation34]. For example, recent evidence shows that behaviour change interventions directed at care home staff can improve pressure ulcer management [Citation35] and resident-staff engagement [Citation36]. However, such interventions in care homes require organisational change, capacity for innovation, and ongoing monitoring to maintain changes in practice [Citation37]. Consequently, changing the culture in care homes to one that privileges PA is challenging since care homes with stretched resources may have little capacity to initiate changes that take up carers’ time [Citation38]. Furthermore, there is increasing evidence that the physical environment in care homes may influence the amount of PA undertaken by residents [Citation22,Citation39]. It is therefore evident that residents face a range of complex and multifaceted barriers that need to be considered if understanding of PA in care homes is to advance.
Multiple influences on health behaviour, such as those described above, are captured by social–ecological models (SEMs), a framework that aims to foster understanding of a range of contextual factors that impact individual’s health and related behaviour [Citation40]. SEMs are based on the premise there are multiple levels of influence that drive behaviour including intrapersonal factors (for example, knowledge, attitudes, or beliefs), interpersonal factors (for example, interactions from family, peers, or social networks), social factors (for example, norms and standards), environmental factors (for example, the built environment) and policy factors (for example, regulations and programmes to support healthy decisions) [Citation41–43]. Consequently, to understand behaviour and to develop strategies to increase PA in care homes, it therefore seems necessary to consider not only the individual and their immediate context, but also wider interpersonal interactions and environmental aspects [Citation44,Citation45]. Therefore, a social–ecological approach to increasing PA would ideally target multiple levels to create care home environments conducive to PA. Despite the importance of considering of the influence of context on PA in care homes, it is unclear how previous interventions to promote PA in care homes have been informed by a comprehensive approach that accounts for multiple levels of context. Such an approach may inform sustainable strategies to increase PA levels in care homes.
The present scoping review emerged from the need to map the nature and range of interventions to increase PA in care homes and to identify which SEM levels have been addressed, and which require further investigation. Therefore, the objectives of this review were (1) to identify the nature and range of interventions to increase PA in care homes and (2) to determine the extent to which interventions addressed care home contextual factors at social–ecological levels.
Methods
Overview
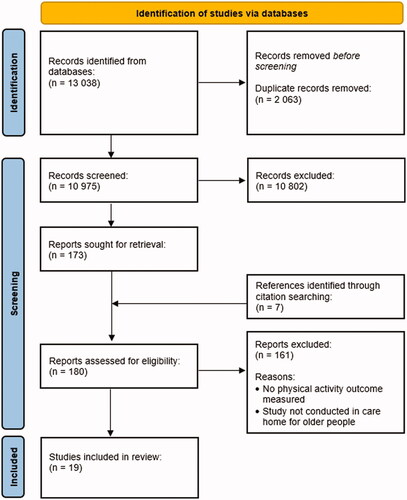
A scoping review methodology was chosen because the objectives of the review were to identify knowledge gaps and map the current body of literature [Citation46]. Furthermore, scoping reviews allow the inclusion of different study types, thus allowing the inclusion of multiple study types, for example, randomised controlled trials (RCTs) and quasi-experimental studies. The review follows the stages outlined in the relevant scoping review guidance [Citation47–49]. The methods and results are reported in line with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews (PRISMA-ScR) checklist [Citation50] (see ).
Table 1. Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) checklist.
Identify the research question
The scoping review question was developed from the need to identify interventions to increase PA in care homes for older people and to explore how context, operationalised at different SEM levels, has been targeted interventions. Two questions were developed for the review:
What is the nature and range of interventions to increase physical activity in care homes (in terms of intervention characteristics, recipients, delivery, theoretical basis, and outcome measures)?
Which SEM level influences on PA in care homes have been targeted by interventions?
Identifying relevant studies
Eligibility criteria
To be included, articles had to focus on the concept of PA within care homes and have PA as an outcome measure, measured either through self-report questionnaires, activity logs, direct observation, or accelerometery. For this review, PA was defined as: any bodily movement that results in energy expenditure [Citation3]. For a study to be included, participants’ mean age had to be over 65 years of age. Participants had to be permanently resident in a care home. Included studies were set in care homes that provide either personal care (for example, washing and dressing), or nursing care (for example, wound care, pressure ulcer management), or a combination of personal and nursing care. No restriction was placed on geographical location. Studies examining interventions aimed at staff, family members, and other members of the resident’s social network were included.
Intervention studies published after 2000 and in English language were included. The date limit was set to include only the most recent literature to ensure that the included studies reflect the contemporary care home context, thus ensuring relevance. The language limit was set because it was felt that resources required for translation would be unlikely to enhance the output of the review.
Clinical commentaries, grey literature, editorials, or other publications with no data were excluded. Studies without an intervention were excluded. Evidence syntheses of any type were excluded; however, their reference lists were checked for relevant studies. Studies involving residents of supported or sheltered housing complexes were excluded. This is because supported or sheltered housing allows older people to live more independently compared to care homes for older people and therefore have different populations and organisation of care.
