Abstract
Objective
This longitudinal case study describes the physical and occupational therapy interventions and recommendations for treatment of a person with bilateral transradial amputations during subacute rehabilitation, as there are currently few recommendations.
Materials and methods
A 53-year-old female with subacute bilateral transradial amputations received inpatient rehabilitation. Impairments include decreased balance, global weakness, and need for assistance with ADLs and transfers. Physical therapy, occupational therapy, nursing, a peer mentor, and a prosthetist collaborated. Interventions included task-specific and generalized strengthening, standing balance re-education, assistive device prescription, education using body-powered prostheses, home adaption recommendations, and activities of daily living practice.
Results
Patient progressed to independent functional mobility but required assist for activities of daily living and stairs negotiation due to limited caregiver support and poor prosthetic dexterity. She discharged to a skilled nursing facility.
Conclusion
Rehabilitation of a person with bilateral transradial amputations requires clinicians experienced with prostheses; excellent interdisciplinary coordination; early discernment of the available social support system; task-specific strengthening and coordination exercises to prepare the patient for prostheses; significant task-practice with prostheses; and a working knowledge of home modifications and adaptive equipment. This article describes recommendations, successful interventions, and lessons learned for future therapists when rehabilitating someone with bilateral transradial amputations.
Bilateral transradial amputations (BTAs) are a life-altering, but rare condition, meaning that literature surrounding this population is sparse and that guidelines for rehabilitation are unclear.
This article provides recommendations so that clinicians can be better informed when treating BTA patients in the subacute phase and more quickly progress patients toward functional independence and discharge to the community.
IMPLICATIONS FOR REHABILITATION
Introduction
Impact statement
The recommendations provided should enable clinicians working with the bilateral transradial amputee population to progress a patient more quickly toward functional independence and discharge to the community.
Background
Bilateral transradial amputations (BTAs) are life-changing [Citation1–5]. Common etiologies for upper extremity (UE) amputations are trauma, cancer, infections, burns, congenital deformities, and vascular disease [Citation4,Citation6–8], with vascular disease being the most common cause of amputations [Citation3]. Dillingham et al. determined that between 1988 and 1996, the number of vascular-related amputations had increased [Citation3]. In addition, the number of individuals with peripheral vascular disease and diabetes continues to rise significantly [Citation9,Citation10], with diabetics being 10–25 times more likely than non-diabetics to receive an amputation [Citation11]. It is paramount for clinicians to understand rehabilitation for individuals with amputations, as the number of amputees may rise in the future [Citation4].
Transradial amputations are the second most common type of UE amputation after finger amputations, with transradial amputations accounting for 15% of all amputations [Citation4,Citation11]. Ziegler-Graham notes that 8% of the UE amputee population has a major amputation (excludes finger amputations), but it is unknown how many of these are bilateral [Citation4]. BTAs are rare and literature is sparse regarding rehabilitating individuals with BTAs with no specific guidelines [Citation12,Citation13]. This case study describes the rehabilitation of a diabetic patient with vascular-related BTAs and suggests recommendations for clinicians who rehabilitate persons with BTAs.
Materials and methods
Case description
The authors obtained informed consent for photos and videos from the participant.
The patient is a 53-year-old female who was admitted to an inpatient rehabilitation unit during Autumn of 2020 after a left transradial amputation status post left-hand necrosis. Five months earlier, she underwent a right transradial amputation and now had BTAs. Both amputations were initially caused by a wound on her hand. Due to her diabetes, proper wound healing did not take place, and she developed osteomyelitis, necessitating amputations. lists the patient’s demographics and social history further.
Table 1. Patient background information.
Tests and measures
See for a comprehensive list of the tests and measures taken upon initial evaluation and discharge. The tests and measures utilized focused on objective and functional tools and included: Manual muscle testing, sensation and balance assessments, and assistance level required for bed mobility, transfers, gait, stair negotiation, grooming, bathing, toileting, dressing, and eating.
Table 2. Evaluation and discharge measurements.
Study design
Since BTAs are a rare condition, finding a large sample size of this population would have been extremely difficult. Therefore, it is appropriate to use a case study design.
Interventions
Experts in amputation rehabilitation were contacted including a peer mentor, physical therapists, and occupational therapists (OTs) with experience treating persons with quadruple limb amputations. Information was also gathered via journal articles [Citation14–17] and YouTube.com©, where persons with amputation(s) demonstrated functional activities.
