Abstract
Purpose
Although a well-established aspect of healthcare practice, the impact of facemasks on verbal communication is surprisingly ambiguous.
Materials and Methods
A systematic search was conducted in APA PSYCHinfo, CINAHL, NHS Knowledge Network, Medline and SPORTDiscus databases from inception to November 2022 according to the PRISMA guidelines. Studies reporting an objective measure of speech understanding in adults, where information was transmitted or received whilst wearing a facemask were included. Risk of bias of included studies was assessed with the Newcastle-Ottawa score.
Results
Four hundred and thirty-three studies were identified, of which fifteen were suitable for inclusion, incorporating 350 participants with a median age of 49 (range 19 to 74) years. Wide heterogeneity of test parameters and outcome measurement prohibited pooling of data. 93% (14 of 15) studies reported a deleterious effect of facemasks on speech understanding, and 100% (5 of 5) of the included studies reported attenuation of sound with facemask usage. Background noise added further deleterious effects on speech understanding which was particularly problematic within hearing-impaired populations. Risk of bias in included studies varied but overall was modest.
Conclusions
Despite considerable complexity and heterogeneity in outcome measure, 93% (14 of 15) articles suggest respiratory protective equipment negatively affects speech understanding in normal hearing and hearing-impaired adults.
Implications for Rehabilitation
As a result of the covid-19 pandemic, facemask use is now commonplace across all healthcare and rehabilitation settings and has material implications for interpersonal communication.
This systematic review of human communicative studies highlights that the use of facemasks does indeed inhibit communication through effects on speech intelligibility and through sound attenuation.
These effects are evident in both normal hearing and hearing-impaired adults due to the visual cues required with lipreading and facial expressions during communication.
The presence of background noise also produces deleterious effects on speech understanding and is more problematic for hearing-impaired populations.
Simple recommendations to reduce background noise (where possible), to step closer (where social-distancing rules permit), to speak louder or to use speech to text applications (if practical) could all mitigate these communicative barriers. Further an awareness of persons with hearing impairments, the function (or otherwise) of hearing aids in those patients that require these, and an ability to use transparent facemasks can be specifically helpful.
Introduction
The use of facemasks in healthcare settings was substantially expanded in response to the severe acute respiratory syndrome coronavirus 2, generally referred to as COVID-19. Throughout the pandemic, non-pharmaceutical interventions were the predominant method adopted by governments in attempts to mitigate the spread and morbidity of the virus [Citation1,Citation2] whilst an effective vaccination campaign was developed[Citation3]. Non-pharmaceutical interventions are essentially behavioural adaptations including, local lockdowns, travel bans, social distancing and the wearing of personal protective equipment (PPE)[Citation4]. In the UK, the wearing of a face covering was built into legislation in 2020[Citation5] and remains a requirement in healthcare settings. Various designs of face coverings with differing material properties were employed to cover the mask and nose, from medical grade equipment to designer fashion, and from fully concealing face coverings to transparent materials. Patients and the public often wore a 2-layer cloth mask as recommended by the UK Government (2021), to overcome the initial global shortage of medical-grade surgical masks[Citation6], whilst healthcare professionals commonly wore a loose-fitting fluid-resistant surgical mask (FRSM) or a close-fitting disposable filtering facepiece (N95)[Citation7]. The surgical masks remain commonplace in healthcare settings.
Communication is a central tenet of delivering healthcare[Citation8]. Miscommunications can result in compromised patient care, misdiagnoses and medication errors, resulting in decreased patient outcomes and unnecessary legal charges[Citation9,Citation10]. In contrast, increased communication between healthcare professionals and patients develops trust, leading to improved patient outcomes, understanding and adherence to interventions[Citation11,Citation12]. Interpersonal communication describes the interaction between individuals through oral or physical interactions (including gestures). Protective masks covering the mouth and the nose can muffle sound, making it more challenging to understand speech, and obscure facial expressions in the mouth and cheeks. Facemasks can challenge communication, especially for deaf or hearing-impaired individuals as non-verbal communication such as facial expressions can be misinterpreted and the critical skill of lip-reading inhibited[Citation13–15]. The effect of respiratory protective equipment (RPE) and facemasks on communication is not a new topic and has been highlighted in relation to previous disease outbreaks [Citation16]. There is a general acceptance that facemasks ‘must’ inhibit communication but surprising ambiguity as to the actual effects of this in the healthcare setting.
