Abstract
Purpose
Life balance is a new and important concept in occupational therapy. New measurements are needed to assess and evaluate life balance and interventions aimed to achieve this concept. This article describes the test-retest reliability of three life balance measures: the Activity Calculator (AC), Activity Card Sort (ACS-NL(18-64)) and Occupational Balance Questionnaire (OBQ11-NL).
Method
Data collection took place among 50 participants with neuromuscular diseases: facioscapulohumeral dystrophy (FSHD, n = 25) or mitochondrial myopathy (MM, n = 25). The AC, the ACS-NL(18–64) and the OBQ11-NL were assessed twice with an interval of one week. Intraclass correlation coefficients (ICC-agreement) were applied to examine test-retest reliability.
Results
The ICC of the AC-average total day score was .95 (95% CI .91-.97), whereas the ICC of the weights allocated to each activity was 0.80 (95% CI .77–0.82). The ICC of the ACS-NL(18–64) percentage retained activities was 0.92 (95% CI 0.86 − 0.96) and the ICC of the importance score per activity was- .76 (95% CI . 0.68–0.89). The ICC of the OBQ11-NL total score was .76 (95% CI 0.62–0.86).
Conclusion
All three tools showed good to excellent test-retest reliability in a sample of patients with FSHD or MM, which is promising for its use in clinical practice and research.
IMPLICATIONS FOR REHABILITATION
The AC, ACS-NL(18–64) and the OBQ11-NL are promising, reliable measures of life balance in patients with neuromuscular diseases.
The development of three new instruments for life balance enlarges the possibility for health professionals to measure life balance in clinical practice and research.
Introduction
Neuromuscular diseases (NMD), such as facioscapulohumeral dystrophy (FSHD) and mitochondrial myopathy (MM), are slowly progressive neurological disorders. Persons with NMD experience personal challenges integrating the consequences of the disease diagnosis and disease symptoms, coping with heredity, adjusting to decreasing functional independence, and coping with the impact on social participation such as maintaining relationships. They also have to adjust to the progressive reliance on assistive devices, giving up activities such as (paid) work, and to dismissive responses from the social environment.
Chronic fatigue is present in at least 60% of the patients with NMD and can be their most prominent and disabling symptom [Citation1,Citation2], In combination with motor impairments, fear of falling, and possible cardiorespiratory involvement, this often results in low levels of physical activity and decreased social participation [Citation3,Citation4]. These health and social problems making it difficult to balance available energy against the energy needed to perform everyday activities [Citation1]. Too many or too strenuous activities lead to overload and exhaustion, whereas a lack of meaningful activities is associated with decreased quality of life and limited well-being [Citation5]. Occupational therapy supports people with NMD experiencing chronic fatigue to obtain balance in available energy and activity demands, often referred to as occupational balance or life balance, which are often used interchangeably. In this article, we will use the term life balance.
Life balance is a complex construct that includes balancing both the physical and psychological energy demands of activities and embedding them in the demands of social roles (e.g., being a worker, parent, or volunteer), while also preserving and creating meaning in life. Backman et al. (2004) argued that its foundation rests on how people choose to allocate and spend time in valued, obligatory, and discretionary activities [Citation6]. She distinguishes four different dimensions of life balance: 1) length, referring to the time allocated to activities or life roles; 2) width, referring to the number of activities and social roles engaged in; 3) depth, referring to the meaning of activities and social roles; and 4) weight, referring to the experienced physical or mental energy burden of activities. Life balance is influenced by culture, values, and environmental expectations (Backman, 2004). Based on content analysis of existing literature, Eklund, Orban [Citation7] proposed three indicators of occupational balance 1): the mix of activities (harmony and variation) 2), the ability and resources to manage the amount of occupations engaged in, and 3) the values and personal meaning of occupations.
Clinical practice and good client care require the ability to measure the different dimensions of life balance accurately and reliably and to detect change over time. To this end, we selected and further developed three potential measures of life balance: the Activity Calculator (AC), the Activity Card Sort (ACS-NL(18–64)), and the Occupational Balance Questionnaire (OBQ11-NL). These three measurements address different dimensions of life balance: the AC measures length and weight, the ACS-NL(18–64) measures both width and depth, and the OBQ11-NL measures the right mix in life balance. These measurements also reflect the indicators of occupational balance as described by Eklund, Orban [Citation7]: mix of occupations, congruence with values, and personal meaning.