OT emphasized UE and core strengthening, completing ADLs, and prostheses training. Physical therapy (PT) practiced LE strengthening, ambulation including device prescription, and strengthening and coordination exercises to improve efficiency with prostheses. Both disciplines worked on improving functional mobility and endurance. PT obtained ankle straps for cable column use (Nylon Ankle Straps, Iron Bull, Sherbrooke, Quebec, Canada) and retrofitted them as forearm cuffs for use with a cable column and resistance bands (Rep Band latex-free exercise bands, Denver, Colorado, USA) for core, scapular, and UE strengthening. See Supplementary Tables 3 and 4 for detailed descriptions of PT and OT interventions.
Additional interdisciplinary interventions contributed to the rehabilitation of this patient. The patient received a body-powered prosthesis early in her rehabilitation stay. A wearing schedule was posted in her room to encourage nursing staff to gradually increase the wearing time of the UE prosthesis until she was wearing it for most of the day. Educational pictures and instructions for nursing staff and PRN therapists of how to don and doff the UE prosthesis were also posted in the patient’s room. When it became apparent that this patient’s core strength was too limited for her to learn to don/doff her prosthesis while it was lying on a bed or couch, a blunted hook was installed on the wall so the patient could learn donning and doffing her prosthesis in standing.
The peer mentor was an individual with bilateral UE amputations: one transhumeral and one transradial. He was present during therapy sessions one to two times weekly to provide emotional encouragement to this patient, demonstrate expert functioning of a body-powered prosthesis, and suggest alternatives in environmental setup of activities for ease of skill acquisition during PT and OT sessions. Although the peer mentor was available to provide emotional and psychological support to the patient during this time of transition, the patient demonstrated excellent acceptance and coping skills with the challenges her amputations caused, likely due to presence of a strong faith tradition (patient’s occupation was that of a pastor).
The prosthetist was also present one to two times weekly to make adjustments to the body-powered prosthesis, including altering harness strap length for efficiency managing the terminal device and ease of donning/doffing; addition of a wrist friction flexion joint; exchanging of terminal device from a cosmetic grasping hand to a more functional hook; and shortening of forearm socket length so as not to compress the patient’s dialysis port when elbow was in 90 degrees or more of flexion.
Our goal and our hypothesis was for the patient to spend a maximum of 3 weeks in inpatient rehabilitation with intensive PT, OT, and nursing care before discharging directly home and demonstrating independent functional mobility and requiring intermittent assistance for all ADLs.
Results
Initial evaluations
PT and OT evaluations revealed deficits in functional mobility, ADLs, strength, balance, and pain. Both surgical and phantom pain were present, but rated low, likely due to the patient’s premorbid peripheral neuropathy from diabetes resulting in distal numbness of her extremities. details the patient’s impairments and functional limitations. The patient’s vital signs varied due to the amount of fluid removed during dialysis. The patient’s goals were to eat, bathe, toilet, and dress independently.
Prosthesis selection and modification
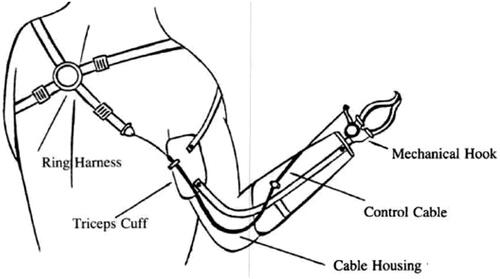
The patient trialed several prostheses. The prosthesis she chose was a preparatory body-powered system with voluntary opening hooks for improved function (). During her stay, a flexion friction wrist joint was added that could lock at 0, 30, and 50 degrees of flexion, and could fixate at any degree of pronation or supination. The prosthetist adjusted the amount of friction needed to rotate and flex the wrist until the ideal setting for patient preference was achieved. A peer mentor with bilateral UE amputations was present for 1–2 sessions per week to aid the patient in using the prosthesis for functional tasks.
