Abstract
Purpose
The study purpose was to, with the help of ICF and the CPS model, describe and explain patterns of co-occurring problems with participation in everyday life activities, body functioning and environment for children who completed brain tumor treatment.
Materials and methods
Hospital, habilitation and school records for nine children (5–11 yrs.) diagnosed with brain tumor, were retrospectively reviewed for everyday problems after treatment completion. These problems were linked to ICF codes. Median code distribution within ICF constructs participation, body function, body structure, activity, and environment were calculated to generate typical (close to median) and atypical (distant from median) patterns of problems on individual and group levels. Two children were in-depth analyzed with collaborative problem-solving (CPS) model to identify participation problems and plausible explanations.
Results
In total, 4543 ICF linked codes revealed similarities and differences between individuals. The selected child-cases displayed educational challenges and peer-relational problems. The ICF codes related to activity, body function and environment revealed plausible explanations for the children’s documented problems with participation in everyday life.
Conclusions
The combination of ICF and CPS can provide a comprehensive view of the child’s problems and guide development of participation in everyday life-focused interventions for children treated for brain tumors.
Care should be guided by interventions and support directed at individual children and their everyday life.
The International Classification of Functioning, Disability and Health (ICF) framework can support identification of the individual child’s patterns of problems and how these affects the child’s everyday life.
It is recommended to start by identifying participation problems when using ICF to identify and describe problems in children’s natural settings.
The collaborative problem-solving model can guide healthcare, habilitation and school services when identifying and acting on typical and atypical problem patterns experienced by these children.
Implications for rehabilitation
Introduction
All children are entitled to meaningful participation in home, school and leisure time situations [Citation1]. Participation in everyday life, is vital for children’s health and wellbeing and associated with positive academic performance and life satisfaction [Citation2,Citation3]. Participation, in International Classification of Functioning, Disability and Health (ICF) terms, is described as having two dimensions: “being there” during an activity and “being involved” in the activity. Participation in life situations occur in children’s interactions with their interpersonal, social and physical environments [Citation4].
Children who complete brain tumor treatment with surgery, chemotherapy and/or radiotherapy, often face problems in their everyday functioning. A problem can be defined as a perceived difference between the child’s current and desired state of functioning [Citation5]. Everyday life for children after brain tumor treatment is frequently characterized by restrictions in participation in life situations at home, in school and in leisure time. Limitations and impairments in cognitive, psychosocial, and physical functions [Citation6–8] often influence their full participation. Balance disturbance [Citation9], impaired vision [Citation10], pain [Citation11], and/or fatigue [Citation12] are common body function problems. However, participation restrictions also depend on environmental characteristics, such as peer interaction, adapted teaching material etcetera. Children who complete brain tumor treatment can experience lack of participation in peer interactions and social belonging during leisure activities. Experiences of participation restriction can negatively affect children’s emotional wellbeing and overall quality of life [Citation13,Citation14]. In addition, treatment-related impairments in short-term memory [Citation15], behavioral regulation [Citation16] and other aspects of executive functioning, contribute to challenges with learning. Problems tend to change and develop into individual patterns over time. When multiple problems co-occur, the combined effect on children’s functioning can be even greater [Citation17,Citation18].
After completing brain tumor treatment, children and their families seek a “new normal” that integrates their cancer experience [Citation19], changed roles and changed relationships [Citation20,Citation21]. Caregivers (parents) who focus on family functioning rather than on the brain tumor and its treatment, report better quality of life [Citation22]. Multi-professional follow-up care based on comprehensive assessment of the child’s needs [Citation23] and medical guidelines [Citation24], can guide the child and family. In Sweden, children with persistent functional problems in performing daily activities can access habilitation service as a supplement to health care [Citation25]. The habilitation service, with its multi-professional team, collaborates with the child and family to establish a specific habilitation plan with goals for developing skills applicable to everyday life. These plans aim to enhance participation and ultimately the child’s wellbeing [Citation26]. Swedish law requires that health care and habilitation plans should be established in dialogue with children and their caregivers [Citation27], and that provision of care in accordance with both plans must be documented in the child’s records [Citation25]. Children who experience problems reaching age-related educational goals following completion of treatment for brain tumor, often require additional educational adjustments. If these adjustments are insufficient to reach set goals, extra support is required, with a written action program to address the child’s needs [Citation28]. This program must be developed by the school’s health care team in collaboration with the child and family [Citation29]. However, coordination of plans between services is not mandated.
Services involved in the child’s care differ in how they perceive their tasks and goals, which is a barrier to collaboration. Health care aspires to identify and address tumor recurrence and treatment-related complications and therefore primarily focus on body functions; habilitation services aspire to restore the child’’s abilities to carry out activities of daily living; and schools aspire to support the child’s achievement of educational goals and social participation in school [Citation30,Citation31]. Ideally, shared goals can maximize the child’s health and functioning in everyday life. Barriers to collaboration within and between services towards achieving shared goals could be overcome by using the ICF [Citation32]. With its biopsychosocial lens, the ICF offers a universal language for describing a persons’ health and functioning in interdisciplinary and everyday settings, with a focus on how health conditions affect body functions, activity performance and participation in everyday activities [Citation32]. Within the ICF framework, body function refers to a persons’ physiological and psychological functioning; body structure to the bodily organ construct, and activity to a persons’ possibility to perform a task or an action; and participation to a persons’ involvement in life situations. Environmental factors include the environments a person operates within [Citation32]. Earlier studies of children treated for brain tumors have raised the awareness that the ICF is a useful tool to describe the child’s functioning, and can thus support plans of care [Citation20,Citation23]. Vanclooster et al. [Citation23] claims that child directed support, school staff attitudes, and collaboration in the network around the child, are beneficial for the child’s school functioning. Other studies highlight the importance of moving professionals’ focus from the child’s physical and psychological functioning to a more comprehensive focus on participation in everyday life [Citation31,Citation33]. However, the ICF is a descriptive classification system without guidelines for how to interpret relationships between the ICF components body, activity, participation and environment [Citation31]. In intervention work, causality is inferred by the timing of improvements in intervention targets relative to the results of prior evaluations and intervention delivery. Intervention can be described as the process of identifying a problem, finding explanations for the problem, setting goals for desired improvements, and implementing methods informed by the explanation and evaluating the outcome. Using participation in everyday life as the starting point, as suggested by prior research [Citation31,Citation33], a problem-solving strategy based on causal reasoning as applied to ICF, can be of use in developing interventions to enhance participation in everyday life.
