Abstract
Purpose
While innovation is known to catalyse solutions to global sustainable development challenges, lack of engagement from stakeholders during conceptualisation and development may influence the degree of success of implementation.
Methods and materials
This paper presents a complete and novel engagement methodology, developed from value led business modelling approaches, for working with multi-sector stakeholders. The methodology can be used to determine barriers and facilitators to clinical practice innovations or translational research, within a country-specific context. The approach has then been applied in the Cambodian prosthetics and orthotics sector to provide a practice-based exemplar application of the framework.
Results
This approach seeks to ensure the suitability and sustainability of clinical practice and research programmes being implemented within a complex ecosystem. A theoretical basis, drawn from academic and business innovation sectors, has been consolidated and adapted for practical application to design, direct, and inform initiatives in low resource settings.
Conclusions
The methods presented provide a way to both develop and articulate the mission, vision, and goals of any proposed change, and to effectively communicate these with stakeholders in a way that engages the personal and professional values that exist in their ecosystem. It provides a structured process through which meaningful conversations can happen, and a basis for relationship management with key stakeholders; intrinsic to enable a sustained legacy from research and development.
Implications for Rehabilitation
The engagement from stakeholders during conceptualisation and throughout development can determine the success, or not, of any implementation and scale of innovation.
This paper presents a conceptual stakeholder-led engagement methodology, developed from value led business modelling approaches, for determining barriers and facilitators to translational global healthcare research in a country-specific context, in this case the Cambodian prosthetics and orthotics sector.
Subsequent research and development work in this area needs to carefully manage and negotiate influencing factors identified through the application of the described methodology, to ensure initiatives (whether research or wider national development work) are sustainable and successful.
Introduction
Innovation is not always good. While innovative solutions are known to catalyse solutions to global sustainable development challenges [Citation1], lack of engagement from stakeholders during conceptualisation and throughout development may influence the success of any implementation and scale of innovation, it’s relevance to a population and that the innovation is inclusive, unbiased and non-discriminatory [Citation2]. Stakeholders are defined as individuals or groups who can affect or are affected by a change, and have a reciprocal, influencing relationship with those proposing change [Citation3]. They can influence the change but can also be influenced by it.
In recent years the involvement of stakeholders in research has become more commonplace. Involving stakeholders as informed partners and advisors has been recommended to make research more meaningful and relevant [Citation4], as they help to frame research priorities, objectives and provide insights on the reality of implementing change within the health and social care sectors. There is an extremely complex interplay between health, capacity, disability and capability, and wellbeing [Citation5–7], where capacity is the ability to use and understand information to make decisions, or communicate any decisions that are made [Citation8], and capability is the ability to do something [Citation9]. Wealth is also a causal factor influencing many of the determinants of development in health system strengthening, such that disability can effect capacity and capability, which can affect health and socioeconomic status, affecting employment, cultural and economic status [Citation10]. Ubiquitous access to healthcare is defined in the United Nation’s 2030 Sustainable Development Goals [Citation7,Citation11]. Therefore, understanding perspectives across and within stakeholder groups, and importantly, where barriers and opportunities for development exist, is paramount to addressing the factors associated with inherent circularity. Specifically this wide range of factors (i.e., wealth, disability, capacity, capability, health, culture, employment, socioeconomic status etc.) can be circular and this represents a complex system. Therefore, stakeholder engagement is the best way to explore this.
Stakeholder engagement has also been linked to successful translation of research into adoption by health systems [Citation4,Citation12,Citation13], and the translation of knowledge between stakeholders within and on the periphery of any sector, which Natera, Tomassini and Vera-Cruz [Citation7], appropriately describe as non-linear and heterogeneous in nature.
Internationally, within the Assistive Technology and Medical Devices sector, technologies have been developed and launched onto the market without engagement from the clinical community, the people who use them, or the wider stakeholders who would ensure they are integrated throughout appropriate service and care models [Citation12–14]. Borsci, et al. provide evidence to show the main barriers to successful implementation into complex healthcare systems from a clinical perspective are “decision-making, impact on practice and the perceived value of the technology,” as well as a number of social, technical and organisational factors [Citation14]. Aside from being an unnecessary drain on resources (time and financial) for any profit or non-profit organisation, this expedited approach to innovation and change is short-sighted and can lead to poor sector engagement and products/services that are not fit for purpose. Within the broader context of health systems, successful change may be reliant on developed and sustained relationships with key stakeholders at every level of an organisation and the wider national level within health policy and governance [Citation15]. Not only do stakeholders often hold influence, depending on their role they may also be invested in the success or failure of any proposed change based on personal and/or professional factors [Citation4]. For any research, new product or service to be impactful and successful, these influencing landscapes should be appreciated, understood, and the stakeholders involved from the onset.
Notable advocates within the field of prosthetics and orthotics, as a sub sector of AT and medical devices, encourage qualitative methodologies to provide a much-needed individual’s voice in global health research [Citation16]. Approaches such as Patient and Public Involvement and Engagement [Citation17,Citation18], co-production [Citation19] and “experienced based design” [Citation20] take this a step further outlining the need to work in partnership with stakeholders to improve healthcare services or develop, implement and disseminate research, and offer a variety of patient centred and accessible methods, tool kits and resources. However, these approaches have tended to focus on engaging with and exploring the experiences of patients, and to a lesser extent clinicians [Citation21]. Significantly less frequent engagement with wider stakeholders, such as sector leaders, policy makers, researchers and influencing organisations, is reported in the literature [Citation2,Citation21,Citation22]. Engaging a full range of stakeholders can offer more in-depth and complete perspectives from key decision makers across the system and may require the use of different approaches. Ignoring wider groups can lead to unwarranted challenges and opposition [Citation2,Citation21,Citation22].
Within value-led businesses there are also notable examples of the use of inclusive stakeholder engagement approaches [Citation23], these include tools such as the Strategyzer® Business Model Canvas and value proposition design [Citation23]. Some also include elements beyond business considerations, such as the environmental and social impact of the innovation [Citation23,Citation24]. However, these methods do not often translate directly into the applied research context. Lessons from value led business are useful in this context because the development of value led propositions gets to the core of the problems that customers, in this case stakeholders, face. Importantly, the customer’s ideas of how to solve the problem define the process. This is where co-development and value led business intersect. The approach also allows a breakdown of all stakeholders into stakeholder segments, mimicking the customer segment analysis of value led business development [Citation25]. This enables tailoring and refinement of the package of engagement that is designed with and for individual stakeholder groups, i.e., segments.