Search strategies and databases
Systematic searches for peer-reviewed literature were conducted in the following databases: Allied and Complementary Medicine (AMED), Cumulative Index to Nursing and Allied Health Literature (CINAHL), Embase, MEDLINE, and PsychINFO. Databases were searched from 2000 to 24 December 2021. Searches were limited to English language with full-text availability (see Supplemental Materials).
The search strategy used free-text and indexing terms to capture studies that investigated the following concepts: long-term care facilities (both residential and nursing care), physical activity, and physical activity interventions. Search terms within each concept were combined with the Boolean operator OR, and the concepts were then combined with the Boolean operator AND. Truncation was used where required to ensure comprehensive results. Hand searching of reference lists of retrieved studies was conducted.
Study selection
One researcher (GW) screened all retrieved titles and abstracts and applied the inclusion and exclusion criteria and decided on inclusion. One other reviewer (MW) independently screened the abstracts. Decisions were compared, and in cases of disagreement, a third reviewer (TK) adjudicated. Reviewer meetings were held throughout the review process to discuss uncertainties relating to study selection and to further refine the search strategy if required. The reference lists of any identified reviews were checked for relevant primary studies to include. Additionally, scoping reviews are intended to provide a map of what evidence has been produced, rather than seeking only the best available evidence to answer a narrow question [Citation51].
Methodological quality appraisal
The methodological quality of the included articles was assessed using the Mixed Methods Assessment Tool (MMAT) [Citation52]. The MMAT is a widely used tool for the quality appraisal of multiple study types and so is well-suited as a valid indicator of methodological quality for the present scoping review [Citation52,Citation53]. Importantly, the MMAT does not generate a single global score; rather the MMAT presents a detailed rating of each criterion to better inform the quality of the included studies [Citation54]. One reviewer (GW) assessed the quality of the included studies. In line with the exploratory nature of scoping reviews, studies were not excluded based on quality assessment.
Extracting and charting the data
A draft data charting form was developed and piloted with three reviewers (GW, MW, and TK). The form was based on an established and published framework for intervention description [Citation55]. One reviewer (GW) independently extracted and charted the data from all included studies. The following data (where available) were extracted from the included studies: intervention description and content described as per the template for intervention, description, and replication (TIDieR) framework [Citation55], author, year of publication, geographical location of study, study design, levels(s) of SEM addressed by the study, and results.
Included studies were screened to identify the level(s) of the SEM addressed by the interventions. The SEM level was identified according to descriptions of levels drawn from the ecological perspective on health promotion programs [Citation56] and the model for active living communities [Citation44]. Descriptions for each level of the SEM as applied to care homes for older people are provided in .
Table 2. Definitions of each social–ecological level used for the review.
Collating, synthesising, and reporting the results
A narrative thematic summary was conducted describing how the identified research relates to the review objectives and questions [Citation57]. The results of the included studies were organised to describe patterns in terms of outcome measures, intervention characteristics and the effects reported. The types of interventions were sorted and presented according to their main characteristic (for example, behavioural intervention or environmental modification) including the social–ecological level(s) where the intervention operated.
Results
Overview of included studies
The flow of studies through the quantitative review is shown in . The search yielded a total of 10 975 non-duplicate citations, from which 173 studies were deemed as being potentially relevant and were reviewed in full. Seven studies were identified through reference searching. One hundred sixty-one studies were excluded following full-text review. Nineteen studies were included in the final review; 10/19 (53%) were randomised controlled trials [Citation58–67]; Two of these were cluster RCTs [Citation59,Citation67]; 9/19 (47%) were quasi-experimental designs [Citation68–76]. Of the quasi-experimental studies, 3/19 (%) were exploratory pilot feasibility studies [Citation68,Citation69,Citation76]. Included studies were all from high income countries with the majority from the USA: USA 6/19 (32%); Spain 2/19 (11%); Netherlands 2/19 (11%); UK 2/19 (11%); Australia 2/19 (11%); Scandinavia 1/19 (5%), China 1/19 (5%); Portugal 1/19 (5%); Belgium 1/19 (5%); and Poland 1/19 (5%). The search results indicated a trend toward an increasing number of intervention studies to increase physical activity in care homes over time. In total, the intervention studies provided data on 2 445 care home residents. The mean age of the participants was 85 years [SD = 8.25]. In terms of age and sex profile (mean age >80, majority female) the sample characteristics of the participants enrolled into these studies were representative of older care home residents [Citation77].
Figure 1. PRISMA flow diagram.
Eleven studies (58%) (12 papers) evaluated interventions to increase physical activity using randomised controlled trial designs [Citation58–67,Citation76,Citation78]. Eight studies (42%) (eight papers) evaluated interventions using quasi-experimental designs [Citation68–75]. Of the quasi-experimental designs, two were single group repeated measures design [Citation69,Citation72], three were pre- and post-test design [Citation68,Citation70,Citation74], two were a prospective longitudinal studies with an experimental design [Citation71,Citation75], and one was an unspecified quasi-experimental design [Citation73]. Three studies (four papers) measured PA as a secondary outcome [Citation60,Citation61,Citation65,Citation74]. provides an overview of the included intervention studies.
Table 3. Overview of characteristics of intervention studies.