Children who complete treatment for various types of brain tumors have individual patterns of co-occurring problems with participation, activity and body function. When the child has completed cancer therapy and re-entering everyday life, school-based and out-of-school services need to support re-entry and optimize participation. However, caregivers report lack of practical guidance about how best to support their child [Citation34]. One approach to enhance the child’s functioning in everyday life and allow the child’s voice to be heard throughout the intervention process, is the Collaborative Problem-Solving (CPS) Model [Citation35], see .
Figure 1. Illustration of the collaborative problem-solving model.
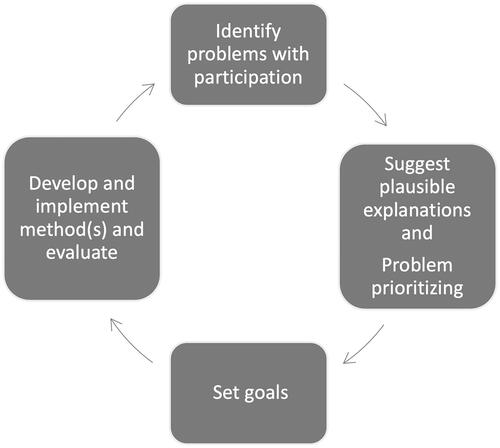
In this model, the child, their caregivers and other key actors in the child’s environments (e.g. school), collaborate to form partnerships that aim to maximize the child’s skills and thus everyday functioning [Citation35]. As the focus in this article is on everyday functioning, the starting point in the CPS model is identifying perceived problems with participation in the child’s everyday life, such as with peer-interactions or schoolwork, rather than the brain tumor or treatment-related complications. Plausible explanations for the identified problems relative to body function, activity performance and environment are named, and intervention targets are prioritized. Goals for increasing participation in these problematic areas are set and methods to reach the goals are developed. This step is followed by implementing methods and evaluating them regularly, and recognition of the outcomes and overall progress towards achieving the goals [Citation35]. Guided by evaluation results, new problems are identified, new goals set and revised, or new methods are implemented. The CPS model has been useful in developing interventions for children with functional limitations [Citation36].
Applying the CPS model to children treated for brain tumor and their parents, requires problem identification and problem solving based on an overview of the child’s participation in everyday activities. To gain an overview of the child’s pattern of problems, the child, caregivers and involved professionals from health care, habilitation and school discuss how the child’s problems in participation relate to problems with body function, activity performance, and facilitators and barriers in the environment. Most problems with participation have several explanations that can be orchestrated to generate a comprehensive view. For example, several reasons could explain why a child seldom finishes tasks in class. One explanation might be difficulty initiating the task or retaining focus; another might be that the teacher assigns tasks that are lengthy and complex; and a third might be that the environment does not provide clues regarding the order of the steps involved. By considering multiple plausible explanations, multiple methods can be applied to help the child reach their goal of completing tasks.
On an aggregate level, typical and atypical patterns of problems with body, activity and participation levels can be identified to guide further assessments and supports typically needed by children with a given medical history [Citation37]. Moreover, patterns of problems for an individual child can provide the basis for personalized interventions. Problems tend to co-occur, possibly due to shared mechanisms that are modifiable. Synergistic interactions among co-occurring problems can intensify adverse effects on functioning beyond what is seen when the problem stands alone [Citation38]. If a problem is targeted for intervention without assessing whether it is part of a pattern of co-occurring problems with shared mechanisms, sustainable effects can be difficult to achieve. Sustainable effects likely require that interventions targeted toward several plausible explanations [Citation39]. Furthermore, intervening without considering the possibility of co-occurrences, could inadvertently worsen the child’s situation. Thus, it is important to identify patterns of problems on an individual basis. Some patterns of co-occurring problems may be typical for persons with a specific health history such as brain tumor and referred to as typical patterns. Other patterns may be highly individual and referred to as atypical patterns. Therefore, patterns of co-occurring problems related to body function, activity, participation, and environment for an individual child, must be identified to form the basis of multi-level (child plus one or more levels of the child’s environment) interventions that maximize the child’s functioning and participation in everyday life.
As concluded in Björklund et al. [Citation31], the first study in this research project, a gap exists in our understanding of the trajectories and modifiable mechanisms underlying patterns of problems with participation in everyday life among children who completed treatment for brain tumor. The combination of ICF and the CPS model could guide healthcare, habilitation and school services in closing this gap when identifying and intervening to address typical and atypical problem patterns experienced by these children.
Purpose
The purpose of this study was to, with the help of ICF and the CPS model, describe and explain patterns of co-occurring problems with participation in everyday life activities, body functioning and environment for children who completed brain tumor treatment.
The research questions were:
What individual variations are seen in proportions of documented problems with participation, activity, body function and environment for the children?
What typical and atypical patterns of co-occurring problems with everyday functioning are illustrated by exemplary child cases?
How can the CPS model be used to explore problems with activity, bodily function and in the child’s environments as plausible explanations for problems with participation?
Materials and methods
Design
The study used a retrospective case design [Citation40]. The ICF framework was used to guide coding of documented problems in nine children’s records, and the selection of two child cases that illustrate children with typical and atypical patterns of co-occurring problems. Thereafter, the CPS model was used to explore co-occurring problems with activity, body function and environment as underlying mechanisms that could explain these two children’s problems with participation.
Sample
The study used convenience sampling for recruitment of children who had (a) been diagnosed with a brain tumor between the ages of 5 and 15 years, (b) successfully completed oncological treatment, and (c) performed post-treatment neuro-psychological assessment. More information about the participant and recruitment strategies are described in Björklund et al. [Citation31].
Setting
Children who had received brain tumor treatment at either of two oncology departments in Mid-Sweden, were followed up at related municipal hospitals, and attended mainstream schools. These two oncology departments yearly provide care for a total of 50 children diagnosed with a primary brain tumor. The oncology departments are responsible for overall medical management, which usually includes surgical removal of the tumor, followed by radiotherapy and/or chemotherapy as indicated by surgical margins, and characteristics of the child and the tumor. Care for acute and long-term complications associated with cancer therapy is given at related municipal hospitals. Habilitation services complement medical care by supporting rehabilitation of the child’s ability to perform activities of daily living. School is responsible for providing children with the knowledge required according to the school law, and to provide the support needed for students that have difficulties with reaching the national goals for education.
