Abstract
Purpose
To systematically review the literature on effectiveness of remote physiotherapeutic e-Health interventions on pain in patients with musculoskeletal disorders.
Materials and methods
Using online data sources PubMed, Embase, and Cochrane in adults with musculoskeletal disorders with a pain-related complaint. Remote physiotherapeutic e-Health interventions were analysed. Control interventions were not specified. Outcomes on effect of remote e-Health interventions in terms of pain intensity.
Results
From 11,811 studies identified, 27 studies were included. There is limited evidence for the effectiveness for remote e-Health for patients with back pain based on five articles. Twelve articles studied chronic pain and the effectiveness was dependent on the control group and involvement of healthcare providers. In patients with osteoarthritis (five articles), total knee surgery (two articles), and knee pain (three articles) no significant effects were found for remote e-Health compared to control groups.
Conclusions
There is limited evidence for the effectiveness of remote physiotherapeutic e-Health interventions to decrease pain intensity in patients with back pain. There is some evidence for effectiveness of remote e-Health in patients with chronic pain. For patients with osteoarthritis, after total knee surgery and knee pain, there appears to be no effect of e-Health when solely looking at reduction of pain.
This review shows that e-Health can be an effective way of reducing pain in some populations.
Remote physiotherapeutic e-Health interventions may decrease pain intensity in patients with back pain.
Autonomous e-Health is more effective than no treatment in patients with chronic pain.
There is no effect of e-Health in reduction of pain for patients with osteoarthritis, after total knee surgery and knee pain.
Implications for rehabilitation
Introduction
Musculoskeletal disorders contain over 150 diagnoses from the locomotor system and are prevalent in over 50% of the adult population [Citation1–3]. The global disability-adjusted life years (DALYs) for musculoskeletal disorders increased by 61.6% between 1990 and 2016, making this the second largest problem in terms of years lived with disability [Citation1]. Pain is the most common complaint in patients with a musculoskeletal disorder. This musculoskeletal pain leads to a decrease in functioning on daily basis [Citation4].
Physiotherapists are specialized in treating musculoskeletal disorders and support patients to increase their daily functioning [Citation5]. The focus of physiotherapeutic treatment in patients with musculoskeletal pain is on offering individualised patient care to develop strategies for managing pain, rehabilitate and restore physical function by delivering education, exercises, and encouragement to engage in regular physical activity [Citation6]. Physiotherapists may use e-Health in their treatment, as e-Health can serve as a supportive tool for education, exercises, and encouragement [Citation7].
E-health can be defined as the delivery of personalized healthcare at a distance through the use of technology [Citation8]. This technology can be computers and mobile phones, but also satellite communications [Citation9]. When smart or portable devices are specifically used, for instance using mobile applications, this often is referred to as mobile health (mHealth) [Citation9]. Besides the mode of delivery (i.e., computer, mobile, tablet), the moment of delivery can also vary. For instance, e-Health can be used in both the diagnostic process (e.g., intake, questionnaires) [Citation10] and therapeutic process (e.g., videoconferencing, online exercises, education) [Citation11–14]. The types of e-Health interventions vary from interactive websites, to internet delivered programs, and to mobile applications. Furthermore, there are different ways e-Health can be implemented: as an addition to face-to-face care (i.e., blended care), or as a complete replacement for physical consults [Citation13,Citation15,Citation16].
In several countries including the Netherlands during the 2019 novel coronavirus (COVID-19) pandemic [Citation17,Citation18], all physiotherapeutic care had to be offered at distance. By applying remote e-Health tools, patients with (chronic) pain still received care during this pandemic. From the available literature it is known that e-Health generally can be just as effective or slightly more effective than usual face-to-face care [Citation19,Citation20]. However, the challenge remains the uncertainty about the effectiveness in different populations [Citation18,Citation19,Citation21]. It is currently still unknown what the effectiveness is of these remote e-Health interventions on patients with musculoskeletal pain-complaints. Therefore, the aim of this study was to systematically review the literature on the effectiveness of remote physiotherapeutic e-Health interventions on pain in patients with musculoskeletal disorders.
Methods
Protocol and registration
Reporting of this review has been done according to PRISMA recommendations [Citation22], and is registered on PROSPERO (registration number CRD42018055386).
Eligibility criteria
Randomized controlled trials of remote physiotherapeutic e-Health interventions in adults with complaints of the musculoskeletal system were included. Inclusion criteria for the studies applied were: (1) the primary or secondary outcome measure had to be pain related (e.g., pain intensity, pain days, pain-related disability); and e-Health interventions must be: (1) remotely transmitted, (2) applied within the field of physiotherapy for patients with musculoskeletal complaints. The inclusion criteria show that interventions that are within the physiotherapeutic domain (e.g., counselling, exercises) [Citation23] are included as long as patients do not go to the clinic to receive their physiotherapeutic treatment, but their physiotherapeutic treatment is given at distance through an e-Health application (interactive websites, internet delivered programs, video consultations or mobile applications). The therapy could consist of exercises, [Citation24] pain education [Citation25,Citation26] or any other intervention that aimed at decreasing pain-related complaints, for example encouragement to engage in regular physical activity.
Exclusion criteria applied were: (1) the e-Health intervention is a complement to usual face-to-face physiotherapeutic care (e.g., blended care), (2) the e-Health intervention is not patient-oriented (i.e., educational intervention for healthcare professionals), (3) the outcome measures were incomplete for baseline or follow-up, (4) the full text article is not available in English or Dutch, and (5) feasibility studies of e-Health.
Information sources
Literature searches were performed in the electronic databases PubMed [1966 − 2022], Embase [1947 − 2022], and Cochrane [1898 − 2022] to identify randomized controlled trials examining the effects of e-Health interventions on patients with musculoskeletal complaints. Database searches were performed on 25 February 2022.
Search
Combinations of keywords, free text and medical subject headings related to telemedicine, Internet, e-Health interventions, musculoskeletal disorders and physiotherapy were the core of the search strategy. The search strategy was developed in PubMed () and thereafter fitted for other online databases. Keywords and medical subject heading terms used in the search were: (1) e-health OR e-Health OR web OR Internet OR online OR computer OR telemedicine OR telerehabilitation, AND (2) musculoskeletal disorders OR physiotherapy, AND (3) intervention OR randomized controlled trial. Screening of articles was done by two researchers (HvdM, ST), a third researcher (CMS) screened those articles with no consensus independently to be included or excluded. The process of screening was based on relevance and pre-set inclusion and exclusion criteria. References of remaining articles were screened for additional studies. The search results were downloaded in a database created using Covidence [Citation27].
Table 1. Best evidence synthesis.
Study selection
Inclusion criteria were applied to the titles and abstracts of all retrieved records by two researchers blinded for each other’s results (ST, HvdM) after removal of duplicates. For eligibility this process was repeated for full text screening of the remaining articles. A third reviewer (CMS) made the decision regarding inclusion of the article when the two reviewers did not reach consensus.
Data collection process, data items and summary measures
Two reviewers (ST, TvB) performed data extraction from the included articles. A third reviewer (HvdM) checked the extracted data for accuracy. The following key data were extracted from the included articles: (1) study characteristics: sample size; (2) participant characteristics: age and gender; (3) intervention & control characteristics: type of (control) intervention(s), frequency, follow-up of interventions; and (4) outcome measures. For the follow-up data the longest available term was included in this systematic review. Mean and standard deviations were derived from the included studies, where possible, for further statistical analysis. When the p-values for the between-group results were not available, these were calculated using the mean and standard deviations from the publication.
Risk of bias in individual studies
The Cochrane “risk of bias” (RoB) tool assessment was used to assess the risk of bias of the included studies. The RoB tool assesses whether a study has high, low or unclear risk of bias, which may influence study validity, across six domains [Citation28]. The tool does not lead to a quality score but solely focuses on internal validity [Citation28]. Two researchers (HvdM, ST) assessed the methodological quality and risk of bias independently. In case of disagreement, a third reviewer (CMS) made the decision. Results of the RoB assessment were also presented graphically individually and in a summary graph using Review Manager (RevMan) [Citation29]. For the assessment of methodological quality, the Physiotherapy Evidence Database scale (PEDro) was used. The PEDro scale is a valid instrument to measure the methodological quality of clinical trials [Citation30]. The PEDro scale consists of 11 items of which ten of the items assess the internal and/or external validity of the article [Citation31]. The sum score of the ten items is used to rate the methodological quality of the article. An article can score a 9–10 (excellent); 6–8 (good); 4–5 (moderate); or 0–3 (poor) [Citation31].
Synthesis of results
Meta-analysis of the results was not possible due to heterogeneity. So, the evidence was weighed based on the present methodological quality of the included studies. A best evidence synthesis was applied, based on the criteria as described by van Tulder et al. () [Citation32]. The synthesis of the between-group results were described per patient population, as well as the level of involvement of the healthcare provider in the intervention group. This level could be when patients had online interactions with their healthcare provider, described as minimal involved, or when patients had no interaction at all with their healthcare provider. Finally, a distinction was made in the comparison of the intervention with the control group. The control group was subdivided into no care (e.g., waiting list, assessment only) or usual care (e.g., face-to-face treatment).
Additional analysis
For each study, within-group effect sizes were calculated according to the standard mean difference [Citation33]. Effect sizes (ES) were classified as small (<0.20), moderate (around 0.50) or large (>0.80), according to Cohen’s criteria [Citation34]. For between-group analysis the p-value was calculated.
Results
Study selection
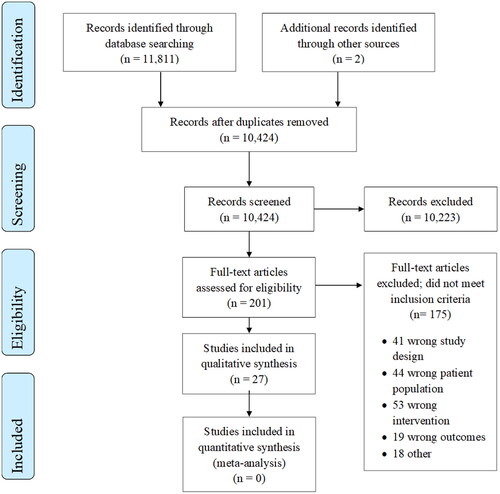
The search strategy revealed 11,811 initial articles from PubMed, Pedro and Cochrane (). Two articles were identified through hand search. After removing double references, Citation10, 424 titles and abstracts were screened for eligibility, resulting in 201 articles which were screened full-text. Finally, 27 articles were included [Citation35–62], and 175 were excluded because inclusion criteria were not met on the study design (n = 41), the patient population (n = 44), the intervention (n = 53), the outcome measures (n = 19), or other reasons (n = 18). A list of excluded references can be found in Appendix 2.