Figure 1. UE prosthesis apparatus. Based on the positioning of the ring harness, straps, and triceps cuff on the posterior torso and upper arm, scapular protraction will increase tension on the control cable. This tension on the control cable facilitates opening of the mechanical hook. A neutral scapula slackens the control cable and the mechanical hook closes. Scapular retraction will allow the mechanical hook to remain closed. Upper Limb Prosthesis Devices. Teodiano Freire Bastos-Filho, Dinesh Kumar, Sridhar Poosapadi Arjunan. Devices for Mobility and Manipulation for People with Reduced Abilities (Rehabilitation Science in Practice Series). Poosapadi Arjunan, Sridhar; Kant Kumar, Dinesh; Bueno, Leandro; Villarejo Mayor, John J.; Bastos Filho, Teodiano F, 2014, by permission of Dr. John Jairo Villarejo Mayor. This image is not covered by the terms of the Creative Commons license of this publication. For permission to reuse, please contact the rights holder.
Outcomes
The patient received inpatient rehabilitation for 32 days. She improved significantly with her functional mobility in all areas except stairs. She improved with her standing balance and strength, demonstrated by initial inability to complete the Timed Up and Go and Five Times Sit to Stand outcome measures, and then improving to scores of 14 s for each outcome measure, indicating reduced risk of falls in the older adult and geriatric population by time of discharge [Citation18,Citation19]. The patient’s activity tolerance also demonstrated significant improvement, evidenced by an initial 6 min Walk Test of 80 ft, which improved to a score of 300 ft by time of discharge, which exceeds the minimally clinically important difference of 164 ft in the older adult and geriatric population [Citation20]. Lastly, the patient’s surgical pain decreased with healing of her wounds and her already low levels of phantom limb pain transitioned primarily into reports of phantom limb sensation by the end of her rehabilitation stay. She lacked independence with her ability to use her prosthesis and therefore, her ability to perform ADLs, especially toileting and dressing, causing her to discharge to a skilled nursing facility. details her impairment and functional-level outcomes.
Discussion
Because the patient did not achieve a level of independence with eating, bathing, toileting, dressing, and stairs, the hypothesis was not met, and the patient discharged to a skilled nursing facility.
The primary reason she did not discharge home was her lack of independence with toileting. Although copious time was spent teaching toileting techniques, toileting was not consistently practiced with prostheses. OT created a custom toileting aide from thermoplastic splinting material in a 90-degree hook configuration, that would stay by the toilet so the patient would not have to don her prostheses every time she toileted, which was a concern for nighttime toileting needs. This hook shape was designed to accommodate the patient’s abdominal pannus and short residual limbs to access her perineal region for hygiene. This was unsuccessful because the patient could not adequately handle toilet paper using the toileting aide. Others with BTAs use an anterior perineal hygiene technique where they obtain toilet paper with their toes, place it on the anterior rim of the toilet, and sit on the toilet paper to wipe. This patient lacked the toe dexterity, LE range of motion (ROM) and strength, and balance to practice this technique. The function of a prosthetic hook is needed for toilet paper usage and pants/underwear management when toileting [Video 1]. A rehab facility should consider obtaining a bidet, which would significantly reduce the burden of care with hygiene.
Dressing was another challenge. The patient learned upper body dressing (UBD) without prostheses, as prostheses are donned after UBD. With practice using excessive head and trunk movements for a shake pull-down method, the patient could independently don a large t-shirt [Video 2]. The patient was unable to don a sports bra, her premorbid clothing preference, independently due to its tight-fitting nature. An option for future clinicians to trial for donning sports bras in this population is a wrap-around sports bra that is modified with loops sewn to the lateral edges of the sports bra so the patient would potentially be able to don it with her residual limbs. A custom UE dressing tree was being fabricated when the patient discharged to a SNF but had potential to improve the patient’s ease of UBD. Following this patient’s discharge, wall mounted dressing hooks were discovered as viable adaptive equipment that others with BTAs use for lower body dressing (LBD), and could have potentially been used for UBD, as well. OT recommended wearing a camisole or no bra, which the patient refused.
For LBD, without prostheses, OT trialed donning pants with residual limbs in pockets and inside of elastic waist pants, but she could not pull them over her hips. She had more success with pulling up pants modified with lateral and posterior loops sewn on, but still needed assist to pull over her hips. Without a prosthesis, LBD wall hooks must be used to pull pants and underwear over and off hips. Significant coordination and understanding of a body powered prosthetic cable system is required for pants management with prostheses [Video 3]: the terminal device grasps and releases by placing tension on the cables with scapular protraction. When the patient reaches posteriorly for her pants, the ipsilateral scapula retracts, requiring the contralateral scapula to protract to achieve cable tension. The prosthesis’ wrist joint must also be in a flexed position for this. A body-powered prosthetic cable system functions best in a 2-foot by 2-foot area directly in front of the patient’s torso, which is what makes hygiene and pants management with toileting extremely difficult. Ultimately, the patient could not perform LBD with body-powered prostheses due to the rigorous scapular coordination requirements, decreased LE and core strength, and obesity. OT recommended wearing a pull-over dress without underwear to make LBD and toileting easier, but the patient refused.