Data collection
Data were collected between May 2018 and March 2019. The first author (A–CB) examined documentation in healthcare, habilitation and school records, for nine children’s problems with everyday life to identify descriptions of problems. As the same children were documented in all three services, descriptions of problems were aggregated across services rather than per professional category. These records were written by physicians, nurses, psychologists, physiotherapists, occupational therapists, teachers and other professionals. A problem was defined as a perceived difference between the child’s present and desired state of functioning [Citation5]. Data were extracted for the period of time between the first neurocognitive assessment, usually about a year after treatment completion, through the data collection date. Median follow-up time of extracted data was 4.4 years after the first neuropsychological evaluation, range 2.7 − 10.4 years.
Data analysis
Descriptive statistics were used to characterize the sample. To identify individual variations of problems in the documentation, problems were linked to ICF codes within the components body function, body structure, activity, participation, and environmental factors. For example, extracted text (meaning units) described that the child had problems with headaches. The meaning of the problem was thus identified “headache” which was linked to the most precise ICF chapter (b2 sensory functions and pain) and ICF code (b280 sensation of pain). More information about the linking process is described in Björklund et al. [Citation31]. A previous child and youth version of ICF (ICF-CY) was merged into the ICF classification in 2012. However, some child-specific codes are not included in the current ICF classification [Citation41]. One of these codes from ICF-CY, a250 managing one’s own behavior was used in the analysis for the current study. The code featured prominently and thus was included here, despite not being part of the updated ICF classification. After linking extracted text from all services to ICF codes, proportions and median proportions of ICF codes within components, were calculated on both the individual child levels and the group level. The most frequently occurring codes identified for all services concerned body function, followed by activity codes (31). Thus, codes were aggregated for all services instead of per profession or service type. The activity/participation domain was divided into activity codes (chapters 1 – 4 in the domain) and participation codes (chapters 5 – 8 in the domain) based on a recommendation in the ICF manual on how to separate activity (performing an activity) from participation (involvement in a life situation).
To identify typical and atypical patterns of co-occurring problems in the study sample, each child’s code distribution was compared to the group median of codes within the ICF components body function, body structure, activity, participation and environmental factors. Based on visual inspection of deviations from the median value for all nine cases, deviations of 5% from the median proportion of codes within each component generated one plus or one minus. For each additional 5% deviation, an additional + or – was added. The 5% deviations were chosen for the sensitivity to detect differences between individuals while preserving the group patterns constructed from the descriptive statistics of code frequency described in Björklund et al. 2021 [Citation31]. Similar reasoning was used in Olsson et al. [Citation42]. Based on the code distributions, two children were selected for in depth examination of their typical (close to median) or atypical (distant from median) pattern of problems and given pseudonyms – “Alice” for the child with the typical pattern and “Peter” for the child with the atypical pattern.
Alice and Peter’s data were subjected to deductive content analysis [Citation43], guided by the CPS model, to generate plausible explanations for the child’s problems with participation within the child’s co-occurring body function, activity and environmental problems [Citation35]. In this study, only the first two steps of the CPS model () defining problems and plausible explanations, were applied. In the first step of the analysis, identified meaning units and assigned ICF codes for the two child cases were read through several times, to gain a deeper understanding of individual problems. In the second step, recurring ICF codes within the components body function, activity, participation, and environmental factors were noted. In the third step, problems assigned to participation codes were identified from the ICF code set as problems linked to p5-p9 (self-care, domestic life, interpersonal interactions and relationships, major life areas and community life) as the initial base for analyzing the pattern of problems. In the fourth step, meaning units linked to the ICF components activity, body function and environment were identified as plausible explanations related to identified participation problems. The component body structure was excluded in this analysis as anatomical focus is not within the realm of CPS. In the fifth step, the identified patterns of problems and plausible explanations were labeled with names that illustrated the participation problem. The process of identifying pattern of problems was done in collaboration by authors A-CB and MB. The remaining steps of CPS, goal setting and designing and implementing intervention methods were deemed unnecessary based on the retrospective approach applied in this study.
Ethical considerations
The study was approved by the Ethical Review Board in Linköping, Sweden (Dnr 2017/475-31). Depending on the child’s age at time of entry to the study, written parental permission and child assent or informed consent for the child’s participation in the study were obtained prior to collecting the child’s data, in accordance to ethical guidelines [Citation44]. Considering the sample size, details about participant characteristics in the following text are sparse to protect the children’s privacy.
Results
The nine children in the study sample were diagnosed with a brain tumor between 5–11 years of age. Slightly more than half of the children were males (5/9). The majority were diagnosed during their pre-school years (6/9), had the tumor type medulloblastoma (6/9), astrocytoma (2/9) or craniopharyngioma (1/9). They were treated with surgery and/or chemotherapy and/or radiation in different combinations.
In total, 4543 single and repeated ICF linked codes within body function, body structure, activity, participation and environmental factors were identified from the extracted text. See for the most common codes within ICF chapters and components.
Table 1. The most frequently linked ICF codes within components.
Variations in proportions of children’s problems with body function, body structure, activity, participation and environment
The results reveal that variations in the proportions of documented problems were related to body function, body structure, activity, participation and their environment. When comparing the proportion for each child’s codes to the proportion for the group, different patterns emerged (). displays the nine children’s deviations from the median for the ICF components, symbolized with either pluses or minuses.
Table 2. Code distribution in relation to median for each of the children.
The number of plus and minus symbolize the size and direction of deviations in ICF components for each child compared to median proportions for the group. Some children differed less in relation to the group (child 1–5, 8). These children displayed a similar pattern of + and - in the different ICF components and were deemed as displaying a typical pattern of problems. Other children (child 6, 7, 9) differed more relative to the group and were therefore deemed as displaying an atypical pattern of problems.