Study characteristics
Overall, the intervention groups consisted of 2,311 patients with a range in age of 35 to 68 years (). Five articles focused on back pain [Citation36,Citation45,Citation52,Citation61,Citation62], twelve on musculoskeletal chronic pain [Citation38,Citation40–42,Citation46,Citation48,Citation51,Citation53,Citation57–60], five on osteoarthritis [Citation35,Citation43,Citation44,Citation47,Citation54], two on total knee surgery [Citation49,Citation50] and three articles on knee pain [Citation37,Citation55,Citation56]. Applied e-Health interventions were interactive websites (n = 8) [Citation36,Citation38,Citation40,Citation46,Citation47,Citation49,Citation52,Citation62], internet delivered programs (n = 15) [Citation35,Citation37,Citation41–43,Citation45,Citation48,Citation50,Citation51,Citation56–60] and mobile applications (n = 5) [Citation44,Citation53–55,Citation61]. Study duration ranged from 6 weeks to 12 months. Six studies [Citation41,Citation49,Citation50,Citation53,Citation58,Citation60] measured pain intensity by the Visual Analog Scale (VAS), a 100 mm line (0 mm: no pain; 100 mm: extreme pain) [Citation64]. Nine studies [Citation35,Citation37,Citation38,Citation42,Citation43,Citation54,Citation56,Citation57,Citation61] measured pain intensity by the Numeric Pain Rating Scale (NPRS), an 11-point scale (0: no pain; 10: extreme pain). Two studies [Citation36,Citation46] used the pain severity subscale of the Multidimensional Pain Inventory (MPI) [Citation65]. Five studies [Citation40,Citation48,Citation51,Citation59,Citation62] used the Brief Pain Inventory (BPI) [Citation66]. Furthermore, three studies [Citation43,Citation50,Citation56] used the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) [Citation67] pain subscale, one study used the Arthritis Impact Measurement Scale 2 (AIMS2) [Citation68] pain subscale [Citation47], one study [Citation55] PROMIS pain and one study [Citation44] used the Hip Disability and Osteoarthritis Outcome Score (HOOS) [Citation69] and Knee Injury and Osteoarthritis Outcome Score (KOOS) [Citation70].
Table 2. Study characteristics.
Risk of bias and methodological quality within studies
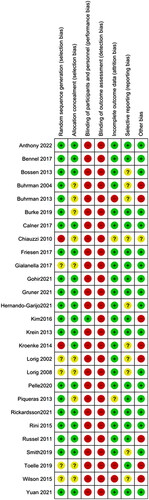
Of the six bias domains assessed with the Cochrane RoB tool (selection bias, performance bias, detection bias, attrition bias, reporting bias and other bias), all except attrition bias had at least 25% unclear or high risk of bias (). Attrition bias and detection bias had the lowest risk of interfering with the results, and detection bias had a 100% high risk of bias score throughout as patients were the outcome assessors for the outcome measure “pain intensity.” depicts the RoB per domain for each individual study. All included studies scored a high risk of bias on at least two domains. Seven studies received a high risk of bias on three or more domains and they also had minimally one other domain with an unclear risk of bias [Citation36,Citation46,Citation48,Citation51,Citation52,Citation61,Citation62]. Two studies did not have any low risk of bias scores [Citation51,Citation62].
Figure 2. Risk of bias graph.
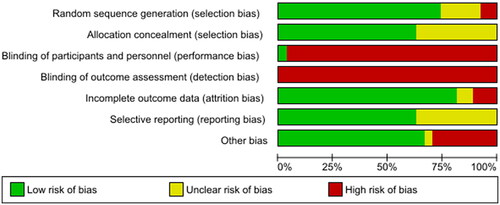
Figure 3. Risk of bias summary.
depicts the PEDro scores per study. The scores for methodological quality ranged from 5 to 8 points, which indicates that all included studies are of moderate to good methodological quality. None of the studies, except for one [Citation37], blinded the participants or therapists and all reported between-group statistical comparisons and point measures for key outcomes.
Table 3. Methodological quality assessment based on the PEDro scale.
Results of studies per patient population
The results of the individual studies and the synthesis of the results are described below per patient population. The between-group effects are used for synthesis of the results as described in the methods. All results are depicted in .
Back pain
Three studies of moderate methodological quality [Citation36,Citation52,Citation61] and two studies of good methodological quality [Citation45,Citation62] assessed the effectiveness of remote e-Health on pain intensity in patients with back pain. Three articles used the NPRS [Citation45,Citation52,Citation61], one study used BPI [Citation61], and one study used both MPI and the VAS through a pain diary [Citation36].
Two studies [Citation36,Citation52] investigated minimally involved care through e-Health and compared their interventions to no care. One study [Citation52] of moderate methodological quality investigated an interactive website which contained a closed moderated discussion group including a book and video about back pain, which was significantly effective on the NPRS compared to the control group [Citation52]. The other study [Citation36], also of moderate methodological quality, used an interactive website for an online self-help program with telephone support as intervention. Compared to the control group, there was no significant effect found on the MPI [Citation36]. Due to inconsistent between-group findings, moderate methodological quality and high risk of bias was found in both studies [Citation36,Citation52]; there is currently no evidence that e-Health with minimal involvement of a healthcare provider is more effective than no care in patients with back pain.
Three studies [Citation45,Citation61,Citation62] described full online programs without healthcare provider involvement. One study [Citation45] compared a group receiving an internet delivered physical activity program where patients received activity trackers, with a group that would upload pedometer data and received email updates. This study was of high methodological quality, low risk of bias and found no statistical difference between both groups on the NPRS. Another study [Citation62] compared an interactive website for an online self-help program to a back pain guide. This study was of good methodological quality, had a high risk of bias and found a significant effect in favour of the intervention on the BPI. These two studies [Citation45,Citation62] compared the online intervention to reading material, but showed conflicting results. The third study [Citation61] which was of moderate methodological quality and had a high risk of bias compared a mobile application to face-to-face physiotherapy and found a significant effect in favour of the mobile application. As this is a moderate quality study, there are indicative findings that e-Health is more effective than face-to-face therapy for patients with back pain.
Overall, there is limited evidence that remote e-Health is more effective than a control intervention on pain intensity in patients with back pain.
Chronic pain
Five studies [Citation38,Citation46,Citation51,Citation58,Citation60] of moderate methodological quality and six studies [Citation41,Citation42,Citation48,Citation53,Citation57,Citation59] of good methodological quality and one article [Citation40] of excellent quality assessed the effectiveness of remote e-Health in patients with chronic or persistent pain. Four studies [Citation40,Citation48,Citation51,Citation59] used the BPI total intensity score, one study [Citation46] used the MPI, three studies [Citation38,Citation42,Citation57] used the NPRS and the VAS was used in four studies [Citation41,Citation53,Citation58,Citation60].
Ten of the interventions used were online with no involvement of the healthcare provider and consisted of internet delivered programs or interactive websites with cognitive behavioural aspects [Citation42,Citation46,Citation51,Citation57,Citation59], telecare management [Citation41,Citation48,Citation53] or a self-guided web-based program [Citation40,Citation58]. Four studies [Citation40,Citation41,Citation48,Citation58] compared their intervention to face-to-face interventions, of which two studies [Citation41,Citation48] found a significant effect for the intervention group, but the other two studies [Citation40,Citation58] did not. Therefore, there is currently no evidence that remote e-Health without involvement of the healthcare provider is more effective than face-to-face interventions in patients with chronic or persistent pain [Citation40,Citation41,Citation48,Citation58]. Four other studies [Citation42,Citation51,Citation57,Citation59] compared their intervention to no intervention and three studies [Citation42,Citation57,Citation59] found a significant difference, indicating that there is moderate evidence for the effectiveness of remote e-Health in patients with chronic or persistent pain when compared to no intervention [Citation42,Citation51,Citation57,Citation59]. One study [Citation46] compared e-Health to an online discussion forum and one study [Citation53] compared e-Health to an paper book, and neither study found statistical differences between groups.
Two studies described e-Health interventions with minimal involvement of a healthcare provider, including telecare management [Citation38,Citation60]. They compared the intervention to usual care, of which both [Citation38,Citation60] found a significant result in favour of the intervention. These findings suggest that there is strong evidence for e-Health interventions with minimal involvement in patients with chronic or persistent pain when compared to a control group (usual care or online).
Osteoarthritis
Five studies [Citation43,Citation44,Citation47,Citation54,Citation71] looked at the effect of different remote e-Health interventions on pain in patients with osteoarthritis. These articles were all assessed as good methodological quality () and consists of internet-based self-management program with minimal involvement of a healthcare provider [Citation43,Citation47] and a fully automatic web-based program or mobile application for patients with osteoarthritis [Citation35,Citation44,Citation54]. Pain intensity was measured with AIMS2 [Citation47], NPRS [Citation35,Citation43,Citation54], WOMAC [Citation43], and HOOS/KOOS [Citation44]. Three interventions [Citation35,Citation47,Citation54] were not significantly more effective than no care and therefore there is currently no evidence for the effectiveness of remote e-Health on pain intensity in patients with osteoarthritis compared to no care. Two studies compared the e-Health intervention to usual care, of which one study found a statistical between-group difference [Citation43] and the other study did not [Citation44]. Therefore, there is currently no evidence for the effectiveness of remote e-Health on pain intensity in patients with osteoarthritis compared to usual care.
Total knee surgery
Two studies [Citation49,Citation50] looked at remote tele-rehabilitation with minimal involvement of a healthcare provider after total knee surgery. The studies were of moderate [Citation49] and high [Citation50] methodological quality and showed no significant improvement on pain measured with the VAS [Citation49,Citation50] and WOMAC [Citation50] when compared to no care. Therefore, there is moderate evidence that e-Health is not effective on pain intensity for patients after total knee surgery compared to no care.
Knee pain
Three studies [Citation37,Citation55,Citation56] investigated on pain outcome in a population of knee pain with online modules measured with NPRS, WOMAC and PROMIS and compared this intervention to a handout with exercises [Citation37], online education [Citation56] and conventional physiotherapy [Citation55]. Two studies [Citation37,Citation56] had good methodological quality and one study [Citation55] with excellent quality showed conflicting results on significance compared to their control group. Therefore, there is limited evidence that e-Health is effective on pain intensity for patients with knee related complaints.
Discussion
This systematic review showed that there is limited evidence for the effectiveness of e-Health on pain intensity in patients with back pain regardless of the extent to which the healthcare professional was involved in the online intervention and regardless of which control group was used. In patients with chronic pain, there is no evidence that remote e-Health without involvement of the healthcare providers is more effective than face-to-face interventions, but there is moderate evidence that it is more effective than no treatment. There is strong evidence that remote e-Health with minimal involvement of the healthcare provider is more effective than a control intervention in patients with chronic pain. For patients after total knee surgery, there appears to be a moderate effect of e-Health intervention with minimal involvement in the reduction of pain compared to no care. While for patients with osteoarthritis and knee pain there was no effect on the pain related outcome.
