Abstract
Purpose
Brain injuries (traumatic-/nontraumatic, TBI/nTBI) in young patients may lead to problems e.g., decreased health-related quality of life (HRQoL), and causes family impact. Knowledge regarding the family impact and the relationship with patients’ HRQoL over time is scarce. This follow-up study describes family impact/HRQoL and their mutual relationship in young patients (5–24 years) after TBI/nTBI.
Materials and methods
Parents of patients that were referred to outpatient rehabilitation completed the PedsQL™Family-Impact-Module questionnaire to assess the family impact and the parent-reported PedsQL™Generic-core-set-4.0 to assess patients’ HRQoL (lower scores: more family impact/worse HRQoL). Questionnaires were completed at the time of referral to rehabilitation (baseline) and one/two years later (T1/T2). Linear-mixed models were used to examine family impact/HRQoL change scores, and repeated-measure correlations (r) to determine longitudinal relationships.
Results
Two-hundred-forty-six parents participated at baseline, 72 (at T2), median patient’s age at baseline was 14 years (IQR:11–16), and 181 (74%) had TBI. Mean (SD) PedsQL™Family-Impact-Module score at baseline was 71.7 (SD:16.4) and PedsQL™Generic-core-set-4.0: 61.4 (SD:17.0). Over time, PedsQL™Family-Impact-Module scores remained stable, while PedsQL™Generic-core-set-4.0 scores improved significantly(p < 0.05). A moderately strong longitudinal correlation was found between family impact&HRQoL (r = 0.51).
Conclusions
Family impact does not tend to decrease over time but remained a considerable problem, although patients’ HRQoL improved. Next to focusing on patients’ HRQoL, it remains important to consider family impact and offer family support throughout rehabilitation.
This longitudinal study found that in young patients with traumatic brain injury (TBI) or non-traumatic brain injury (nTBI) referred for rehabilitation there is a considerable impact on the family until two years after referral, whereas the patients’ health-related quality of life (HRQoL) improved significantly.
Improvements in patients’ quality of life status may not automatically lead to a decrease of family impact.
Rehabilitation clinicians should monitor the impact on the family over time and provide long-term family support with special attention to parental worrying when needed.
Clinicians should be aware that, despite significant differences between the clinical characteristics of patients with TBI and nTBI, the courses of family impact are very similar.
IMPLICATIONS FOR REHABILITATION
Introduction
Acquired brain injury (ABI) is common among children, adolescents, and young adults under the age of 25 years and can be categorized into traumatic brain injury (TBI; caused by external trauma) and non-traumatic brain injury (nTBI; internal causes) [Citation1,Citation2]. Due to natural brain adaptation, it is expected that in approximately 70% of all ABI cases, most problems experienced by patients reduce within the first year after onset [Citation3–11]. However, about 30% remain with persistent problems that could considerably affect daily life functioning, where the severity of the problems is often related to the type and severity of the initial injury [Citation3–11]. These problems can have a significant negative impact on the patient’s daily life functioning, participation, health-related quality of life (HRQoL) and it can have an impact on the whole family as well [Citation3–11]. TBI or nTBI is a critical and often acute life event in young people and may lead to a considerable impact on the family. The impact can be emotional, social, or financial and include consequences such as increased stress, worrying, and changes in the families’ routines, roles, and responsibilities [Citation8,Citation11]. The impact on the family may be particularly substantial in patients with persistent problems, a subgroup of about 30% of all patients [Citation3–11]. Some of these patients are referred to multidisciplinary rehabilitation, mostly provided in an outpatient rehabilitation setting [Citation12–15].
Previous literature has emphasized the existence of family impact during all stages of recovery of young patients with both TBI and nTBI, i.e., in the acute, subacute, and rehabilitation stages [Citation3,Citation8,Citation11,Citation16–22]. One of those studies described various factors that negatively influenced family impact at the time of referral to rehabilitation. These factors included the time between brain injury onset and referral to rehabilitation of more than six months and the presence of pre-morbid problems in the child [Citation3]. Furthermore, having nTBI resulted in more family impact compared to having TBI [Citation3].
Previous studies also described the relationship between higher parent-reported family impact and a decreased patients’ HRQoL in young patients with chronic diseases, including both TBI and nTBI [Citation3,Citation16,Citation17,Citation20,Citation23,Citation24]. However, most of these studies only reported cross-sectional relations, [Citation3,Citation20] only studied an adult population, [Citation16] or only assessed this relationship in patients with either only general chronic health conditions, [Citation24] or only severe TBI and/or nTBI [Citation17,Citation23,Citation24].
Longitudinal studies, among young children with TBI, found that families experience a long-lasting impact related to their child’s injury for more than 12 months. [Citation25–28]. This was also found in two studies among adult patients with TBI [Citation29,Citation30]. However, these studies only included patients with TBI, and patients with more severe injuries only considered a limited age range of patients (only children or only adults), or only looked at limited aspects of family functioning [Citation25–30].