Although the patient lacked mastery of prostheses use, her dressing needs could have been met with intermittent caregiver assist at the beginning and end of the day. However, the pants management required for toileting could only have been satisfied with clothing and environmental modification such as use of a bidet combined with wearing a dress without underwear or with a live-in caregiver.
Showering was another limitation for discharge. Due to low endurance, OT recommended a transfer tub bench. Many bathing techniques were trialed; a long-handled sponge (LHS) with a modified bent handle was helpful but attaching this device to the patient’s residual limb was difficult. OT trialed CobanTM (3M, United States) to attach the LHS to her residual limb, but the patient still needed minimal assistance (MinA) to clean her perineal and buttock area because the handle was not rigid enough to remain attached during hygiene. The patient also tried sitting on a sponge with multi-directional weight shifts to clean her perineal area. Although able to perform this technique, it proved laborious. The patient could have bathed at home with assistance, but support was unavailable.
Lastly, the patient achieved independent eating with use of universal cuffs (Universal Cuff Utensil Holder – Adjustable Cuff, Ableware Company, Wayne, New Jersey, USA) [Video 4]. The patient would have ideally progressed to independent eating with her prostheses [Video 5], but OT interventions did not routinely occur during mealtimes due to scheduling limitations and extensive effort required when the patient was hungry. The patient would have benefited from consistently eating with prostheses with nursing or OT. Her peer mentor recommended eating 50% of the meal before practicing with prostheses to avoid frustration.
The authors devised recommendations for future clinicians working with individuals with BTAs:
Incorporate prosthesis practice early and consistently [Citation21]. Focus on ADLs, especially toileting and eating. Practice eating with prostheses with a trained therapist or nursing staff for each meal. Teach placing utensils at correct angles for eating and managing the top harness straps which must be moved anterior to the shoulder to allow increased ROM for utensils to reach the mouth. Build up endurance as it takes extra energy to eat with prostheses; a minimum of 10 h of practice is required to see improvement with prosthesis usage [Citation22]. Use of a universal cuff is an effective regression, although the lumen of the universal cuff needed to be modified/tightened into a smaller opening to maintain its grip on the utensils during eating.
Practice donning/doffing prostheses—from wall hooks or supine on bed. This can be done with prostheses set up on the bed/couch, hanging from two blunted hooks with long projections on the wall, or with use of an UBD tree. Preservation of residual limb length allows generation of greater force due to longer lever-length, which improves the functional utility of a prosthesis [Citation5]. However, a longer residual limb will require greater glenohumeral and spinal ROM to don the UE prostheses. Without hooks or a dressing tree, significant core strength and coordination is required to don the prosthesis in standing [Video 6, Video 7].
Trial home modifications during rehab. Home modifications have been found to be useful in increasing functional independence and reducing falls in both the elderly and lower extremity amputee population and have potential to do the same for the UE amputee population [Citation23,Citation24]. Two recommendations are trialing a bidet during toileting and use of a LHS with bent and fortified handle to promote thorough cleaning, but a sturdy strapping system to the residual limb is needed. There are also YouTube® video examples of extensive home bathroom modifications including built in benches with pump soap dispenser holders in the shower for foot access, shower wall mounted loofas/sponges for trunk cleaning, an additional foot faucet inside the shower for those who use their feet to manipulate objects, and full body air dryers to eliminate the need for towel drying.
Involve a peer mentor from the amputee population, preferably someone with BTAs. A peer mentor can promote confidence, discuss expectations, and recommend prosthesis techniques. It is important to evaluate and treat the psychological impact of BTAs and a peer mentor is uniquely positioned to provide empathy and encouragement to a person with BTAs [Citation21].
Incorporate UE, core, and LE resistance training [Citation21]. Prostheses are heavy, which make prosthesis management difficulty with weak core and UE musculature. Patients must maximize LE strength to improve capacity for toileting, LBD, and stair/ramp negotiation.