When we look at the between-group effect, this systematic review shows that there is no evidence between minimal healthcare provider involvement and no care in patients with back pain. There is, however, an indication that remote autonomous e-Health is more effective compared to face-to-face (usual care) treatments. Actually, according to another systematic review, autonomous e-Health interventions were not more effective than usual care in patients with low back pain [Citation72]. According to the conflicting results in patients with low back pain, it may be that the interventions are insufficient tailored. Gains can be made when interventions are more adapted to individual needs and wishes. For low back pain, for example, the StarT-back screening tool is developed in which a treatment guideline is specified based on the risk profile [Citation73]. The stepped care principle can also support personalized care, because the inclusion of giving autonomous home-based e-Health, blended care of face-to-face treatment requires careful consideration of whether a patient has motivation, access to digital services and the ability to process information [Citation74]. The current systematic review looked into remote e-Health interventions. As it has been shown that a physiotherapist can positively influence treatment outcomes by providing positive feedback, giving answers on patient’s questions, and providing clear instructions for home practice [Citation75], it could be useful to see with the studies included in the current review what the effect of just the e-Health application is, rather than the influence of the physiotherapist.
For patients with chronic pain, we found conflicting results regarding the effectiveness of remote e-Health interventions depending on the involvement of the healthcare provider and the control group. This study showed that when the online involvement of the healthcare provider increases, the evidence of effectiveness of remote e-Health compared to usual care also increases. Autonomous e-Health is more effective than no treatment, but not more effective than usual care unless there is minimal involvement of the healthcare provider. This is comparable to other studies in which they have shown that there is no evidence that autonomous remote e-Health has additional value next to usual care in patients with chronic pain [Citation76], other than their cost-effectiveness [Citation12,Citation14,Citation77,Citation78]. Therefore, when applying e-Health in this population, it should be integrated in the intervention, also known as blended care, to provide effective treatment with lower costs [Citation13,Citation79].
The amount of effect of e-Health depends on usage and adherence [Citation80]. Usage contains activity on the e-Health application, such as number of logins, minutes or activities completed [Citation81]. Adherence is the extent to which a person uses the e-Health application as intended [Citation81]. The studies included in the current review show contradictory evidence regarding usage, adherence and effect of the e-Health intervention [Citation47,Citation51,Citation57,Citation58,Citation60,Citation61]. For instance, some studies report low adherence rates but did not correct for this in the assessment of effectiveness [Citation51,Citation57,Citation58]. In case of low adherence, i.e., the e-Health intervention was often not completely followed as intended, interpretation of the findings becomes more challenging [Citation81].
In this systematic review, no significant effect was found in the population of osteoarthritis or patients with knee pain or knee surgery. Reasons why no effect was found is because of the relatively low number of studies included in this systematic review. Another explanation is that the pain outcome measure may not be the most obvious physical outcome measure for these populations. When looking at other outcome measures, for example physical activity, there is a significant long-term effect in favour of remote e-Health. At last, there might be a potential ceiling effect of the amount of therapy a patient can receive in which additional treatment would no longer lead to improved recovery [Citation82]. In the case of pain intensity, evidence suggests that the content of the intervention is more important than the mode of delivery (i.e., in person or e-Health) [Citation82]. Furthermore, there are big within-patient differences in the course of pain in patients with knee osteoarthritis [Citation83], so with small sample sized and limited number of studies the interpretation of these results should be done with caution.
Limitations and strengths
A limitation is that even though this review only included remote e-Health interventions, there was still a large variety of intervention types (e.g., interactive websites, internet delivered programs and mobile applications) and pain related outcome measurements (VAS, NPRS, MDI, etc). Because of this, it was not possible to do a meta-analysis and interpretation of results must be done with caution. Another reason to be cautious is that the interventions in this review sometimes were given by a professional other than physiotherapists, for example by a physician-pain specialist [Citation48], psychologists [Citation42], nurse [Citation60] or undefined therapists [Citation38,Citation40,Citation45,Citation51,Citation62]. However, all included interventions can be delivered by physiotherapists as they are part of the modality physiotherapist have in the management of pain related complaints [Citation23]. The final limitation of this study is that only within-group effect sizes are presented. It indicates the direction of the effectiveness of the intervention itself. Unfortunately, we were unable to abstract enough information from the articles to calculate the between-group effect sizes. Therefore, we extracted the p value of the between group effects per article which are presented in . A strength of this study is that all included articles were at least of moderate methodological quality, as assessed with the PEDro scale. All steps of this review were done with minimally two researchers independent from each other, which increases the reliability of the results. Additionally, both Pedro scale and Cochrane RoB tool were used so a more accurate conclusion can be drawn, as there are some slight discrepancies between the two tools.
Recommendations for future research and clinical practice
Based on the heterogeneity of interventions and outcome measures, we recommend to describe the used e-Health intervention carefully in future research so these interventions can be reproduced optimally. For example, by using the TIDieR checklist which aims to improve the completeness of reporting of interventions [Citation84]. The TIDieR checklist includes 12 items, like brief name, why, what (materials), what (procedure), who provided, how, where, when and how much, tailoring, modifications and how well (planned) [Citation84]. Additionally, future studies should look into the impact of patients’ experience of pain on daily functioning, and how e-Health can contribute to decrease the impact of pain.
While remote e-Health and usual care has no preference based on pain-outcome, literature shows in some cases that e-Health is more cost-effective than usual care [Citation79,Citation85]. The cost-effectiveness is in most studies still unclear and should be studied. It would be interesting for instance to determine the cost-effectiveness of e-Health interventions in chronic pain populations because of their social and economic burden [Citation77,Citation63].
When applying e-Health in the clinical practice, the amount of e-Health should be able to tailor specific needs of patients [Citation86]. Some patients may have limited motivation to online consultation or other aspects of e-Health and patient preferences are an important aspect of evidence-based practice [Citation87]. Another aspect of evidence-based practice is available evidence, to which this review contributes and shows that e-Health can be an effective way of reducing pain in some populations. However, this review is regarding autonomous e-Health interventions, and most physiotherapists will apply blended e-Health to ensure their full skillset, including hands-on therapy, can be used to help their patient with pain complaints [Citation88–90].
Conclusion
There is limited evidence for the effectiveness of remote physiotherapeutic e-Health interventions to decrease pain intensity in patients with back pain. Autonomous e-Health is more effective than no treatment in patients with chronic pain, but not more effective than usual care unless there is minimal involvement of the healthcare provider. For patients with osteoarthritis, after total knee surgery and knee pain, there appears to be no effect of e-Health in the reduction of pain.
Disclosure statement
No potential conflict was reported by the author(s).
References
- Briggs AM, Woolf AD, Dreinhöfer K, et al. Reducing the global burden of musculoskeletal conditions. Bull World Health Organ. 2018;96(5):366–368.
- Blackwell DL, Lucas JW, Clarke TC. Summary health statistics for U.S. adults: national health interview survey, 2012. Vital Health Stat 10. 2014;(260):1–161.
- Murray CJL, Richards MA, Newton JN, et al. UK health performance: findings of the global burden of disease study 2010. Lancet. 2013;381(9871):997–1020.
- Dueñas M, Ojeda B, Salazar A, et al. A review of chronic pain impact on patients, their social environment and the health care system. J Pain Res. 2016;9:457–467.
- Childs JD, Whitman JM, Sizer PS, et al. A description of physical therapists’ knowledge in managing musculoskeletal conditions. BMC Musculoskelet Disord. 2005;6:32.
- Hodges PW, Smeets RJ. Interaction between pain, movement, and physical activity: short-term benefits, long-term consequences, and targets for treatment. Clin J Pain. 2015;31(2):97–107.
- Alpay L, Van Der Boog P, Dumaij A. An empowerment-based approach to developing innovative e-health tools for self-management. Health Informatics J. 2011;17(4):247–255.
- Elbert NJ, van Os-Medendorp H, van Renselaar W, et al. Effectiveness and cost-effectiveness of ehealth interventions in somatic diseases: a systematic review of systematic reviews and meta-analyses. J Med Internet Res. 2014;16(4):e110.
- Moss RJ, Süle A, Kohl S. EHealth and mHealth. Eur J Hosp Pharm. 2019;26(1):57–58.
- Mani S, Sharma S, Omar B, et al. Validity and reliability of internet-based physiotherapy assessment for musculoskeletal disorders: a systematic review. J Telemed Telecare. 2017;23(3):379–391.
- Grona SL, Bath B, Busch A, et al. Use of videoconferencing for physical therapy in people with musculoskeletal conditions: a systematic review. J Telemed Telecare. 2018;24(5):341–355.
- Adamse C, Dekker-Van Weering MGH, van Etten-Jamaludin FS, et al. The effectiveness of exercise-based telemedicine on pain, physical activity and quality of life in the treatment of chronic pain: a systematic review. J Telemed Telecare. 2018;24(8):511–526.
- Kloek C, Bossen D, de Bakker DH, et al. Blended interventions to change behavior in patients with chronic somatic disorders: systematic review. J Med Internet Res. 2017;19(12):e418.
- Kloek CJJ, Bossen D, Spreeuwenberg PM, et al. Effectiveness of a blended physical therapist intervention in people with hip osteoarthritis, knee osteoarthritis, or both: a Cluster-Randomized controlled trial. Phys Ther. 2018;17:560–570.
- Barak A, Klein B, Proudfoot JG. Defining Internet-supported therapeutic interventions. Ann Behav Med. 2009;38(1):4–17.
- Wentzel J, van der Vaart R, Bohlmeijer ET, et al. Mixing online and face-to-Face therapy: how to benefit from blended care in mental health care. JMIR Ment Health. 2016;3(1):e9.
- Kinross P, Suetens C, Gomes Dias J, European Centre for Disease Prevention and Control (ECDC) Public Health Emergency Team, et al. Rapidly increasing cumulative incidence of coronavirus disease (COVID-19) in the european union/european economic area and the United Kingdom, 1 january to 15 march 2020. Eurosurveillance. 2020;25(11):2000285.
- Ghai B, Malhotra N, Bajwa S. Telemedicine for chronic pain management during COVID-19 pandemic. Indian J Anaesth. 2020;64(6):456–462.
- Seron P, Oliveros M-J, Gutierrez-Arias R, et al. Effectiveness of telerehabilitation in physical therapy: a rapid overview. Phys Ther. 2021;101(6):1–18.
- Bucki FM, Clay MB, Tobiczyk H, et al. Scoping review of telehealth for musculoskeletal disorders: applications for the COVID-19 pandemic. J Manipulative Physiol Ther. 2021;44(7):558–565.
- Corso M, Cancelliere C, Mior S, et al. Are nonpharmacologic interventions delivered through synchronous telehealth as effective and safe as in-Person interventions for the management of patients with nonacute musculoskeletal conditions? A systematic rapid review. Arch Phys Med Rehabil. 2022;103(1):145–154.e11.
- Moher D, Liberati A, Tetzlaff J, PRISMA Group, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLOS Med. 2009;6(7):e1000097.