Despite the potential of stakeholder engagement within research and innovation, it’s implementation and reporting within the current evidence base has been described as highly variable, in both quality and content [Citation4,Citation26]. This has led to calls for descriptive research on stakeholder engagement, and development of tools that can be used to support this work in the future [Citation21]. This paper therefore presents a start-to-finish engagement methodology with appropriate tools to visualise and analyse results for application within the health service design and health system strengthening domains. The engagement methodology has evolved from well-documented, established, value-led business modelling approaches [Citation25] and existing stakeholder engagement methods, and is combined here in a novel approach, adapted for use in health innovation and technology design. Where context is essential, this project emerged from a research partnership with an international non-government organisation (Exceed Worldwide)) and a desire to improve access to prosthetic service provision in Cambodia focusing on quality, sustainability, and patient experience [Citation27].
The aims of this paper are therefore addressed in two parts. Part 1 presents the engagement methodology and accompanying set of tools to guide developing, undertaking, analysing, and visualising of stakeholder engagement activities in global health innovation, for use in both research and practice. Part 2 provides an exemplar application of the methodology, highlighting stakeholder perspectives on barriers and opportunities for change in the real-world practice example of prosthetics service delivery in Cambodia. This two-part process contextualises the methodology and provides an opportunity to highlight important lessons.
Materials and methods
While qualitative research is focused and in-depth [Citation28] this paper aims to present a methodology for engagement with wider stakeholders to understand the breadth of perspectives that influence innovation and change, whether from a government or policy perspective, or from a clinical and service user perspective. This is not presented as a research methodology, but an engagement methodology. It is not intended to produce quantifiable results or qualitative themes, but to be used as a means of exploring and understanding the complex landscape in which development takes place, and to ensure that the research or practice it defines as a result is meaningful, locally owned, collaborative and fit-for-purpose. The approach proposed is an intersection between market analytics within business development [Citation25] and the Public and Patient Involvement framework [Citation29] that involves members of the public, wider stakeholders, and users of health services as partners in research, rather than just as participants.
Part 1 – Engagement methodology and definition of tools
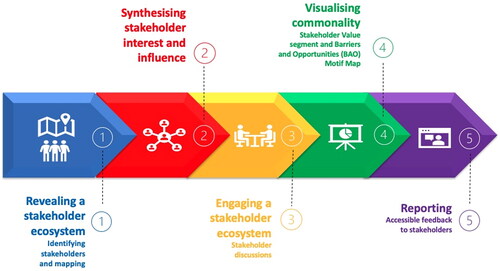
The following section outlines a proposed five-phase framework of stakeholder engagement for global health innovation contexts. The five phases are summarised in . For each phase, an associated methodology will be defined, and visualisation tools proposed.
Figure 1. Workflow for five phase framework for stakeholder engagement.
Phase 1: Revealing a stakeholder ecosystem: identifying stakeholders and mapping
Phase 1 can be initiated as early as the development of the research funding application with partner stakeholders. It relies on initial partnerships between organisations, where one or more have knowledge and wider contacts relative to the healthcare ecosystem.
Stakeholders can be identified via:
Exploring the roles of key organisations with initial partner stakeholders.
Desk research to explore macroeconomics, influencing and related organisations.
Snowballing through engagement with these different stakeholders.
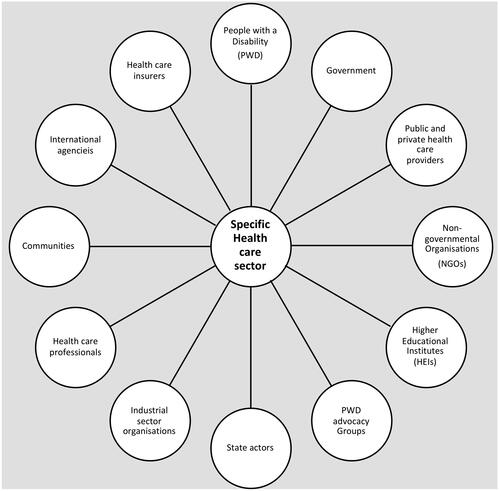
To produce an effective Stakeholder Map, stakeholder groups are defined at various interacting points within the project. For example, groups include patients or persons with disability (PWD), patient advocate groups, healthcare insurers, private hospitals, public hospitals, clinical groups, non-government organisations, government organisations or industrial sector organisations, and others depending on the context. provides a simplified illustration of a Stakeholder Map adapted from Freeman [Citation30]. Stakeholder maps can take the form of a visual map as depicted by Freeman [Citation30], or in the form of a table [Citation31].
Figure 2. Example Stakeholder Map showing a representation of stakeholders (actors) within a health sector in a Low Resource Setting. Adapted from Freeman (1984).
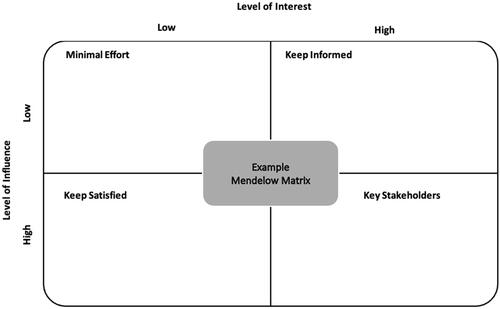
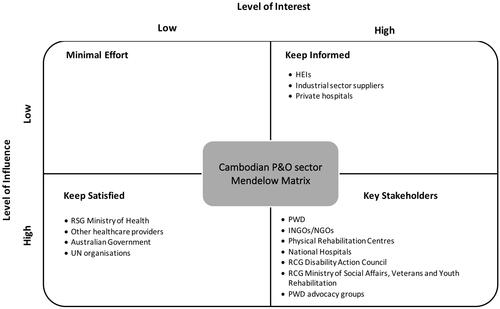
Phase 2: Synthesising Stakeholder interest and influence
Stakeholder segments, or groups of stakeholders that have similar influences, can be classified into comparator groups, for example all manufacturers, all hospitals in the private sector, all hospitals in the public sector, or all international or bilateral donors. These can then be classified using a Mendelow Matrix [Citation32] () to further analyse the level of influence a stakeholder has with reference to a project, development or service. This can be done with the initial partner stakeholders as part of a workshop, but the Matrix should be seen as a flexible creation, evolving throughout the project as more stakeholders’ views are incorporated.