RPE may impact speech understanding through a physical sound attenuation effect and additionally by influencing speech intelligibility and interpretation. Sound attenuation describes the loss of intensity and perceptibility by a listener, and this may be more profound when using RPE [Citation17]. Speech intelligibility describes how clearly a person speaks so that what they are saying is comprehensible to the listener. When speech intelligibility is reduced, the listener may become frustrated and/or lose interest, which may have a negative impact on interactions with healthcare practitioners [Citation18]. Speech perception is a multilevel procedure through which biomechanical, neural, computational, and cognitive processes use auditory signals to give meaning and understanding to a person’s speech [Citation19]. Hearing impaired service users have particular challenges compared to non-hearing-impaired individuals when RPE is used. The World Health Organisation estimate that, worldwide, 466 million people live with disabling hearing loss and that this number is likely to rise with an aging global population [Citation20]. In the UK, the prevalence of profound hearing loss has been estimated at 6.7% in those accessing healthcare compared to a background prevalence of <1% in the general population [Citation21]. As such, the purpose of this project was to review the literature as to the effects of respiratory protective equipment on speech understanding in healthcare settings.
Methods
A systematic literature review was undertaken in accordance with the Cochrane guidance [Citation22] and the search protocol reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines [Citation23].
Information sources and search strategy
We applied the PEO criteria to inform our search strategy, which aimed to find articles that evaluated an outcome of speech understanding in direct person-person communication with the use of facemasks. Five databases; APA PSYCHinfo, CINAHL, NHS Knowledge Network, Medline and SPORTDiscus were searched from inception to 15 November 2022. The search terms included “face mask OR surgical mask OR mask” AND “communication barrier OR communicat*” AND “hearing.” MESH terms and Boolean operators were employed in each search. We applied an English language restriction but no other filters to the search. The electronic database search was supplemented by searching Google Scholar and screening the references of included publications.
Study selection and eligibility criteria
Due to the breadth and somewhat exploratory nature of the research question, all study types were considered for inclusion provided they were published as peer-reviewed primary research articles and contained relevant data. We sought quantitative outcome-based studies to determine the effect of a mask on communication. Studies were included if they reported a measure of speech understanding as a primary outcome variable in an in-person communication setting where information was transmitted or received whilst wearing a facemask. Any cohort of adults (over the age of 18 years) was eligible, including groups with hearing impairments, participating within a healthcare or simulated healthcare setting. Exclusion criteria comprised study reports that were not peer-reviewed, conference abstracts and editorial or commentary articles. Experimental investigations without human participation were excluded. Qualitative information as to speech interpretation was not considered for this review.
The searches and initial screening by title were performed by one investigator (RF). Abstracts were reviewed independently by two investigators (RF and DFH). In cases of doubt, articles were included for full-text review. The same two investigators independently assessed the appropriateness of the selected full-text articles against the selection criteria and consensus was reached for inclusion with additional review by a third individual (CM) where required.
Data extraction and synthesis
The following characteristics of each study were extracted to a bespoke Excel database: author, year of publication, geographical location of study, type of study, study population and setting, numbers of participants, participant demographics, outcome measures, and study results. Data extraction forms were created and 2 researchers (RF and DFH) independently extracted the data from included articles. The 2 researchers cross-checked each-other extracted data to ensure consistency. There was no dispute in the extracted parameters and a consensus was reached.
As there was substantial heterogeneity in the parameters related to speech understanding that were assessed across the included studies and the specific data collected by the individual researchers varied substantially, pooling of outcome data across the included studies was not feasible. Results are therefore presented descriptively.
Methodological quality Assessment
The methodological quality of included studies was assessed using the modified Newcastle-Ottawa scale (NOS) [Citation24], risk of bias assessment tool appraising studies based on dimensions of selection, comparability and outcome. Eight items may be awarded a maximum of one star for selection and outcome and two for comparability. As has been proposed [Citation25], we accepted a total score of >7 stars to reflect high-quality studies with a low risk of bias, 4–6 stars as moderate quality studies and <4 stars to be low-quality with an increased risk of bias. Two researchers (RF and DFH) independently evaluated the included papers against these criteria and a third researcher (CM) resolved controversial assessments by independently looking at the included study.
Results
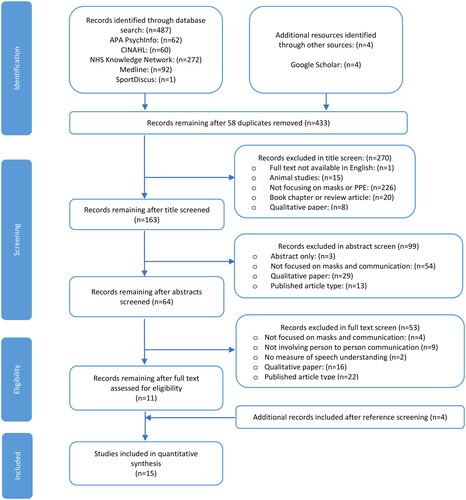
The literature search generated 487 potential articles with four additional studies found via the Google Scholar search engine. After the removal of duplicates, 433 papers were evaluated against the eligibility criteria. After screening, 64 articles were available for full-text review, of which fifteen met the inclusion criteria. Full details are displayed in the PRISMA flowchart ().