The Activity Calculator (AC) is widely used by occupational therapists in the Netherlands for patients with chronic fatigue or chronic pain and is recommended as an intervention in several evidence-based occupational therapy guidelines for people with chronic conditions and chronic fatigue [Citation8–10]. The AC emerged from occupational therapy practice as part of an intervention protocol to coach individual patients to balance their activity levels. Internationally, similar intervention protocols have been developed, such as the Pacing Points Program by Parkwood Institute [Citation11]. The AC records daily activities and their duration. Clients assign a weight to the perceived energy demand of half an hour of activity. It is administered via an interview, supported by a structured record form [Citation12]. The current study is the first to explore the potential of the AC as an outcome measure. Psychometric properties have not yet been studied.
The original version of the Activity Card Sort (ACS) was developed in the United States of America [Citation13] to measure the level of engagement in current and previous activities of older adults (>60 years of age). The ACS uses Q-sort methodology with photo cards of people engaged in common, everyday activities. The ACS has been translated and culturally adapted in various countries [Citation14–19]. In 2013 the Dutch ACS-NL, consisting of 79 photo cards with activities, was introduced for older adults (>64 years of age) in the Netherlands [Citation20,Citation21]. The Dutch ACS-NL has shown good to excellent intra- and interrater reliability [Citation21]. To be able to assess an adult population younger than 65 years of age, a new version of the ACS-NL was developed for this study. The ACS-NL(18-64) consists of 84 photo cards reflecting the most common activities of adults younger than age 65 [Citation22]. Psychometric properties of the Dutch ACS-NL(18-64) have not yet been examined.
The Occupational Balance Questionnaire (OBQ) measures the overall perception of life balance in a harmonic mix of occupations [Citation23,Citation24]. The original Swedish version consists of 13 items and has shown good internal consistency, no floor or ceiling effects, and all items have proven to be stable with sufficient test-retest reliability [Citation23,Citation24]. After internal consistency analyses, the OBQ was reduced to 11 items: the OBQ11 [Citation25]. The OBQ11 has been translated into Spanish [Citation26] and Norwegian [Citation27] and for this study into Dutch. The OBQ11-NL is an authorized and validated test based on forward and backward translation carried out in collaboration with the original authors. The psychometric properties of the translated version have not been studied.
The selected measures of life balance hold promise as potential outcome measures. In preparation for planned effectiveness studies, research into the psychometric properties of the life balance outcome measures is needed. Therefore, the aim of this study was to assess the test-retest reliability of the AC, the ACS-NL(18–64), and the OBQ11-NL in a sample of patients with NMD in the Netherlands. More specifically, we included patients with facioscapulohumeral dystrophy (FSHD) and mitochondrial myopathy (MM); two different, slowly progressive, inherited disorders both with a high prevalence of chronic fatigue.
Methods
Participants
Participants were recruited with the assistance of the Dutch patient organization for neuromuscular diseases, Spierziekten Nederland [Citation28]. This organization mailed study information to members diagnosed with FSHD or MM, and published information on their website and in newsletters. Interested participants contacted the primary researcher (JL) by email. In response, they received a flyer with a study summary and a request for permission to contact them by telephone. After oral confirmation of willingness to participate and an explanation of the inclusion and exclusion criteria, eligible participants received the patient information letter and the informed consent form by post. After returning the signed informed consent by post, baseline assessments were administered.
Participants were included if they: 1) were diagnosed with FSHD or MM (oral confirmation by the participant), 2) were at least 18 years of age, 3) had self-reported chronic fatigue that impacted their activity and social participation, and 4) had the ability to read and comprehend self-reported outcome measures in Dutch. Potential participants were excluded if they had co-morbidity known to have a high prevalence of (chronic) fatigue (e.g., cancer, recent surgery, stroke). Recruitment continued until fifty participants had been enrolled, 25 participants in each diagnostic group.
The Medical Ethical Committee (METC) of the region Arnhem-Nijmegen provided an exemption from formal ethical approval (NL2018-4513).
Procedure
After obtaining signed, informed consent, each participant completed a questionnaire by email including demographic (age, relationship status, educational level) and clinical (diagnosis, years since diagnosis, co-morbidities) questions. To be able to characterize fatigue severity, the fatigue subscale of the Checklist Individual Strength (CIS-Fatigue) was also sent, completed, and returned by email. The CIS-Fatigue measures experienced fatigue and consists of 8 statements, each rated on a 7-point response scale. A summed score of ≥ 35 indicates severe fatigue. The CIS-Fatigue has been well validated in various patient groups [Citation29].