- APTA. Who are physical therapists? [Published 2015; cited 2018 Feb 1]. Available from: http://www.apta.org/AboutPTs/.
- Lima LV, Abner TSS, Sluka KA. Does exercise increase or decrease pain? Central mechanisms underlying these two phenomena. J Physiol. 2017;595(13):4141–4150.
- Louw A, Nijs J, Puentedura EJ. A clinical perspective on a pain neuroscience education approach to manual therapy. J Man Manip Ther. 2017;25(3):160–168.
- Watson JA, Ryan CG, Cooper L, et al. Pain neuroscience education for adults with chronic musculoskeletal pain: a mixed-methods systematic review and meta-analysis. J Pain. 2019;20(10):1140.e1-1140–e22.
- Covidence Systematic Review software. Veritas health innovation. Melbourne, Australia. https://www.covidence.org
- Higgins JPT, Altman DG, Gøtzsche PC, Cochrane Bias Methods Group, et al. The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343(2):d5928–d5928.
- RevMan Published online 2014. https://revman.cochrane.org/
- de Morton NA. The PEDro scale is a valid measure of the methodological quality of clinical trials: a demographic study. Aust J Physiother. 2009;55(2):129–133.
- Maher CG, Sherrington C, Herbert RD, et al. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83(8):713–721.
- van Tulder MW, Cherkin DC, Berman B, et al. The effectiveness of acupuncture in the management of acute and chronic low back pain. A systematic review within the framework of the cochrane collaboration back review group. Spine. 1999;24(11):1113–1123.
- Hedges L, Olkin I. Statistical methods for Meta-Analysis. 1st ed. Washington, DC: National Institute of Education; 1985.
- Cohen J. Statistical power analysis for behavioural sciences. 2nd ed. New York: Lawrence Eribaum Associates; 1988.
- Bossen D, Veenhof C, Van Beek KE, et al. Effectiveness of a web-based physical activity intervention in patients with knee and/or hip osteoarthritis: randomized controlled trial. J Med Internet Res. 2013;15(11):e257.
- Buhrman M, Fältenhag S, Ström L, et al. Controlled trial of internet-based treatment with telephone support for chronic back pain. Pain. 2004;111(3):368–377.
- Kim TWB, Gay N, Khemka A, et al. Internet-based exercise therapy using algorithms for conservative treatment of anterior knee pain: a pragmatic randomized controlled trial. JMIR Rehabil Assist Technol. 2016;3(2):e12.
- Lorig KR, Ritter PL, Laurent DD, et al. The internet-based arthritis self-management program: a one-year randomized trial for patients with arthritis or fibromyalgia. Arthritis Rheum. 2008;59(7):1009–1017.
- Kohns DJ, Urbanik CP, Geisser ME, et al. The effects of a pain psychology and neuroscience Self-Evaluation internet intervention. Clin J Pain. 2020;36(9):683–692.
- Smith J, Faux SG, Gardner T, et al. Reboot online: a randomized controlled trial comparing an online multidisciplinary pain management program with usual care for chronic pain. Pain Med. 2019;20(12):2385–2396.
- Hernando-Garijo I, Ceballos-Laita L, Mingo-Gómez MT, et al. Immediate effects of a telerehabilitation program based on aerobic exercise in women with fibromyalgia. IJERPH. 2021;18(4):2075.
- Rickardsson J, Gentili C, Holmström L, et al. Internet-delivered acceptance and commitment therapy as microlearning for chronic pain: a randomized controlled trial with 1-year follow-up. Eur J Pain. 2021;25(5):1012–1030.
- Gohir SA, Eek F, Kelly A, et al. Effectiveness of Internet-Based exercises aimed at treating knee osteoarthritis: the iBEAT-OA randomized clinical trial. JAMA Netw Open. 2021;4(2):e210012–e210012.
- Pelle T, Bevers K, van der Palen J, et al. Effect of the dr. Bart application on healthcare use and clinical outcomes in people with osteoarthritis of the knee and/or hip in The Netherlands; a randomized controlled trial. Osteoarthritis Cartilage. 2020;28(4):418–427.
- Krein SL, Kadri R, Hughes M, et al. Pedometer-based internet-mediated intervention for adults with chronic low back pain: randomized controlled trial. J Med Internet Res. 2013;15(8):e181.
- Buhrman M, Skoglund A, Husell J, et al. Guided internet-delivered acceptance and commitment therapy for chronic pain patients: a randomized controlled trial. Behav Res Ther. 2013;51(6):307–315.
- Rini C, Porter LS, Somers TJ, et al. Automated internet-based pain coping skills training to manage osteoarthritis pain: a randomized controlled trial. Pain. 2015;156(5):837–848.
- Kroenke K, Krebs EE, Wu J, et al. Telecare collaborative management of chronic pain in primary care a randomized clinical trial. JAMA - J Am Med Assoc. 2014;312(3):240–248.
- Piqueras M, Marco E, Coll M, et al. Effectiveness of an interactive virtual telerehabilitation system in patients after total knee arthoplasty: a randomized controlled trial. J Rehabil Med. 2013;45(4):392–396.
- Russell TG, Buttrum P, Wootton R, et al. Internet-based outpatient telerehabilitation for patients following total knee arthroplasty: a randomized controlled trial. J Bone Joint Surg Am. 2011;93(2):113–120.
- Wilson M, Roll JM, Corbett C, et al. Empowering patients with persistent pain using an internet-based self-management program. Pain Manag Nurs. 2015;16(4):503–514.
- Lorig KR, Laurent DD, Deyo RA, et al. Can a back pain e-mail discussion group improve health status and lower health care costs? A randomized study. Arch Intern Med. 2002;162(7):792–796.
- Yuan SLK, Couto LA, Marques AP. Effects of a six-week mobile app versus paper book intervention on quality of life, symptoms, and self-care in patients with fibromyalgia: a randomized parallel trial. Braz J Phys Ther. 2021;25(4):428–436.
- Anthony CA, Rojas E, Glass N, et al. A psycholgical intervention delivered by automated mobile phone messaging stabilized hip and knee function during the COVID-19 pandemic: a randomized controlled trial. J Arthroplasty. 2022;37(3):431–437.e3.
- Gruner MP, Hogaboom N, Hasley I, et al. Prospective, single-blind, randomized controlled trial to evaluate the effectiveness of a digital exercise therapy application compared with conventional physical therapy for the treatment of nonoperative knee conditions. Arch Rehabil Res Clin Transl. 2021;3(4):100151.
- Bennell KL, Nelligan R, Dobson F, et al. Effectiveness of an internet-delivered exercise and pain-coping skills training intervention for persons with chronic knee pain: a randomized trial. Ann Intern Med. 2017;166(7):453–462.
- Burke D, Lennon O, Blake C, et al. An internet-delivered cognitive behavioural therapy pain management programme for spinal cord injury pain: a randomized controlled trial. Eur J Pain. 2019;(23)7:1264–1282.
- Calner T, Nordin C, Eriksson MK, et al. Effects of a self-guided, web-based activity programme for patients with persistent musculoskeletal pain in primary healthcare: a randomized controlled trial. Eur J Pain. 2017;21(6):1110–1120.
- Friesen LN, Hadjistavropoulos HD, Schneider LH, et al. Examination of an internet-delivered cognitive behavioural pain management course for adults with fibromyalgia: a randomized controlled trial. Pain. 2017;158(4):593–604.
- Gialanella B, Ettori T, Faustini S, et al. Home-based telemedicine in patients with chronic neck pain. Am J Phys Med Rehabil. 2017;96(5):327–332.
- Toelle TR, Utpadel-Fischler DA, Haas K-K, et al. App-based multidisciplinary back pain treatment versus combined physiotherapy plus online education: a randomized controlled trial. NPJ Digit Med. 2019;2:34.
- Chiauzzi E, Pujol LA, Wood M, et al. painACTION-back pain: a self-management website for people with chronic back pain. Pain Med. 2010;11(7):1044–1058.
- Jamison DT, Breman JG, Measham AR, et al. Cost-effectiveness analysis. In Priorities in health. Washington, DC: The International Bank for Reconstruction and Development/The World Bank; 2006.
- Kahl C, Cleland J A Visual analogue scale, numeric pain rating scale and the McGill pain questionnaire: an overview of psychometric properties. Phys Ther Rev. 2005;10(2):123–128.
- Verra ML, Angst F, Staal JB, et al. Reliability of the multidimensional pain inventory and stability of the MPI classification system in chronic back pain. BMC Musculoskelet Disord. 2012;13(1):155.
- Poquet N, Lin C. The brief pain inventory (BPI). J Physiother. 2016;62(1):52.
- Gandek B. Measurement properties of the Western Ontario and McMaster universities osteoarthritis index: a systematic review. Arthritis Care Res. 2015;67(2):216–229.
- Meenan RF, Mason JH, Anderson JJ, et al. AIMS2. The content and properties of a revised and expanded arthritis impact measurement scales health status questionnaire. Arthritis Rheum. 1992;35(1):1–10.
- Thorborg K, Roos E, Bartels E, et al. Validity, reliability and responsiveness of patient-reported outcome questionnaires when assessing hip and groin disability: a systematic review. Br J Sports Med. 2010;44(16):1186–1196.
- Collins N, Prinsen C, Christensen R, et al. Knee injury and osteoarthritis outcome score (KOOS): systematic review and meta-analysis of measurement properties. Osteoarthritis Cartilage. 2016;24(8):1317–1329.
- Bossen D, Veenhof C, Dekker J, et al. The usability and preliminary effectiveness of a web-based physical activity intervention in patients with knee and/or hip osteoarthritis. BMC Med Inform Decis Mak. 2013;13:61.
- Dario AB, Moreti Cabral A, Almeida L, et al. Effectiveness of telehealth-based interventions in the management of non-specific low back pain: a systematic review with meta-analysis. Spine J. 2017;17(9):1342–1351.
- Hill JC, Dunn KM, Lewis M, et al. A primary care back pain screening tool: identifying patient subgroups for initial treatment. Arthritis Rheum. 2008;59(5):632–641.
- Kloek CJJ, Janssen J, Veenhof C. Development of a checklist to assist physiotherapists in determination of patients’ suitability for a blended treatment. Telemed J E Health. 2020;26(8):1051–1065.
- Hall AM, Ferreira PH, Maher CG, et al. The influence of the therapist-patient relationship on treatment outcome in physical rehabilitation: a systematic review. Phys Ther. 2010;90(8):1099–1110.
- de Oliveira Lima L, Saragiotto BT, Costa LOP, et al. Self-guided web-based pain education for people with musculoskeletal pain: a systematic review and meta-analysis. Phys Ther. 2021;101(10):1–12.
- Gaskin DJ, Richard P. The economic costs of pain in the United States. J Pain. 2012;13(8):715–724.