Figure 1. PRISMA flow diagram of study selection process.
Study characteristics
The included studies constituted eight cross-sectional and seven quasi-experimental designs, the data and characteristics of which are summarised in . A combined total of 350 participants were included with individual study sample sizes ranging from n = 5 to n = 42. The median age of participants was 49 (range 19 to 74) years. The participants' sex was reported within 73% (11/15) of the studies; in these studies, there were 150 female participants (65%) and 83 male participants (35%). Six studies were conducted in the USA, two in the UK, and in India, and one in each of Germany, Holland, China, Korea and Australia.
Table 1. Included study, demographics and outcomes.
Speech understanding outcomes
Three broad categories of sound attenuation, speech intelligibility and speech perception were examined across the fifteen studies with a variety of outcome measures employed to quantify these ().
Sound attenuation
100% of studies (5 of 5) reported reduced sound attenuation with facemask use, however, variation was evident with different types of face covering. Llamas et al.[Citation26] report almost no differences in sound attenuation between control conditions and the fabric niqab, balaclava, handkerchief, scarf, fleece and nylon cover, however, a significant difference was found for the surgical facemask. The regions in which marked decreases in the acoustic signal were seen are between 2.5 kHz and 12.5 kHz and a high-frequency cut-off 24 kHz. Bottalico et al. [Citation27] following a similar methodology reported attenuation in all masks with the fabric mask being the most attenuating (4.2 dB) compared with N95 and FRSM: 2.9 dB and 2.3 dB respectively. The threshold of perceptibility of difference in sound detectable by the human ear is 2db [Citation28] thus this mask difference may not be observable. Kumar et al. [Citation29] however reported that speech recognition thresholds increased by 1.8 dB, 4.4 dB, and 5.05 dB, when wearing surgical, cloth, and N95 masks respectively, which may be detectable differences. Zhou et al. [Citation30], reported more stark differences with RPE use at high frequencies. Surgical masks attenuated high frequencies by about 4 dB, transparent masks blocked about 8 dB and N95 masks with face shields caused the most-severe attenuation of around 10 dB. Significantly increased sound attenuation was also noted by Moon et al. [Citation31] comparing no mask and a surgical mask (p < 0.001) and no mask and an N95 mask (p< .001). When the speakers were wearing the surgical and N95 mask, sound pressure levels were significantly reduced.
Measured speech intelligibility
83% of studies (5 of 6) suggested reduced speech intelligibility with facemask use. Bandaru et al. [Citation32] reported a significant difference in speech reception threshold and speech discrimination score whilst wearing RPE. However, Magee et al. [Citation33] describe no significant difference in intelligibility using the Assessment of Intelligibility of Dysarthric Speech (ASSIDS) tool for single words or sentences when wearing a facemask. The identification accuracy of single words and sentences showed variance between phrase types and mask conditions but not to a significant level. Similarly, the type of facemask (cloth, surgical and N95) introduced variation and generally reduced accuracy, but not to a significant level. Radonovich et al.[Citation34] presented data that was measured within a simulated, and actual, intensive care unit (ICU). They reported an overall significant difference between intelligibility applying various facemask conditions at a distance of 7 ft compared with 3 ft (p < 0.0001). Word accuracy identification reduced between 1–17% across facemask designs compared to control conditions however, statistical differences in speech intelligibility score were seen only in full respirator masks. Bottalico et al. [Citation27] report reduced speech intelligibility of 12%, 13% and 16% when wearing the surgical, N95 and fabric facemasks respectively, in comparison to an unmasked control. A further comparison between the mask types demonstrated statistically significant differences in speech intelligibility between the fabric and FRSM (p < 0.001). This study also examined listening effort and found there was a greater difference when wearing a fabric, N95 or FRSM (p < 0.001) compared to the control. Ritter et al.[Citation35] demonstrated a significant decrease in the word recognition score when using an N95 mask compared to no mask. Thirty-six words were selected from a standardized audiological list (Central Institute for the Deaf Auditory List W-1) to determine the speech recognition score, which was calculated by determining the percentage of correctly repeated words. Words were presented to participants in a closed clinical room at a distance of 6 feet at a normal speech intensity level to replicate the classic healthcare outpatient situation. Participants with self-reported hearing loss performed worse across all mask conditions compared to participants with normal hearing. Gutz et al. [Citation36], suggested that speakers adapt their articulatory patterns when wearing a mask. These adaptations appear to overcome losses in both intensity and intelligibility caused by the mask. Increased intelligibility in Speech Intelligibility Test scores was observed when the speaker was instructed to speak loudly (p = 0.01), with non-significant differences apparent when instructed to speak clearly (p = 0.07) or slowly (p = 0.24).