Quality review
We applied the Mixed Methods Assessment Tool [Citation52] (see Supplemental Materials). In 6/10 (60%) RCTs, there was a clear statement on whether or not participants competed the assigned intervention as planned [Citation58,Citation59,Citation63,Citation64,Citation66,Citation78]. One of these RCTs conducted a detailed process evaluation to explore reasons for participant non-completion [Citation78]. In 3/9 (33%) quasi-experimental studies, the intervention was delivered as intended [Citation69,Citation70,Citation72]. In one RCT, there were differences between the intervention and control groups at baseline; in addition, it was not possible to determine whether the outcome assessors were blinded to participant allocation [Citation65].
It was unclear if quasi-experimental studies accounted for confounders in their analyses. In 5/9 (56%) quasi-experimental studies and 4/10 (40%) RCTs, data were either incomplete, or the completeness of the data were unclear. For the purposes of this review, incomplete outcome data were defined as at least 80% of the planned outcome data available at the study end point [Citation54]. Incomplete data was due to study attrition such as participant withdrawal from the study or loss to follow-up. In studies with missing data, methods of imputation were applied in three studies [Citation59,Citation66,Citation67]. In the quasi-experimental studies, with three exceptions [Citation69,Citation70,Citation72], there was overall lack of clarity on the extent to which participants adhered to the intervention or if interventions were delivered as described in study reports.
Intervention characteristics
The following sections describe the nature and range of interventions according to research question one, with research question two addressed in the final section. Each intervention is described according to the items on the checklist contained in the Template for Intervention Description and Replication (TIDieR guidelines) where it was possible to extract these [Citation55] (see ). The review identified a range of interventions that were aimed at improving PA in care home residents. Interventions could be categorised as either single-component or multifaceted interventions. For this review, we defined single-component interventions as those addressing a single barrier to PA [Citation79]. Multifaceted interventions were defined as any intervention including two or more components [Citation79,Citation80]. Single interventions were either behavioural or exercise interventions, whereas multifaceted interventions included combinations of behavioural interventions, exercise, interventions that included the provision of fluids and snacks, or environmental interventions to modify the social, organisational, or physical environment.
Table 4. Template for intervention description and replication (TIDieR) for the included studies.
Single-component interventions were: resistance training [Citation58,Citation60–62,Citation66,Citation75]; functional skills training [Citation62]; reinforcement of social norms in terms of physical activity [Citation76]; a behavioural intervention to reduce PA as an intervention to limit the behavioural and psychological symptoms of dementia [Citation67]; video game based exercise intervention [Citation73]; aerobic training [Citation71]; strength training [Citation71,Citation75]; health education programme [Citation71]; and modification of the care home environment [Citation72]. One intervention was contrary to the aim of all other included studies in that it aimed to reduce PA in the context of limiting behavioural and psychological symptoms of dementia (BPSD) through use of a plush robotic toy [Citation67].
Multicomponent interventions were: resistance training combined with functional skills training [Citation62,Citation66]; goal setting combined with progressive and tailored physical and daily activities [Citation64]; environmental and policy assessment, education, goal setting, and behavioural change techniques aimed at mentoring and motivating staff and residents [Citation59,Citation63,Citation68,Citation69,Citation78]; goal setting, information provision, exercise provision [Citation70]; toileting assistance, exercise, and choices of food and fluid snacks [Citation65]; and incontinence care combined with exercise [Citation74].
Completeness of intervention description was determined by the extent of adherence to the TIDieR checklist [Citation55] (). Overall, the standard of reporting of the intervention details was varied, with many failing to detail specific materials required or failing to provide details of information contained in training manuals/handouts. However, one study did provide intervention details in the TIDieR format [Citation68], with another study providing extensive detail on the intervention in study appendices [Citation78]. One study [Citation70] provided an internet link to further intervention details, but the link provided was not persistent and could not be accessed.
Intervention recipients
Thirteen of the nineteen (13/19; 68%) studies targeted their intervention directly to care home residents. One study [Citation64] which investigated exercise plus behavioural interventions, had residents and staff as the recipients of the intervention. Four studies targeted care home staff but not residents directly [Citation59,Citation63,Citation69,Citation78].
Intervention delivery
Seven of the nineteen (7/19; 37%) studies had the intervention delivered by a member of the research team conducting the study [Citation65,Citation67,Citation70,Citation72–74,Citation76]. Four of the nineteen (4/19; 21%) studies deployed research nurses to train care home staff to deliver the deliver the intervention [Citation59,Citation63,Citation69,Citation78]. In several studies, the intervention was delivered by qualified health professionals such as physiotherapists, trained instructors, or exercise professionals that were external to the care home, but recruited by the research team [Citation58,Citation60–62,Citation64,Citation66,Citation68,Citation71,Citation75].
Cognitive and physical characteristics of participants
Participant’s cognitive ability was provided in 9/19 (53%) studies, with the Mini-Mental State Exam (MMSE) used exclusively as a measure of cognitive ability. The mean MMSE ranged from 3.2 [Citation69] to 26.1 [Citation75]. Of the studies that had MMSE data available, most scores were suggestive of dementia in their samples (mean MMSE score of all studies <24) [Citation59,Citation63–65,Citation69,Citation72,Citation74,Citation75]. One study’s mean MMSE score suggested preserved cognitive function (>24/30) [Citation71].