- Bitton R. The economic burden of osteoarthritis. Am J Manag Care. 2009;15(8 Suppl):230–235.
- de la Torre-Díez I, López-Coronado M, Vaca C, et al. Cost-Utility and Cost-Effectiveness studies of telemedicine, electronic, and mobile health systems in the literature: a systematic review. Telemed J E Health. 2015;21(2):81–85.
- Donkin L, Christensen H, Naismith SL, et al. A systematic review of the impact of adherence on the effectiveness of e-therapies. J Med Internet Res. 2011;13(3):e52.
- Sieverink F, Kelders SM, Gemert-Pijnen V. Clarifying the concept of adherence to e-Health technology: systematic review on when usage becomes adherence. J Med Internet Res. 2017;19(12):e402.
- Latif-Zade T, Tucci B, Verbovetskaya D, et al. Systematic review shows tele-rehabilitation might achieve comparable results to office-based rehabilitation for decreasing pain in patients with knee osteoarthritis. Med. 2021;57(8):764.
- De Rooij M, Van Der Leeden M, Heymans MW, et al. Prognosis of pain and physical functioning in patients with knee osteoarthritis: a systematic review and meta-analysis. Arthritis Care Res. 2016;68(4):481–492.
- Hoffmann TC, Glasziou PP, Boutron I, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ. 2014;348:g1687.
- Sanyal C, Stolee P, Juzwishin D, et al. Economic evaluations of eHealth technologies: a systematic review. PLOS One. 2018;13(6):e0198112.
- Kloek CJJ, Bossen D, de Vries HJ, et al. Physiotherapists’ experiences with a blended osteoarthritis intervention: a mixed methods study. Physiother Theory Pract. 2018;36(5):572–579.
- Barnard S, Wiles R. Evidence-based physiotherapy. Physiotherapy. 2001;87(3):115–124.
- van der Meer HA, Doomen A, Visscher CM, et al. The additional value of e-Health for patients with a temporomandibular disorder: a mixed methods study on the perspectives of orofacial physical therapists and patients. Disabil Rehabil Assist Technol. 2022;12:1–13.
- Barton CJ, Ezzat AM, Merolli M, et al. “Its second best” a mixed-methods evaluation of the experiences and attitudes of people with musculoskeletal pain towards physiotherapist delivered telehealth during the COVID-19 pandemic. Musculoskelet Sci Pract. 2022;58:102500.
- Malliaras P, Merolli M, Williams CM, et al. It’s not hands-on therapy, so it’s very limited’: telehealth use and views among allied health clinicians during the coronavirus pandemic. Musculoskelet Sci Pract. 2021;52:102340.
Appendix 1
Table A1. Search strategies.
Appendix 2.
List of excluded articles
175 were excluded because:
the study design was not a RCT or had other issues (n = 41) [1–41],
the patient population was not in line with our in- and exclusion criteria (n = 44) [42–85],
the intervention was not in line with our in- and exclusion criteria (n = 53) [86–138],
the outcome measures were not in line with our in- and exclusion criteria (n = 19) [139–157],
other reasons (n = 18) [158–175].
References
[1]Alley S, Jennings C, Plotnikoff R, et al. My Activity Coach – using video-coaching to assist a web-based computer-tailored physical activity intervention: a randomised controlled trial protocol. BMC Public Health. 2014;14:738.
[2]Azevedo R, Bernardes M, Fonseca J, et al. Smartphone application for rheumatoid arthritis self-management: cross-sectional study revealed the usefulness, willingness to use and patients’ needs. Rheumatol Int. 2015;35(10):1675–1685.
[3]Geraghty A, Stanford R, Little P, et al. Using an internet intervention to support self-management of low back pain in primary care: protocol for a randomised controlled feasibility trial (SupportBack). BMJ Open. 2015;5(9):e009524.
[4]Hill AJ, Theodoros DG, Russell TG, et al. The redesign and re-evaluation of an internet-based telerehabilitation system for the assessment of dysarthria in adults. Telemed J E Health. 2009;15(9):840–850.
[5]Hollinghurst S, Coast J, Busby J, et al. A pragmatic randomised controlled trial of “PhysioDirect” telephone assessment and advice services for patients with musculoskeletal problems: economic evaluation. BMJ Open. 2013;3(10):e003406.
[6]Hui E, Lee PSC, Woo J. Management of urinary incontinence in older women using videoconferencing versus conventional management: a randomized controlled trial. J Telemed Telecare. 2006;12(7):343–347.
[7]Iles R. A randomized controlled trial of telephone coaching for return to usual activity in low back pain. Spine J. 2011;11(4):231–238.
[8]Ljótsson B, Atterlöf E, Lagerlöf M, et al. Internet-delivered acceptance and values-based exposure treatment for fibromyalgia: a pilot study. Cogn Behav Ther. 2014;43(2):93–104.
[9]Moe RH, Grotle M, Kjeken I, et al. A telephone follow-up after an integrated outpatient osteoarthritis intervention does not enhance patient health at 12 months-results from a randomised controlled trial. Ann Rheum Dis. 2014;73(Suppl 2):1230.2–1230.
[10]Nosek MA, Robinson-Whelen S, Hughes RB, et al. An internet-based virtual reality intervention for enhancing self-esteem in women with disabilities: results of a feasibility study. Rehabil Psychol. 2016;61(4):358–370.
[11]Paul L, Coulter E, Cameron S, et al. Web-based physiotherapy for people with axial spondyloarthritis (WEBPASS) – a study protocol. BMC Musculoskelet Disord. 2016;17(1):360.
[12]Russell T, Truter P, Blumke R, et al. The diagnostic accuracy of telerehabilitation for nonarticular lower-limb musculoskeletal disorders. Telemed J E Health. 2010;16(5):585–594.
[13]Bossen D, Kloek C, Snippe HW, et al. A blended intervention for patients with knee and hip osteoarthritis in the physical therapy practice: development and a pilot study. JMIR Res Protoc. 2016;5(1):e32.
[14]Schell E, Theorell T, Hasson D, et al. Impact of a web-based stress management and health promotion program on neck-shoulder-back pain in knowledge workers? 12 month prospective controlled follow-up. J Occup Environ Med. 2008;50(6):667–676.
[15]Sciamanna C, Harrold L, Manocchia M, et al. The effect of web-based, personalized, osteoarthritis quality improvement feedback on patient satisfaction with osteoarthritis care. Am J Med Qual. 2005;20(3):127–137.
[16]Shigaki C, Smarr K, Gong Y, et al. Social interactions in an online self-management program for rheumatoid arthritis. Chronic Illn. 2008;4(4):239–246.
[17]Shukla H, Nair S, Thakker D. Role of telerehabilitation in patients following total knee arthroplasty: evidence from a systematic literature review and meta-analysis. J Telemed Telecare. 2017;23(2):339–346.
[18]Slater M, Atkinson J, Weickgenant A, et al. Six-month follow-up of a telehealth intervention for chronic back pain. J Pain. 2012;13(4):S97.
[19]Spasić I, Button K, Divoli A, et al. TRAK App suite: a web-based intervention for delivering standard care for the rehabilitation of knee conditions. JMIR Res Protoc. 2015;4(4):e122.
[20]Suri P, Rainville J, Fitzmaurice GM, et al. Acute low back pain is marked by variability: an internet-based pilot study. BMC Musculoskelet Disord. 2011;12(1):220. (Hunter DJ([email protected]) Northern Clinical School, University of Sydney, Sydney, Australia PG-)
[21]Tierce-Hazard S, Sadarangani T. Optimizing the primary care management of chronic pain through Telecare. J Clin Outcomes Manag. 2014;21(11):493–495
[22]Valenzuela-Pascual F, Molina F, Corbi F, et al. The influence of a biopsychosocial educational internet-based intervention on pain, dysfunction, quality of life, and pain cognition in chronic low back pain patients in primary care: a mixed methods approach. BMC Med Inform Decis Mak. 2015;15:97.
[23]van den Berg M, Ronday H, Peeters A, et al. Engagement and satisfaction with an Internet-based physical activity intervention in patients with rheumatoid arthritis. Rheumatology. 2007;46(3):545–552.
[24]Bossen D, Veenhof C, Dekker J, et al. The usability and preliminary effectiveness of a web-based physical activity intervention in patients with knee and/or hip osteoarthritis. BMC Med Inform Decis Mak. 2013;13:61.
[25]Voerman JS, Remerie S, Westendorp T, et al. Effects of a guided internet-delivered self-help intervention for adolescents with chronic pain. J Pain. 2015;16(11):1115–1126.
[26]White M, Stinson JN, Lingley-Pottie P, et al. Exploring therapeutic alliance with an internet-based self-management program with brief telephone support for youth with arthritis: a pilot study. Telemed J E Health. 2012;18(4):271–276.
[27]Adamse C, Dekker-Van Weering MGH, van Etten-Jamaludin FS, et al. The effectiveness of exercise-based telemedicine on pain, physical activity and quality of life in the treatment of chronic pain: a systematic review. J Telemed Telecare. 2018;24(8):511–526.
[28]Beneciuk JM, George SZ, Greco CM, et al. Targeted interventions to prevent transitioning from acute to chronic low back pain in high-risk patients: development and delivery of a pragmatic training course of psychologically informed physical therapy for the TARGET trial. Trials. 2019;20(1):256.
[29]Bernardy K, Klose P, Welsch P, et al. Efficacy, acceptability and safety of Internet‐delivered psychological therapies for fibromyalgia syndrome: a systematic review and meta‐analysis of randomized controlled trials. Eur J Pain. 2019;23(1):3–14.
[30]Dario AB, Moreti Cabral A, Almeida L, et al. Effectiveness of telehealth-based interventions in the management of non-specific low back pain: a systematic review with meta-analysis. Spine J. 2017;17(9):1342–1351.
[31]Dear BF, Courtney C, Khor KE, et al. The pain course. Clin J Pain. 2018;34(6):505–514.
[32]Schultz R, Smith J, Newby JM, et al. Pilot trial of the reboot online program: an internet-delivered, multidisciplinary pain management program for chronic pain. Pain Res Manag. 2018;2018:1–11.
[33]Pelle T, Bevers K, van den HF, et al. Economic evaluation of the Dr. Bart app in people with knee and/or hip osteoarthritis. Osteoarthr Cartil. 2021;29:S386.
[34]Tabacof L, Baker TS, Durbin JR, et al. Telehealth treatment for nonspecific low back pain: a review of the current state in mobile health. PM&R. 2022;14(9):1086–1098.
[35]Bossen D, Veenhof C, Dekker J, et al. The effectiveness of self-guided web-based physical activity interventions among patients with a chronic disease: a systematic review. J Phys Act Health. 2014;11(3):665–677.
[36]Vermeir JF, White MJ, Johnson D, et al. Gamified web-delivered attentional bias modification training for adults with chronic pain: protocol for a randomized, double-blind, placebo-controlled trial. JMIR Res Protoc. 2022;11(1):e32359.