Figure 3. Example Mendelow Matrix defining the quadrants for classification of stakeholders’ levels of interest and influence.
Phase 3: Engaging a Stakeholder Ecosystem: stakeholder discussions
Initial partner stakeholders can act as facilitators to introduce and coordinate discussions with other stakeholders (e.g., government officials or policy makers/influencers). Discussion guides are developed specifically for each stakeholder group. Open, non-leading questions form the basis of these discussions, where project holders are not guiding or limiting the discussion, but where the focus is based upon a particular area of common interest. These discussions require the participation of a minimum of one member of project staff and one partner stakeholder. Within the discussion, notes are taken which then form the basis of a post-discussion reflective session within the project team and initial partner stakeholders. This reflective session provides an important opportunity to verify interpretations of the discussion, allow for sociocultural context to be included and, if necessary, allow for post-translation questions within the team.
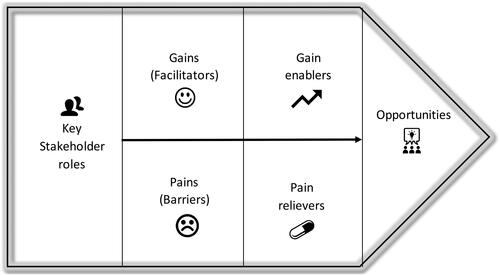
Phase 4: Visualising commonality: Stakeholder value segment and Barriers and Opportunities (BaO) Motif Map
Stakeholders are grouped based on common factors, such as type and power of influence (referencing Phase 2 above). A “motif” in this context is a recurring idea identified and consolidated for each group, and common motifs are highlighted when they emerge from more than one group. This process can be visualised using the Stakeholder Value Segment (), which was adapted from Customer Segment Analysis [Citation25] specifically for use within this engagement methodology and the global health context. This phase is iterative and can be revisited throughout the lifecycle of a project, adding a layer of legitimacy to the motif by continuous monitoring, evaluation, and adjustment with additional stakeholder discussions. One of the main advantages of this phase is allowing the stakeholder an opportunity to propose solutions, which can then be highlighted during reporting (Phase 5). This provides the opportunity for championing of any embryonic solutions by stakeholders and is a critical component of relationship building and acceptance of change. Value is thereby defined by what stakeholders perceive as important, and this method allows them to see value reflected in any future proposal for change.
Figure 4. Stakeholder Value Segment can be used to articulate the motif emerging from a group or groups of stakeholders.
Having a method of visualising stakeholder value in the topics that were discussed requires a new method of presentation: the BaO Motif Map (). The BaO Motif Map is divided into two types of influencing factors: “Barriers” and “Opportunities.” A motif is presented as a single, discrete theme where each motif depicts a barrier or opportunity identified by the stakeholder groups. Barriers are depicted on the outside and opportunities on the inside of the circle. Importantly, overlapping Barrier and Opportunity motifs (named Pivotal Motifs) highlight areas of commonality, which are important as identifiers of strategic importance in the success or failure of any proposed innovation or change. These motifs should be carefully managed as their innate complexity could influence the success or failure of any innovation.
Figure 5. The Barriers and Opportunities (BaO) Motif Map, which visualises discrete motifs, identifying them as a Barrier or Opportunity, and allows clear visualisation of Pivotal Motifs that are both a Barrier and an Opportunity.
The BaO Motif Map represents barriers and opportunities at a single point in time, and should any of these factors change, the map can rotate, expand, or contract. With this flexibility, the BaO Motif Map could also be used to track progress within a sector over time or be used to compare stakeholder views across related sectors (health and social care, for example) or countries. The outcomes elucidated from the BaO Motif Map can be included in further evidence alongside the macroeconomic environment and context analyses such as STEEPLE [Citation33] PEST[LED] [Citation34], Lewin’s Force Field Analysis [Citation35] and Porter’s Five Forces [Citation36].
Phase 5: Reporting: accessible feedback to Stakeholders
The final iteration of this partnership process is to provide a structured report back to stakeholders. This allows them to leverage the synthesised motifs to advocate for change. This is an important, and often overlooked step in establishing a reciprocal and sustained relationship with stakeholders and organisations. Depending on the stakeholder’s influence, the report can be used to inform research priorities, national policy, strategy development and social change. Importantly, by using this method, all stakeholders will be able to recognise their own influence and perspective in the report, as well as those alternative perspectives, where there might be a collective opportunity to solve or leverage change aligned with motifs. Conflicting views would be articulated in Pivotal Motifs and a more granulated overview would be presented in the structured report.
Part 2 – Exemplar application: a Stakeholder perspective to barriers and opportunities for change in Prosthetic & Orthotic(P&O) service delivery in Cambodia
The following section provides an exemplar application of the proposed engagement methodology and associated tools. This exemplar will illustrate the use of the proposed methodology and highlight lessons learnt from a real-world application.
Exemplar application background
A relationship was developed between academic partners and our initial partner stakeholder. The focus of this collaboration was to explore and understand the barriers to and opportunities for change in P&O service delivery in Cambodia from a stakeholder perspective.
Approximately 100 million people worldwide need P&O devices [Citation37]. In low-income and low- and middle-income contexts (collectively referred to here as low resource settings – LRSs), low-cost, robust prostheses and orthoses are not the main barrier to care: an estimated 80–90% do not have access to P&O services “due to a shortage of personnel, service units and health rehabilitation infrastructures” [Citation38]. However, the benefit of providing such services was recently highlighted by identifying that 86% of people who have a prosthetic device would describe themselves as being employed [Citation39]. Therefore, the wider socioeconomic and direct patient benefits cannot be underestimated, and this provides a powerful context for innovation and change alongside global equality initiatives such as the WHO Rehab2030 [Citation40] and the UN Sustainable Development Goals [Citation11] and Universal Health Coverage.