The AC and ACS-NL(18-64) were each administered by the same research assistant twice, via interview, with a test-retest interval of 1-2 weeks. This interval was believed to be short enough to prevent changes in health or personal conditions, but long enough to prevent recall given the length and complexity of the tools [Citation30].
All testing took place within 3 weeks of consent. Research assistants were occupational therapists, trained to administer both the AC and the ACS-NL(18–64). To administer the AC, participants received activity diaries one week before the interview with instructions to record their activities every half hour for three consecutive days. The interview administration of the AC and ACS-NL(18–64) took place at participants” home or a location chosen by the participant. As the interviews for both the ACS-NL(18–64) and the AC took place in one session, they could be strenuous for people with NMD and fatigue. Therefore, extra time and pauses were planned. Data collection at both times (T1 = test; T2 = retest) took place under similar conditions (method of administering, same rater, appointments on a similar day and time of day). Participants also completed the OBQ11-NL twice using a digital survey, with a planned interval of 1 week.
Measurements
The Activity Calculator (AC)
As described above, participants completed an activity diary for three days prior to the first interview (T1), entering descriptions of their activities for every half hour. During the interview, participants were asked to allocate a “weight score” (relaxing = −1, light =1, medium =2 and strenuous = 3), representing the energy cost of performing each activity recorded on the activity diary. We instructed the participants to apply the following basic rules: 1) assign weight scores regardless of the energy level before starting the activity or the time of the day; and 2) allocate weights based on an activity duration of half an hour. Research using cognitive interviewing showed that participants had difficulty applying these basic rules [Citation31]. Therefore, we added instruction cards with descriptions for the weight scores.
For each day a “total day score” was calculated by summing the weight scores of all activities recorded in a single day. An “average day score” was calculated by adding up the three-day scores and dividing by three. Initially, the “total day scores” were calculated manually by the research assistants. These calculations were checked in a random sample of ten participants. Because of miscalculations on a regular basis, we implemented an excel sheet to calculate the “total day scores” and the “average day score” for the whole sample of 50 participants, both at T1 and T2.
At the second interview (T2) participants were not asked to complete a new activity diary. Instead, they were asked to reassign a weight score to each of the activities from the original activity diary (i.e., the same activities as at T1). Participants and the research assistants were all masked to the weights allocated at T1. Based on the newly assigned T2 weights, the “total day score” and “average days score” were recalculated using the original T1 activity diary.
The Activity Card Sort (ACS-NL(18–64))
The ACS-NL(18–64) contains 84 photo cards of activities in the domains of activities of daily life (ADL) (32 items), low physical demand leisure activities (24 items), high physical demand leisure activities (10 items), and social activities (18 items). The 84 activities represent the activities of Dutch adults aged 18 to 64 [Citation22].
The ACS-NL(18-64) was administered using Q-sort methodology with standardized instructions. Comparing their current activities to those performed two years previously, participants sorted the photo cards into six categories (numbers indicate corresponding ratings): Don”t do this anymore (0)–Do it less (0.5)–Starting to do it again (0.5)–Kept doing it [Citation1]–New activity (1)–Never done (0). The activities in the categories Don”t do this anymore–Do it less–Starting to do it again–Kept doing it, were marked as “past,” whereas the activities that were currently performed (categories Do it less–Starting to do it again–Kept doing it–New activity) were marked as “current.” The “percentage of retained activities” was calculated by dividing the sum score of “current” activities by the sum score of “past” activities. Higher scores indicate a higher percentage of retained activities.
In addition, participants rated the importance of the 84 activities using the categories (scores): not at all important (-2), not important (-1), neutral (0), important (1), very important (2). An average importance score was calculated by dividing the total importance scores of the current activities by the number of current activities. Both the percentage of retained activities and the average importance score were used in the analysis.
Occupational Balance Questionnaire (OBQ11-NL)
The OBQ11-NL was translated with the permission of the Swedish authors [Citation23]. The OBQ11-NL consists of 11 statements, each scored on a four-point ordinal scale, ranging from completely disagree (0), disagree (1), agree (2), to completely agree (3). The “total score” is the sum of scores on the 11 items (range 0-33), with higher scores indicating better life balance. For the analyses in the current reliability study the OBQ11-NL total score was used.
