Abstract
Purpose
To determine needs, expectations, facilitators, and barriers of insurance physicians (IPs) for using eHealth in their work. Also, we investigated differences between age groups.
Materials and methods
All insurance physicians employed at the Dutch Social Security Institute (SSI) received an online anonymous survey in July 2020.
Results
Three hundred and fifteen IPs (31%) responded. According to these IPs, the most important need for using eHealth was to collect medical information more effectively and efficiently (71%).
Main facilitators were that eHealth could make IPs’ work more effectively and efficiently (61%) and more future-proof (60%). Main barriers were losing human interaction (54%) and security issues (51%). Younger IPs saw more options for using eHealth, compared to older IPs.
Conclusions
The majority of IPs (in particular younger IPs) had a positive view towards using eHealth in their daily work. Nevertheless, differences in needs, expectations, facilitators and barriers between the age groups should be taken into account for the successful development and implementation of interventions using eHealth in insurance medicine.
Implications for Rehabilitation
For the successful development and implementation of eHealth interventions in insurance medicine and rehabilitation, the needs, expectations, facilitators, and barriers that physicians indicate should be taken into account.
Insurance physicians support the use of eHealth interventions to collect medical information more effectively and efficiently, to contribute to and maintain the quality of care, in the perspective of managing expected shortages in insurance physicians.
When concretizing eHealth interventions for rehabilitation professionals, one should take the importance of face to face interaction with patients into account.
Extra education and training for older insurance physicians may improve the implementation of eHealth interventions, because they are less inclined to see its value and feel less competent to use it.
Introduction
In the last decade, eHealth has increasingly been used to provide, deliver, and improve healthcare [Citation1]. The COVID pandemic further increased its use out of necessity, but also turned out to be a great catalyst for eHealth interventions [Citation2,Citation3]. According to the World Health Organization (WHO), eHealth is the cost-effective and secure use of information and communication technologies (ICT) in support of health and health-related fields. It encompasses multiple interventions, including telehealth, telemedicine, mobile health (mHealth), electronic medical or health records (eMR/eHR), big data, wearables, and even artificial intelligence [Citation4,Citation5]. eHealth is thus a complex term. To better grasp this term for our participants, we referred to eHealth in this study as eHealth interventions, interventions that are delivered through new technologies, such as ICT-solutions (decision rule), applications on smartphones, wearables or the use of artificial intelligence.
Interesting examples of eHealth interventions being employed in medical fields adjacent to insurance medicine are telehealth for physical medicine and rehabilitation [Citation6], internet-based exercise interventions for cancer survivors [Citation7], and online interventions for supporting mental health concerns, such as anxiety disorders and depression [Citation8–10]. Studies show that eHealth interventions could contribute in important and positive ways to health care outcomes, such as by improving effectiveness, quality of care [Citation11,Citation12], and reducing health care costs [Citation13,Citation14]. For example, telehealth has been shown to improve access to care in areas with provider shortages, enhance efficiency and convenience (by reducing patient travel and wait times), and allow for comparable or improved health care quality [Citation15–17].
Despite the associated benefits and the diligent exploration of eHealth interventions in health care within the medical field, however, the use of eHealth within insurance medicine (IM) is still remarkably scarce. IM is distinct from general health care in that IPs take a monitoring and assessment perspective in which symptoms of sickness are translated to work ability, whereas other medical disciplines take a more curative approach towards disease. Even so, both fields care for populations with underlying medical complaints and/or diseases. We, therefore, suspect that eHealth interventions could add value to the field of IM just as it does to general medicine. EHealth interventions could support IPs in their work by improving the quality and efficiency of work disability assessments and in their advisory role on issues concerning return to work. Likewise, eHealth interventions could offer improved opportunities for empowering persons with disability benefits and promoting return-to-work outcomes [Citation18].
In addition to supporting healthcare professionals in their work, the use of eHealth interventions may also contribute to solving another urgent problem in the near future, namely the expected shortage of healthcare professionals, including IPs. This problem arises due to a substantial group of older healthcare professionals retiring, combined with a low influx of younger healthcare professionals to take over their work [Citation18]. Using eHealth interventions like telehealth in IM might serve as a promising solution for addressing this capacity problem -at least in part- by offering patients access to medical expertise even when IPs are not available to be physically present [Citation19,Citation20].