Where physical performance data were reported, the approach to reporting was heterogeneous, and included self-reported PA levels, timed-up-and-go test, functional ambulation category (FAC), physical activity scale in long-term care (PAS-LTC) measure, and the six-minute walk test. Two studies did not report any physical characteristics of their participants [Citation65,Citation74]. Overall, heterogeneity of reporting physical performance characteristics made it challenging to compare between studies.
Outcome measures
Across the included studies there were direct and indirect approaches to measuring PA. Accelerometery was the most widely used direct measure of physical activity, and was used in 13/19 (68%) studies [Citation58,Citation59,Citation62,Citation63,Citation65–67,Citation69,Citation71,Citation72,Citation74,Citation75,Citation78]. One study (two papers) used Pedometers as a direct measure of PA [Citation60,Citation61]. Indirect subjective methods of measuring PA were the Nursing Home Life Space Diameter measure [Citation64], the Rapid Assessment of Physical Activity Measure (RAPA) [Citation73], the International Physical Activity Questionnaire (IPAQ) [Citation70], the Assessment of Physical Activity [Citation68] and the Physical Activity Scale for Long-term Care [Citation72].
Theories and models as a basis for intervention
The theoretical basis for the interventional studies were explicit in 6/19 (32%) of included studies. Theories and models explicitly represented were: evolutionary—biological theory [Citation62], SEM [Citation59,Citation63,Citation72], social-cognitive theory [Citation59,Citation69], self-determination theory [Citation75] and health promotion model [Citation70].
Congruence of the included studies with social–ecological models
Eighteen of the nineteen (18/19; 95%) studies addressed the intrapersonal level of the SEM either alone or in combination with other levels. Fourteen of the nineteen (14/19; 74%) interventions (15 papers) addressed the intrapersonal level of the SEM alone, meaning that the interventions focussed on individual-level change for residents, but did not factors that influence PA levels through changes to the wider care home context [Citation58,Citation60–65,Citation67,Citation69–71,Citation73–76]. Few studies were located that addressed the physical environment, either alone or in combination with other levels of the SEM (N = 4). Similarly, few studies were located that addressed organisational-level factors as part of the intervention (N = 4).
Most interventions addressing the intrapersonal level alone. Studies that addressed four or all levels of the SEM simultaneously were in a minority (N = 2). One UK study addressed the intrapersonal, interpersonal, organisational, and policy levels of the SEM simultaneously [Citation78]. One study from the USA addressed the intrapersonal, interpersonal, policy, and perceived physical environment levels. One cluster RCT from the USA and one small feasibility study from the UK (that was not designed to determine effectiveness) addressed all levels of the SEM simultaneously [Citation63,Citation68].
Discussion
This present scoping review sought to examine the nature and range of interventions to increase physical activity in care homes. In addition, the review systematically examined how (or if) interventions addressed the wider care home context through levels of influencing factors on PA that are highlighted by SEMs [Citation44]. Despite repeated calls from previous reviews [Citation22,Citation32,Citation81,Citation82] for interventions to address multiple levels of context, the present scoping review found that individual-level factors alone (for example, muscle strength) were predominantly addressed in interventions rather than wider aspects of context such as organisational culture or the physical environment. Encouragingly more recent studies considered wider aspects of care home context [Citation63,Citation68,Citation78].
One study reported an intervention designed to reduce PA levels in the context of managing the behavioural and psychological symptoms of dementia [Citation67]. The results from this study suggest that interventions to reduce BPSD may involve decreasing PA, which may have negative consequences on the health of care home residents. In addition, the results from that study also run contrary to the prevailing view that wandering behaviours as part of BPSD are not necessarily negative or unwanted [Citation83–86].
Intervention studies were often characterised by the delivery of time-limited activities delivered by staff external to care homes. External staff were either those from research teams conducting the study, or external health professionals (for example, physiotherapists). This may be because care homes did not have the necessary resources to allow their own staff time to be trained in the delivery of interventions. Long-term delivery of strategies to increase PA in care homes by staff external to care homes, such as registered health professionals or research staff, may not be feasible or sustainable particularly if funding for the delivery of programs is limited [Citation38]. Furthermore, it is possible that a delivery model reliant on staff external to care homes—whilst deliverable in a research context—may not be sustainable beyond the life cycle of a research project. This is problematic for the long-term sustainability of the intervention because for interventions to be sustainable beyond the study period, they need to be embedded into usual-care home work practices, rather than added to existing care home routines [Citation34]. One approach may be to have interventions delivered by care home staff that are already embedded in care homes—those staff who look after residents on daily basis. Such an approach may well enhance the sustainability of interventions beyond a research study. Therefore, the results from the present review partly explain the uncertainty around the sustainability of interventions to increase PA in care homes highlighted by previous work [Citation8].