Speech perception
100% (9 of 9) studies suggested a reduction in speech perception with facemask use, though again there was large heterogeneity in setting and assessment measures. Atcherson et al. [Citation37] and Mendel et al. [Citation10] report significant differences in the spectral analyses of recorded speech stimuli with and without a facemask; p < 0.0001 and p = 0.038 respectively. Mendel et al. [Citation10] reported no significant differences when conditions or different facemasks were compared, however Atcherson et al. [Citation37] found that when unmasked, auditory conditions scored significantly higher (p < 0.05) than when using surgical facemasks, or transparent facemasks, or transparent facemasks with additional audio-visual cues. Moon et al. [Citation31] asked participants to complete a listen-and-repeat task while watching video recordings. The availability of visual cues was beneficial for speech understanding, with significant improvements in speech perception seen when listeners were able to see the speaker without the mask. However, when the speakers were wearing a mask, no differences were observed between no visual cues and visual cues conditions. Similarly, Zhou et al. [Citation30] recruited young ward nurses and had them listen to the simulated speech (attenuated by several types of PPE) and simultaneously watch the speaker’s videos with or without visual cues. They reported that wearing either a surgical mask or an N95 mask with a face shield decreased the performance of speech perception relative to wearing no mask. Notably, speech perception with the transparent mask was comparable to the unmasked condition. Kumar et al. [Citation29] reported that word recognition scores decreased by 32% without a mask, 43.7% in a surgical mask, 46.3% in a cloth mask, and 46.7% in N95 mask conditions, comparing high to low levels of signal-to-noise ratios (background noise). Surgical masks did not affect the word recognition scores at lower background noise levels, however, as the signal-to-noise ratio decreased, the surgical, cloth, and N95 masks significantly impacted the word recognition score. Hampton et al. [Citation38] considered the effects of RPE on speech perception within different noise level simulated environments using the Bamford-Kowal-Bench sentence test. The wearing of RPE significantly affected speech perception within the hospital ICU (p = 0.02) and operating theatre (p = 0.001) but not within the office or emergency department settings; p = 0.26 and p = 0.58 respectively. A masked condition significantly altered sentence test results (p = 0.001) over an unmasked condition overall and was particularly problematic within an operating theatre (p = 0.04). During this experiment, participants were also asked to raise their voices when wearing a facemask and this exhibited a significant effect (p = 0.04). In an un-masked condition, raising voice volume had no significant effects (p = 0.50). Llamas et al. [Citation26] reported a 2% decrease in speech perception overall for all three face coverings: balaclava, niqab and FRSM. No statistical analysis or p-value was reported, however, the FRSM was ranked as ‘easiest to understand’. This study also reports a higher number of misperceptions under audio-only communication conditions in comparison with audio-visual communication conditions, suggesting an effect of visual cues in speech perception. Weiss et al. [Citation39] looked at the most extreme PPE situation evaluating speech perception when wearing a powered air-purifying respirator (PAPR), the type of equipment used by surgeons in high-risk aerosol producing procedures. A small cohort of naïve (but trained) equipment users reported average number recognition score and an average monosyllabic word recognition score significantly decreased with the PAPR (p < 0.001). Correspondingly mean speech recognition thresholds significantly increased (deteriorated) when using the PAPR system (p < 0.001).