To date, knowledge regarding the course of family impact and patients’ HRQoL over time in families of young patients in the rehabilitation phase is scarce. Therefore, this study aims to describe differences between patients with TBI and nTBI regarding the family impact and patients’ HRQoL, to describe the course of parent-reported family impact, as well as parent-reported patients’ HRQoL over time in young patients with TBI or nTBI (5–24 years old), referred for outpatient rehabilitation. Furthermore, this study aims to determine the longitudinal relationship between family impact and patients’ HRQoL.
We hypothesize that family impact has decreased and patients’ HRQoL has improved two years after referral to rehabilitation. Furthermore, we hypothesize that family impact decreases less in patients with nTBI compared to TBI. Finally, we hypothesize that there is a longitudinal relationship between a decrease in family impact and an improvement in patients’ HRQoL.
Methods
Design
This longitudinal study was part of a Dutch observational multicentre cohort on family impact, fatigue, participation, and quality of life among young patients (5–24 years) with ABI and their families in the outpatient rehabilitation setting [Citation3,Citation31,Citation32]. The multicentre study was carried out between 2015 and 2019 in ten rehabilitation centers in the Netherlands that were specialised in treating young patients with acquired brain injury. The multicentre study protocol was reviewed by the medical ethical review board of the Leiden University Medical Centre (P15.165), with an exemption from full medical ethical review being provided as the data were collected as part of routine care. All local research committees from the participating centers approved the study as well. All data used in the multicentre study were anonymised before analysis and securely stored in a central database by a data manager at Basalt Rehabilitation (The Hague, The Netherlands). In the current study, only parent-reported data were used. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines were used for the reporting of the results [Citation33].
Participants
Participants in the current study were parents of young patients (5–24 years) with ABI that were referred by a family practitioner or medical specialist to one of the ten outpatient rehabilitation centers. Participants were not eligible if they were unable and/or limited to write and/or understand the Dutch language. The current study included 246 parents with a child with either a TBI or nTBI between 5–24 years old admitted for rehabilitation in one of the participating centres. More than half of the patients (52%) were female and 74% of the patients had a diagnosis of TBI, which provided us with a good cross-section of the general Dutch ABI population [Citation1,Citation34].
Assessments
Patient and family characteristics
At baseline, the patient’s demographics- and injury characteristics were collected from their medical records by the treating physician i.e., sex (male/female/other), age, and the cause of brain injury, which was divided into a TBI group, a nTBI group, and a total group. TBI severity levels were divided into three groups: mild and moderate/severe/’unknown’ (based on the Glasgow coma scale [Citation35]). If the GCS was unknown but there was no history of conscious loss, the severity level was also considered ‘mild’. Causes of nTBI were divided into stroke, brain tumours, meningitis or encephalitis, hypoxia or intoxication, and ‘other’. Since there are no valid/commonly used instruments to measure nTBI severity, no nTBI severity levels were noted. The time between TBI/nTBI onset (date of injury) and referral to the rehabilitation centre was calculated and divided into ‘less than six months’ or ‘more than six months’ after onset (< 6 months/> 6 months). The family characteristics included: single-parent household/two parents, siblings/no siblings, the cultural background of the parents (Dutch/non-Dutch), and parents’ educational levels (low (prevocational practical education or less)/intermediate (prevocational theoretical education and upper secondary vocational education)/high (secondary education, higher education, and university level education)).
Outcome measures
To measure family impact and HRQoL the Pediatric Quality of Life Inventory™Family Impact Module (PedsQL™FIM) [Citation36] and the Pediatric Quality of Life Inventory™Generic Core Scales-4.0 (PedsQL™GCS-4.0) were used [Citation37–39]. These instruments have good psychometric properties, and they have previously been validated and used among young patients with TBI and nTBI. Dutch language versions for both outcomes were available [Citation3,Citation21,Citation36,Citation40–42].
- Family impact
The 36-item PedsQ™FIM questionnaire was used to assess family impact. A four-point Likert scale from ‘never’ to ‘almost always’ was used to answer the questions. It yields a total score and four domain scores. The four domains were: ‘parental quality of life summary score’ (e.g., “I have trouble getting support from others”) with twenty items, a ‘family functioning summary score’ (e.g., “Stress or tension between family members”) with eight items, the domain ‘worrying’ (e.g., “I worry about my child’s future”) with five items, and the domain ‘communication’ (e.g., “It is hard for me to talk about my child’s health with others”) with three items. After completion, the scores were linearly transformed on a scale from 0 to 100 (0 = 100, 1 = 75, 2 = 50, 3 = 25, 4 = 0). The total and domain scores were calculated by the sum of the items answered, divided by the number of items answered, resulting in a score ranging from 0 to 100, where lower scores indicate more (i.e., worse) parent-reported family impact [Citation36].
- Health-related quality of life (HRQoL)
The 23-item parent-reported PedsQL™GCS-4.0 was used to measure patients’ HRQoL. It yields a total score and four domain scores, i.e., physical functioning (eight items), emotional functioning (five items), social functioning (five items), and school/work functioning (five items). Scores are calculated in the same manner as with the PedsQL™FIM. It is also resulting in a score ranging from 0–100 with lower scores indicating lower HRQoL [Citation37–39].