Typical and atypical patterns illustrated by exemplary child cases
Two children were selected as exemplars based on the results shown in . Alice’s (child 4) typical pattern of problems differed only slightly from the children with a typical pattern of problem when compared to median proportion in several components. Peter (child 7) displayed an atypical pattern deviated particularly in the body function and activity components compared to the group (). The distribution of codes within ICF components identified in Alice and Peter’s documentation indicates both similarities and differences compared to the group.
Alice exemplifying typical patterns of problems
Alice was diagnosed at pre-school age and treated with surgery and radiotherapy. Documentation about Alice encompassed four years of compulsory schooling. In total, 414 ICF codes were identified in the analysis of documentation about Alice. Sixteen codes related to body structure, which were excluded from the total sample, as previously explained. There were 59/414 codes related to participation, 70/414 codes related to activity, 240/414 to body function and 45/414 codes related to the environment. The greatest proportion of Alice’s ICF linked problems (296/430), were in documentation from health care, while 111/430 were in documentation from school and 23/430 in documentation from habilitation; habilitation services were involved for a shorter period of time than health care or school services. While most codes related to body function components, many codes also related to activity, participation, and environment, especially among problems documented by health care services and school professionals.
Peter exemplifying atypical patterns of problems
Peter was also diagnosed at pre-school age and treated with surgery, chemotherapy and radiotherapy. He presented an atypical pattern of problems in relation to the distribution of codes in all children described in . Documentation spanning seven years from preschool to compulsory school were collected. In Peters case, a distribution of 396 ICF codes were identified, 15 codes related to body structure were excluded from the final sample. There were 26/396 codes related to participation. Activity accounted for the greatest proportion of codes 153/396 which was a marked deviation relative to the other children’s codes. Body function were the most frequently identified codes 172/396, which was a lower proportion compared to the other children. The proportion of environmental codes 45/396 resembled the group median. Most problems (359/411) were detected in health care documents while problems identified in habilitation (27/411) and school (25/411) documents were relatively sparse.
Using the CPS model to explore explanations for problems with participation
The results of the analysis to identify typical and atypical patterns of co-occurring problems with everyday functioning exposed Alice and Peter’s considerable problems with participation in school. Thus, we explored if the CPS model could be used to identify plausible explanations for both children’s problems with participation in school.
Plausible explanations for alice’s problems with participation in school
Alice problems with participation in school (p820) co-occurred with problems with daily routines, problems with carrying out tasks, problems with basic learning activities, problems with vision-demanding activities and moving around, and problems with interpersonal relationships.
Problems with daily routines linked to school
One plausible explanation for Alice’s problems with participation in school were her problems with carrying out daily routines (a230) and managing one’s own behavior (a250). Alice had difficulties with medication adherence, completing homework and arriving late to school or missing school due to staying up too late. Another plausible explanation for Alice’s problems with participation in school were her problems with sleep functions (b134). She had difficulty falling asleep in the evenings and with waking in the night, which contributed to problems with energy and drive functions (b130). Alice therefore had difficulty getting up in the mornings due to tiredness and needed to rest or sleep after school.
Problems carrying out tasks in school
Plausible explanations for Alice’s problems carrying out tasks in school included problems with focusing attention (a160) and directing attention (a161). Alice had documented difficulties perceiving context and listening to instructions without interrupting or forgetting what she was told to do. Alice’s problems with focus and attention might also explain her documented difficulties undertaking a single task (a210) without assistance. Plausible explanations could also be found in codes within the body function component, where Alice had documented problems with memory functions (b144) as she could not remember content covered previously. Furthermore, documentation revealed plausible explanations for participation problems in the environment component - Alice had documented problems related to sound (e250) in the classroom. Her sensitivity to auditory stimuli, for example, led to disrupted focus on reading tasks.
Problems with basic learning activities in school
Several plausible explanations emerged related to Alice’s problems with basic learning activities in school. For example, Alice had documented problems acquiring concepts (a137), displayed by delayed development of vocabulary and word mobilization. Alice also had documented difficulties learning to read (a140), which could explain her difficulty with maintaining flow of reading a text; reading (a166). Writing (a170) was also a documented problem for Alice, specifically writing capital letters, remembering to put periods at the end of sentences, and staying on topic. Furthermore, Alice had difficulty calculating (a172), understanding arithmetic, and telling time using a clock. The documentation also revealed plausible explanations related to communication with-receiving-spoken messages (a310), described as Alice having difficulty with phonological word flow, retelling, explaining what she meant and producing words.
Problems with vision-demanding activities and moving around in school
Documented problems with Alice’s vision also provided plausible explanations for problems with participation in school. For example, Alice had documented difficulty running during physical education (PE) due to visual impairment, unstable gait and frequent stumbling. These problems had bodily explanations related to seeing functions (b210) and functions of structures adjoining the eye (b215). Alice had impaired visual fields resulting in difficulty catching balls in PE and performing other tasks that required both peripheral and central vision. Plausible explanations related to Alice’s school environment include inattention to people in positions of authority (e330) and individual attitudes of friends (e420) concerning the appearance of Alice’s eyes and her gaze. Documentation also noted Alice’s problems watching movies in the classroom even if placed up front, which related to problems with products and technology for education (e130).
Plausible explanations for Alice’s documented problems with moving around include impaired balance as Alice stumbled and was uncoordinated, as shown by codes for involuntary movement reaction functions (b755), control of voluntary movement functions (b760), and sensation related to muscles and movement functions (b780).
Other plausible explanations for Alice’s problems participating in vision-demanding activities, as well as moving around at school, related to the natural environment and human-made changes to environment, other specified (e298), documented as difficulty walking on uneven surfaces due to visual impairment.
Problems with interpersonal relationships
One plausible explanation for Alice’s problems with participation in school was her problems with interpersonal relationships both within and outside of her family – temperament and personality functions (b126). This was shown by the documentation of Alice “ruling” over her family, (e310). The documentation showed that her parents had difficulty setting boundaries for Alice’s behavior and daily routines such as coming in time to school, because they felt sympathy for Alice being “sick” and worried about her tumor recurring.
Other plausible explanations for Alice’s problems with interpersonal relationships are problems managing (her) behavior (a250). The documentation revealed that instructions from peers during play, and by their expectations about taking turns and compromising caused Alice to easily get upset. This problem can also be plausibly explained by her temperament and personality functions (b126). An example of this is Alice’s being stubborn and determined, and in a moody and uncooperative state, especially when “uncomfortable” things came up during interactions with peers. Plausible explanations related to the environmental component include attitudes of friends (e420), documented as reports that friends were not nice to her in play during breaks and by insufficient education and training services, systems, and policies (e585), documented as parents’ concerns about lack of action by school professionals, despite multiple meetings.