Access to P&O services is particularly poor for people in LRSs, who are typically younger and can often have higher physical working demands than those in high income countries, for whom most P&O technology has been developed and where services are often more readily accessible. The demographics of those affected also differs, with some LRSs having high levels of traumatic amputation from road and workplace accidents, conflict and landmine injuries, and humanitarian crises [Citation41]. By contrast, the primary reason for amputation in high income countries is vascular compromise associated with diabetes, although the prevalence—predicted to be 700 million people by 2045—is growing fastest in LRSs [Citation42].
Over the last 40 years, Cambodia’s healthcare service has been heavily supported by international aid donors. However more recent humanitarian crises require these donors to refocus their effort to other countries and are therefore slowly withdrawing support in Cambodia. In recent years, bilateral government aid arrangements—for example, the Department of Foreign Affairs and Trade of Australia and the Korean Overseas International Cooperation Agency—focus increasingly on disability policy development in the country. Despite such major international contributions, significant challenges still exist facing professional service delivery to people with disabilities due to financial hardships at a grass-root level [Citation43].
The aim of this practice-based exemplar application is to demonstrate the use of the presented engagement methodology and tools and contextualise them for a use case in the Cambodian P&O sector. Following the Patient and Public Involvement framework [Citation44], ethical approval was not sought for this exemplar as stakeholders are not participants in research; rather, they are future partners to ensure the sustainability of any research or innovation initiatives. Unlike qualitative research, the findings from this project are attributed to all stakeholders as a group, rather than individuals. Again, because stakeholders are future partners instead of research participants, it is not appropriate to present quotations.
Exemplar application methodology
Phase 1: Revealing a Stakeholder Ecosystem: identifying stakeholders and mapping
This project adhered to the International Society of Prosthetics & Orthotics/Exceed Research Network position paper “Ethical considerations and approaches for conducting clinical research studies related to prosthetics, orthotics and wheelchair technology in the low- and middle-income countries” [Citation45] during the wider programme of research and this associated stakeholder engagement. The project was co-developed between the University of Southampton ( UoS, research team) and an international non-government organisation (INGO) Exceed Worldwide (EW, initial partner stakeholder), collectively known as the project team. EW “supports people with disabilities living in poverty by providing free P&O services in South and Southeast Asia” and training the future P&O workforce. Through their work in the region, EW had observed the paucity of services and the depletion of the international aid model to financially support P&O services in the long term. The project team conceptualised a technology-focused research project to widen access to services, however wanted to incorporate wider stakeholder views in the proposal for change. Mapping the stakeholder ecosystem was undertaken via a series of meetings with EW staff exploring pathways of care, multidisciplinary teams, governance, supporting organisations, patient groups, health care systems, wider INGO involvement and associated professional organisations. This was supplemented with a period of desk research to widen and consolidate the team’s understanding of national and international influencing factors, such as the United Nation’s Sustainable Development Goals and the WHO Rehab2030 agenda. This was followed by further meetings with the partner stakeholder to build upon and verify the emerging ecosystem.
summarises the types of stakeholders included in the map. An extensive range of stakeholders were mapped to capture actors within the field and allow the team to build knowledge about their involvement, influence, and priorities, and understand how they interact.
Figure 6. Summary of Cambodian Prosthetics & Orthotics sector stakeholders identified as part of the stakeholder mapping (Phase 1). A complete version can be found in the supplementary materials online.

Phase 2: Synthesising Stakeholder interest and influence
In collaboration with EW, stakeholders were identified who had the most interest and influence, and whose views and insights would be most valuable to understand how the sector would respond to change ().
Figure 7. Cambodian prosthetics & orthotics sector Mendelow matrix of influence vs. interest.
Phase 3: Engaging a Stakeholder Ecosystem: stakeholder discussions
EW were crucial to engaging with the key stakeholders identified in phase 2. They sourced well-placed stakeholders within each group and acted as advocates to introduce the project team, explain the project and co-ordinate a schedule of meetings. Discussion guides were developed for each group and based on initial partner stakeholder feedback and desk research.
Meetings often took different formats depending on who the stakeholders were, varying from discussions with prosthetic users in their homes to formal meetings with members of the Royal Cambodian Government (RCG). This also led to variation in translation practices, which reflected the needs of the stakeholder at the time. For example, two translators worked formally during government meetings, some meetings employed a single translator and others were undertaken in English. Notes were taken throughout the meetings by two members of the project team.
An important reflection during the application to Cambodia was the crucial interfacing role the initial partner stakeholder played, which appeared key to the success of this phase. The best outcomes were achieved when partner stakeholders were able to approach key stakeholders at all levels. They were pivotal to the success of the meeting arrangements. In this situation, it was also important that the initial partner stakeholder was fully engaged in the development of the overarching project, as well as the previous phases described above, so that they were able to stakeholders with context the wider project agenda.
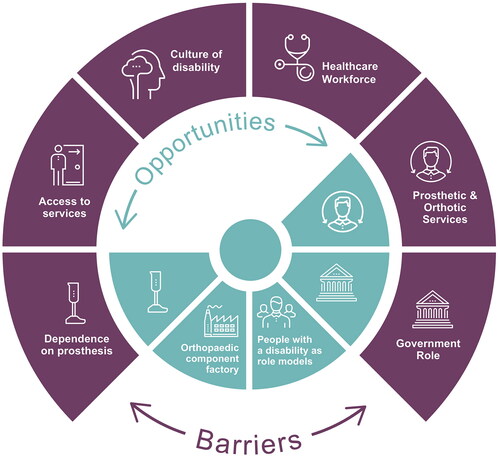
Phase 4: Visualising commonality – Barriers and Opportunities (BaO) Motif Map
Themes were developed iteratively from amalgamated field notes. On completion of the Value Stakeholder Segment, BaO Motif Map was produced (), which describes the P&O sector at a single point in time (October 2019) and visualises the themes from the P&O stakeholder engagement in Cambodia.
Figure 8. Barriers and Opportunities Motif Map for the P&O sector in Cambodia, as of October 2019.