[37]Buhrman M, Nilsson-Ihrfeldt E, Jannert M, et al. Guided internet-based cognitive behavioural treatment for chronic back pain reduces pain catastrophizing: a randomized controlled trial. J Rehabil Med. 2011;43(6):500–505.
[38]Delbaere K, Valenzuela T, Woodbury A, et al. Evaluating the effectiveness of a home-based exercise programme delivered through a tablet computer for preventing falls in older community-dwelling people over 2 years: study protocol for the standing tall randomised controlled trial. BMJ Open. 2015;5(10):e009173.
[39]Eriksson L, B L, Gard G, et al. Physiotherapy at a distance: a controlled study of rehabilitation at home after a shoulder joint operation. J Telemed Telecare. 2009;15(5):215–220.
[40]Fisher E, Law E, Palermo TM, et al. Psychological therapies (remotely delivered) for the management of chronic and recurrent pain in children and adolescents. Cochrane database Syst Rev. 2014 May 14;2014:CD011118.
[41]Geraghty A, Kirby S, Essery R, et al. Internet-based vestibular rehabilitation for adults aged 50 years and over: a protocol for a randomised controlled trial. BMJ Open. 2014;4(7):e005871.
[42]Al-Riyami S, Moles D, Leeson R, et al. Comparison of the instructional efficacy of an internet-based temporomandibular joint (TMJ) tutorial with a traditional seminar. Br Dent J. 2010;209(11):571–576.
[43]Bombardier C, Ehde D, Gibbons L, et al. Telephone-based physical activity counseling for major depression in people with multiple sclerosis. J Consult Clin Psychol. 2013;81(1):89–99.
[44]Ghahari S, Leigh Packer T, Passmore A. Effectiveness of an online fatigue self-management programme for people with chronic neurological conditions: a randomized controlled trial. Clin Rehabil. 2010;24(8):727–744.
[45]Gutiérrez R, Galán Del Río F, Cano de la Cuerda R, et al. A telerehabilitation program by virtual reality-video games improves balance and postural control in multiple sclerosis patients. NeuroRehabilitation. 2013;33(4):545–554.
[46]Hansen A, Grønbaek M, Helge J, et al. Effect of a Web-based intervention to promote physical activity and improve health among physically inactive adults: a population-based randomized controlled trial. J Med Internet Res. 2012;14(5):e145.
[47]Hoaas H, Andreassen H, Lien L, et al. Adherence and factors affecting satisfaction in long-term telerehabilitation for patients with chronic obstructive pulmonary disease: a mixed methods study. BMC Med Inform Decis Mak. 2016;16:26.
[48]Hobson EV, Baird WO, Bradbury M, et al. Telehealth in motor neurone disease. A mixed methods, randomised controlled, pilot study of the use of the TiM telehealth system to deliver highly specialised care in motor neurone disease, at a distance. Amyotroph Lateral Scler Front Degener. 2016;17:54–55.
[49]Hong J, Kim J, Kim S, et al. Effects of home-based tele-exercise on sarcopenia among community-dwelling elderly adults: body composition and functional fitness. Exp Gerontol. 2017;87(Pt A):33–39.
[50]Irvine AB, Gelatt V, Seeley J, et al. Web-based intervention to promote physical activity by sedentary older adults: randomized controlled trial. J Med Internet Res. 2013;15(2):e19.
[51]Kraal J, Peek N, van den Akker-Van Marle M, et al. Effects and costs of home-based training with telemonitoring guidance in low to moderate risk patients entering cardiac rehabilitation: the FIT@Home study. BMC Cardiovasc Disord. 2013;13:82.
[52]Lelieveld O, Armbrust W, Geertzen JHB, et al. Promoting physical activity in children with juvenile idiopathic arthritis through an internet-based program: results of a pilot randomized controlled trial. Arthritis Care Res. 2010;62(5):697–703.
[53]Lloréns R, Noé E, Colomer C, et al. Effectiveness, usability, and cost-benefit of a virtual reality-based telerehabilitation program for balance recovery after stroke: a randomized controlled trial. Arch Phys Med Rehabil. 2015;96(3):418–425.e2.
[54]Bos J, Armbrust W, Geertzen J, et al. PReS-FINAL-2148: Rheumates@work a cognitive behavioural internet based intervention promoting physical activity in children with juvenile idiopathic arthritis: Preliminary results of a randomized clinical trail. Pediatr Rheumatol. 2013;11(S2):160.
[55]Maloney S, Haas R, Keating J, et al. Effectiveness of web-based versus face-to-face delivery of education in prescription of falls-prevention exercise to health professionals: randomized trial. J Med Internet Res. 2011;13(4):e116.
[56]Marios T, Smart N, Dalton S. The effect of tele-monitoring on exercise training adherence, functional capacity, quality of life and glycemic control in patients with type II diabetes. J Sports Sci Med. 2012;11(1):51–56.
[57]Mitchell LE, Ziviani J, Boyd RN. A randomized controlled trial of web-based training to increase activity in children with cerebral palsy. Dev Med Child Neurol. 2016;58(7):767–773.
[58]Nijhof S, Bleijenberg G, Uiterwaal C, et al. Effectiveness of internet-based cognitive behavioural treatment for adolescents with chronic fatigue syndrome (FITNET): a randomised controlled trial. Lancet. 2012;379(9824):1412–1418.
[59]Nijhof S, Priesterbach L, Uiterwaal C, et al. Internet-based therapy for adolescents with chronic fatigue syndrome: long-term follow-up. Pediatrics. 2013;131(6):e1788–95.
[60]Palermo TM, Law EF, Fales J, et al. Internet-delivered cognitive-behavioral treatment for adolescents with chronic pain and their parents: a randomized controlled multicenter trial. Pain. 2016;157(1):174–185.
[61]Palermo TM, Wilson A, Peters M, et al. Randomized controlled trial of an Internet-delivered family cognitive-behavioral therapy intervention for children and adolescents with chronic pain. Pain. 2009;146(1–2):205–213.
[62]Pardo G, Thiessen A, Fjeldstad C. Telerehabilitation in multiple sclerosis: Results of a randomized, 3-arm, rater blinded, feasibility and efficacy pilot study; gait and balance report. Multiple Sclerosis Conference 32nd Congress European Committee for Treatment and Research in Multiple Sclerosis, ECTRIMS 2016, United Kingdom, Conference Start 20160914, Conference End 20160917; 2016. Vol. 22, p. 30.
[63]Piga M, Tradori I, Pani D, et al. Telemedicine applied to kinesiotherapy for hand dysfunction in patients with systemic sclerosis and rheumatoid arthritis: recovery of movement and telemonitoring technology. J Rheumatol. 2014;41(7):1324–1333.
[64]Piotrowicz E, Stepnowska M, Leszczyńska-Iwanicka K, et al. Quality of life in heart failure patients undergoing home-based telerehabilitation versus outpatient rehabilitation--a randomized controlled study. Eur J Cardiovasc Nurs. 2015;14(3):256–263.
[65]Brough C, Boyce S, Houchen-Wolloff L, et al. Evaluating the interactive web-based program, activate your heart, for cardiac rehabilitation patients: a pilot study. J Med Internet Res. 2014;16(10):e242.
[66]Sanford J, Griffiths P, Richardson P, et al. The effects of in-home rehabilitation on task self-efficacy in mobility-impaired adults: a randomized clinical trial. J Am Geriatr Soc. 2006;54(11):1641–1648.
[67]Sjöström M, Umefjord G, Stenlund H, et al. Internet-based treatment of stress urinary incontinence: a randomised controlled study with focus on pelvic floor muscle training. BJU Int. 2013;112(3):362–372.
[68]Sjöström M, Umefjord G, Stenlund H, et al. Internet-based treatment of stress urinary incontinence: 1- and 2-year results of a randomized controlled trial with a focus on pelvic floor muscle training. BJU Int. 2015;116(6):955–964.
[69]Sparrow D, Gottlieb D, Demolles D, et al. Increases in muscle strength and balance using a resistance training program administered via a telecommunications system in older adults. J Gerontol A Biol Sci Med Sci. 2011;66(11):1251–1257.
[70]Stinson J, Ahola Kohut S, Forgeron P, et al. The iPeer2Peer program: a pilot randomized controlled trial in adolescents with juvenile idiopathic arthritis. Pediatr Rheumatol. 2016;14(1):48.
[71]Stinson JN, McGrath PJ, Hodnett EE, et al. Feasibility testing of an online self-management program for adolescents with juvenile idiopathic arthritis (JIA): a pilot randomized controlled trial. Arthritis Rheum. 2009;60:238.
[72]Stinson JN, McGrath PJ, Hodnett E, et al. An internet-based self-management program with telephone support for adolescents with arthritis: a pilot randomized controlled trial. J Rheumatol. 2010;37(9):1944–1952.
[73]Trautmann E, Kröner-Herwig B. A randomized controlled trial of Internet-based self-help training for recurrent headache in childhood and adolescence. Behav Res Ther. 2010;48(1):28:37.
[74]Veroff DR, Ochoa-Arvelo T, Venator B. A randomized study of telephonic care support in populations at risk for musculoskeletal preference-sensitive surgeries. BMC Med Inform Decis Mak. 2013;13:21.
[75]Wang J, Cadmus-Bertram L, Natarajan L, et al. Wearable sensor/device (Fitbit One) and SMS text-messaging prompts to increase physical activity in overweight and obese adults: a randomized controlled trial. Telemed J E Health. 2015;21(10):782–792.
[76]Coulter E, McLean A, Hasler J, et al. The effectiveness and satisfaction of web-based physiotherapy in people with spinal cord injury: a pilot randomised controlled trial. Spinal Cord. 2017;55(4):383–389.
[77]Ammerlaan J, van Os-Medendorp H, Scholtus L, et al. Feasibility of an online and a face-to-face version of a self-management program for young adults with a rheumatic disease: experiences of young adults and peer leaders. Pediatr Rheumatol Online J. 2014;12:10.
[78]Arman N, Tarakci E, Tarakci D, et al. Effects of video games–based task-oriented activity training (Xbox 360 Kinect) on activity performance and participation in patients with juvenile idiopathic arthritis. Am J Phys Med Rehabil. 2019;98(3):174–181.
[79]Armbrust W, Bos GJFJ, Wulffraat NM, et al. Internet program for physical activity and exercise capacity in children with juvenile idiopathic arthritis: a multicenter randomized controlled trial. Arthritis Care Res. 2017;69(7):1040–1049.
[80]Raiszadeh K, Tapicer J, Taitano L, et al. In-clinic versus web-based multidisciplinary exercise-based rehabilitation for treatment of low back pain: prospective clinical trial in an integrated practice unit model. J Med Internet Res. 2021;23(3):e22548.
[81]Eberl R, Kaminski A, Reckwitz N, et al. The tele-visit as a telemedical technique in daily clinical practice. First results for elbow joint arthrolysis. Unfallchirurg. 2006;109(5):383–390.