Mendel et al. [Citation10] additionally identified differences in speech perception between normal-hearing and hearing-impaired groups (p < 0.007), with background noise (p = 0.004) and whilst wearing a facemask (p= <0.000). Surprisingly, and presenting data to odds with wider literature, for normal-hearing persons, wearing a facemask caused a significant increase in speech perception scores (p < 0.007), however, the environmental noise produced a significantly decreased effect (p < 0.05). These authors reported similarly surprising data for hearing-impaired persons who also showed a significant increase in speech perception scores when the speaker wore a facemask (p < 0.007) but a greater significant decrease in speech perception scores in the noisy environment (p < 0.01). Atcherson et al. [Citation37] found similar results in terms of overall significant deleterious effects for impaired hearing status (p < 0.001), type of mask used (p < 0.001) and when combining hearing level and mask type (p < 0.001). Those individuals with severe-profound hearing loss performed significantly worse than those with normal hearing or moderate hearing loss (p < 0.001). No differences were identified between participants with normal hearing and with moderate hearing loss within unmasked audio transmission conditions, unmasked audio-visual transmission and transparent mask audio-visual transmission conditions. Those with moderate hearing loss did however show a significant increase in speech perception scores under unmasked audio-visual communications conditions when compared to surgical and transparent facemask audio-only conditions (p < 0.001). In a study of people with moderate to severe hearing impairments, Homans and Vroegop [Citation40] report significant reductions in Speech Tracking Test (STT) wearing a surgical facemask (p < 0.001). The test was conducted at a 1.5 m distance simulating typical covid-19 distancing conditions. In those with the worst hearing impairment a face shield also caused significantly reduced STT scores compared to no mask conditions (p = 0.03).
Risk of bias assessment of included studies
The methodological quality of the included studies was mixed, though generally reasonable, with 27% (4/15) of studies scoring >7 stars (high quality), 53% (8/15) of studies scoring five or six stars (moderate quality) and only 20% (3/12) studies <4 stars (poor quality) (). 100% (15/15) of studies met the criteria for outcome assessment and 93% (14/15) included appropriate statistical analysis. Some 80% (12/15) of studies met the criteria for sample representation. Only 13% (2/15) of the studies however considered appropriate test sample sizes, this being the most poorly reported measure. 100% of the studies recorded zero dropouts and all participant results were included.
Table 2. Methodological quality of included studies (Newcastle-Ottawa Scale).
Discussion
During the COVID-19 pandemic, the use of facemasks in healthcare settings has become widespread and routine across all settings beyond the controlled environments in which mask usage would have previously been expected. As such, the influence of mask use on interpersonal communication is important to consider. This systematic review of human studies found clear overall results in reduced levels of speech understanding through increased sound attenuation by the mask and also via reduced speech intelligibility and perception, of the speaker and listener respectively, with facemask usage.
The diverse clinical/environmental settings, study designs and outcome assessments of the papers included in our review inhibited formal pooling of the findings. Notably, the outcome measures used by the included studies to assess aspects of speech interpretation varied substantially. The modified rhyme test (MRT) and speech recognition threshold (SRT) based tests are widely used to provide a measure of speech intelligibility through single-word identification. However, single-word testing shows limited reliability and lacks validity in real-world situations with continuous speech [Citation38]. As such, Nilsson et al. [Citation41] suggest sentence SRTs may offer higher statistical reliability. The Assessment of Intelligibility of Dysarthric Speech (ASSIDS), Consonant-Nucleus-Consonant (CNC), Connected Speech Test (CST) and Bamford-Kowal-Bench Speech-in-Noise (BKB-SIN) test used within Magee et al. [Citation33], Bottalico et al. [Citation27], Mendel et al. [Citation10], and Hampton et al. [Citation38] respectively, provide a measure of both single words alongside sentences and may therefore offer more robust results. The British Standards Institution [Citation42] advise that context provision can increase success by as much as 30%. As such, the selected word banks of individual tests could affect results if these are not in context with the environment studied. Interestingly, Radonovich et al. [Citation34] suggest if medical terminology were used within the clinical setting in their study a different speech intelligibility result may have been returned.
Bandaru et al. [Citation32], Magee et al. [Citation33] and Mendel et al. [Citation10] all conducted studies within a ‘gold standard’ sterilised audiometry setting with background noise controlled. While undoubtably useful in determining experimental accuracy, the utility of this controlled setting as a surrogate for the clinical environment is debatable and must be interpreted accordingly. Mendel et al. [Citation10] actually reported the listening conditions “too good,” and a ceiling effect was seen in Bottalico et al. [Citation27] which could affect the reliability of the produced results. To combat this, Atcherson et al. [Citation37] and Mendel et al. [Citation10] applied a conversion of data to rationalised arcsine units to stabilise the variance encountered. Nonetheless, this may present an underestimation of significance between the unmasked and masked conditions and potentially a type 2 error. Perhaps the most ‘clinically’ useful data comes from the directly applied designs[Citation34,Citation35,Citation40] where communication was directly assessed in healthcare environments using covid-19 distancing measures. Here, clear blockages to communication were evident with mask use.