Phase 5: Reporting: accessible feedback to stakeholders
The findings, including the BaO Motif Map, were summarised in a variety of formats for stakeholders. A communication plan was created to understand the key messages from the findings and their value to the different stakeholders. Appropriate and accessible methods of communication were discussed with the initial partner stakeholder EW to ensure that feedback took the right format for each stakeholder group to maximise dissemination. For example, a written report was provided to Higher Education Institutions and departments of the RCG, whereas animated videos and Facebook posts were created for clinicians and PWDs, with links available to more detailed summaries. Online seminars and symposia at an international congress were held for NGOs, service funders and academic researcher stakeholders.
Exemplar application findings
The findings of the exemplar application are presented below. The discrete themes, or motifs in the BAO motif map (), are categorised as either barriers to change, opportunities to support development and capacity building, or those themes which overlap, as both barriers and opportunities (Pivotal Motifs).
Barriers to change
Healthcare workforce
Concerns were raised by several stakeholders about the availability of qualified and experienced healthcare professionals to deliver post-amputation prosthetic rehabilitation services in Cambodia. Although degree-level courses in both Physiotherapy and Prosthetics and Orthotics are available in the country, these roles are not well understood or respected by the wider public, thus impacting national workforce recruitment opportunities. Despite support in recent years from INGOs offering bursaries, uptake of training places remains poor. As well as limited numbers of new graduates, there are only small numbers of Physiotherapists and Prosthetists currently practicing. Stakeholders felt that poor awareness of the role by the public and key referrers, such as Doctors and Surgeons, can lead to underutilisation of services and patients getting lost along the post-amputation rehabilitation pathway. There is an intrinsic link to health system strengthening and integrated services with this theme.
Low wages of P&O and Physiotherapy staff was identified as a key driver affecting the uptake of training places and the retention of qualified staff. For Physiotherapists, this can result in a pull to the more lucrative private sector, leaving notable skill gaps within public services. Private roles are also used to supplement low wages within the public sector, but these opportunities are currently not available for clinical Prosthetists/Orthotists or Prosthetic and Orthotic Technicians. Their wages and conditions of employment are often disadvantageous as they are not awarded civil servant status. Stakeholders involved in service delivery were concerned that this gap in the current prosthetic rehabilitation workforce makes service delivery challenging both now, and in the future, and will have a notable impact on the availability, effectiveness, and quality of prosthetic care [Citation43]. It is important to note that at the time the study was conducted key roles in the prosthetic multidisciplinary team (MDT), such as Occupational Therapists and Doctors of Rehabilitation Medicine were absent from prosthetic services and higher educational training in Cambodia.
Access to services
Access to health care services is a known problem throughout LRSs [Citation41], and Cambodian P&O services are no exception with stakeholders highlighting that access is challenging for people with both new and established amputations. Following a new amputation, many people face lengthy delays before they are fitted with a prosthesis due to an absence of widespread referral systems post-surgery and continuity of care between health and physical rehabilitation services. Stakeholders identified factors that contribute to delays in accessing services, notably the lack of awareness from potential medical referrers, and concerns over costs in a health care system with high out-of-pocket expenses. These delays may have a significant impact on the individual’s physical, psychological, and socioeconomic stability and recovery.
The cost of attending a P&O service was also thought to be prohibitive for many patients, especially those from more rural areas. The monetary impact of travelling to the centre, accommodation costs whilst limbs are manufactured and time away from family and earning an income can lead to a significant financial burden for the patient or result in non-attendance. INGOs often have financial support available for transport, meals and accommodation expenses in the form of reimbursement, however many stakeholders felt this did not resolve these issues, as money still had to be found upfront for costs such as travel to the clinic. The lifelong requirement for prosthetic repair, renewal and replacement following an amputation, raised concerns amongst stakeholders that the monetary impact of accessing P&O services over time can lead to a spiral of poverty and disability [Citation46,Citation47] as costs accumulate.
Culture of disability
Stakeholders described a culture of disability in Cambodia associated with stigmatization and made comments to the perception of previous “bad karma” and punishment. Stakeholders described situations where individuals were socially excluded, unable to gain employment and struggled to access education following amputation. People with an amputation were often described as the poorest people in their communities and these aspects of socioeconomic status, and perhaps social stigma, were viewed as linked to poor health and poor health seeking behaviours, respectively. This is well known as the Disability Poverty Nexus or Spiral [Citation48]. First line health care was frequently described as being sought from local (often unqualified) pharmacists rather than public health centres. Stakeholders felt that this perception of people with a disability as struggling for acceptance in society led to them becoming very dependent on any support available. This in turn was described as negatively affecting their independence and autonomy, which may impact their ability to raise their voice and defend their newly established rights within the eyes of the government.
Pivotal motifs – both barriers and opportunities
Prosthetic and Orthotic services
Cambodia today has a country-wide network of Physical Rehabilitation Centres, delivered by or with support from INGOs, to provide P&O services to people following amputation. As Cambodia has strived to move away from reliance on aid toward a more sustainable, publicly provided service, the Persons with Disabilities Foundation (PWDF) was established within the Ministry of Social Affairs, Veterans and Youth Rehabilitation (MoSVY) to realise this ambition.
Stakeholders identified this existing network and infrastructure, with its well-established government and INGO partnerships, as an excellent platform for development. However significant variation was highlighted in service provision across the country, especially in newly transitioned public services where several stakeholders, including representatives from government, identified that public services lack the budget and knowledge to provide the required standard of care compared to INGOs [Citation43].
Stakeholders highlighted that variation across services is compounded by a lack of focus within the sector on quality-of-service provision, efficiency, and outcome. Stakeholders reported that due to the above-described workforce issues, MDT working is a challenge for most centres and many focus on the provision of prosthetic devices rather than providing rehabilitation. Stakeholders felt that improved leadership and co-ordination and transparency across the sector would promote greater partnership working at a national health systems level and more equitable service provision.