Data analyses
All data were entered into the Castor Data Management system. After testing for normalcy, ICC estimates and their 95% confidence intervals were calculated using the SPSS statistical package version 25. ICC estimates were based on single measurement, absolute agreement, 2-way mixed-effects models. Mean estimations along with 95% confidence intervals (CI) were reported for each ICC.
The ICC between T1 and T2 was calculated for the following data:
AC: weight score of each activity and average total day scores;
ACS-NL (18-64): percentage retained activities and average importance score; and
OBQ11-NL: total score.
Interpretation of the results was according to Koo and Li [Citation32]: ICC values less than 0.5 are indicative of poor reliability, values between 0.5 and 0.75 indicate moderate reliability, values between 0.75 and 0.9 indicate good reliability, and values larger than 0.90 indicate excellent reliability.
Bland-Altman plots were used to visualize and quantify absolute assessment consistency for each of the three measures [Citation33]. The differences between T1 and T2 (y-axis) for each participant were plotted against the average values of T1 and T2 (x-axis). For each measure, the variation of the differences at group level was expressed in the 95% limits of agreement (LOA) (mean difference ± 1.96 * standard deviation of the individual differences).
Results
Fifty participants (25 with MM and 25 with FSHD) matched the inclusion criteria and were enrolled. provides a summary of the participants” demographic and clinical characteristics.
Table 1. Demographic and clinical characteristics of participants (n = 50).
Test-retest reliability
Descriptive findings (mean, standard deviation and range) for the three life balance measures at T1 and T2 are reported in . There were no missing data.
Table 2. Descriptive data of the AC, ACS-NL(18-64) and the OBQ11-NL at T1 and T2.
Activity Calculator
Over the three days, the 50 participants logged a total of 1084 activity entries in their activity diaries. The number of entries ranged from 11 to 39 per participant over three days. The AC showed good reliability for the weight scores per activity entry: ICC =0.80 (95% CI 0.77 − 0.82) and excellent reliability for the AC-average total day scores: ICC =0.95 (95% CI 0.91 − 0.97) (). The LOA for AC-average total score ranged from −8.93 to 6.50 ().
Figure 1. Bland-Altman plot of the difference of scores against the mean scores of the AC- average total day score (n = 50). The solid line represents the mean of differences (-1.22). The two dashed lines define limits of agreement (đ ± 1.95*SD = -8.93 - 6.5.
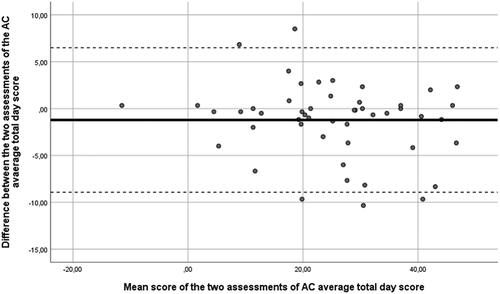
Figure 2. Bland-Altman plot of the difference of scores against the mean scores of the ACS-NL(18-64)-percentage retained activities scores (n = 50). The solid line represents the mean of differences (1.43). The two dashed lines define limits of agreement (đ ± 1.95*SD = -6.91 - 9.77).
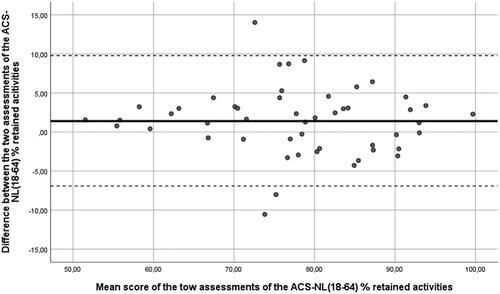
Table 3. Test-retest reliability of the Activity Calculator (AC), Activity Card Sort-NL (18–64) and OBQ11-NL.
Activity Card Sort
The ACS-NL(18-64) showed excellent reliability on retained activities: ICC =0.92 (95% CI 0.86 − 0.96) () and good reliability for the average importance score per current activity: ICC =0.76 (95% CI 0.68 − 0.89) (). The LOA of the ACS-NL(18–64)–percentage retained activities ranged from −6.91 to 9.77 ().