Procedure
Participants filled out an online questionnaire that contained the above-described outcome measures (PedsQL™FIM and PedsQL™GCS-4.0). Before completing the questionnaire, parents (and/or patients where appropriate) signed an informed consent to participate. Prior to the first appointment with the rehabilitation physician (baseline), parents received a link by email to complete an online questionnaire (via www.questback.nl). One year (T1) and two years (T2) after the first appointment, parents were invited to complete the questionnaire again voluntarily.
Statistical analysis
All data were analysed for the TBI group, the nTBI group, and the total group separately and at the three time points (baseline, T1, and T2). Descriptive statistics were used for all characteristics and variables. Continuous variables were expressed as medians (with interquartile ranges; IQR) or means (with standard deviations; SD), based on their distributions (Kolmogorov–Smirnoff test). Independent sample T-tests were performed to determine differences in outcomes between the TBI and the nTBI groups at all time points and presented as t-values (t), degrees of freedom (Df), and p-values.
To check if the known missing data at T1/T2 were ‘missing completely at random’ (MCAR) and therefore suitable to use in a linear mixed model (LMM), Little’s-test was performed [Citation43]. Results of this test showed that cases were MCAR (Chi-Square of 22.4, p 0.07), allowing analysis in a LMM where missing repeated measures are being corrected within the model. [Citation44] In the LMM, the follow-up time points were the fixed effects, and the participants were the random effects. The PedsQL™FIM and the PedsQL™GCS-4.0 scores were expressed as means with standard deviations (SD) at baseline. Change scores (with 95% confidence intervals; 95% CI) were computed between baseline and T1, between T1 and T2, and between baseline and T2. All analyses in the LMM were corrected for age and sex. All above-described data were analysed using SPSS software, version 28.0 (IBM SPSS Statistics for Mac, Armonk, NY: IBM Corp).
To determine longitudinal correlations between the PedsQL™FIM and the PedsQL™GCS-4.0, repeated measures correlations (rmcorr) were used. With this method, the non-independence of repeated measures was considered by determining the relationship between two continuous variables (the PedsQL™MFS and the PedsQL™GCS-4.0) where between-patient variance is being controlled [Citation45]. All analyses in the repeated measure correlations (rmcorr) were corrected for age and sex as well. The results were noted as correlation coefficients (r), 95% Confidence Intervals (95%CI), and p-values. The correlation coefficients’ strength can be considered: >0.8 = very strong; 0.6 up to 0.8 = moderately strong; 0.3 to 0.5 = fair; and < 0.3 = poor [Citation46]. For this method, ‘R’ version 4.1.0, and the rmcorr module, version 0.5.2 were used [Citation45].
The level of statistical significance was set at p < 0.05 for all analyses.
Results
In total, 246 parents of young patients with TBI or nTBI participated in this study. At the one- and two-year follow-ups (T1/T2), 71 and 72 parents completed the questionnaires, respectively (). presents the demographic, injury, and family characteristics at baseline. The median age of the patients in the total group was 14 years (IQR 11–16). Seventy-four percent (n = 181) had a TBI, of which 78% were classified as ‘mild’. In the nTBI group (n = 65, 26%), 40% had a brain tumour, and 24% had a stroke. Ninety-six (40%) of the patients were referred for outpatient rehabilitation more than six months after the onset of the brain injury and 17% of the patients were living in a single-parent household.
Figure 1. Flow chart of the participants in this study.
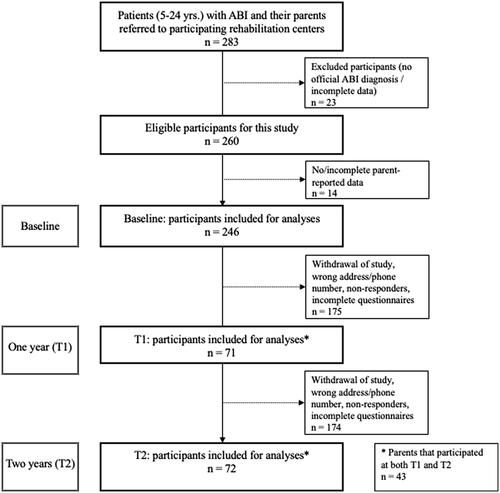
Table 1. Demographic, injury, and family characteristics in children, adolescents, and young adults with TBI/nTBI, referred to outpatient rehabilitation, at baseline.
Family impact and HRQoL: TBI versus nTBI
As seen in , the total mean (SD) PedsQL™FIM score in the TBI group at baseline was 73.8 (SD 19.2), and 65.6 (SD 15.7) in the nTBI group. For all groups at baseline, the lowest scores, i.e., more family impact, were found on the ‘worrying’ domain and the highest on the domain ‘communication’.
Table 2. Differences in parent reported family impact and patients’ Health related quality of life between patients with TBI and nTBI at baseline and one and two years later.