Government role
The World Health Organisation Rehab2030 strategy [Citation40] highlights the need for rehabilitation services to be aligned with wider health care systems and be governed by a country’s Ministry of Health to ensure rehabilitation is included in efforts towards universal health coverage. Cambodian P&O services sit within the remit of the Ministry of Social Affairs, Veterans and Youth Rehabilitation (MoSVY) rather than the Ministry of Health, and although cross ministry working is apparent, P&O services were described by stakeholders as being viewed as a social intervention. Stakeholders in this project felt that the MoSVY struggled with a restricted budget when compared to the Ministry of Health, which resulted in low wages, lack of civil servant status for employees and self-acknowledged challenges contributing to, and ensuring, equitable access to welfare initiatives. However, despite these challenges there appeared to be a drive for collaboration from all government stakeholders involved, and the development of a new national centre is intended to bring together health and rehabilitation services, assistive technology, and manufacturing with the aim of highlighting this level of service provision both nationally and internationally.
Dependence on prostheses
Many of the stakeholder meetings were with users of prosthetic devices. They reported that their prosthesis allows them the chance to make a significant recovery, by re-establishing employment opportunities, the ability to travel, acceptance and engagement within their community. They described being very dependent on their prosthetic devices, demonstrating a significant need for service provision within the country. However, this dependency was felt to have mixed consequences, with any threat to limb wearing, such as prosthesis damage, being described as having a major impact on choices affecting their participation and way of life, for example engaging in family and community activities or maintaining employment.
Opportunities to support development and capacity building
People with a disability as role models
Stakeholders described how people with disabilities in Cambodia face challenges associated with social stigma every day, but many can find meaningful employment, participate in education, and fulfil roles within their communities. Stakeholders in this project, especially prosthesis users felt PWD need to become role models for independence and empowerment. They highlighted important opportunities to actively break the stigma of disability, provide peer support for others with a disability and advocate for people in need. Although this group is unlikely to represent the views of disabled people throughout and beyond Cambodia, it is important to recognise the need for PWD to have their voices heard and the opportunity to embody the changes they wish to see in their society. As a group they are important stakeholders to involve as they are both highly interested and influential amongst their peers and are increasingly involved at a government policy level.
Orthopaedic component factory
The handover of technical, financial and managerial responsibility of the Cambodian Orthopaedic Component Factory to the MoSVY from the International Committee of the Red Cross was completed in 2018. This established, and regionally connected organisation, facilitates opportunities for income generation for the MoSVY. The P&O devices they produce are an appropriate technology, beyond simply matching rural Cambodian users’ requirements of durability and low initial cost. They are also commercially and environmentally sustainable, with on-site polypropylene recovery and recycling from manufacturing waste and returned P&O devices reducing dependence on importing material. Development of new prosthetic products and manufacturing techniques, as well as the production of wider assistive technology to meet the social and cultural needs of Cambodian people, was viewed as presenting significant opportunities for development within the country and international export throughout the region.
Discussion
This paper provides a collective understanding and language to facilitate productive and impactful research through the definition and application of an engagement methodology and can be used to understand the contexts in which development happens. Specifically, stakeholders are involved in “prioritising research” and “commenting on the feasibility of the research design” in the phase prior to participant research being undertaken [Citation29]. This stakeholder-led methodology determines the value of any perspectives on proposed change resulting from research and therefore makes positive steps to ensure subsequent research is appropriate, meaningful, and has the best chance of use translation through clinical and service adoption.
The proposed engagement methodology may be used to realise the reported limitations in the context of translational research, where science, technology and innovation arising from academic research is translated linearly into healthcare to improve service quality or delivery [Citation7]. This methodology was designed to dovetail with user-led or design thinking principles of health technology development, in this case through data systems to support access to P&O services [Citation27] to ensure that technologies are useable (using the former user-centric design methods) through to ensuring that knowledge in transferred non-linearly throughout the research process, ensuring that the health system and its stakeholders value the proposed change and have influenced their part in it. It can also serve to complement existing conceptual frameworks, such as the 4Fs: Function, Form, Field and Flows [Citation6] and the 5S-5M-5C [Citation49], and toward articulating and realising innovation systems thinking.
The application of the engagement methodology to a Cambodian P&O sector exemplar highlighted areas of influence and the potential barriers and opportunities from different stakeholder perspectives, which helped to broaden our understanding of the current issues they face. The considerable impact that prosthetic provision has on the lives of people following limb loss is evident. These findings contribute to the growing case for ongoing funding and provision of services in Cambodia to both rehabilitate people with a prosthetic limb and to ensure their continued independence through effective and timely maintenance services.
As in many LRSs, providing and sustaining a skilled workforce to deliver health care services is a major challenge. The International Society for Prosthetics and Orthotics suggest that the number of P&O professionals, as well as technicians, does not meet this recommended provision in high income countries, and in Southeast Asia the available workforce may be as low as one tenth of the number required [Citation50]. The WHO estimate there are less than 10 skilled rehabilitation professionals per 1 million population in many LMICs [Citation40]. With an estimated 0.5% of the global population in need of a prosthetic device—equivalent to 35–40 million people [Citation51]—and the increasing global prevalence of non-communicable diseases, road traffic accidents and work-based accidents, this requirement is only going to increase.
In Cambodia training and providing a sustainable multidisciplinary workforce to deliver P&O services is difficult. Both P&O and Physiotherapy training programmes struggle to fill their places, and programmes for other prosthetic multidisciplinary team roles do not yet exist within the country. Khan et al. [Citation52] suggested that specialised multidisciplinary teams, such as those seen within prosthetic rehabilitation may not be feasible in less-resourced settings, and alternative approaches should be considered such as task shifting, supporting community-based programmes and the use of telerehabilitation. However, such innovations should be undertaken in a systematic way to ensure quality and safety, and not be adopted at the expense of investment in training [Citation53]. Who the tasks are shifted to, particularly in rehabilitation settings, should also be carefully considered as previous studies within stroke rehabilitation in LRSs have found shifting to family members is not effective [Citation54,Citation55].
Access appears to be an important barrier to prosthetic use and services must strive for greater accessibility, particularly focusing on how best to support patients getting to services that are available [Citation27]. New models of care should be considered that are not based on historical High Income Country ways of working but develop out of, and in response to, the needs of local contexts, such as decentralised systems with mobile teams and transportable manufacturing solutions [Citation39].