To enhance positive outcomes in the development and implementation of promising eHealth interventions, it is important to understand healthcare professionals’ perspectives on the use of these technologies in their daily clinical practice [Citation21,Citation22]. Therefore, we conducted a needs assessment with insurance physicians (IPs). This needs assessment was the first step in the six-step behavioral change protocol of Intervention Mapping. The collected needs from the survey are important to identify specific objectives and goals (step 2) of the eHealth intervention program for IM we strive to develop and evaluate. Following the Intervention Mapping protocol, next, we will design and develop the intervention using theory-based intervention methods and practical applications (step 3), generate an adaptation and implementation plan (steps 4 and 5), and finally create an evaluation plan (step 6) in order to evaluate the developed intervention for insurance physicians [Citation23,Citation24].
We were also interested in the differences and similarities between younger and older IPs in their views towards the use of eHealth interventions. Age is an important factor of digital literacy and thus can lead to different views on the use of eHealth interventions [Citation25]. Acknowledging and investigating these age-related differences could give better direction to the implementation strategy of eHealth interventions [Citation26,Citation27].
In the present study, we therefore aimed to investigate needs, expectations, facilitators, and barriers of IPs with respect to the use of eHealth interventions in their daily practice by means of a cross-sectional survey. Our secondary aim was to explore whether differences existed in our findings between younger and older IPs.
Materials and methods
Study design and ethics
In this cross-sectional study, an online survey was distributed among IPs working at the Dutch SSI to investigate their needs, expectations, and facilitators and barriers to their use of eHealth interventions in the daily practice. The Dutch SSI is an autonomous semi-governmental agency in the Netherlands that assesses work disability and return to work services support of claimants. In addition, the SSI provides and regulates disability benefits payments.
Survey-data was collected anonymously. The study was approved by the Medical Ethical Committee of the VU University Medical Centre as a non-WMO research study (registration number 2020.372).
Development and content of the online survey
Survey questions were (wherever possible) based on existing, validated surveys – the MIDI (Measurement Instrument for Determinants of Innovations) [Citation27] in particular. Where necessary, questions were adjusted to our specific target population and their work content. These adjustments were made in consensus with all authors and reviewed by a selection of researchers and stakeholders to ensure all changes were adequate. For more detailed information about the content of the survey, we refer to .
When applicable, the statements in the survey questioned the possible contribution of eHealth interventions to (a) the quality of the work of insurance physicians and (b) the efficiency and effectiveness. A “contribution to quality” meant that interventions live up to clients demands of proper insurance medicine services. A “contribution to efficiency and effectiveness” meant that the interventions accomplish for clients what these are intended for, with maximum benefits relative to invested efforts.
Study population and data collection
All IPs (N = 1022) were registered or in-training and working at the SSI. Participants were approached by email by the first researcher. This email provided a link to an online survey. Two reminders were sent to the IPs at intervals of one and three weeks after the first invitation. Data were collected in July and August 2020. After approximately four weeks, the survey was taken offline and data was locked and collected (11 August 2020). For the construction of the survey and data collection Survalyzer software (Survalyzer Nederland BV, Utrecht, the Netherlands) was used.
The first page of the survey obtained informed consent for participation and the anonymous use of participant data. Researchers could not link the incoming data to the participants and thus could not identify responders and non-responders. An indication of non-response bias was provided by comparing demographics of participants with demographic data about the general population of IPs, which was obtained with permission of the SSI.
Statistics and statistical analysis
Data were analyzed using SPSS version 26 (IBM Inc., Armonk, NY, USA). Descriptive statistics were used to report demographic and professional characteristics. Descriptive data from the total population working at the SSI was collected.
General characteristics of the participants
Of the 1022 invited respondents, 315 IPs (31%) participated in and completed the survey. Due to the anonymous design of the survey, information on non-participation could not be retrieved. The majority of participants were male (52%), age 40 or older (69%), with a mean age of 49.3, SD± 13.4), registered as an IP (64%), and had more than 15 years of work experience at the SSI (46%). In the total population of IPs at the SSI, 48% of IPs were male and the mean age of 49 years (SD± 13.3). These characteristics appear to reflect those of the participant sample. Years of work experience are unknown for the total population.
Results
The results of each of the sections of the survey (general characteristics, needs, expectations, facilitators, and barriers) are presented separately. The statements that the majority of the total group agreed with are discussed, followed by the description of the differences between IPs under the age of 40 and IPs over 40 years. Finally, we discuss the items where the majority of the total group did not agree with and subsequently, the differences between the age groups.