A significant difference was found between the TBI group and the nTBI group concerning family impact total and almost all domain scores at baseline (total score; t = 3.6, Df = 116, p < 0.001), at T1 (total score; t = 2.1, Df = 54, p = 0.04), and at T2 (total score; t = 2.4, Df = 32, p = 0.02), except for the domain ‘parental-HRQoL summary score’ at T1 (t = 1.4, Df = 57, p = 0.08) and T2 (t = 1.5, Df = 36, p = 0.07). The total mean (SD) PedsQL™GCS-4.0 score at baseline was 61.9 (SD 16.9) for the TBI group and 60.0 (SD 17.3) for the nTBI group. For all groups, the lowest scores were found on the ‘School/work functioning’ domain and the highest on the ‘social functioning’ domain. Regarding HRQoL scores between the TBI group and the nTBI group, significant differences were only found on the domains ‘emotional functioning’ (p < 0.05 at baseline) and ‘social functioning’ (p < 0.05 at all time points).
Family impact over time
PedsQL™FIM change scores, analysed with the linear mixed model (LMM) between baseline and T1, between T1 and T2, and between baseline and T2 are presented in .
Table 3. Parent-reported family impact over the course of time.
The total group
In the total group, the total change score between baseline and T1 was: +2.2 (95%CI −2.3;6.7, p > 0.05), and in the second year (between T1 and T2); +1.7 (95%CI −4.1;7.5, p > 0.05). Only significant improvement was found in the ‘worrying’ domain, between baseline and T1: +6.9 (95%CI 1.5;12.3) p < 0.05, and between baseline and T2: +9.9 (95%CI 4.5;15.3), p < 0.001. Scores on the ‘communication’ domain decreased in 2 years over time (baseline-T2) yet, not significantly: −1.2 (95%CI −8.1;5.8) p > 0.05.
The TBI group
In the TBI group, the improvement of the total score in the first year (baseline-T1) was: +2.8 (95%CI −2.6;8.2, p > 0.05) and +0.4 (95%CI −6.6;7.5, p > 0.05) between T1 and T2. In line with the results from the total group, significant improvement between baseline and T2 was seen on the domain ‘worrying’ (p < 0.05) and a (non-significant) decrease in the domain ‘communication’ between baseline and T2.
The nTBI group
Regarding the nTBI group, improvements of PedsQL™FIM total scores in the first year and the second were: +2.3 (95%CI −5.3;9.9), and +3.2 (95%CI 6.8;13.2) yet both were non-significant (p > 0.05). In almost all domain scores more improvements were seen in the second year, except on the ‘worrying’ domain where most improvement was seen between baseline and the first year: +10.0 (95%CI 1.0;18.9, p < 0.05).
HRQoL in young patients over time
PedsQL™GCS-4.0 change scores between all time points are presented in .
Table 4. Parent-reported Health-Related Quality of Life (HRQoL) for their child over the course of time.
The total group
The change scores for the total score in the total group were +9.6 (95%CI 4.9;13.8, p < 0.001) in the first year and +1.4 (95%CI 4.2;7.2, p > 0.05) in the second. Similar results were found in all domain scores with the largest overall improvement on the domain school/work functioning (baseline-T2): +17.7 (95%CI 11.7;23.7, p < 0.001).
The TBI group
Significant improvement in PedsQL™GCS-4.0 total scores in the first year was found: +10.8 (95%CI 5.2;16.4), p < 0.001. Change scores were non-significant in the second year: +1.1 (95%CI −5.9;8.1), p > 0.05. Significant improvements were found between baseline and T1 in all domain scores (p < 0.05).
The nTBI group
Overall less improvement was found in the nTBI group regarding the HRQoL outcomes compared to the TBI group (in the total score and all domain scores).
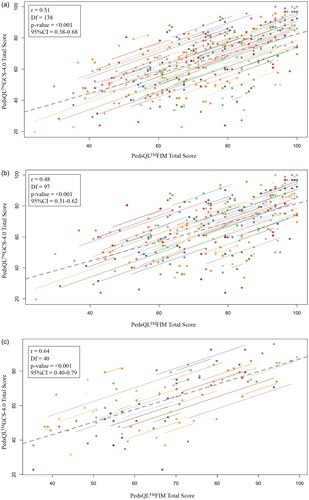
Relationship between family impact and HRQoL
The longitudinal correlations between PedsQL FIM (family impact) and PedsQL GCS-4.0 (HRQoL) over time for the total/TBI/nTBI groups can be found in . Regarding the total group a fair longitudinal correlation was found over time: r = 0.51 (95%CI: 0.38–0.68, p < 0.001). A fair longitudinal correlation between family impact and HRQoL in the TBI group r = 0.48 (95%CI: 0.31–0.62, p < 0.001). A moderately strong correlation was found in the nTBI group r = 0.64 (95%CI: 0.40–0.79, p < 0.001) for nTBI, respectively.