Perform therapy with prostheses in every session [Citation21]. The patient used her prosthesis only half of the time which may explain why she did not achieve independence with her prosthesis. Work quickly to accommodate the patient’s body to wearing prostheses most of the day [Citation21]. Post a schedule in the patient’s room so clinicians can document prostheses don/doffing times.
Consider use of an ambulatory assistive device [Citation21]. Rollators and platform rolling walkers are viable options to improve balance for people with BTAs, as they can rest their elbows on the assistive device to support themselves and provide proprioception necessary for balance. This option is especially important for people with BTAs who have poor LE strength and balance, and, prior to their amputations, relied heavily on their UEs for functional activities. Assistive devices may even be necessary in the short term for those with BTAs that have good LE strength, as a bilateral amputation may alter the individual’s center of gravity and cause imbalances. An assistive device can minimize these imbalances while the individual adjusts to their new center of gravity.
Hold a family conference early to clarify the expected level of assist needed at discharge [Citation21]. Having a well-planned discharge plan promotes therapy tailored towards achieving independence in necessary ADLs. The level of assistance available must be clear. A live-in caregiver is recommended at discharge for everyone with new BTAs, but it is possible for a person with new BTAs to live alone, despite lacking proficiency with prostheses, if they have intermittent ADL assistance and adaptive equipment. The rehabilitation team must be clear with the patient and caregivers regarding expected level of assist needed at discharge and help the patient set realistic short- and long-term goals [Citation21].
Use an experienced prosthetist and limit changing prosthetic design. A prosthetist experienced with UE prostheses can determine the most comfortable and functional preparatory prosthetic components, design, and fit to the patient [Citation5]. A harness-based suspension system is a versatile option for those with BTAs and traditionally uses a body-powered prosthesis with a distal hook that opens or closes based on a person’s residual limb movement [Citation5]. Given the substantial practice required to obtain proficiency using UE prostheses, it is important to limit changing this design.
Long-term follow-up
This patient discharged to a skilled nursing facility, where she continued to receive rehabilitation for 23 days and then discharged home. Once home, she resumed home health occupational therapy and PT and received assistance from family members for instrumental activities of daily living. Approximately 3 months following discharge from inpatient rehabilitation, this patient received her definitive prostheses, which were myoelectric prostheses with Ottobock Bebionic (Ottobock, Austin, Texas, USA) hands. These hands have 14 different grip patterns and independent finger motion making them highly functional. To receive myoelectric prostheses, this patient’s prosthetist explains that a patient must show that she can operate a myoelectric prosthesis, has a need to complete tasks that require operating a prosthesis outside of a 2-foot by 2-foot window in front of the torso, will benefit from different grip patterns, and meets the minimum microvolt threshold to operate. The myoelectric prostheses typically use a skin suction suspension system so that the patient’s skin will contact the electrodes inside of the prostheses to read the muscle firing signals [Citation5]. The patient uses alcohol rub over her arms and then slides her residual limbs into the socket. Suction sockets use a one-way valve to create a vacuum between a prosthesis and a residual limb, which then creates a seal holding the prosthesis in place [Citation5]. This patient’s myoelectric prostheses do not have wrist rotators, as this requires an additional microprocessor unit, and only one microprocessor code can be delivered at one time for each amputated side. However, her technician who made her myoelectric prostheses left space for this additional microprocessor unit in case it needed to be added later, but this would also add additional weight to the prostheses.
There were limitations to this study. Due to the paucity of research surrounding rehabilitation of individuals with BTAs, there were limited innovative interventions that could be created and trialed. Additionally, due to the lack of information available from peer-reviewed research, there does not exist a robust plan for rehabilitating individuals with BTAs, and thus, the patient’s quality of care could have been better had a robust plan existed. It is the hope of these authors that this case study provides framework for a robust plan of care and options for innovative interventions for future clinicians who may rehabilitate individuals with BTAs. Due to the rare nature of BTAs, the authors were unable to rehabilitate any other patients with BTAs, preventing this article from becoming a case series which has stronger clinical implications than a case study. Therefore, this individual’s course of rehabilitation may not accurately reflect that of the general population with BTAs.
In conclusion, the intent of this article is to offer interventions, recommendations, and realistic expectations for patients with BTAs and guide clinicians to maximize therapy time during inpatient rehabilitation.