Needs for the use of eHealth
The majority of IPs (50% or more) agreed to all three statements related to efficiency and effectiveness of eHealth interventions. 71% concerning collection of medical information, 66% regarding disability assessments, and 55% for return to work services (see ). With respect to the statements pertaining “quality,” the majority of IPs only agreed on the statements about collecting of medical information (68%), and disability assessments (52%).
Figure 1. Agreement with the statements of all participating IPs (total (agree)), the IPs under 40 (age < 40 years (agree)) and the IPs 40 and older (age ≥ 40 years (agree)). The cut-off age of 40 years was based on previous studies about digital literacy and the specific characteristics of this population (mean age, work experience, educational level)) [Citation21,Citation26,Citation28]. A five-point Likert response scale was provided to specify the level of agreement to each statement, with higher scores indicating elevated agreement. Choices of responses consisted of: “strongly disagree,” “disagree,” “neither agree nor disagree,” “agree,” “strongly agree.” The category “neither agree nor disagree” was added to “disagree.” Differences were analyzed with a Pearson’s chi-squared test and significant differences (p < 0.05) are marked with an asterisk (*).
![Figure 1. Agreement with the statements of all participating IPs (total (agree)), the IPs under 40 (age < 40 years (agree)) and the IPs 40 and older (age ≥ 40 years (agree)). The cut-off age of 40 years was based on previous studies about digital literacy and the specific characteristics of this population (mean age, work experience, educational level)) [Citation21,Citation26,Citation28]. A five-point Likert response scale was provided to specify the level of agreement to each statement, with higher scores indicating elevated agreement. Choices of responses consisted of: “strongly disagree,” “disagree,” “neither agree nor disagree,” “agree,” “strongly agree.” The category “neither agree nor disagree” was added to “disagree.” Differences were analyzed with a Pearson’s chi-squared test and significant differences (p < 0.05) are marked with an asterisk (*).](/cms/asset/57057c8f-61fb-4fd0-8f36-c6e8a5be133b/idre_a_2224083_f0001_b.jpg)
In general, IPs under 40 years were more likely than IPs of 40 years and older to agree that they would like to use eHealth interventions to improve the quality (65% vs. 46%; χ2 = 10,24, p = 0.001) and efficiency and effectiveness (78% vs. 61%; χ2 = 8,57, p = 0.003) of work disability assessments, as well as to improve the quality (86% vs 44%; χ2 = 20,87, p = 0.000) and efficiency and effectiveness (82% vs 60%; χ2 = 7,78, p = 0.005) of the collection of medical information. For the need to improve the effectiveness of return to work services, no significant differences between the younger and older age groups were found (see ).
Only a minority agreed on the statement to improve the quality of return to work services (48%). No significant differences between the younger and older age groups were found (see ).
Expectations for the use of eHealth
The primary areas in which the majority of IPs expected that eHealth interventions could support their work most, were in collecting information about daily activities of a claimant, based on a chronological story of activities on a random day (63%) and the monitoring of health (62%) (see ). The majority of the total group also agreed with the items concerning: functional capacities, personal and social functioning, cognitive symptoms, dynamic actions, and recovery behavior.
Figure 2. Agreement with the statements of all participating IPs (total (agree)), the IPs under 40 (age < 40 years (agree)) and the IPs 40 and older (age ≥ 40 years (agree)). The cut-off age of 40 years was based on previous studies about digital literacy and the specific characteristics of this population (mean age, work experience, educational level)) [Citation21,Citation26,Citation28]. A five-point Likert response scale was provided to specify the level of agreement to each statement, with higher scores indicating elevated agreement. Choices of responses consisted of: “strongly disagree,” “disagree,” “neither agree nor disagree,” “agree,” “strongly agree.” The category “neither agree nor disagree” was added to “disagree.” Differences were analyzed with a Pearson’s chi-squared test and significant differences (p < 0.05) are marked with an asterisk (*).