Plausible explanations for peter’s problems with participation in school
Peter’s problems with participation in school (p820) co-occurred with problems with basic learning activities, which led to difficulties achieving educational goals in some subjects.
Problems with basic learning activities in school
Possible explanations for Peter’s problems with participation in school were problems with basic learning activities. The documentation showed problems with reading (a166), writing (d170) and fine hand use (a440). Peter’s problems related to reading were described as difficulty with decoding words, reading speed and understanding the text. Peter had difficulty writing on paper and at the computer. The problems with reading and writing contributed to problems handling stress and other psychological demands (a240). Peter cried about having to write and that completing his homework took a lot of time, which meant less time with friends. These problems had possible bodily explanations within psychomotor functions (b147) in that Peter was described as being low in cognitive processing speed. Environmental explanations for Peter’s problems with basic learning activities related to people in position of authority (e330), where professionals in habilitation service had documented problems that should have been addressed in school, but were not. School staff did not encourage Peter to use the technical aids provided by school and habilitation nor did teachers collaborate to assist him, which relates respectively to products and technology for education (e130) and to education and training services, systems and policies (e585). Environmental explanations also related to Peter’s immediate family (e310) in that the school’s lack of engagement in Peter’s problems led to parents placing excessive demands on him regarding homework.
Discussion
Children in the study sample displayed various patterns of co-occurring problems based on code proportions relative to ICF component median values. The fact that several patterns are also found within this small sample, stress the importance of looking at individual patterns when assessing and intervening for everyday functioning across both home/family, leisure and school environments. The variability in patterns highlights the importance of investigating how co-occurring problems affect the child’s participation in everyday life on individual level, as illustrated by the two exemplar cases. Patterns of co-occurrence can inform hypothetical explanations for the child’s diminished functioning related to activity performance, physical-, psychological- and environmental factors. As argued by Rusk et al. [Citation39], problems with everyday functioning tend to have multiple causes. If interventions target too few of the causes, treatment effects are unlikely to be sustained over time. Moreover, improvements may not lead to meaningful differences in the child’s ability to participate in everyday life. Long-term complications among children treated for brain tumors are usually presented on a group level and in relation to tumor type and treatment exposures, including risk for secondary health conditions and poorer quality of life compared to healthy age peers [Citation13,Citation17]. However, these group patterns do not consider the similarities and differences within the individual child’s pattern of problems and seldom illustrate the critical role that the child’s environments play in activity limitations and participation restrictions. As proposed by Wallander [Citation37] as early as 1998, children with different types of disorders share difficulties with everyday functioning. Thus, interventions have to be designed to address the child’s pattern of problems in activity and participation, in addition to medical problems such as features of the tumor and of the medical treatment.
The results of the current study showed that Alice and Peter both experienced school-related problems. Problems reaching educational goals after treatment for a brain tumor is consistent with earlier Nordic studies that found that children treated for brain tumor had poorer grades than healthy peers [Citation45–47]. The reasons for poorer grades include problems with daily routines leading to late arrival or absence from school [Citation48]. Another explanation, also seen in the exemplar cases, related to late bedtime or disrupted night-sleep at home, leading to tiredness [Citation49]. Daytime sleepiness is a feature of the “cancer-related fatigue” that commonly occurs in cancer populations, particularly those treated for a brain tumor [Citation12], and has consistently been associated with poorer quality of life [Citation50,Citation51]. Documentation directly investigating how impaired sleep and tiredness are related to school achievement should be of concern for families and professionals [Citation52].
While children typically view re-entry to school after treatment completion with positive feelings related to reconnecting with friends and participating in school activities [Citation53], symptoms like tiredness can led to absenteeism. School staff may tolerate absenteeism given the child’s medical history, although Swedish law requires school age child to regularly attend school. Irregular school attendance presents challenges for the development of individual educational plans and, perhaps more importantly, peer relationships. Peer relationships serve as a link between out of school contexts like family and school. School staff must involve not only the child but also the family in the process of school re-entry. Engaged parents with knowledge of strategies which support their child in daily processes and school issues (e.g. learning tools, educational resources) can enhance the child’s developmental progress and school functioning [Citation54]. This study illuminates the need for collaboration among the child and family, health care, habilitation and school. Collaboration is a prerequisite to obtaining a comprehensive view of the child’s co-occurring problem patterns and to establish priorities for orchestrated complex interventions that target body function, activity and environment. Collaboration will ultimately support the child’s educational achievement and overall wellbeing.
Children’s cognitive functioning is closely linked to educational achievement [Citation55]. In the present study, Alice and Peter both had difficulty with basic learning (reading, writing and math) and with executive functions. Problems with remembering appointments or the steps in a task were highlighted, as were problems with paying attention to instructions and regulating behavior to task. These challenges for children with brain tumors are consistent with the literature [Citation56,Citation57] and indicate a need for adapting learning activities to the cognitive functioning of the individual child.
The child’s environment interacts with overall functioning to influence the child’s activity performance and participation in everyday life. The results of this study show that problems detected in the environmental component were related to barriers restricting the child’s capacity for key functions of everyday life, such as carrying out daily routines. Some children may need environmental support, e.g. social scripts, to carry out daily routines. Furthermore, parents worry about tumor recurrence and sympathy for the child, may lead to challenges setting expectations and boundaries for the child’s behavior. Parents of children treated for cancer experience challenges creating a new normal that acknowledges both the possibility of recurrence and hope for a full life [Citation21,Citation58]. Environmental problems related to the school system, use of individualized supports (e.g. use of adapted material, individualized schedule) and attitudes of school staff and friends, were also highlighted.