While all facemasks inhibited communication to some degree, variation in performance was reported by type. Fabric facemasks produced the highest negative effects on speech intelligibility, while surgical and N95 masks comparatively offered less of a barrier to communication. Confusingly Mendel et al. [Citation10] reported the use of facemasks to increase speech perception scores. It is unclear why this paper differs in its findings to the wider literature but this may be related to the specific methodology employed in which a trained, clearly articulate, professional radio broadcaster was utilised to record speech stimuli. This paper scored lowest in quality assessment and bias may then confound the reports results.
Unsurprisingly, communication in people with hearing loss is more affected by mask-wearing than in those with normal hearing. Transparent face masks were introduced as part of the covid-19 safety measures to support communication between those who have hearing difficulties or are deaf, patients/service users with cognitive problems such as dementia, and those with learning disabilities [Citation43]. Generally, these include a transparent area, which allows the wearer’s mouth and areas of the face to be visible to others, as required for lip reading or other facial visibility requirements. These transparent masks (with a transparent mouth covering within a standard facemask) are importantly different to face shields, which are separate articles, typically worn over facemasks as an extra layer of splatter protection. Atcherson et al.[Citation37] and Homans et al. [Citation40] found the transparent facemask and face shield responsible for the greatest sound attenuation. While transparent masks do attenuate (restrict) sound transmission more than opaque masks (due to the materials used in construction) people with hearing loss do seem to benefit from their use, due to these allowing for visual facial ques and lipreading, which corresponds with data from experimental data from loudspeaker experimentation [Citation13]. An unforeseen drawback of the transparent facemask or face shield though is that it can reflect glare into the eyes of the listener, therefore reducing visual cues and lipreading ability; a very real situation occurring within the clinical practice that can be a specific issue for hearing impaired individuals. Overall, the data suggests facemasks significantly affect speech understanding and more so within the presence of background noise and for those in hearing-impaired populations. Individuals with severe-profound hearing-impairment without electronic aids but lipread are affected less by background noise, however, this cohort is increasingly affected by the RPE presence.
Several suggestions have been offered to explain the variation in results obtained including the ‘Lombard effect’ where people with a facemask speak louder to overcome the physical/perceived communication barrier or an ‘occlusion’ effect where positive feedback of the spoken sound is increased due to the facemask. Increasing voice volume is a simple and effective method of volume compensation when the mouth is obstructed [Citation44] and Hampton et al. [Citation38] report a significant effect on speech understanding when raising speech volume whilst wearing RPE. Atcherson et al. [Citation37] identified that for normal hearing participants in quiet environments, facial expressions and lipreading did not affect the results significantly but increased the confidence with which participants answered. However, for those with severe-profound hearing impairment, the results significantly increased when visual cues were allowed. This may be an example of the “McGurk” effect where audio-visual cues are relied upon in speech perception [Citation45]. Where these cues are removed, such as when wearing RPE, speech understanding can be impaired. High sound attenuation was seen with the transparent facemask, therefore, reducing the audio cues, but arguably increasing the visual cues available to the listener. Whether these visual cues are needed or not may depend on the hearing-impairment level of the listener. Chládková et al. [Citation46] demonstrated that adults with normal hearing adapt their speech perception by reducing reliance on visual cues, this was not an immediate effect and reduced over a 4-week period. As RPE may continue to be worn in clinical settings for some time it may be helpful to consider what type of covering is most appropriate in the context of interpersonal communication as opposed to droplet spread. Specific consideration should be given to hearing-impaired individuals and whether they may benefit from visual cues, in which case transparent face coverings would be beneficial, or audio cues, where FRSM performs highest for speech intelligibility and understanding. The benefits of different masks may be different for individuals and providing an element of choice in design may be useful. General advice to mitigate the barriers posed by the protective facemask in clinical settings are to, where possible, reduce the level of background noise, speak loudly and clearly, and to use gestures. This may pose something of a challenge in clinical environments where confidentiality is important. Writing down information may then be the most practical measure to augment a consultation that is challenged by masks. Further awareness of persons with hearing impairments, the function (or otherwise) of hearing aids in patients that require these, and an ability to use transparent materials where appropriate may help facilitate masked communication in healthcare settings.
Strengths and limitations
Strengths of this work include the extensive search undertaken of five databases plus Google Scholar that present a cohesive summary of the effects of facemasks on speech understanding in adult human populations. Limitations include the comparatively modest number of studies that could be evaluated, the variation of clinical settings and outcome measures used along with the inherent small sample sizes which may limit generalisability.