OBQ11-NL
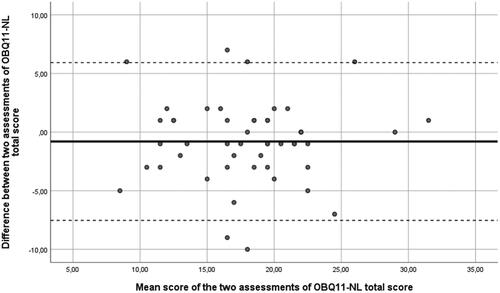
The OBQ11-NL-total score showed good reliability: ICC = .76 (95% CI .62 −.86) (). The LOA of the OBQ11-NL ranged from −7.53 to 5.93 ().
Figure 3. Bland-Altman plot of the difference of scores against the mean scores of the OBQ11-NL (n = 50). The solid line shows the mean absolute difference (-0.80), while the two dashed lines show the absolute limits of agreement: (đ ± 1.95*SD = -7.53–5.93).
Discussion
The results of this study show that three new life balance measures, the AC, ACS-NL(18–64) and the OBQ11-NL are reliable in a Dutch sample of patients with neuromuscular disease. This is the first step in validating these new instruments for the purpose of assessing and evaluating life balance interventions.
Values for the test-retest reliability varied from 0.76 to 0.95 across the measurements. This range in test-retest outcomes could, on the one hand, be explained by differences in content, with each measure addressing a different dimension of life balance. Alternatively, differences may have been due to the method of data collection. The AC is conducted by collecting activity diaries and guided by an interview to measure the weight of activities on a four-point Likert scale; the ACS-NL(18–64) is conducted by q-sort methodology and applies a nominal response scale of answering options and Likert scales to measure the importance of activities; and the OBQ11-NL is a self-report questionnaire with Likert style response scales.
For the AC, which has originally been designed as a tool for clinical practice to gain insight in the burden of activities during different days, we firstly focused on examining the reliability of the weights allocated to the activities, because this is fundamental to calculating a total day score or an average score over a set of days. Importantly, we found that participants in this study consistently gave the same weight scores to the activities. In clinical use of the AC, it is common to record activities for 3–5 days. Based on these 3–5 days, a total average day score is calculated. As can be expected, there are differences in total scores per day, for example between working days and weekend or non-working days. In this study we therefore chose to collect the activity diaries only once (on T1) and recalculated the total average day scores of the same activities allocating new weight scores at T2. In clinical use, we recommend selecting 3–5 days with various activity characteristics (e.g., working days, weekend days) before an intervention and a similar set of days after an intervention. Further research is needed to explore responsiveness of the AC.
The test-retest reliability of the ACS-NL(18–64) in our study was similar to findings in studies of earlier versions [Citation21]. To explore life balance constructs, we complemented the original version of the ACS-NL with an importance scale, to assess whether people with limited energy engage in activities that are important to them. We applied a 5-point Likert scale, varying from not at all important to very important. Likert scales are commonly used in outcome measures, but different lengths of the scale might influence test-retest reliability. Th highest test-retest reliability is found for response scales varying from 7 to 10 points; and the lowest for 3-point scales. The tendency is that the reliability increases with the number of responses and 5-point or 7-point scales score highest in the aspect of “easy to use” [Citation34]. On the other hand response preferences were the 10-point scale, followed by the 7-point and 9-point scale. Currently we are collecting data for construct validity and responsiveness analyses of the life balance measures. After analyses we will consider if there is a need to reconsider the number of responses for the important measure of the ACS-NL(18–64).
The good test-retest reliability of the OBQ11-NL is in agreement with reliability studies of the Spanish version (OBQ11-E), that also found good test–retest reliability (rs = 0.73) [Citation26]. Of the three life balance outcome measures in our study, the OBQ11-NL is the only one specifically designed to measure the construct of life balance. The AC was not specifically designed as an outcome measure and the ACS-NL(18–64) is originally designed for the construct of participation. Further research is needed to enlarge the understanding of the construct of life balance.
In the past few years the increasing interest in the construct of occupational or life balance led to the development of more instruments that are promising in measuring aspects of life balance. We selected the OBQ because of its first impression face validity, user-friendliness and because the OBQ covered different aspects of life balance that were not covered by the other measures [Citation35]. The OBQ has been further developed since the start of our study and has been translated into different languages (Dutch, Norwegian and Spanish), which facilitates international implementation of this instrument.