In this study, Alice (the child with typical patterns of co-occurring problems) displayed problems with social interaction, felt lonely and had no friends to engage in play in school. Explanations found in documentation describing the child’s behavior as “ruling”, being stubborn and moody with peers. Similar behaviors have been described in previous studies reporting poor social relationships among children treated for brain tumors [Citation59]. The results of neuropsychological assessments by training health professionals can help school staff understand how the child’s cognitive functioning can affect their social interactions and pinpoint strategies designed to mitigate risk for social isolation [Citation59]. However, these kinds of interventions demand that assessments include the school environment and the child’s social interactions and not only neuropsychological assessment of the child. These additional assessments are necessary to determine how to best manage problems with cognitive functioning given the context. Additionally, interactions in the family environment should be discussed with child and the family. Earlier findings highlight that the child’s behavior can generate conflicts within the family, more specifically between child-parents and child-siblings [Citation21]. Therefore, parents and children may need assistance transitioning to life after the cancer, where parental distress frequently concerns navigating child-parent conflicts and conflicts between siblings [Citation60].
The collaborative problem-solving model was applied to the current study with the intention to identify patterns of co-occurring problems within activity, body function and environmental areas, that might explain the problems with participation. The problems with activity, body and environment are thus considered as being plausible explanations to participation problems. If professionals in health care, habilitation and school define problems based solely on the focus of their discipline, the overall pattern of the child’s everyday functioning in context may be overseen. Therefore, supportive care following the ending of a cancer directed treatment should be individually tailored to individual needs based on experienced everyday problems, in context [Citation55]. A comprehensive view of the child’s everyday problems requires that the child, parents, and school staff are involved in defining the problems before detailing an intervention based on the child’s experienced problems. That will enhance the child’s health and wellbeing as well as inclusive education with lifelong learning, which is in line with the UN′s declaration on the rights of the child [Citation1] and the sustainable developmental goals 2030 [Citation61].
This study is based on an analysis of child problems documented in medical, habilitation and school records rather than soliciting child-reported experiences. This approach raises the question of whether children’s voice were considered and the extent of their involvement in the collaborative problem-solving process. Studies based on growth curve modelling by Dunst and his colleagues [Citation62,Citation63] show that families report higher wellbeing and better child functioning when they have collaborated with professionals in a family centred fashion. This type of approach includes active involvement of child and parents throughout the process, from defining and prioritizing among problems evaluating the effects of interventions on individual and family functioning and wellbeing [Citation62]. In a Swedish study, Huus et al. [Citation64] reported that parents of children with mild intellectual disability who rated the support from social and habilitation services as very useful, also rated a lower need for support and higher parenting self-efficacy. To further conclude from Dunst et al. [Citation62] it seems like child and care-provider involvement in the intervention development process improves the feasibility and acceptability of the intervention to them. This in turn improves enactment of the intervention and ultimately the effects on wellbeing. The identified patterns in the present study, describing co-occurring problems across ICF domains, indicate that the CPS model might provide a framework for obtaining a comprehensive view of the problems experienced by children who have completed treatment for brain tumor. Application of the CPS model should begin with problems with participation, that is, contextualized descriptions of problems with everyday functions. This everyday perspective is where children and families are the experts. The combination of the use of ICF and CPS framework were used in this study to explore the possibility of using them together in future research that involves children in identifying and prioritizing problems, and then generating methods to increase their participation in everyday life with the support of caregivers and other stakeholders.
Methodological considerations
This study selected two children from the study sample as exemplars of typical and atypical patterns of co-occurring problems. The sample included children of various ages who underwent treatment of different types of brain tumors. Overall treatment was intensive in that all of the children were treated using at least two modalities, and the children were diagnosed and treated during their pre-school years; these factors placed the children at heightened risk for future problems with participation in daily life. The children came from a geographically wide ranging area of Sweden that included urban and urban-rural areas, which facilitates generalization of the results. While other high-income countries may currently use different guidelines for long-term follow up care and documentation in service records, harmonization efforts are underway.
The positioning of a child’s pattern of problems as typical or atypical based analyses of documentation in records for nine children must be considered. The study findings illustrate similarities and differences in the pattern of co-occurring problems on individual child and group levels. Each child’s problem pattern is unique to that child. However, the analyzed documents describe results of standardized psychometric assessments and professionals’ interpretations of caregiver/child descriptions. Thus, the circumstances in the environments around the child are missing and documentation in the child’s records might not fully capture the child’s experience with everyday life. Moreover, documentation in records does not ensure representation of the child’s voice. Earlier studies testify that professionals are hesitant to document sensitive psychosocial issues in the child’s records [Citation65], and prefer to transmit this type of information verbally [Citation66]. Bear in mind that the main purpose of professional’s documentation is to capture information to inform the child’s care, and, in some countries, justify billing, not for research. Nevertheless, documentation conveyed the focus and outcomes of encounters between the child, their parents and professionals involved in the child’s care. The authors (A-CB & MB) extensive experience in caring for children with cancer may have interpreted identification of problems in the documents and code linking of text. The coding and linking process was time- and labor intensive, which complicates the feasibility of ICF implication in larger samples and in clinical arenas and schools. However, the analytic process was discussed with all co-authors, two of whom (LD & SJS) also have substantial expertise in comprehensive care and research of children diagnosed with cancer and their families.
Conclusion
This study illustrates the complexity of problems seen in children following successful completion of treatment for brain tumor. Similarities and differences are seen within and between patterns of co-occurring problems at group level. This complexity requires that professionals carefully reflect on each child’s unique pattern of problems with participation in daily life and how various problems co-occur. Using ICF in combination with CPS provides a more comprehensive view of the child’s problem with participation, which can then be prioritized and targeted with multiple component interventions.
Acknowledgements
We are grateful to the children, adolescents and parents that consented review of the child’s documentation from health care services, habilitation and school. We also thank the staff who facilitated the data collection at the different sites.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- United Nations Convention on the Rights of the Child (UNCRC). Convention of the rights of the child New York: United Nations; 1989 [cited 2021 Sep 17]. Available from: https://www.unicef.org.uk/what-we-do/un-convention-child-rights/.
- de Róiste A, Kelly C, Molcho M, et al. Is school participation good for children? Associations with health and wellbeing. Health Education. 2012;112(2):88–104.
- Alerby E, Bergmark U. Delaktighet för lärande. Stockholm: Skolverket; 2015 (Forskning för skolan).
- Imms C, Granlund M, Wilson PH, et al. Participation, both a means and an end: a conceptual analysis of processes and outcomes in childhood disability. Dev Med Child Neurol. 2017;59(1):16–25.