Supplemental Material
Download MS Word (28.5 KB)Acknowledgements
The authors of the study wish to acknowledge Stephen Shope, the peer mentor, for his assistance and education guiding each of us during this patient’s rehabilitation journey.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Bastidas N, Cassidy L, Hoffman L, et al. A single-institution experience of hand surgery litigation in a major replantation center. Plast Reconstr Surg. 2011;127(1):284–292.
- Mattiassich G, Rittenschober F, Dorninger L, et al. Long-term outcome following upper extremity replantation after major traumatic amputation. BMC Musculoskelet Disord. 2017;18(1):77.
- Dillingham TR, Pezzin LE, MacKenzie EJ. Limb amputation and limb deficiency: epidemiology and recent trends in the United States. South Med J. 2002;95(8):875–883.
- Ziegler-Graham K, MacKenzie EJ, Ephraim PL, et al. Estimating the prevalence of limb loss in the United States: 2005 to 2050. Arch Phys Med Rehabil. 2008;89(3):422–429.
- Ovadia SA, Askari M. Upper extremity amputations and prosthetics. Semin Plast Surg. 2015;29(1):55–61.
- Esquenazi A, Meier R. Rehabilitation in limb deficiency: part 4. Limb amputation. Arch Phys Med Rehabil. 1996;77(Suppl.):18.
- Cioffi WG. Upper extremity amputations. In Cioffi WG, Asenio JA, eds. Atlas of trauma: emergency surgical techniques. Philadelphia, PA: Elsevier/Saunders; 2014. 297–320.
- Cuccurullo S. Physical medicine and rehabilitation board review. New York: Demos Medical; 2004.
- Newhall K, Spangler E, Dzebisashvili N, et al. Amputation rates for patients with diabetes and peripheral arterial disease: the effects of race and region. Ann Vasc Surg. 2016;30(1):292–298.e1.
- Ephraim PL, Dillingham TR, Sector M, et al. Epidemiology of limb loss and congenital limb deficiency: a review of the literature. Arch Phys Med Rehabil. 2003;84(5):747–761.
- Esquenazi A. Amputation rehabilitation and prosthetic restoration. From surgery to community reintegration. Disabil Rehabil. 2004;26(14-15):831–836.
- Allami M, Mousavi B, Masoumi M, et al. A comprehensive musculoskeletal and peripheral nervous system assessment of war-related bilateral upper extremity amputees. Military Med Res. 2016;3(1):1–8.
- Pasquina PF, Miller M, Carvalho AJ, et al. Special considerations for multiple limb amputation. Curr Phys Med Rehabil Rep. 2014;2(4):273–289.
- Kimble SL. Acute inpatient rehabilitation interventions and outcomes for a person with quadrilateral amputation. Phys Ther. 2017;97(2):161–166.
- Davidson JH, Jones LE, Cornet J, et al. Management of the multiple limb amputee. Disabil Rehabil. 2002;24(13):688–699.
- Davidson JH, Champion S, Cousins R, et al. Rehabilitation of a quadruple amputee subsequent to electrical burns sustained whilst hang gliding. Disabil Rehabil. 2001;23(2):90–95.
- Garrison S, Merritt B. Functional outcome of quadruple amputees with end-stage renal disease. Am J Phys Med Rehabil. 1997;76(3):226–230.
- Buatois S, Miljkovic D, Manckoundia P, et al. Five times sit to stand test is a predictor of recurrent falls in healthy community-living subjects aged 65 and older. J Am Geriatr Soc. 2008;56(8):1575–1577.
- Shumway-Cook A, Brauer S, Woollacott M, et al. Predicting the probability for falls in community-dwelling older adults using the timed up & go test. Phys Ther. 2000;80(9):896–903.
- Perera S, Mody SH, Woodman RC, et al. Meaningful change and responsiveness in common physical performance measures in older adults. J Am Geriatr Soc. 2006;54(5):743–749.
- Esquenazi A, DiGiacomo R. Rehabilitation after amputation. J Am Podiatr Med Assoc. 2001;91(1):13–22.
- Hancock L, Correia S, Ahern D, et al. Cognitive predictors of skilled performance with an advanced upper limb multifunction prosthesis: a preliminary analysis. Disabil Rehabil Assist Technol. 2017;12(5):504–511.
- Lin JT, Lane JM. Falls in the elderly population. Phys Med Rehabil Clin N Am. 2005;16(1):109–128.
- Pandian G, Kowalske K. Daily functioning of patients with an amputated lower extremity. Clin Orthop Relat Res. 1999;361:91–97.