The strong test-retest reliability of the instruments provides the first evidence for the value as outcome measures, provided that they are conducted according to standardised procedures. These included: 1) trained research assistants for the interviews for the AC and ACS-NL(18–64); 2) scoring cards with descriptions of the meaning of weights (AC) and importance scores (ACS-NL(18–64)); and 3) use of excel spreadsheets to calculate total scores (AC). Occupational therapists who want to apply life balance measures in clinical practice for individual decision making and follow-up are advised to use these measures under these standardized procedures.
The AC and ACS-NL are already well-known in occupational therapy practice as valuable clinical tools to guide occupational therapy interventions. This facilitates their implementation as outcome measures in clinical practice. Still, measuring life balance can be time-consuming for both patients and therapists. For instance, administration of the AC and the ACS-NL(18–64) each require a 30–45 min interview. Digital applications (apps) of the AC and the ACS-NL(18–64) are currently being developed to facilitate easier completion by patients and scoring by therapists. Using app administration of the AC would offer the possibility to prompt participants to record activities every half hour, collecting data in real time, at the moment the activities are performed. We assume that this would improve the accuracy of reporting of activities and reduce the report time needed. For the ACS-NL(18–64) the use of an app or web-based portal would provide the possibility of self-report instead of the time consuming interview [Citation36]. New studies would be needed to demonstrate if similar psychometric results regarding reliability can be achieved using these new digital formats.
Conclusion
Considering the increasing interest in life balance as an important outcome of occupational therapy interventions, it is essential to assess life balance in a reliable way. Our results demonstrate that the AC, ACS-NL(18–64) and the OBQ11-NL all show good to excellent test-retest reliability. Further studies of their construct validity and responsiveness are needed.
In memoriam
Dr. Esther Steultjens contributed extensively to the conceptualization, data collection and article writing. Sadly she was no longer with us when finishing this article. Her input during the research was extremely valuable.
Acknowledgements
First of all, we thank all participants in this study for their time and contribution, especially in view of their limited energy. We thank the patient organization Spierziekten Nederland for their assistance to promote the study and recruit participants. We want to thank the research assistants: Jana Zajec, Eirlys Pijpers, Erwin Jonker and Franny van Bergen-Ubbink for collecting the data. We thank the developers of the measures: Greke Hulstein and Karin ten Hove (Activity Calculator); Soemitro Poerbodipoero and Lennard Bijl (Activity Card Sort-NL); and Carita Håkansson and Petra Wagman (Occupational Balance Questionnaire) for the collaboration and sharing their knowledge.
Disclosure statement
The authors report no conflict of interest. Funding for this work was provided by Prinses Beatrix Spier Fonds [project number W.OK16-04].
Additional information
Funding
References
- Kalkman JS, Schillings ML, van der Werf SP, et al. Experienced fatigue in facioscapulohumeral dystrophy, myotonic dystrophy, and HMSN-I. J Neurol Neurosurg Psychiatry. 2005;76(10):1406–1409.
- Schillings ML, Kalkman JS, Janssen HMHA, et al. Experienced and physiological fatigue in neuromuscular disorders. Clin Neurophysiol. 2007;118(2):292–300.
- Veenhuizen Y, Cup EH, Groothuis JT, et al. Effectiveness and cost-effectiveness of a self-management group program to improve social participation in patients with neuromuscular disease and chronic fatigue: protocol of the energetic study. BMC Neurol. 2015;15:58.
- Lou J-S, Weiss MD, Carter GT. Assessment and management of fatigue in neuromuscular disease. Am J Hosp Palliat Care. 2010;27(2):145–157.
- Anaby D, Jarus T, Backman CL, et al. The role of occupational characteristics and occupational imbalance in explaining well-being. Appl Res Qual Life. 2010;5(2):81–104.
- Backman CL. Occupational balance: exploring the relationships among daily occupations and their influence on well-being. Can J Occup Ther. 2004;71(4):202–209.
- Eklund M, Orban K, Argentzell E, et al. The linkage between patterns of daily occupations and occupational balance: applications within occupational science and occupational therapy practice. Scand J Occup Ther. 2017;24(1):41–56.
- Wassink D, Ven Stevens L. Handreiking ergotherapie bij COVID-19 cliënten in de herstelfase; 2021.
- Evenhuis E, Eyssen IC. Ergotherapierichtlijn vermoeidheid bij MS, CVA of de ziekte van parkinson. Amsterdam: VU medisch centrum Amsterdam, afdeling Revalidatiegeneeskunde sE; 2012.