![Figure 2. Agreement with the statements of all participating IPs (total (agree)), the IPs under 40 (age < 40 years (agree)) and the IPs 40 and older (age ≥ 40 years (agree)). The cut-off age of 40 years was based on previous studies about digital literacy and the specific characteristics of this population (mean age, work experience, educational level)) [Citation21,Citation26,Citation28]. A five-point Likert response scale was provided to specify the level of agreement to each statement, with higher scores indicating elevated agreement. Choices of responses consisted of: “strongly disagree,” “disagree,” “neither agree nor disagree,” “agree,” “strongly agree.” The category “neither agree nor disagree” was added to “disagree.” Differences were analyzed with a Pearson’s chi-squared test and significant differences (p < 0.05) are marked with an asterisk (*).](/cms/asset/73f111e7-e625-4d21-ae1b-16f13250633d/idre_a_2224083_f0002_b.jpg)
IPs under 40 had overall higher expectations with regard to all presented statements.
A minority (<50% of the IPs) agreed with the items: prognosis, psychosocial symptoms, working environment, statistic postures, working hours and endurance, and return to work services. Also here, IPs under 40 years were more likely to have higher expectations in comparison to IPs of 40 years and older.
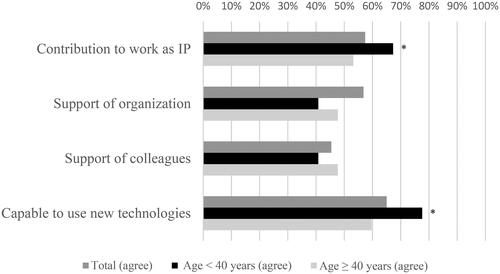
Regarding the statements about the execution of the medical aspect of their work, the majority of IPs (57%) expected that eHealth interventions could contribute (see , Appendix A). Sixty-five percent of IPs felt capable enough to use eHealth interventions in their work. With regard to social support, 57% of IPs expected that they would receive sufficient support from their organization to use eHealth interventions.
IPs under 40 were significantly more likely to have high expectations of the contribution of eHealth (67% vs 53%; χ2 = 5.49, p = 0.02). IPs under the age of 40 likewise felt more competent in using eHealth in their work than their older colleagues (78% vs 60%; χ2 = 9.46, p = 0.002).
Only a minority (45%) expected sufficient support from their colleagues. IPs under 40 agreed even less on this item than their older colleagues (41%).
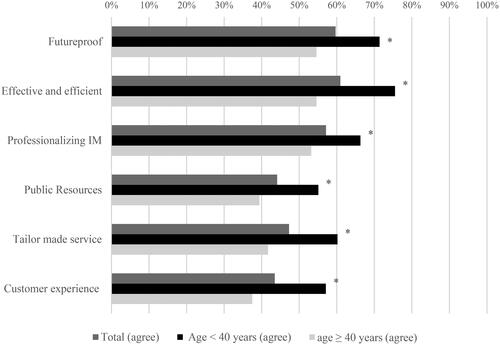
Facilitating factors for the use of eHealth
The most important facilitators to use eHealth interventions in their work according to the IPs were that the technologies could make their work more effective and efficient (61%), more future-proof (60%) and they could contribute to the further professionalization of IM (57%) (see , Appendix A).
The majority of IPs younger than 40 years were more likely than older IPs to agree with all the presented facilitators in this study. The biggest differences in agreement between the two age groups were on the items suggesting that eHealth interventions could make their work more “efficient and effective” (χ2 = 12.37, p = 0.000) or could improve the “customer experience” (χ2 = 10.58, p = 0.001) and the “tailor-made service” (χ2 = 9.29, p = 0.001).
While the minority of the total group of IPs agreed with regard to the items about public resources, tailor made services, and customer experience, the majority of IPs younger than 40 actually agreed with these items compared to their older colleagues.
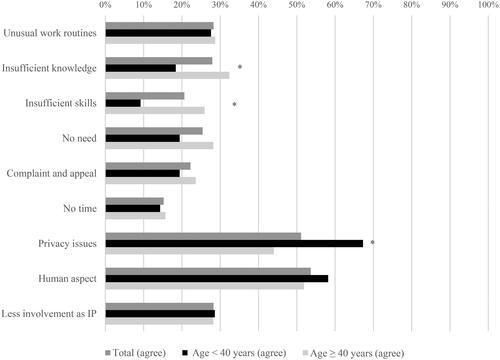
Barriers for the use of eHealth
Reduction of the human aspect in work (54%) and concerns about privacy and security of medical information (51%) were indicated by the participants as the main barriers to the use of eHealth interventions in the field of IM (, see Appendix A).