Service should go beyond just the provision of assistive technology, and crucially quality should also not be overlooked in the struggle to improve access [Citation56]. Variation in prosthetic providers in Cambodia inevitably leads to variation in service provision. A nationwide service specification or minimum package of activities is necessary and should strive for a user-centred rehabilitation approach [Citation40]. The future inclusion of quality indicators, agreed in partnership with current stakeholders and service providers, alongside an understanding of what outcomes are important to capture in Cambodia [Citation27], could assist in equitably raising the quality of prosthetic rehabilitation and assist in the evaluation of services to improve efficiency, quality, and user experience.
This study has also highlighted opportunities for engaging further with key stakeholders in the development of future projects to address the findings presented here. Important stakeholders in this sector are the users of prosthetic services. People with disabilities in Cambodia face significant stigma and social exclusion [Citation27,Citation57]. P&O health care providers have a unique opportunity to challenge this by engaging patients, who may be lifelong users of their services, and working together in partnership. Translating this co-production approach, more commonly used in HICs and in technology development, into LRSs could give PWD the opportunity to act as role models, improve empowerment and work together with health care providers to shape services that meet their needs and improve their outcomes [Citation58]. As well as service users, opportunities also exist, and are welcomed, for engagement with government. Key assets and ongoing development projects, alongside skills gaps identified by the stakeholders themselves, present unique opportunities to leverage and build on existing assets to maximise impact.
Conclusion
This paper presents a stakeholder-led engagement methodology for determining barriers and facilitators to translational global healthcare research in a country-specific context and demonstrated its application on an exemplar situation of Cambodian prosthetics service delivery. Subsequent research and development work in this area needs to carefully manage and negotiate influencing factors to ensure initiatives (whether research or wider national development work) are sustainable and successful. The reports which result from this approach can be used to ensure that interpretations of stakeholder perspectives are valid and allow stakeholders to leverage consolidated sector-wide intelligence to their advantage, mobilising local, regional, and national drivers and influencers to change. In many respects, these reports can harness the values of these respective groups and encourage championing of initiatives that are recognised as locally owned by stakeholders and reflecting their perspectives. Cambodia, with its long, complex historical context and rich, increasingly diverse P&O services, could be used as a regional demonstration case, and it may be feasible that this country could pioneer innovative approaches for working systems for this LRS and capacity building. This level of engagement would not be possible without a value-embedded approach.
Understanding the value perceived by various stakeholders is at the heart of this engagement methodology. It is important to acknowledge that while this is not a research methodology, it provides important insights into the appropriate contexts from which meaningful qualitative and quantitative research can take place.
The methods presented provide a way to articulate the mission, vision, and goals of any proposed change and to effectively communicate these with stakeholders in a way that engages the personal and professional values that exist in their ecosystem. It provides a structured process through which meaningful conversations can happen, and a basis for relationship management with key stakeholders, enabling a sustained legacy of research and development. Importantly, it provides a start-to-finish methodology to ensure the sustainability of research outcomes that should be the driving motivation for research in engaging multisector stakeholders to identify priorities for global health innovation, change and research.
Supplemental Material
Download PDF (41.1 KB)Acknowledgements
Removed for anonymity.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Silva AL. Innovation in development cooperation: emerging trajectories and implications for inclusive sustainable development in the 21st century. Innov Dev. 2021;11(1):151–171.
- Petkovic J, Riddle A, Akl EA, et al. Protocol for the development of guidance for stakeholder engagement in health and healthcare guideline development and implementation. Syst Rev. 2020;9(1):1–11.
- Freeman RE, Harrison JS, Zyglidopoulos S. Stakeholder Theory. Cambridge: Cambridge University Press; 2018.
- Esmail L, Moore E, Rein A. Evaluating patient and stakeholder engagement in research: moving from theory to practice. J Comp Eff Res. 2015;4(2):133–145.
- Husain MJ. Contribution of health to economic development: a survey and overview. Economics. 2010;4(1):14.
- Hanlin R, Andersen MH. Putting knowledge flows front and Centre in health systems strengthening. Innov Dev. 2019;9(2):169–186.
- Natera JM, Tomassini C, Vera-Cruz AO. Policy analysis and knowledge application for building a healthy health innovation system in developing countries. Innov Dev. 2019;9(2):159–168.
- NHS England. Assessing capacity. www.nhs.co.uk. 2022.
- Anon. Cambridge Dictionary. www.dictionary.cambridge.org. 2022.
- Banks LM, Kuper H, Polack S. Poverty and disability in low-And middleincome countries: a systematic review. PLoS One. 2017;12(12):1–19.
- United Nations. Transforming our world: the 2030 agenda for sustainable development. New York (NY): United Nations; 2015.
- Peters DH, Bhuiya A, Ghaffar A. Engaging stakeholders in implementation research: lessons from the future health systems research programme experience. Heal Res Policy Syst. 2017;15:4–6.
- Kok MO, Gyapong JO, Wolffers I, et al. Which health research gets used and why? An empirical analysis of 30 cases. Heal Res Policy Syst. 2016;14:36.
- Borsci S, Uchegbu I, Buckle P, et al. Designing medical technology for resilience: integrating health economics and human factors approaches. Expert Rev Med Devices. 2018;15(1):15–26.
- Holcomb J, Ferguson GM, Sun J, et al. Stakeholder engagement in adoption, implementation, and sustainment of an Evidence-Based intervention to increase mammography adherence among Low-Income women. J Cancer Educ. 2022;37(5):1486–1495.
- Dillon MP, Fatone S, Ramstrand N, et al. Prosthetics and orthotics international welcomes qualitative research submissions. Prosthet Orthot Int. 2019;43(4):366–368.
- INVOLVE. Briefing notes for researchers: involving the public in NHS, public health and social care research. Eastleigh: INVOLVE; 2012.
- Partnership UPISD. UK standards for public involvement. NIHR. 2019.
- Realpe A, Wallace LM. What is co-production. London: The Health Foundation; 2010:1–1.
- Foundation T point of care. Experience based design toolkit. www.pointofcarefoundation.org.uk/resource/experience-based-co-design-ebcd-toolkit. 2022.