- Cup EHC, Satink T. Ergotherapierichtlijn QVS–coaching bij activiteiten van het dagelijks leven. Nijmegen: Radboudumc & Hogeschool van Arnhem en Nijmegen; 2017.
- Joseph S. https://www.sjhc.london.on.ca/regional-acquired-brain-injury-outpatient-program/patients/activity-and-exercise#pacing. London: St Joseph Health care; 2013.
- Pinxterhuis I, Hulstein-van Gennep G, Hove-Moerdijk K, et al. Activity calculator, a method for achieving a balanced lifestyle for people with chronic fatigue. JOccup Ther, Iceland. 2019;40(1):26–28.
- Baum CM. History, development and psychometric properties of the Activity Card Sort. Unpublished manusscript. 1995.
- Alegre-Muelas C, Alegre-Ayala J, Huertas-Hoyas E, et al. Spanish transcultural adaptation of the activity card sort. Occup Ther Int [Internet]. 2019;2019:1–9.
- Gustafsson L, de Jonge D, Lai Y, et al. Development of an activity card sort for Australian adults aged 18–64 years. Aust Occup Ther J. 2014;61(6):403–414.
- Hamed R, Holm MB. Psychometric properties of the arab heritage activity card sort. Occup Ther Int. 2013;20(1):23–34.
- Laver-Fawcett AJ, Mallinson SH. Development of the activity card Sort-United Kingdom version (ACS-UK). OTJR. 2013;33(3):134–145.
- Uemura JI, Hoshino A, Igarashi G, et al. Selection of activity items for development of the activity card sort-Japan version. OTJR. 2018;39(1):23–32.
- Packer TL, Boshoff K, DeJonge D. Development of the activity card sort—Australia. Aust Occup Ther J. 2008;55(3):199–206.
- Poerbodipoero SJ, Sturkenboom IH, van Hartingsveldt MJ, et al. The construct validity of the Dutch version of the activity card sort. Disabil Rehabil. 2016;38(19):1943–1951.
- Jong AM, van Nes FA, Lindeboom R. The Dutch activity card sort institutional version was reproducible, but biased against women. Disabil Rehabil. 2012;34(18):1550–1555.
- Alberts N, Borra V, Borrenbergs L. Een bijdrage aan de ontwikkeling van de ACS-NL(18-64) Amsterdam University of applied sciences; 2018.
- Wagman P, Håkansson C. Introducing the occupational balance questionnaire (OBQ). Scand J Occup Ther. 2014;21(3):227–231.
- Wagman P, Håkansson C. Occupational balance from the interpersonal perspective: a scoping review. J Occup Sci. 2019;26(4):537–545.
- Håkansson C, Wagman P, Hagell P. Construct validity of a revised version of the occupational balance questionnaire. Scand J Occup Ther. 2020;27(6):441–449.
- Peral-Gómez P, López-Roig S, Pastor-Mira M, et al. Cultural adaptation and psychometric properties of the Spanish version of the occupational balance questionnaire: an instrument for occupation-based research. Int J Environ Res Public Health. 2021;18(14):7506.
- Uhrmann L, Hovengen I, Wagman P, et al. The Norwegian occupational balance questionnaire (OBQ11-N)–development and pilot study. Scand Jou Occup Therapy. 2019;26(7):546–551.
- Spierziekten-Nederland. Spierziekten.nl 2022 [11-11-2022]. Available from: www.spierziekten.nl.
- Worm-Smeitink M, Gielissen M, Bloot L, et al. The assessment of fatigue: psychometric qualities and norms for the checklist individual strength. J Psychosom Res. 2017;98:40–46.
- Terwee CB, Bot SDM, de Boer MR, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60(1):34–42.
- Christ B, Dijkhuizen R, Epping J et al.De Activiteitenweger, het meten van de zwaarte van activiteiten. In: HAN uoas, editor. Nijmegen, 2018.
- Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15(2):155–163.
- Giavarina D. Understanding bland altman analysis. Biochem Med. 2015;25(2):141–151.
- Taherdoost H. What is the best response scale for survey and questionnaire design; review of different lengths of rating scale/attitude scale/likert scale. Hamed Taherdoost. 2019;8:1–10.
- Dür M, Unger J, Stoffer M, et al. Definitions of occupational balance and their coverage by instruments. Br J Occup Ther. 2015;78(1):4–15.
- Boone A, Wolf T, Carolyn Baum M. Development and testing of an electronic activity card sort. Arch Phys Med Rehabil. 2021;102(10):e83.