Figure 2. (a) Longitudinal correlation between Family impact (PedsQL™FIM) and HRQoL (PedsQL™GCS-4.0) in the total group. LEGEND: PedsQL™FIM: Pediatric Quality of Life Inventory™Family Impact Module. PedsQL™GCS-4.0: Pediatric Quality of Life Inventory™Generic Core Scales-4.0. * Correlation coefficient (r): very strong = > 0.8; moderately strong = 0.6 to 0.8; fair = 0.3 to 0.5; and poor = < 0.3. # p-value <0.05 = statistically significant. Df: Degrees of freedom, 95%CI = 95% Confidence Interval. Analyses were corrected for age and sex. (b) Longitudinal correlation between Family impact (PedsQL™FIM) and HRQoL (PedsQL™GCS-4.0) in the TBI group. LEGEND: PedsQL™FIM: Pediatric Quality of Life Inventory™Family Impact Module. PedsQL™GCS-4.0: Pediatric Quality of Life Inventory™Generic Core Scales-4.0. TBI: Traumatic brain injury. * Correlation coefficient (r): very strong = > 0.8; moderately strong = 0.6 to 0.8; fair = 0.3 to 0.5; and poor = < 0.3. # p-value <0.05 = statistically significant. Df: Degrees of freedom, 95%CI = 95% Confidence Interval. Analyses were corrected for age and sex. (c) Longitudinal correlation between Family impact (PedsQL™FIM) and HRQoL (PedsQL™GCS-4.0) in the nTBI group. LEGEND: PedsQL™FIM: Pediatric Quality of Life Inventory™Family Impact Module. PedsQL™GCS-4.0: Pediatric Quality of Life Inventory™Generic Core Scales-4.0. nTBI: Non-traumatic brain injury. * Correlation coefficient (r): very strong = > 0.8; moderately strong = 0.6 to 0.8; fair = 0.3 to 0.5; and poor = < 0.3. # p-value <0.05 = statistically significant. Df: Degrees of freedom, 95%CI = 95% Confidence Interval. Analyses were corrected for age and sex.
Discussion
This longitudinal multicentre study among parents of young patients (5–24 years) with TBI or nTBI found considerable family impact and decreased patients’ HRQoL at the time of referral to outpatient rehabilitation (baseline). Significant differences in family impact were found between the TBI and nTBI groups with more family impact in the nTBI group. Contrary to what we hypothesized, only a slight decrease in family impact in both the TBI and the nTBI groups over two years after referral to rehabilitation was found and was non-significant (in the total and almost all domain scores). This was a large contrast with patients’ HRQoL, which improved significantly over time in both groups. A fair longitudinal relationship between decreased family impact and an improvement in patients’ HRQoL was found in the TBI group, whereas moderately strong relationships were found in the nTBI group.
Results showed a significant difference in family impact scores between the TBI and nTBI groups at all time points, whereas the nTBI group had significantly lower scores both at baseline and almost all time points. When looking at the change scores, the course of family impact over time differed among the TBI and nTBI groups as well. Family impact in the TBI group tended to decrease the most in the first year after referral to rehabilitation, while in the nTBI group, family impact decreased more between the first and second year after referral.
This could be explained by the fact that nTBI has a less predictable prognosis compared to TBI, which could require more time for family adjustment. This rehabilitation-based study revealed more family impact in both the TBI and nTBI groups at the time of referral to rehabilitation compared to a Dutch hospital-based study (our TBI group: 73.8 SD 16.2, our nTBI group: 65.6 SD 15.7 versus TBI: 83.6 SD16.2, nTBI: 70.8 SD19.6 in the hospital study) [Citation21]. This can be explained by the fact that patients in our cohort were referred for rehabilitation due to persisting TBI- or nTBI-related daily life problems that cause considerable impact on families compared to a hospital cohort where patients may have improved considerably in the acute of subacute phase after their brain injury. In conclusion, family impact persists in both groups with a different trajectory over time but is always higher than in a hospital cohort [Citation21]. These results underline the importance of measuring the impact on families over time and taking the cause of brain injury into account during the different stages of recovery.
Until now, knowledge on parent-reported family impact over time in families with a child with persisting problems after a TBI or nTBI is scarce. The findings of our study suggest that in the two years after referral to rehabilitation only the aspect ‘worrying’ decreased significantly within families in both the TBI and nTBI groups. This contrasts with our hypothesis that family impact would decrease over time in all domains among families with a child that suffered from a brain injury. This finding is in line with previous hospital- or community-based studies in families of children with TBI, that did not find a decrease of family impact one year after brain injury onset as well [Citation25–30].
Comparisons of our results with those from previous studies must be done with caution as studies are different with respect to age, causes, daily life functioning, and presence of persisting problems [Citation25–30]. The reasons for the persistence of family impact remain unclear, but it could be hypothesized that factors such as suboptimal long-term care, lack of information, or unrealistic expectations regarding the prognosis could play a role. During rehabilitation, the focus lies on the patient by improving HRQoL and participation abilities and there might be less focus on their families which could overshadow the potential still-existing family problems that are not fully considered. These results and considerations underline the importance of focusing on the patients’ families in all phases of recovery and over time.