The role of the physical and social environments are critical in creating opportunity for PA in a way that is embedded in everyday life and may be another way of ensuring the sustainability of interventions. Such an approach allows residents to do what they wish and at the same time move around without necessarily relying direct delivery of intervention activities from staff to residents. The role of social and physical environments are central in facilitating such an approach [Citation87]. Additionally, interventions to address social and physical environments with the aim of increasing PA may have the capacity to reach many residents at once, with evidence suggesting that environmental adaptations to enhance residents’ perceptions of walkability in care homes may increase PA levels [Citation88].
The results from this scoping review build on those of other reviews by highlighting gaps in most intervention strategies to increase PA in care homes. For example, a previous review highlighted barriers for PA in care homes at resident (for example, health status), physical environment (for example, accessibility), and organisational (for example, funding constraints and staffing) levels [Citation32]. Furthermore, another systematic review that focussed on the physical environment found that positive effects on PA were found for small home-like environments and modifications to the physical environment to accommodate residents’ functional limitations [Citation22]. Such wider influencing factors were least addressed by the included studies in the present review.
Several methodological and reporting issues in the included studies require comment. First, future studies need to be more comprehensive in their descriptions of the context in which studies have been undertaken; SEMs may provide a useful framework to address such contextual factors [Citation89]. Secondly, most interventions have been tested with populations that are not as cognitively impaired as most of the care home population. Interventions are therefore needed that address PA levels in cognitively impaired older people. Third, just under half of the studies did not include a control group. Fourth, with four exceptions [Citation58,Citation59,Citation63,Citation78] interventions were trialled in a single centre, leading to interventions that may not be implementable elsewhere. Fifth, there was limited detail provided on care homes where interventions were delivered, making it difficult to know where and when effective interventions to enhance PA levels are best delivered. Finally, intervention description was not consistently clear in the study reports. We were guided by the Template for Intervention Description and Replication (TIDiER) to extract data pertaining to intervention description [Citation55]. With three exceptions [Citation59,Citation68,Citation78] studies did not adhere to current reporting guidelines, with descriptions that were insufficient to facilitate replication. This may be largely attributable to the fact that many of the studies included in this review pre-date intervention description checklists which have since become commonplace [Citation55]. Importantly, the implication is that without sufficient intervention description (for example, lack of training manuals) then it will be difficult—if not impossible—for others to implement an intervention in practice. The results suggest that the quality of reporting has seen improvements in more recent studies, and future work should continue to adhere to reporting guidelines for interventions descriptions.
Most intervention studies were carried out in the USA. This may represent bias in favour of studies published in the USA within the databases that were searched but may also be a result of the inclusion criteria for this review, which restricted inclusion to English language studies only. Conclusions on international generalisability of the findings of these intervention studies may not possible since it could not be ascertained that the settings, populations, and interventions were similar in any way to the UK context. Nonetheless, this review provides an international snapshot of the current evidence for interventions to increase PA in care homes.
Limitations of the review
First, although scoping reviews are comprehensive, they are not exhaustive in identifying literature [Citation90]. In addition, although few studies were located where the focus was at higher levels of SEMs and many lacked a theoretical foundation other than individual-level models. This may be because the search resulted in quasi-experimental and RCT studies rather than policy interventions which may limit the extent to which strategies influenced higher levels of SEMs. Therefore, despite a comprehensive search strategy, not all relevant publications may have been identified. However, the search strategy recognised the balance between the breadth and depth of the analysis.
Care home residents are a different population to community dwelling older people in ways that will likely influence their ability to participate in PA. However, it was difficult to identify confounding factors that may influence intervention effectiveness (for example, functional status, cognitive ability, or care home characteristics). Nonetheless attempts were made throughout the design and conduct of the study to appraise and report these in a rigorous way. Although it may have been useful to conduct further analysis to explore how levels of the SEM were addressed by geography, there was not sufficient geographical variation for meaningful analysis. Finally, although some studies detailed methods to assess the fidelity of the intervention such as diaries, data are lacking on how that data were used since the extent of fidelity was often not reported. It is therefore unclear if residents and staff adhered to the interventions provided, and for how long.
Conclusion
Most interventions addressed individual-level influences on PA, and it is important to acknowledge that they alone cannot address the issue of low PA in care homes. Although there is evidence emerging from studies of interventions that address multiple levels of SEM simultaneously, that evidence remains scant. Future interventions should account for care home context through the development of interventions that address multiple levels of the SEM simultaneously. In addition, future interventions should be clearly described according to intervention description guidance.
Supplemental_material.docx
Download MS Word (19.4 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Goodman C, Dening T, Gordon AL, et al. Effective health care for older people living and dying in care homes: a realist review. BMC Health Serv Res. 2016;16(1):14.
- Luppa M, Luck T, Weyerer S, et al. Prediction of institutionalization in the elderly. A systematic review. Age Ageing. 2010;39(1):31–38.
- Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. 1985;100(2):126–131.
- den Ouden M, Bleijlevens MHC, Meijers JMM, et al. Daily (in)activities of nursing home residents in their wards: an observation study. J Am Med Dir Assoc. 2015;16(11):963–968.
- Barber SE, Forster A, Birch KM. Levels and patterns of daily physical activity and sedentary behavior measured objectively in older care home residents in the United Kingdom. J Aging Phys Act. 2015;23(1):133–143.