Conclusions
This systematic review highlights complexity and heterogeneity in outcome assessment measures of communication with facemask usage, but, broadly, RPE negatively affects speech understanding. This is evident in both normal hearing and particularly challenging in hearing-impaired adults due to the visual cues required with lipreading and facial expressions during communication. The presence of background noise also produces deleterious effects on speech understanding more so within hearing-impaired populations. Simple recommendations to step closer (where social-distancing rules permit), to speak louder or to use speech-to-text applications (if practical) could all mitigate the barrier RPE poses.
Acknowledgements
There was no specific funding for this work.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Garcia LP. Use of facemasks to limit COVID-19 transmission. Epidemiol Serv Saude. 2020;29(2):e2020023.
- Liu Y, Morgenstern C, Kelly J, et al. The impact of non-pharmaceutical interventions on SARS-CoV-2 transmission across 130 countries and territories. BMC Med. 2021;19(1):40.
- Regmi K, Lwin C. Impact of non-pharmaceutical interventions for reducing transmission of COVID-19: a systematic review and meta-analysis protocol. BMJ Open. 2020;10(10):e041383.
- Perra N. Non-pharmaceutical interventions during the COVID-19 pandemic: a review. Phys Rep. 2021;913:1–52.
- The Health Protection. Coronavirus, Wearing of Face-Coverings in a Relevant Place (England) Regulations 2020. UK Statutory Instruments 2020 No 791. UK Government; 2020.
- Mahase E. Covid-19: are cloth masks still effective? And other questions answered. BMJ. 2021;372:n432–n432.
- Round M, Isherwood P. Speech intelligibility in respiratory protective equipment – Implications for verbal communication in critical care. Trends Anaesth Critl Care. 2021;36:23–29.
- Judd M. Broken communication in nursing can kill: teaching communication is vital. Creat Nurs. 2013;19(2):101–104.
- Trotter AR, Matt SB, Wojnar D. Communication strategies and accommodations utilized by health care providers with hearing loss: a pilot study. Am J Audiol. 2014;23(1):7–19.
- Mendel L, Gardino J, Atcherson S. Speech understanding using surgical masks: a problem in health care? Am J Audiol. 2008;19:686–695.
- Kratzke I, Rosenbaum M, Cox C, et al. Effect of clear vs standard covered masks on communication with patients during surgical clinic encounters: a randomized clinical trial. JAMA Surg. 2021;156(4):372–378.
- Meyer EC, Sellers DE, Browning DM, et al. Difficult conversations: improving communication skills and relational abilities in health care. Pediatr Crit Care Med. 2009;10(3):352–359.
- Corey R, Jones U, Singer A. Acoustic effects of medical, cloth, and transparent face masks on speech signals. J. Acoust. Soc. Am. 2020;148(4):2371–2375.
- Hüfner K, Hofer A, Sperner-Unterweger B. On the difficulties of building therapeutic relationships when wearing face masks. J Psychosom Res. 2020;138:110226.
- Palmiero A, Symons D, Morgan IJ, et al. Facemasks and air-purifying respirators. J Occup Environ Hyg. 2016;13(12):960–968.
- Nelson H. USA: objections to protective respirators. Lancet. 1992;340(8827):1088.
- Atcherson S, McDowell B, Howard M. Acoustic effects of non-transparent and transparent face coverings. J Acoust Soc Am. 2021;149(4):2249–2254.
- Coppens-Hofman M, Terband H, Snik A, et al. Speech characteristics and intelligibility in adults with mild and moderate intellectual disabilities. Folia Phoniatr Logop. 2016;68(4):175–182.
- Poeppel D. Speech perception. In Social cognitive neuroscience, cognitive neuroscience, clinical brain mapping. Vol 3. Elsevier Inc. 2015. p.429–434.
- World Health Organization. Addressing the rising prevalence of hearing loss. ISBN 978-92-4-155026-0 © 2018.
- Turton L, Smith P. Prevalence & characteristics of severe and profound hearing loss in adults in a UK national health service clinic. Int J Audiol. 2013;52(2):92–97.
- Lasserson TJ, Thomas J, Higgins JPT. Chapter 1: starting a review. In: higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane handbook for systematic reviews of interventions version 6.2 (updated february 2021). Cochrane, 2021. Available from www.training.cochrane.org/handbook.
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339(jul21 1):e78–336–b2535.
- Moskalewicz A, Oremus M. No clear choice between Newcastle–Ottawa scale and appraisal tool for cross-sectional studies to assess methodological quality in cross-sectional studies of health-related quality of life and breast cancer. J Clin Epidemiol. 2020;120:94–103.
- Wells GA, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality if nonrandomized studies in meta-analyses, 2012. Available from: http://wwwohrica/programs/clinical_epidemiology/oxfordasp.