- Concannon TW, Fuster M, Saunders T, et al. A systematic review of stakeholder engagement in comparative effectiveness and patient-centered outcomes research. J Gen Intern Med. 2014;29(12):1692–1701.
- Shrestha A, Tamrakar D, Shrestha B, et al. Stakeholder engagement in a hypertension and diabetes prevention research program: description and lessons learned. PLoS One. 2022;17(10):e0276478–13.
- Joyce A, Paquin RL. The triple layered business model canvas: a tool to design more sustainable business models. J Clean Prod. 2016;135:1474–1486.
- Carayannis EG, Barth TD, Campbell DF. The Quintuple helix innovation model: global warming as a challenge and driver for innovation. J Innov Entrep. 2012;1(1):2.
- Osterwalder A, Pigneur Y, Bernarda G, et al. Value proposition design: how to create products and services customers want. Hoboken, NJ: John Wiley & Sons, Inc.; 2014.
- Lane J. Aligning policy and practice in science, technology and innovation to deliver the intended socio-economic results: the case of assistive technology. Int J Transitions Innov Syst. 2015;4(3/4):221–248.
- Dickinson A, Donovan-Hall M, Kheng S, et al. Technologies to enhance quality and access to prosthetics and orthotics: the importance of a multidisciplinary, user-centred approach. WHO Global Report on Assistive Technology (GReAT) consultation. Geneva, Switzerland; 2019.
- Braun V, Clarke V. Successful qualitative research: a practical guide for beginners. Los Angeles, USA: SAGE Publications Ltd; 2013.
- INVOLVE. Public involvement in research and research ethics committee review. Eastleigh: INVOLVE; 2016.
- Freeman RE. Stakeholder management: framework and philosophy. In Strategic management: a Stakeholder approach. Cambridge: Cambridge University Press; 1984. pp 52–82.
- Mtika W, Wilcox H, Feune De Colombi N. Stakeholder engagement for applying Research to Policy and Practice for Health (ARCH); 2021.
- Johnson G, Scholes K, Whittington R. Stakeholder mapping: the power/interest matrix. In Exploring corporate strategy. 8th ed. Essex, England: Pearson Education Limited; 2008. P. 156.
- More E, Probert D, Phaal R. Improving long-term strategic planning: an analysis of STEEPLE factors identified in environmental scanning brainstorms In 2015 Portland International Conference on Management of Engineering and Technology (PICMET); 2015. pp. 381–394.
- Whittington R, Regnér P, Angwin D, et al. Macro-environment analysis. In Exploring strategy. 12th ed. Harlow, England: Pearson Education Limited; 2020. Pp. 34–58.
- Lewin K. Field theory of social science: selected theoretical papers. New York: Harper & Brothers; 1951.
- Porter M. How competitive forces shape strategy. Harv Bus Rev. 1979;57:137–145.
- WHO. World report in disability. Geneva, Switzerland: WHO; 2013.
- Sexton S. Rehabilitation of people with physical disabilities in developing countries. Denmark: Køge; 2015.
- CHAI/ATScale. Product narrative: prostheses. London, UK: CHAI/ATScale; 2020.
- WHO. Rehabilitation in health systems: guide for action. Geneva: WHO; 2019.
- Marino M, Pattni S, Greenberg M, et al. Access to prosthetic devices in developing countries: pathways and challenges. In: 2015 IEEE Global Humanitarian Technology Conference (GHTC); 2015. pp. 45–51.
- Saeedi P, Petersohn I, Salpea P, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the international diabetes federation diabetes Atlas, 9(th) edition. Diabetes Res Clin Pract. 2019;157:107843. November;157:
- Bailey S, Nguon SK. Situation analysis for disability-inclusive governance and community development in Cambodia; 2014.
- NIHR. Briefing notes for researchers: public involvement in NHS, public health and social care research. INVOLVE [Internet]. 2012; [cited 2020 July 8]. Available from: https://www.invo.org.uk/wp-content/uploads/2014/11/9938_INVOLVE_Briefing_Notes_WEB.pdf.
- Andrysek J, Berthaume M, Boone D, et al. Ethical considerations and approaches for conducting clinical research studies related to prosthetics, orthotics and wheelchair technology in the low- and middle-income countries. Brussels, Belgium: International Society of Prosthetics and Orthotics; 2021.
- Cobley D. Disability and international development. London, UK: Routeledge; 2018.
- Ramani SV. On consortium driven sanitation interventions to end open defecation: insights from an Indian village study. Innov Dev. 2020;10(2):245–261.
- Dalal AK. Disability–poverty nexus: psycho-social impediments to participatory development. Psychol Dev Soc J. 2010;22:409–437.
- Bitton A, Veillard JH, Basu L, et al. The 5S-5M-5C schematic: transforming primary care inputs to outcomes in low-income and Middle-income countries. BMJ Glob Health. 2018;3(Suppl 3):e001020.
- Bailey S. Ensuring sustainability of physical rehabilitation services in cambodia: analysis of transition process; 2015.
- WHO. WHO Standards for Prosthetics and Orthotics. 2017.
- Khan F, Amatya B, de Groote W, et al. Capacity-building in clinical skills of rehabilitation workforce in low- and Middle-income countries. J Rehabil Med. 2018;50(5):472–479.
- WHO. Task shifting: rational redistribution of tasks among health workforce teams: global recommendations and guidelines. Geneva: WHO; 2008.
- Lindley RI, Anderson CS, Billot L, et al. Family-led rehabilitation after stroke in India (ATTEND): a randomised controlled trial. Lancet. 2017;390(10094):588–599.
- Zhou B, Zhang J, Zhao Y, et al. Caregiver-delivered stroke rehabilitation in Rural China. Stroke. 2019;50(7):1825–1830.
- Matter R, Harniss M, Oderud T, et al. Assistive technology in resource-limited environments: a scoping review. Disabil Rehabil Assist Technol. 2017;12(2):105–114.
- Thomas P. Poverty reduction and development in Cambodia: enabling disabled people to play a role; 2005.
- Ellen ME, Shach R, Kok MC, et al. There is much to learn when you listen: exploring citizen engagement in high- and Low-Income countries. World Health Popul. 2017;17(3):31–42.