[82]Ebert D, Tarnowski T, Gollwitzer M, et al. A transdiagnostic internet-based maintenance treatment enhances the stability of outcome after inpatient cognitive behavioral therapy: a randomized controlled trial. Psychother Psychosom. 2013;82(4):246–256.
[83]Fjeldstad C, Thiessen A, Pardo G. Telerehabilitation in multiple sclerosis: results of a randomized, 3-arm, rater blinded, feasibility and efficacy pilot study; patient-reported outcomes report. Multiple Sclerosis Conference 32nd Congress European Committee Treatment Research Multiple Sclerosis, ECTRIMS 2016, United Kingdom, Conference Start 20160914, Conference End 20160917; 2016. Vol. 22, p. 390.
[84]Frederix I, Hansen D, Coninx K, et al. Telerehab III: a multi-center randomized, controlled trial investigating the long-term effectiveness of a comprehensive cardiac telerehabilitation program--rationale and study design. BMC Cardiovasc Disord. 2015;15:29.
[85]Frevel D, Mäurer M. Internet-based home training is capable to improve balance in multiple sclerosis: a randomized controlled trial. Eur J Phys Rehabil Med. 2015;51(1):23–30.
[86]Aragones E, Lopez-Cortacans G, Caballero A, et al. Evaluation of a multicomponent programme for the management of musculoskeletal pain and depression in primary care: a cluster-randomised clinical trial (the DROP study). BMC Psychiatry. 2016;16(1):69.
[87]Baker K, Ledingham A, Lavalley MP, et al. Automated telephone-linked communication: a novel approach to enhance long-term adherence to resistance training exercise among people with knee osteoarthritis. Arthritis Rheum. 2013;65.
[88]Kosterink S, Huis In ’t Veld R, Cagnie B, et al. The clinical effectiveness of a myofeedback-based teletreatment service in patients with non-specific neck and shoulder pain: a randomized controlled trial. J Telemed Telecare. 2010;16(6):316–321.
[89]Latham NK, Harris BA, Bean JF, et al. Effect of a home-based exercise program on functional recovery following rehabilitation after hip fracture: a randomized clinical trial. Jama. 2014;311(7):700–708.
[90]Mecklenburg G, Smittenaar P, Erhart-Hledik JC, et al. Effects of a 12-week digital care program for chronic knee pain on pain, mobility, and surgery risk: randomized controlled trial. J Med Internet Res. 2018;20(4):e156.
[91]Rangarathnam B, McCullough G, Pickett H, et al. Telepractice versus in-person delivery of voice therapy for primary muscle tension dysphonia. Am J Speech Lang Pathol. 2015;24(3):386–399.
[92]Salaffi F, Carotti M, Ciapetti A, et al. Effectiveness of a telemonitoring intensive strategy in early rheumatoid arthritis: comparison with the conventional management approach. BMC Musculoskelet Disord. 2016;17:146.
[93]Salisbury C. Physiodirect telephone assessment and treatment services: results of a randomized controlled trial. Rheumatology. 2014;53(suppl_1):i24–i25.
[94]Salisbury C, Foster NE, Bishop A, et al. The MRC physiodirect trial: a pragmatic randomized controlled trial of physiodirect telephone assessment and advice services versus usual care for musculoskeletal problems. Rheumatology. 2012;51:iii36.
[95]Trudeau K, Pujol L, DasMahapatra P, et al. A randomized controlled trial of an online self-management program for adults with arthritis pain. J Behav Med. 2015;38(3):483–496.
[96]Williams D, Kuper D, Segar M, et al. Internet-enhanced management of fibromyalgia: a randomized controlled trial. Pain. 2010;151(3):694–702.
[97]Alasfour M, Almarwani M. The effect of innovative smartphone application on adherence to a home-based exercise programs for female older adults with knee osteoarthritis in Saudi Arabia: a randomized controlled trial. 2022;44(11):2420–2427.
[98]Barzel A, Ketels G, Stark A, et al. Home-based constraint-induced movement therapy for patients with upper limb dysfunction after stroke (HOMECIMT): a cluster-randomised, controlled trial. Lancet Neurol. 2015;14(9):893–902.
[99]Allen KD, Arbeeva L, Callahan LF, et al. Physical therapy vs internet-based exercise training for patients with knee osteoarthritis: results of a randomized controlled trial. Osteoarthritis Cartilage. 2018;26(3):383–396.
[100]Amorim AB, Pappas E, Simic M, et al. Integrating Mobile-health, health coaching, and physical activity to reduce the burden of chronic low back pain trial (IMPACT): a pilot randomised controlled trial. BMC Musculoskelet Disord. 2019;20(1):71.
[101]Azma K, RezaSoltani Z, Rezaeimoghaddam F, et al. Efficacy of tele-rehabilitation compared with office-based physical therapy in patients with knee osteoarthritis: a randomized clinical trial. J Telemed Telecare. 2018;24(8):560–565.
[102]Bennell KL, Nelligan RK, Rini C, et al. Effects of internet-based pain coping skills training before home exercise for individuals with hip osteoarthritis (HOPE trial). Pain. 2018;159(9):1833–1842.
[103]Bennell KL, Campbell PK, Egerton T, et al. Telephone coaching to enhance a home-based physical activity program for knee osteoarthritis: a randomized clinical trial. Arthritis Care Res. 2017;69(1):84–94.
[104]Calner T, Nordin C, Eriksson MK, et al. Effects of a self-guided, web-based activity programme for patients with persistent musculoskeletal pain in primary healthcare: a randomized controlled trial. Eur J Pain. 2017;21(6):1110–1120.
[105]Clark H, Bassett S, Siegert R. The effectiveness of web-based patient education and action and coping plans as an adjunct to patient treatment in physiotherapy: a randomized controlled trial. Physiother Theory Pract. 2019;35(10):930–939.
[106]Del Pozo-Cruz B, Parraca JA, Del Pozo-Cruz J, et al. An occupational, internet-based intervention to prevent chronicity in subacute lower back pain: a randomized controlled trial. J Rehabil Med. 2012;44(7):581–587.
[107]Devineni T, Blanchard EB. A randomized controlled trial of an internet-based treatment for chronic headache. Behav Res Ther. 2005;43(3):277–292.
[108]Gannon J, Atkinson JH, Chircop-Rollick T, et al. Telehealth therapy effects of nurses and mental health professionals from 2 randomized controlled trials for chronic back pain. Clin J Pain. 2019;35(4):295–303.
[109]Bini S, Mahajan J. Clinical outcomes of remote asynchronous telerehabilitation are equivalent to traditional therapy following total knee arthroplasty: a randomized control study. J Telemed Telecare. 2017;23(2):239–247.
[110]Hurkmans EJ, van den Berg MH, Ronday KH, et al. Maintenance of physical activity after Internet-based physical activity interventions in patients with rheumatoid arthritis. Rheumatology. 2010;49(1):167–172.
[111]Irvine AB, Russell H, Manocchia M, et al. Mobile-web app to self-manage low back pain: Randomized controlled trial. J Med Internet Res. 2015;17(1):e1.
[112]Kohns DJ, Urbanik CP, Geisser ME, et al. The effects of a pain psychology and neuroscience self-evaluation internet intervention. Clin J Pain. 2020;36(9):683–692.
[113]Kravitz RL, Schmid CH, Marois M, et al. Effect of mobile device-supported single-patient multi-crossover trials on treatment of chronic musculoskeletal pain: a randomized clinical trial. JAMA Intern Med. 2018;178(10):1368–1377.
[114]Lanhers C, Pereira B, Garde G, et al. Evaluation of ‘I-Preventive’: a digital preventive tool for musculoskeletal disorders in computer workers—a pilot cluster randomised trial. BMJ Open. 2016;6(9):e011304.
[115]Moessner M, Schiltenwolf M, Neubauer E. Internet-based aftercare for patients with back pain-A pilot study. Telemed J E Health. 2012;18(6):413–419.
[116]Nordin CA, Michaelson P, Gard G, et al. Effects of the web behavior change program for activity and multimodal pain rehabilitation: randomized controlled trial. J Med Internet Res. 2016;18(10):e265.
[117]Odole AC, Ojo OD. A telephone-based physiotherapy intervention for patients with osteoarthritis of the knee. Int J Telerehabil. 2013;5(2):11–20.
[118]Pariser D, O'Hanlon A. A. Effects of telephone intervention on arthritis self-efficacy, depression, pain, and fatigue in older adults with arthritis. J Geriatr Phys Ther. 2005;28(3):67–73.
[119]Prvu Bettger J, Green CL, Holmes DN, et al. Effects of virtual exercise rehabilitation in-home therapy compared with traditional care after total knee arthroplasty. J Bone Joint Surg Am. 2020;102(2):101–109.
[120]Boissy P, Tousignant M, Moffet H, et al. Conditions of use, reliability, and quality of audio/video-mediated communications during in-home rehabilitation teletreatment for postknee arthroplasty. Telemed J E Health. 2016;22(8):637–649.
[121]Riva S, Camerini AL, Allam A, et al. Interactive sections of an Internet-based intervention increase empowerment of chronic back pain patients: randomized controlled trial. J Med Internet Res. 2014;16(8):e180.
[122]Russell TG, Buttrum P, Wootton R, et al. Low-bandwidth telerehabilitation for patients who have undergone total knee replacement: preliminary results. J Telemed Telecare. 2003;9(2_suppl):44–47.
[123]Rutledge T, Atkinson JH, Holloway R, et al. Randomized controlled trial of nurse-delivered cognitive-behavioral therapy versus supportive psychotherapy telehealth interventions for chronic back pain. J Pain. 2018;19(9):1033–1039.
[124]Shigaki CL, Smarr KL, Siva C, et al. RAHelp: an online intervention for individuals with rheumatoid arthritis. Arthritis Care Res. 2013;65(10):1573–1581.
[125]Wijnen A, Hoogland J, Munsterman T, et al. Effectiveness of a home-based rehabilitation program after total hip arthroplasty driven by a tablet app and remote coaching: nonrandomized controlled trial combining a single-arm intervention cohort with historical controls. JMIR Rehabil Assist Technol. 2020;7(1):e14139.
[126]Ferwerda M, van Beugen S, van Middendorp H, et al. A tailored-guided internet-based cognitive-behavioral intervention for patients with rheumatoid arthritis as an adjunct to standard rheumatological care. Pain. 2017;158(5):868–878.
[127]Kloek CJJ, Bossen D, Spreeuwenberg PM, et al. Effectiveness of a blended physical therapist intervention in people with hip osteoarthritis, knee osteoarthritis, or both: a cluster-randomized controlled trial. Phys Ther. 2018;98(7):560–570.
[128]Kloek CJJ, van Tilburg ML, Staal JB, et al. Development and proof of concept of a blended physiotherapeutic intervention for patients with non-specific low back pain. Physiotherapy. 2019;105(4):483–491.