Contrary to the results of the course of family impact over time, almost no significant differences were found regarding patients’ HRQoL between the TBI and nTBI groups at all time points. In both the TBI and nTBI groups, the patients’ HRQoL mean scores reported by parents were considerably low at baseline compared to scores from healthy peers i.e., between 82.1 (SD: 8.9) and 83.9 (SD:13.1) depending on the age, versus 61.4 (SD: 17.0) in our total group of young patients with TBI/nTBI [Citation40,Citation41]. Furthermore, even though HRQoL improved significantly over time in both groups, scores remained considerably lower compared to healthy peers [Citation40,Citation41]. Furthermore, in line with family impact scores in our study, HRQoL scores are lower compared to scores in the hospital-based study by de Kloet et al. (despite the similarities between the populations) [Citation21]. This can be explained by the fact that patients in our cohort were all referred to outpatient rehabilitation with persisting daily life problems after TBI/nTBI while we assume that only a subpopulation of the hospital cohort needed a referral to outpatient rehabilitation. The results of our study underline the importance of measuring and monitoring patients’ HRQoL over time in clinical practice to monitor improvement or decrease in patients’ functioning.
Regarding the relationship between family impact and HRQoL results showed that family impact and HRQoL had a moderately strong correlation when measuring individual patients over time in the total group. However, significant differences between de TBI and nTBI groups were found, where a moderately strong longitudinal correlation between family impact and patients’ HRQoL was found in the nTBI group yet, only a ‘fair’ correlation in the TBI group. These results were contrary to the expectation of strong correlations between family impact and HRQoL over time for both the TBI and nTBI groups. Only a few previous studies have described associations between patients’ diminished HRQoL and a higher parent-reported family impact among patients with chronic diseases (including TBI and nTBI) [Citation3,Citation16,Citation20,Citation23,Citation24]. However, these studies did not include patients older than 18 years of age or did not measure these associations over time [Citation3,Citation16,Citation20,Citation23,Citation24]. Furthermore, these studies found only investigated correlations between family impact and HRQoL on the group level (and did not consider individual repeated measurements on the same patients). The current study can be considered the first that investigated the correlation between FI and HRQoL over time using a method that takes into account the individual non-independence of repeated measurements on the same patients. To conclude, strong correlations between outcome measures at one time point in a whole group do not automatically seem to correlate as strongly in the individual patient over time. Therefore, these results suggest looking into the individual patient and his/her family when measuring FI and HRQoL is important for using these measures in clinical practice.
Strengths and limitations
This study had several limitations. First, only parent-reported data were analysed, while siblings or perspectives from other family members were not included. However, to date, the PedsQLTMFIM is the only outcome measure that assesses the impact on the family in several domains. Future research should focus on developing outcome measures and/or modifying the PedsQLTMFIM to consider including perspectives of other important people in the lives of patients with TBI/nTBI. Furthermore, there is no normative data for the general population in The Netherlands; this data would give insight into the course of family impact during the development of healthy children and could help to better interpret outcomes of studies in TBI/nTBI.
Second, many participants were lost to follow-up. An explanation for this is that the questionnaires at the time that a patient was referred for rehabilitation were completed in terms of routine care, while one and two years later, parents were asked to complete the questionnaires voluntarily, often after the patient no longer had visits to the clinic. The relatively high non-response (even after a significant number of reminders) could be decreased by sharing the results directly after the administration of the questionnaires and involving the patient and parents in the results and the importance of testing over time. Nevertheless, missing data were missing completely at random, meaning that missing data in the dataset happened by coincidence (the observed values at T1 and T2 in the dataset are a random sample from the dataset when it would have been complete). Furthermore, we used two statistical methods that took repeated measures into account within the same participant, and we thereby corrected for missing observations (a linear mixed model to determine change over time and repeated measure correlations to determine correlations over time).
Third, there were 20 patients in the TBI (12%) group with unknown TBI severity levels (based on the GCS). However, in all these patients there was no history of conscious loss, and therefore the severity level could be also considered ‘mild’, which was confirmed by all treating rehabilitation physicians in all participating rehabilitation centers. This may suggest that some patients designated as having a mild injury might be young patients with concussions, which may have influenced outcomes. However, even in these patients persisting problems were found for which they had been referred for rehabilitation.
Fourth, in our study, we found differences in family impact between the TBI and the nTBI group, whereas in the nTBI group greater family impact was found. This could possibly be explained by the initial between-sample differences in the severity of injury-related disability and the expected duration of symptoms. To outline these differences, we chose to report outcomes for both groups separately as well.
Fifth, the authors acknowledge the lack of additional (parental) information e.g., parental mental and physical health, disability status, extra-family support potential, and patients’ needed care from parents to look into additional potential correlations with the PedsQL™FIM. We recommend collecting more detailed data on characteristics of parental functioning in future research.
Finally, the results of the questionnaires could be biased by the parents’ motivation, stress, and mood at the time of completion.