- Llamas C, Harrison P, Donnelly D, et al. Effects of different types of face coverings on speech acoustics and intelligibility. York Papers in Linguistics Series 2. 2008;9:80–104. http://www.york.ac.uk/language/ypl/ypl2issue9/YPL9_04_Llamas.pdf
- Bottalico P, Murgia S, Puglisi G, et al. Effect of masks on speech intelligibility in auralized classrooms. J Acoust Soc Am. 2020;148(5):2878–2884.
- Singh S, Mohanty AR. HVAC noise control using natural materials to improve vehicle interior sound quality. Appl Acoust. 2018;140:100–109.
- Kumar R, Munjal SK, Sharma A, et al. Effect of face masks on speech understanding: a clinical perspective during speech audiometry. J Otol. 2022;17(3):140–145.
- Zhou P, Zong S, Xi X, et al. Effect of wearing personal protective equipment on acoustic characteristics and speech perception during COVID-19. Appl Acoust. 2022;197:108940.
- Moon IJ, Jo M, Kim GY, et al. How does a face mask impact speech perception? Healthcare. 2022;10(9):1709.
- Bandaru S, Augustine A, Lepcha A, et al. The effects of N95 mask and face shield on speech perception among healthcare workers in the coronavirus disease 2019 pandemic scenario. J Laryngol Otol. 2020;134(10):895–898.
- Magee M, Lewis C, Noffs G, et al. Effects of face masks on acoustic analysis and speech perception: implications for peri-pandemic protocols. J Acoust Soc Am. 2020;148(6):3562–3568.
- Radonovich L, Yanke R, Cheng J, et al. Diminished speech intelligibility associated with certain types of respirators worn by healthcare workers. J Occup Environ Hyg. 2010;7(1):63–70.
- Ritter E, Miller C, Morse J, et al. Impact of masks on speech recognition in adult patients with and without hearing loss. ORL J Otorhinolaryngol Relat Spec. 2022;84(4):302–308.
- Gutz SE, Rowe HP, Tilton-Bolowsky VE, et al. Speaking with a KN95 face mask: a within-subjects study on speaker adaptation and strategies to improve intelligibility. Cogn Res Princ Implic. 2022;7(1):73.
- Atcherson S, Mendel L, Baltimore W, et al. The effect of conventional and transparent surgical masks on speech understanding in individuals with and without hearing loss. Am J Audiol. 2017;28:58–67.
- Hampton T, Crunkhorn R, Lowe N, et al. Speech discrimination challenges of healthcare professionals whilst wearing personal protective equipment (PPE) during the coronavirus disease 2019 (COVID-19) pandemic. Authorea. 2020; http://www.york.ac.uk/language/ypl/ypl2issue9/YPL9_04_Llamas.pdf
- Weiss R, Guchlerner L, Weissgerber T, et al. Powered air-purifying respirators used during the SARS-CoV-2 pandemic significantly reduce speech perception. J Occup Med Toxicol. 2021;16(1):43.
- Homans NC, Vroegop JL. The impact of face masks on the communication of adults with hearing loss during COVID-19 in a clinical setting. Int J Audiol. 2022; 61(5):365–370. Epub 2021 Jul 28. PMID: 34319825
- Nilsson M, Soli SD, Sullivan JA. Development of the hearing in noise test for the measurement of speech reception thresholds in quiet and in noise. J Acoust Soc Am. 1994;95(2):1085–1099.
- British Standards Institution (BSI). 2011. EN 60268-16:2011: sound system equipment. Objective rating of speech intelligibility by speech transmission index. British Standards Institute: London. https://bsol-bsigroup-com.ezproxy.napier.ac.uk/Bibliographic/BibliographicInfoData/000000000030249993
- Department of Health and Social Care 2022. Guidance document: transparent face mask technical specification. Cabinet Office, London. https://www.gov.uk/government/publications/technical-specifications-for-personal-protective-equipment-ppe/transparent-face-mask-technical-specification#:∼:text=A%20transparent%20face%20mask%20can,and%20those%20with%20learning%20disabilities
- Pörschmann C, Lübeck T, Arend J. Impact of face masks on voice radiation. J Acoust Soc Am. 2020;148(6):3663–3670.
- McGurk H, MacDonald J. Hearing lips and seeing voices. Nature. 1976;264(5588):746–748.
- Chládková K, Podlipský V, Nudga N, et al. The McGurk effect in the time of pandemic: age-dependent adaptation to an environmental loss of visual speech cues. Psychon Bull Rev. 2021;28(3):992–1002.