- De Souto Barreto P, Demougeot L, Vellas B, et al. How much exercise are older adults living in nursing homes doing in daily life? A cross-sectional study. J Sports Sci. 2015;33(2):116–124.
- Gustavsson M, Liedberg GM. Larsson Ranada Å. Everyday doings in a nursing home – described by residents and staff. Scand J Occup Ther. 2015;22:1–7.
- Crocker T, Forster A, Young J, et al. Physical rehabilitation for older people in long-term care. Cochrane Database Syst Rev. 2013; 2:CD004294.
- Keevil VL, Romero-Ortuno R. Ageing well: a review of sarcopenia and frailty. Proc Nutr Soc. 2015;74(4):337–347.
- Patel HP, Syddall HE, Jameson K, et al. Prevalence of sarcopenia in community-dwelling older people in the UK using the European working group on sarcopenia in older people (EWGSOP) definition: findings from the Hertfordshire cohort study (HCS). Age Ageing. 2013;42(3):378–384.
- Moore SA, Hrisos N, Errington L, et al. Exercise as a treatment for sarcopenia: an umbrella review of systematic review evidence. Physiotherapy. 2020;107:189–201.
- Landi F, Liperoti R, Fusco D, et al. Sarcopenia and mortality among older nursing home residents. J Am Med Dir Assoc. 2012;13(2):121–126.
- Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–56.
- Zhang X, Wang C, Dou Q, et al. Sarcopenia as a predictor of all-cause mortality among older nursing home residents: a systematic review and meta-analysis. BMJ Open. 2018;8(11):e021252–10.
- Steffl M, Bohannon RW, Sontakova L, et al. Relationship between sarcopenia and physical activity in older people: a systematic review and meta-analysis. Clin Interv Aging. 2017;12:835–845.
- Da Silva VD, Tribess S, Meneguci J, et al. Association between frailty and the combination of physical activity level and sedentary behavior in older adults. BMC Public Health. 2019;19(1):1–6.
- Rockwood K, Mitnitski A. Frailty defined by deficit accumulation and geriatric medicine defined by frailty. Clin Geriatr Med. 2011;27(1):17–26.
- Morley JE, Vellas B, van Kan GA, et al. Frailty consensus: a call to action. J Am Med Dir Assoc. 2013;14(6):392–397.
- Rockwood K, Mitnitski A. Frailty in relation to the accumulation of deficits. J Gerontol A Biol Sci Med Sci. 2007;62(7):722–727.
- Kojima G. Prevalence of frailty in nursing homes: a systematic review and meta-analysis. J Am Med Dir Assoc. 2015;16(11):940–945.
- Satariano WA, McAuley E. Promoting physical activity among older adults: from ecology to the individual. Am J Prev Med. 2003;25(3):184–192.
- Anderiesen H, Scherder EA, Goossens RHM, et al. A systematic review - physical activity in dementia: the influence of the nursing home environment. Appl Ergon. 2014;45(6):1678–1686.
- Peterson MJ, Giuliani C, Morey MC, et al. Physical activity as a preventative factor for frailty: the health, aging, and body composition study. J Gerontol A Biol Sci Med Sci. 2009;64(1):61–68.
- Vogel T, Brechat P-H, Leprêtre P-M, et al. Health benefits of physical activity in older patients: a review. Int J Clin Pract. 2009;63(2):303–320.
- Blake H, Mo P, Malik S, et al. How effective are physical activity interventions for alleviating depressive symptoms in older people? A systematic review. Clin Rehabil. 2009;23(10):873–887.
- Nuzum H, Stickel A, Corona M, et al. Potential benefits of physical activity in MCI and dementia. Behav Neurol. 2020;2020:1–10.
- Booth V, Harwood RH, Hood-Moore V, et al. Promoting activity, independence and stability in early dementia and mild cognitive impairment (PrAISED): development of an intervention for people with mild cognitive impairment and dementia. Clin Rehabil. 2018;32(7):855–864.
- Panter J, Guell C, Prins R, et al. Physical activity and the environment: conceptual review and framework for intervention research. Int J Behav Nutr Phys Act. 2017;14(1):1–13.
- Nakrem S. Understanding organizational and cultural premises for quality of care in nursing homes: an ethnographic study. BMC Health Serv Res. 2015;15:508.
- Benjamin K, Edwards N, Guitard P, et al. Factors that influence physical activity in long-term care: perspectives of residents, staff, and significant others. Can J Aging. 2011;30(2):247–258.
- Resnick B, Petzer-Aboff I, Galik E, et al. Barriers and benefits to implementing a restorative care intervention in nursing homes. J Am Med Dir Assoc. 2008;9(2):102–108.
- Benjamin K, Edwards N, Ploeg J, et al. Barriers to physical activity and restorative care for residents in long-term care: a review of the literature. J Aging Phys Act. 2014;22(1):154–165.
- Schnelle JF, Cruise PA, Rahman A, et al. Developing rehabilitative behavioral interventions for long-term care: technology transfer, acceptance, and maintenance issues. J Am Geriatr Soc. 1998;46(6):771–777.