Conclusions
This study showed that family impact in families with a child who suffers from a TBI or nTBI referred for rehabilitation treatment is considerable, especially in patients with a nTBI. In general, the impact on the family remains stable over time, even though patients’ HRQoL improved. The findings of this study underline the importance of measuring and monitoring family impact and HRQoL over time. Furthermore, it is important to investigate family impact separately for patients with TBI and patients with nTBI as both groups follow a different course over time. Future studies should focus on selecting and evaluating approaches during rehabilitation treatment that both increases the HRQoL of the patient and reduces family impact after a child has either TBI or nTBI.
Clinical Message: Next to focusing on the patient’s HRQoL, it is important to monitor the wishes and needs of the family and support them throughout the rehabilitation process since the improvement of the patient’s HRQoL does not always automatically lead to reduced family impact.
Acknowledgments
The authors thank all families who participated in this study for filling out the questionnaires as part of usual care at baseline and all families who voluntarily filled out the questionnaires 1 and 2 years later after the first appointment. Additionally, the authors thank all clinical healthcare professionals and medical secretaries of participating rehabilitation centers for providing the data. Finally, the authors thank Bart Mertens (biostatistician) for advising us regarding the statistical analyses in this study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- de Kloet AJ, Hilberink SR, Roebroeck ME, et al. Youth with acquired brain injury in The Netherlands: a multi-Centre study. Brain Inj. 2013;27(7-8):843–849.
- Greenwald BD, Burnett DM, Miller MA. Congenital and acquired brain injury. 1. Brain injury: epidemiology and pathophysiology. Arch Phys Med Rehabil. 2003;84(3 Suppl 1):S3–S7.
- Allonsius F, De Kloet AJ, Van Markus-Doornbosch F, et al. Parent-reported family impact in children and young adults with acquired brain injury in the outpatient rehabilitation setting. Brain Inj. 2021;35(5):563–573.
- Anaby D, Law M, Hanna S, et al. Predictors of change in participation rates following acquired brain injury: results of a longitudinal study. Dev Med Child Neurol. 2012;54(4):339–346.
- Arakelyan S, Maciver D, Rush R, et al. Family factors associated with participation of children with disabilities: a systematic review. Dev Med Child Neurol. 2019;61(5):514–522.
- Camara-Costa H, Francillette L, Opatowski M, et al. Participation seven years after severe childhood traumatic brain injury. Disabil Rehabil. 2019;42(17):2402–2411.
- Camara-Costa H, Opatowski M, Francillette L, et al. Self- and parent-reported quality of life 7 years after severe childhood traumatic brain injury in the traumatisme grave de l’Enfant cohort: associations with objective and subjective factors and outcomes. Qual Life Res. 2020;29(2):515–528.
- Rashid M, Goez HR, Mabood N, et al. The impact of pediatric traumatic brain injury (TBI) on family functioning: a systematic review. J Pediatr Rehabil Med. 2014;7(3):241–254.
- van Markus-Doornbosch F, van der Holst M, de Kloet AJ, et al. Fatigue, participation and quality of life in adolescents and young adults with acquired brain injury in an outpatient rehabilitation cohort. Dev Neurorehabil. 2020;23(5):328–335.
- Ilmer EC, Lambregts SA, Berger MA, et al. Health-related quality of life in children and youth with acquired brain injury: two years after injury. Eur J Paediatr Neurol. 2016;20(1):131–139.
- Grant CJ, Doig LF, Everson J, et al. Impact of patient and family involvement in Long-Term outcomes. Crit Care Nurs Clin North Am. 2020;32(2):227–242.
- Knight S, Takagi M, Fisher E, et al. A systematic critical appraisal of Evidence-Based clinical practice guidelines for the rehabilitation of children With moderate or severe acquired brain injury. Arch Phys Med Rehabil. 2019;100(4):711–723.
- Anderson V, Catroppa C. Advances in postacute rehabilitation after childhood-acquired brain injury: a focus on cognitive, behavioral, and social domains. Am J Phys Med Rehabil. 2006;85(9):767–778.
- Reuter-Rice K, Eads JK, Berndt S, et al. The initiation of rehabilitation therapies and observed outcomes in pediatric traumatic brain injury. Rehabil Nurs. 2018;43(6):327–334.
- Forsyth R. The difference rehabilitation can make after acquired brain injury. Dev Med Child Neurol. 2022;64(1):7.
- Hocking MC, Hobbie WL, Deatrick JA, et al. Neurocognitive and family functioning and quality of life among young adult survivors of childhood brain tumors. Clin Neuropsychol. 2011;25(6):942–962.
- Moscato E, Patronick J, Wade SL. Family functioning and adaptation following pediatric brain tumor: a systematic review. Pediatr Blood Cancer. 2022;69(2):e29470.
- Moore M, Robinson G, Mink R, et al. Developing a Family-Centered care model for critical care After pediatric traumatic brain injury. Pediatr Crit Care Med. 2015;16(8):758–765.
- Hickey L, Anderson V, Jordan B. Australian parent and sibling perspectives on the impact of paediatric acquired brain injury on family relationships during the first 6 weeks at home. Health Soc Care Community. 2022;30(6):e5204–e5212.