[129]Malfliet A, Kregel J, Meeus M, et al. Blended-learning pain neuroscience education for people with chronic spinal pain: randomized controlled multicenter trial. Phys Ther. 2018;98(5):357–368.
[130]Tavallaei V, Rezapour-Mirsaleh Y, Rezaiemaram P, et al. Mindfulness for female outpatients with chronic primary headaches: an internet-based bibliotherapy. Eur J Transl Myol. 2018;28(2):175–184.
[131]Carrión Pérez F, Rodríguez Moreno M, Carnerero Córdoba L, et al. Telerehabilitation to treat stress urinary incontinence. Pilot study. Med Clin. 2015;144(10):445–448.
[132]Suso-Ribera C, Castilla D, Zaragozá I, et al. Telemonitoring in chronic pain management using smartphone apps: a randomized controlled trial comparing usual assessment against app-based monitoring with and without clinical alarms. IJERPH. 2020;17(18):6568.
[133]Yuan SLK, Couto LA, Marques AP. Effects of a six-week mobile app versus paper book intervention on quality of life, symptoms, and self-care in patients with fibromyalgia: a randomized parallel trial. Brazilian J Phys Ther. 2020;25(4):428–436.
[134]Zheng F, Zheng Y, Liu S, et al. The effect of M-health-based core stability exercise combined with self-compassion training for patients with nonspecific chronic low back pain: a randomized controlled pilot study. Pain Ther. 2022;11(2):511–528.
[135]Chen P, Wei S, Hsieh W, et al. Lower limb power rehabilitation (LLPR) using interactive video game for improvement of balance function in older people. Arch Gerontol Geriatr. 2012;55(3):677–682.
[136]Eriksson L, Ekenberg L, Gard G, et al. Effects and patients’ experiences of telerehabilitation at home after shoulder joint replacement. Physiotherapy. 2011;97:eS1479.
[137]Grant JA, Mohtadi NG, Maitland ME, et al. Comparison of home versus physical therapy-supervised rehabilitation programs after anterior cruciate ligament reconstruction: a randomized clinical trial. Am J Sports Med. 2005;33(9):1288–1297.
[138]Hennig T, Haehre L, Hornburg V, et al. Effect of home-based hand exercises in women with hand osteoarthritis: a randomised controlled trial. Ann Rheum Dis. 2015;74(8):1501–1508.
[139]Allen KD, Sanders L, Olsen M, et al. Effectiveness of internet and DVD decision aids for patients with hip and knee osteoarthritis. Osteoarthr Cartil. 2014;22:S203.
[140]Antón D, Nelson M, Russell T, et al. Validation of a Kinect-based telerehabilitation system with total hip replacement patients. J Telemed Telecare. 2016;22(3):192–197.
[141]Polly DW. An internet-delivered cognitive-behavioral intervention with telephone support improved some coping skills in patients with chronic low back pain. J Bone Jt Surg Ser A. 2005;87(5):1169.
[142]Sathiyakumar V, Apfeld JC, Obremskey WT, et al. Prospective randomized controlled trial using telemedicine for follow-ups in an orthopedic trauma population: a pilot study. J Orthop Trauma. 2015;29(3):e139–e145.
[143]Tousignant M, Moffet H, Boissy P, et al. Patients and physiotherapists satisfaction of in-home telerehabilittion for post-knee arthroplasty. Physiotherapy. 2011;97:eS1246–eS1247.
[144]Tousignant M, Moffet H, Nadeau S, et al. Cost analysis of in-home telerehabilitation for post-knee arthroplasty. J Med Internet Res. 2015;17(3):e83.
[145]Levinger P, Hallam K, Fraser D, et al. A novel web-support intervention to promote recovery following anterior cruciate ligament reconstruction: a pilot randomised controlled trial. Phys Ther Sport. 2017;27:29–37.
[146]Uesugi Y, Koyanagi J, Takagi K, et al. Exercise therapy interventions in patients with hip osteoarthritis: Comparison of the effects of DVD and website-based interventions. JMIR Rehabil Assist Technol. 2018;5(1):e10.
[147]Wang J, Tong Y, Jiang Y, et al. The effectiveness of extended care based on Internet and home care platform for orthopaedics after hip replacement surgery in China. J Clin Nurs. 2018;27(21–22):4077–4088.
[148]Colomina J, Drudis R, Torra M, CONNECARE-Lleida Group, et al. Implementing mHealth-enabled integrated care for complex chronic patients with osteoarthritis undergoing primary hip or knee arthroplasty: prospective, two-arm, parallel trial. J Med Internet Res. 2021;23(9):e28320.
[149]Anan T, Kajiki S, Oka H, et al. Effects of an artificial intelligence–assisted health program on workers with neck/shoulder pain/stiffness and low back pain: randomized controlled trial. JMIR Mhealth Uhealth. 2021;9(9):e27535.
[150]Armbrust W, Bos J, Cappon J, et al. Design and acceptance of Rheumates@Work, a combined internet-based and in person instruction model, an interactive, educational, and cognitive behavioral program for children with juvenile idiopathic arthritis. Pediatr Rheumatol Online J. 2015;13:31.
[151]Cuperus N, van den Hout W, Hoogeboom TJ, et al. Cost-utility and cost-effectiveness analyses of face-to-face versus telephone-based nonpharmacologic multidisciplinary treatments for patients with generalized osteoarthritis. Arthritis Care Res. 2016;68(4):502–510.
[152]Davis M, Zautra A. An online mindfulness intervention targeting socioemotional regulation in fibromyalgia: results of a randomized controlled trial. Ann Behav Med. 2013;46(3):273–284.
[153]Gossec L, Servy H, Soubrier M, et al. Access to an active, interactive self-assessment e-health platform improves patient-physician communication in rheumatoid arthritis: Results of a randomized controlled trial including 320 patients over 1 year. Arthritis Rheumatol. 2016;68:1770–1771.
[154]Jay K, Schraefel M, Brandt M, et al. Effect of video-based versus personalized instruction on errors during elastic tubing exercises for musculoskeletal pain: a randomized controlled trial. Biomed Res Int. 2014;2014:790937.
[155]Langford D, Fleig L, Brown K, et al. Back to the future - feasibility of recruitment and retention to patient education and telephone follow-up after hip fracture: a pilot randomized controlled trial. Patient Prefer Adherence. 2015;9:1343–1351.
[156]Marsh J, Bryant D, MacDonald S, et al. Feasibility, effectiveness and costs associated with a web-based follow-up assessment following total joint arthroplasty. J Arthroplasty. 2014;29(9):1723–1728.
[157]Müller KI, Alstadhaug KB, Bekkelund SI. Acceptability, feasibility, and cost of telemedicine for nonacute headaches: a randomized study comparing video and traditional consultations. J Med Internet Res. 2016;18(5):e140.
[158]Moessner M, Aufdermauer N, Baier C, et al. Efficacy of an internet-delivered aftercare program for patients with chronic back pain. Psychother Psychosom Medizinische Psychol. 2013;64(2):47–53.
[159]Prochazka A, Kowalczewski J, Galea M. In-home tele-rehabilitation of the upper extremity. Physiotherapy. 2011;97:eS1022–eS1023.
[160]Sander L, Paganini S, Lin J, et al. Effectiveness and cost-effectiveness of a guided Internet- and mobile-based intervention for the indicated prevention of major depression in patients with chronic back pain-study protocol of the PROD-BP multicenter pragmatic RCT. BMC Psychiatry. 2017;17(1):36.
[161]Thurah A, Steengaard-Pedersen K, Axelsen M, et al. Tele-health follow-up strategy for tight control of disease activity in rheumatoid arthritis: results of the non-inferiority randomised controlled trail (the TeRA study). Arthr Care Res. 2017;76:454.2–455.
[162]Yen C-H, Lyu S-R, Hung S-S, et al. Telemedicine management with kinetic sensor for post-surgical knee osteoarthritis patients. Arch Phys Med Rehabil. 2017;98(10):e114.
[163]Zuidema R, van Gaal B, Meek I, et al. Effectiveness of an e-health tailored self-management program for patients with rheumatoid arthritis: an explorative Rct. Pediat Rheumatol. 2018;14:130.2–130.
[164]Allen KD, Woolson S, Hoenig HM, et al. Stepped exercise program for patients with knee osteoarthritis. Ann Intern Med. 2021;174(3):298–307.
[165]Allen KD, Woolson S, Hoenig HM, et al. Stepped exercise program for patients with knee osteoarthritis a randomized controlled trial. Ann Intern Med. 2021;174(3):298–307.
[166]Müller KI, Alstadhaug KB, Bekkelund SI. Telemedicine in the management of non-acute headaches: a prospective, open-labelled non-inferiority, randomised clinical trial. Cephalalgia. 2017;37(9):855–863.
[167]Salaffi F, Ciapetti A, Gasparini S, et al. Web/Internet-based telemonitoring of a randomized controlled trial evaluating the time-integrated effects of a 24-week multicomponent intervention on key health outcomes in patients with fibromyalgia. Clin Exp Rheumatol. 2015;33(1 Suppl 88):S93–101.
[168]De Oliveira Silva D, Pazzinatto M, Azevedo F, et al. Web-based multimedia education for people with patellofemoral pain: a preliminary analysis of a randomised controlled trial. J Sci Med Sport. 2018;21:S52–S53.
[169]Hadley C, McGrath M, Prodoehl JP, et al. Comparison of traditional physical therapy to internet-based physical therapy after knee arthroscopy: a prospective randomized controlled trial comparing patient outcomes and satisfaction. Orthop J Sport Med. 2019;7(suppl5):2325967119S0034.
[170]Mohsenolhosseini S. Efficacy of tele-rehabilitation compared with office-based physical therapy in patients with knee osteoarthritis: a randomized clinical trial. Ann Phys Rehabil Med. 2018;61:e6.
[171]Hospodarskyy A. Telerehabilitation of patients with injuries of the elbow joint of the upper extremities. Ann Phys Rehabil Med. 2018;61:e516.
[172]Ulcoq S, Hadley CJ, McGrath M, et al. Comparison of traditional physical therapy to internet-based physical therapy after knee arthroscopy: a prospective randomized controlled trial comparing patient outcomes and satisfaction. Arthrosc J Arthrosc Relat Surg. 2019;35(12):e5.
[173]Bennell KL, Nelligan R, Dobson F, et al. Internet-delivered exercise and pain-coping skills training for chronic knee pain. Ann Intern Med. 2017;166(7):453.
[174]Hedman-Lagerlöf M, Hedman-Lagerlöf E, Axelsson E, et al. Internet-delivered exposure therapy for fibromyalgia. Clin J Pain. 2018;34(6):532–542.
[175]Adeyemo WL, Akadiri OA. A systematic review of the diagnostic role of ultrasonography in maxillofacial fractures. Int J Oral Maxillofac Surg. 2011;40(7):655–661.