- Low LF, Fletcher J, Goodenough B, et al. A systematic review of interventions to change staff care practices in order to improve resident outcomes in nursing homes. PLoS One. 2015;10(11):e0140711–e0140760.
- Lavallée JF, Gray TA, Dumville JC, et al. Preventing pressure injury in nursing homes: developing a care bundle using the behaviour change wheel. BMJ Open. 2019;9(6):e026639.
- Hartmann CW, Mills WL, Pimentel CB, et al. Impact of intervention to improve nursing home resident-staff interactions and engagement. Gerontologist. 2018;58(4):e291–e301.
- Keenan J, Poland F, Manthorpe J, et al. Implementing e-learning and e-tools for care home staff supporting residents with dementia and challenging behaviour: a process evaluation of the ResCare study using normalisation process theory. Dementia. 2020;19(5):1604–1620.
- Ellard DR, Thorogood M, Underwood M, et al. Whole home exercise intervention for depression in older care home residents (the OPERA study): a process evaluation. BMC Med. 2014;12:1.
- Moran M, Van Cauwenberg J, Hercky-Linnewiel R, et al. Understanding the relationships between the physical environment and physical activity in older adults: a systematic review of qualitative studies. Int J Behav Nutr Phys Act. 2014;11:79.
- Richard L, Gauvin L, Raine K. Ecological models revisited: their uses and evolution in health promotion over two decades. Annu Rev Public Health. 2011;32:307–326.
- Moore GF, Evans RE. What theory, for whom and in which context? Reflections on the application of theory in the development and evaluation of complex population health interventions. SSM Popul Health. 2017;3:132–135.
- Golden SD, McLeroy KR, Green LW, et al. Upending the social ecological model to guide health promotion efforts toward policy and environmental change. Heal Educ Behav. 2015;42:8–14.
- Bauman AE, Reis RS, Sallis JF, et al. Correlates of physical activity: why are some people physically active and others not? Lancet. 2012;380(9838):258–271.
- Sallis JF, Cervero RB, Ascher W, et al. An ecological approach to creating active living communities. Annu Rev Public Health. 2006;27:297–322.
- Green LW, Richard L, Potvin L. Ecological foundations of health promotion. Am J Health Promot. 1996;10(4):270–281.
- Munn Z, Peters MDJ, Stern C, et al. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):1–7.
- Peters MDJ, Godfrey CM, Khalil H, et al. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc. 2015;13(3):141–146.
- Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
- Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5:69.
- Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–473.
- Colquhoun HL, Levac D, O’Brien KK, et al. Scoping reviews: time for clarity in definition, methods, and reporting. J Clin Epidemiol. 2014;67(12):1291–1294.
- Hong QN, Fàbregues S, Bartlett G, et al. The mixed methods appraisal tool (MMAT) version 2018 for information professionals and researchers. EFI. 2018;34(4):285–291.
- Murray RM, Conroy E, Connolly M, et al. Scoping review: suicide specific intervention programmes for people experiencing homelessness. Int J Environ Res Public Health. 2021;18(13):6729.
- Hong QN, Pluye P, Fàbregues S, et al. Mixed methods appraisal tool (MMAT), version 2018. User guide. Canada: McGill University; 2018.
- Hoffmann TC, Glasziou PP, Boutron I, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ. 2014;348:g1687.
- McLeroy KR, Bibeau D, Steckler A, et al. Ecological perspective on promotion programs. Health Educ Q. 1988;15(4):351–377.
- Popay J, Roberts H, Sowden A, et al. Guidance on the conduct of narrative synthesis in systematic reviews. A product from the ESRC methods programme Version. 2006;1(1):b92.
- Arrieta H, Rezola-Pardo C, Zarrazquin I, et al. A multicomponent exercise program improves physical function in long-term nursing home residents: a randomized controlled trial. Exp Gerontol. 2018;103:94–100.
- Galik EM, Resnick B, Holmes SD, et al. Cluster randomized controlled trial testing the impact of function and behavior focused care for nursing home residents with dementia. J Am Med Dir Assoc. 2021;22:1421–1428.
- Nawrat-Szołtysik A, Polak A, Małecki A, et al. Effect of physical activity on the sequelae of osteoporosis in female residents of residential care facilities. Adv Clin Exp Med. 2018;27(5):633–642.
- Nawrat-Szołtysik A, Miodońska Z, Opara J, et al. Effect of physical activity on the quality of life in osteoporotic females living in residential facilities: a randomized controlled trial. J Geriatr Phys Ther. 2019;42(2):98–104.
- Chin A Paw MJM, van Poppel MNM, van Mechelen W. Effects of resistance and functional-skills training on habitual activity and constipation among older adults living in long-term care facilities: a randomized controlled trial. BMC Geriatr. 2006;6:9.
- Galik E, Resnick B, Hammersla M, et al. Optimizing function and physical activity among nursing home residents with dementia: testing the impact of function-focused care. Gerontologist. 2014;54(6):930–943.
- Grönstedt H, Frändin K, Bergland A, et al. Effects of individually tailored physical and daily activities in nursing home residents on activities of daily living, physical performance and physical activity level: a randomized controlled trial. Gerontology. 2013;59(3):220–229.