- Brown FL, Whittingham K, Sofronoff K, et al. Parenting a child with a traumatic brain injury: experiences of parents and health professionals. Brain Inj. 2013;27(13-14):1570–1582.
- de Kloet AJ, Lambregts SA, Berger MA, et al. Family impact of acquired brain injury in children and youth. J Dev Behav Pediatr. 2015;36(5):342–351.
- Jones S, Tyson S, Yorke J, et al. The impact of injury: the experiences of children and families after a child’s traumatic injury. Clin Rehabil. 2021;35(4):614–625.
- Tramonti F, Bonfiglio L, Di Bernardo C, et al. Family functioning in severe brain injuries: correlations with caregivers’ burden, perceived social support and quality of life. Psychol Health Med. 2015;20(8):933–939.
- Huang IC, Anderson M, Gandhi P, et al. The relationships between fatigue, quality of life, and family impact among children with special health care needs. J Pediatr Psychol. 2013;38(7):722–731.
- Wade SL, Gerry Taylor H, Yeates KO, et al. Long-term parental and family adaptation following pediatric brain injury. J Pediatr Psychol. 2006;31(10):1072–1083.
- Rivara JM, Jaffe KM, Polissar NL, et al. Predictors of family functioning and change 3 years after traumatic brain injury in children. Arch Phys Med Rehabil. 1996;77(8):754–764.
- Micklewright JL, King TZ, O’Toole K, et al. Parental distress, parenting practices, and child adaptive outcomes following traumatic brain injury. J Int Neuropsychol Soc. 2012;18(2):343–350.
- Yeates KO, Taylor HG, Rusin J, et al. Premorbid child and family functioning as predictors of post-concussive symptoms in children with mild traumatic brain injuries. Int J Dev Neurosci. 2012;30(3):231–237.
- Ponsford J, Schonberger M. Family functioning and emotional state two and five years after traumatic brain injury. J Int Neuropsychol Soc. 2010;16(2):306–317.
- Sady MD, Sander AM, Clark AN, et al. Relationship of preinjury caregiver and family functioning to community integration in adults with traumatic brain injury. Arch Phys Med Rehabil. 2010;91(10):1542–1550.
- Allonsius F, van Markus-Doornbosch F, de Kloet AJ, et al. Fatigue in young patients with acquired brain injury in the rehabilitation setting: categorizing and interpreting fatigue severity levels. Dev Neurorehabil. 2022;25(8):542–553.
- Allonsius F, de Kloet A, Bedell G, et al. Participation restrictions among children and young adults with acquired brain injury in a pediatric outpatient rehabilitation cohort: the patients’ and parents’ perspective. Int J Environ Res Public Health. 2021;18(4):1625.
- Cuschieri S. The STROBE guidelines. Saudi J Anaesth. 2019;13(Suppl 1):S31–S34.
- van Pelt DE, de Kloet A, Hilberink SR, et al. The incidence of traumatic brain injury in young people in the catchment area of the university hospital rotterdam, The Netherlands. Eur J Paediatr Neurol. 2011;15(6):519–526.
- Jain S, Iverson LM. Glasgow coma scale. Treasure Island (FL): StatPearls; 2020.
- Varni JW, Sherman SA, Burwinkle TM, et al. The PedsQL family impact module: preliminary reliability and validity. Health Qual Life Outcomes. 2004;2:55.
- Varni JW, Burwinkle TM, Lane MM. Health-related quality of life measurement in pediatric clinical practice: an appraisal and precept for future research and application. Health Qual Life Outcomes. 2005;3:34.
- Varni JW, Burwinkle TM, Seid M, et al. The PedsQL 4.0 as a pediatric population health measure: feasibility, reliability, and validity. Ambul Pediatr. 2003;3(6):329–341.
- Varni JW, Limbers CA, Burwinkle TM. Parent proxy-report of their children’s health-related quality of life: an analysis of 13,878 parents’ reliability and validity across age subgroups using the PedsQL 4.0 generic core scales. Health Qual Life Outcomes. 2007;5:2.
- Engelen V, Haentjens MM, Detmar SB, et al. Health related quality of life of dutch children: psychometric properties of the PedsQL in The Netherlands. BMC Pediatr. 2009;9:68.
- Limperg PF, Haverman L, van Oers HA, et al. Health related quality of life in dutch young adults: psychometric properties of the PedsQL generic core scales young adult version. Health Qual Life Outcomes. 2014;12:9.
- Medrano GR, Berlin KS, Hobart Davies W. Utility of the PedsQL family impact module: assessing the psychometric properties in a community sample. Qual Life Res. 2013;22(10):2899–2907.
- Roderick JAL. A test of missing completely at random for multivariate data with missing values. J Am Stat Assoc. 1988;83(404):1198–1202.
- Heymans MW, Eekhout I. Applied Missing Data Analysis With SPSS and R(Studio). 2019. https://bookdown.org/mwheymans/bookmi/.
- Bakdash JZ, Marusich LR. Repeated measures correlation. Front Psychol. 2017;8:456.
- Chan YH. Biostatistics 104: correlational analysis. Singapore Med J. 2003;44(12):614–619.