- Ylven R, Granlund M, Persson C. Problem solving in relation to resources in everyday life in families of children with disabilities: a pilot study. Int J Rehabil Res. 2012;35(2):102–108.
- Robinson KE, Kuttesch JF, Champion JE, et al. A quantitative meta-analysis of neurocognitive sequelae in survivors of pediatric brain tumors. Pediatr Blood Cancer. 2010;55(3):525–531.
- Stavinoha PL, Askins MA, Powell SK, et al. Neurocognitive and psychosocial outcomes in pediatric brain tumor survivors. Bioengineering. 2018;5(3):73.
- Sato I, Higuchi A, Yanagisawa T, et al. Impact of late effects on Health-Related quality of life in survivors of pediatric brain tumors: motility disturbance of limb(s), seizure, ocular/visual impairment, endocrine abnormality, and higher brain dysfunction. Cancer Nurs. 2014;37(6):E1–E14.
- Varedi M, Lu L, Phillips NS, et al. Balance impairment in survivors of pediatric brain cancers: risk factors and associated physical limitations. J Cancer Surviv. 2021;15(2):311–324.
- Nuijts MA, Degeling MH, Stegeman I, et al. Visual impairment in children with a brain tumor: a prospective nationwide multicenter study using standard visual testing and optical coherence tomography (CCISS study). BMC Ophthalmol. 2019;19(1):220–220.
- Johnson AH, Jordan C, Mazewski CM. Off-Therapy headaches in pediatric brain tumor patients: a retrospective review. J Pediatr Oncol Nurs. 2009;26(6):354–361.
- Irestorm E, Tonning Olsson I, Johansson B, et al. Cognitive fatigue in relation to depressive symptoms after treatment for childhood cancer. BMC Psychol. 2020;8(1):31–31.
- Gunn ME, Malila N, Lahdesmaki T, et al. Late new morbidity in survivors of adolescent and young-adulthood brain tumors in Finland: a registry-based study. Neuro Oncol. 2015;17(10):1412–1418.
- Ness K, Gurney JGP, Zeltzer LKMD, et al. The impact of limitations in physical, executive, and emotional function on health-related quality of life among adult survivors of childhood cancer: a report from the childhood cancer survivor study. Arch Phys Med Rehabil. 2008;89(1):128–136.
- Araujo GC, Antonini TN, Anderson V, et al. Profiles of executive function across children with distinct brain disorders: traumatic brain injury, stroke, and brain tumor. J Int Neuropsychol Soc. 2017;23(7):529–538.
- Salley CG, Hewitt LL, Patenaude AF, et al. Temperament and social behavior in pediatric brain tumor survivors and comparison peers. J Pediatr Psychol. 2015;40(3):297–308.
- Boman KK, Hoven E, Anclair M, et al. Health and persistent functional late effects in adult survivors of childhood CNS tumours: a population-based cohort study. Eur J Cancer. 2009;45(14):2552–2561.
- Oeffinger KC, Mertens AC, Sklar CA. Chronic health conditions in adult survivors of childhood cancer. Oncology Times. 2007;29(1):26–26.
- Clarke-Steffen L. A model of the family transition to living with childhood cancer. Cancer Pract. 1993;1(4):285–292.
- Ajovalasit D, Vago C, Usilla A, et al. Use of ICF to describe functioning and disability in children with brain tumours. Disabil Rehabil. 2009;31(sup1):S100–S107.
- Björk M, Nordström B, Wiebe T, et al. Returning to a changed ordinary life – families’ lived experience after completing a child’s cancer treatment. Eur J Cancer Care. 2011;20(2):163–169.
- Deatrick JA, Barakat LP, Knafl GJ, et al. Patterns of family management for adolescent and young adult brain tumor survivors. J Fam Psychol. 2018;32(3):321–332.
- Vanclooster S, Van Hoeck K, Peremans L, et al. Reintegration into school of childhood brain tumor survivors: a qualitative study using the International Classification of Functioning, Disability and Health – children and youth framework. Disabil Rehabil. 2021;43(18):2610–2620.
- Regionala cancercentrum i samverkan. Nationellt vårdprogram långtidsuppföljning efter barncancer 2019 [cited 2021 Jan 10]. Available from: https://kunskapsbanken.cancercentrum.se/diagnoser/langtidsuppfoljning-efter-barncancer/vardprogram/.
- SFS (2017:30). Hälso- och sjukvårdslagen [Health and Medical Service Act]. Stockholm: Socialdepartementet;2017. Swedish.
- Wettergren BMD, Blennow MMD, Hjern AMD, et al. Child health systems in Sweden. J Pediat. 2016;177(Suppl):S187–S202.
- SFS (2014:821). Patientdatalag [The patient record data law]. Stockholm: Socialdepartementet [Ministry of Health and Social Affairs]; 2014. Swedish.
- Swedish National Agency for Education. Support activities in school – what do I need to know as parent?; 2015 [cited 2022 Feb 19]. Available from: https://www.skolverket.se/download/18.6bfaca41169863e6a65b87a/1553966180451/pdf3477.pdf.
- SFS (2010:800). Den nya skollagen - för kunskap, valfrihet och trygghet [Education Act]. Stockholm: Utbildningsdepartementet;2010. Swedish.
- Strand A-SM, Granlund M. The school situation for students with a high level of absenteeism in compulsory school: is there a pattern in documented support? Scand J Educ Res. 2014;58(5):551–569.
- Björklund A-C, Granlund M, Santacroce SJ, et al. Using ICF to describe problems With functioning in everyday life for children who completed treatment for brain tumor: an analysis based on professionals’ documentation. Front Rehabil Sci. 2021;2(45):708265.
- World Health Organization. International classification of functioning, disability and health (ICF) Geneva2001 [cited 2021 Jan 4]. Available from: https://apps.who.int/iris/bitstream/handle/10665/42407/9241545429.pdf.
- Backman E, Granlund M, Karlsson A-K. Documentation of everyday life and health care following gastrostomy tube placement in children: a content analysis of medical records. Disabil Rehabil. 2020;42(19):2747–2757.
- Inhestern L, Peikert ML, Krauth KA, et al. Parents’ perception of their children’s process of reintegration after childhood cancer treatment. PLOS One. 2020;15(10):e0239967–e0239967.