- Schnelle JF, Leung FW, Rao SSC, et al. A controlled trial of an intervention to improve urinary and fecal incontinence and constipation. J Am Geriatr Soc. 2010;58(8):1504–1511.
- Rezola-Pardo C, Rodriguez-Larrad A, Bidaurrazaga-Letona I, et al. Comparison between multicomponent exercise and walking interventions in long-term nursing homes: a randomized controlled trial. Gerontologist. 2020;60(7):1364–1373.
- Moyle W, Jones C, Murfield J, et al. Effect of a robotic seal on the motor activity and sleep patterns of older people with dementia, as measured by wearable technology: a cluster-randomised controlled trial. Maturitas. 2018;110:10–17.
- Hurley MV, Wood J, Smith R, et al. The feasibility of increasing physical activity in care home residents: active residents in care homes (ARCH) programme. Physiotherapy. 2020;107:50–57.
- Galik EM, Resnick B, Gruber-Baldini A, et al. Pilot testing of the restorative care intervention for the cognitively impaired. J Am Med Dir Assoc. 2008;9(7):516–522.
- Liu XX, Hu J. The effects of an intervention on physical activity among nursing home residents in Wuhan, China. J Gerontol Nurs. 2015;41(3):30–39.
- Lobo A, Carvalho J, Santos P. Effects of training and detraining on physical fitness, physical activity patterns, cardiovascular variables, and HRQoL after 3 Health-Promotion interventions in institutionalized elders. Int J Family Med. 2010;2010:486097.
- Pomeroy SH, Scherer Y, Runkawatt V, et al. Person–environment fit and functioning among older adults in a long-term care setting. Geriatr Nurs. 2011;32(5):368–378.
- Keogh JWL, Power N, Wooller L, et al. Physical and psychosocial function in residential aged-care elders: effect of Nintendo Wii sports games. J Aging Phys Act. 2014;22(2):235–244.
- Simmons SF, Schnelle JF. Effects of an exercise and scheduled-toileting intervention on appetite and constipation in nursing home residents. J Nutr Health Aging. 2004;8(2):116–121.
- Mouton A, Gillet N, Mouton F, et al. Effects of a giant exercising board game intervention on ambulatory physical activity among nursing home residents: a preliminary study. Osteoporos Int. 2017;28:S320–S321.
- Koeneman MA, Chorus A, Hopman-Rock M, et al. Novel method to promote physical activity among older adults in residential care: an exploratory field study on implicit social norms. BMC Geriatr. 2017;17(1):8.
- Gordon AL, Franklin M, Bradshaw L, et al. Health status of UK care home residents: a cohort study. Age Ageing. 2014;43(1):97–103.
- Forster A, Airlie J, Ellwood A, et al. An intervention to increase physical activity in care home residents: results of a cluster-randomised, controlled feasibility trial (the REACH trial). Age Ageing. 2021;23:1–16.
- Squires JE, Sullivan K, Eccles MP, et al. Are multifaceted interventions more effective than single-component interventions in changing health-care professionals’ behaviours? An overview of systematic reviews. Implement Sci. 2014;9:152.
- Eldh AC, Wallin L. How single is “single” - some pragmatic reflections on single versus multifaceted interventions to facilitate implementation: comment on “translating evidence into healthcare policy and practice: single versus multifaceted implementation strategies - is there a simple answer to a complex question?.” Int J Health Policy Manag. 2015;4(10):699–701.
- Baert V, Gorus E, Mets T, et al. Motivators and barriers for physical activity in the oldest old: a systematic review. Ageing Res Rev. 2011;10(4):464–474.
- van Alphen HJM, Hortobágyi T, van Heuvelen MJG. Barriers, motivators, and facilitators of physical activity in dementia patients: a systematic review. Arch Gerontol Geriatr. 2016;66:109–118.
- Dewing J. Wandering into the future: reconceptualizing wandering ‘a natural and good thing’. Int J Older People Nurs. 2006;1(4):239–249.
- McDuff J, Phinney A. Walking with meaning: subjective experiences of physical activity in dementia. Glob Qual Nurs Res. 2015;2:1–9.
- Algase DL. What’s new about wandering behaviour? An assessment of recent studies. Int J Older People Nurs. 2006;1(4):226–234.
- Neville CC, McMinn B, Cave P. Implementing the wandering evidence for older people with dementia. Int J Older People Nurs. 2006;1(4):235–238.
- Carlson JA, Sallis JF, Conway TL, et al. Interactions between psychosocial and built environment factors in explaining older adults’ physical activity. Prev Med. 2012;54(1):68–73.
- Lu Z, Rodiek SD, Shepley MM, et al. Influences of physical environment on corridor walking Among assisted living residents: findings from focus group discussions. J Appl Gerontol. 2011;30(4):463–484.
- Golden SD, Earp JAL. Social ecological approaches to individuals and their contexts: twenty years of health education & behavior health promotion interventions. Health Educ Behav. 2012;39(3):364–372.
- Nilsen P, Bernhardsson S. Context matters in implementation science: a scoping review of determinant frameworks that describe contextual determinants for implementation outcomes. BMC Health Serv Res. 2019;19(1):21.