- Björck-Åkesson E. The ICF-CY and collaborative problem solving in inclusive early childhood education and care. In Castro S, Palikara O, editors. An emerging approach for education and care: implementing a worldwide classification of functioning and disability. London, [England] Routledge; 2018. p. 134–146.
- Johnson M, Ostlund S, Fransson G, et al. Attention-deficit/hyperactivity disorder with oppositional defiant disorder in Swedish children – an open study of collaborative problem solving. Acta Paediatr. 2012;101(6):624–630.
- Wallander JL, Varni JW. Effects of pediatric chronic physical disorders on child and family adjustment. J Child Psychol Psychiatry. 1998;39(1):29–46.
- Sameroff AJ, Seifer R, Barocas R, et al. Intelligence quotient scores of 4-year-old children: social-environmental risk factors. Pediatrics. 1987;79(3):343–350.
- Rusk RD, Vella-Brodrick DA, Waters L. A complex dynamic systems approach to lasting positive change: the synergistic change model. J Positive Psychol. 2018;13(4):406–418.
- Taylor R, Thomas-Gregory A. Case study research. Nurs Stand. 2015;29(41):36–40.
- Noten S, Troenosemito LAA, Limsakul C, ICF Core Set for Adults with Cerebral Palsy Study Group, et al. Development of an ICF core set for adults with cerebral palsy: capturing their perspective on functioning. Dev Med Child Neurol. 2021;63(7):846–852.
- Olsson C. The use of communicative functions among pre-school children with multiple disabilities in two different setting conditions: group versus individual patterns. AAC. 2005;21(1):3–18.
- Elo S, Kyngas H. The qualitative content analysis process. J Adv Nurs. 2008;62(1):107–115.
- SFS (2003:460). Lagen om etikprövning av forskning som avser människor [The Ethical Review Act]. Stockholm: Utbildningsdepartementet;2003. Swedish.
- Ahomaki R, Harila-Saari A, Matomaki J, et al. Non-graduation after comprehensive school, and early retirement but not unemployment are prominent in childhood cancer survivors—a Finnish registry-based study. J Cancer Surviv. 2017;11(2):284–294.
- Lönnerblad M, Van’t Hooft I, Blomgren K, et al. A nationwide, population-based study of school grades, delayed graduation, and qualification for school years 10–12, in children with brain tumors in Sweden. Pediatr Blood Cancer. 2020;67(2):e28014.
- Andersen KK, Duun-Henriksen AK, Frederiksen MH, et al. Ninth grade school performance in Danish childhood cancer survivors. Br J Cancer. 2017;116(3):398–404.
- Yilmaz MC, Sari HY, Cetingul N, et al. Determination of school-related problems in children treated for cancer. J Sch Nurs. 2014;30(5):376–384.
- Brimeyer C, Adams L, Zhu L, et al. Sleep complaints in survivors of pediatric brain tumors. Support Care Cancer. 2016;24(1):23–31.
- van Kooten JAMC, Maurice-Stam H, Schouten AYN, et al. High occurrence of sleep problems in survivors of a childhood brain tumor with neurocognitive complaints: the association with psychosocial and behavioral executive functioning. Pediatr Blood Cancer. 2019;66(11):e27947.
- Macartney G, VanDenKerkhof E, Harrison MB, et al. Symptom experience and quality of life in pediatric brain tumor survivors: a cross-sectional study. J Pain Symptom Manage. 2014;48(5):957–967.
- af Sandeberg M, Johansson E, Björk O, et al. Health-related quality of life relates to school attendance in children on treatment for cancer. J Pediatr Oncol Nurs. 2008;25(5):265–274.
- Vanclooster S, Bilsen J, Peremans L, et al. Attending school after treatment for a brain tumor: experiences of children and key figures. J Health Psychol. 2019;24(10):1436–1447.
- Patel SK, Johansen C, Gold AO, et al. Social-ecological predictors of school functioning in Hispanic children treated for cancer with central nervous system–directed therapies. Pediatr Blood Cancer. 2020;67(10):e28320.
- Nicklin E, Velikova G, Hulme C, et al. Long‐term issues and supportive care needs of adolescent and young adult childhood brain tumour survivors and their caregivers: a systematic review. Psychooncology. 2019;28(3):477–487.
- Barkon B. Learning profiles of survivors of pediatric brain tumors. Phys Disabil. 2009;28(1):34.
- de Ruiter MA, van Mourik R, Schouten-van Meeteren AY, et al. Neurocognitive consequences of a paediatric brain tumour and its treatment: a meta-analysis. Dev Med Child Neurol. 2013;55(5):408–417.
- Sundler AJ, Hallström I, Hammarlund K, et al. Living an everyday life through a child’s cancer trajectory: families’ lived experiences 7 years after diagnosis. J Pediatr Oncol Nurs. 2013;30(6):293–300.
- Schulte F, Brinkman TM, Li C, et al. Social adjustment in adolescent survivors of pediatric central nervous system tumors: a report from the childhood cancer survivor study. Cancer. 2018;124(17):3596–3608.
- Schepers SA, Okado Y, Russell K, et al. Adjustment in childhood cancer survivors, healthy peers, and their parents: the mediating role of the parent-child relationship. J Pediatr Psychol. 2019;44(2):186–196.
- United Nations. Sustainable development goals; 2015 [cited 2022 Feb 2]. Available from: https://sdgs.un.org/goals.
- Dunst CJ. Implications of Evidence-Based practices for personnel preparation development in early childhood intervention. Infant Young Child. 2009;22(1):44–53.
- Dunst CJ, Trivette CM, Hamby DW. Meta-Analysis of studies incorporating the interests of young children with autism spectrum disorders into early intervention practices. Autism Res Treat. 2012;2012:462510–462531.
- Huus K, Olsson LM, Elgmark Andersson E, et al. Perceived needs among parents of children with a mild intellectual disability in Sweden. SJDR. 2017;19(4):307–317.
- Ståhl Y, Granlund M, Simeonsson R, et al. Psychosocial health information in free text notes of Swedish children’s health records. Scand J Caring Sci. 2013;27(3):616–623.
- Clausson EK, Berg A, Janlöv A-C. Challenges of documenting schoolchildren’s psychosocial health: a qualitative study. J Sch Nurs. 2015;31(3):205–211.