The opinions of IPs under 40 were quite similar to those of IPs 40 and older with regard to barriers. Their opinions differed significantly on only three out of nine barriers. IPs 40 and older agreed more often that insufficient knowledge (χ2 = 6.56, p = 0.010) and insufficient skills (χ2 = 11.55, p = 0.001) were barriers for making use of eHealth interventions in their work. IPs younger than 40 years old were more likely to experience privacy concerns as a barrier for the use of eHealth interventions than older IPs (χ2 = 11.51, p = 0.000).
A minority of IPs indicated unusual work routines, insufficient knowledge and skills, no need, no time, and filing complaints and appeal as a barrier to use eHealth interventions.
Discussion
In the present study, we investigated the view of IPs towards the use of eHealth and the presence of age related differences. The results showed that IPs saw the need for using eHealth, especially for collecting medical information and conducting disability assessments. They expected eHealth to be useful in assessing daily activities, health and recovery behavior. Important barriers included concerns about privacy and reduction of human interaction with their clients.
We found that, for IPs, one of the most important facilitators to use eHealth was making daily work processes more effective and efficient. In line with our results, other studies have also shown that increasing the effectiveness and efficiency of work is an important facilitator for using eHealth. Efficiency was found to be important for healthcare professionals in the adoption of eHealth such as mobile health and social media [Citation29,Citation30]. A study in which clinical psychologists in the Netherlands were interviewed about drivers and barriers in adopting e-mental Health tools showed that increased efficiency in administrative tasks was one of the practical benefits [Citation31].
A main barrier was the prospect of reduced face-to-face contact in the process of medical assessment of work disability. A similar disadvantage of eHealth interventions was reported by other healthcare providers using e-mental health or telehealth. These health care providers believed that a face-to-face setting is crucial for an accurate understanding of their client because of the ability to identify subtle signs in facial expressions, posture, and appearance [Citation31–33]. Nevertheless, blended care (with a reduction of face-to-face contact) showed promising results as a good alternative for traditional care, without affecting quality of treatment and beneficial outcomes [Citation34].
More than half of the IPs in our study identified privacy issues as a barrier for the use of eHealth. Other studies have also shown that the security of medical and personal information is a prerequisite for healthcare professionals to use eHealth. A systematic literature review on the perceived barriers of physicians to using electronic medical records found that physicians have doubts about the security and confidentiality of patient data [Citation35]. Another review on telemedicine supports these findings and also expressed concerns about the patients’ privacy [Citation19,Citation36]. In addition, clinicians in primary care using remote monitoring technology had concerns about legal liability when using and relying on technology [Citation37].
IPs 40 and older had more concerns about insufficient skills and knowledge, which was consistent with the outcomes of earlier studies that demonstrated differences in the level of digital literacy which is being highly associated with age [Citation38–40]. Younger IPs seem to have more experience with the advantages and challenges of using eHealth, which likely explains why they had positive expectations and were more confident about using eHealth in their work [Citation25,Citation41]. Other studies showed that physicians with previous experience with telemedicine scored its utility higher and perceived greater possibilities or benefits in its use [Citation21]. Affinity with technology more generally also has an impact on the adoption of eHealth. A qualitative Cochrane review among healthcare workers showed that those who were accustomed to using mHealth had more positive experiences and perceptions towards the use of mHealth [Citation42]. Another noticeable element was that a larger portion of the younger professionals found privacy issues to be a barrier to use eHealth compared to their older colleagues, which could also be due to higher level of digital literacy and experience among the younger professionals [Citation41,Citation43].
Strengths and limitations of this study
This cross-sectional survey was, to the best of our knowledge, the first survey-based study among IPs which questioned their needs, expectations, facilitators, and barriers related to the use of eHealth [Citation38]. Moreover, we consider the relatively high participation rate in this study, 31% of the entire population of IPs working at the SSI, to be a strength. The high participation rate might indicate the work-related use of eHealth to be a main point of interest to IPs nowadays. Furthermore, we consider it to be a strength that the selection of IPs that participated in this study appeared to be representative of the general population of IPs working at the SSI in demographical terms.
In addition, the timing of our study during the first wave of the COVID-19 pandemic was convenient. The survey was sent approximately two months after IPs had to change their daily practical routines drastically. These changes required them to adapt quickly in real life to non-traditional and more technologically-supported work routines and had significantly increased insights into the use of eHealth in their work [Citation40]. The question remains whether the changed attitude due to obliged use of eHealth will prove to be sustainable when all COVID-19 restrictions have been phased out [Citation44,Citation45].
Another potential limitation of our study is that selection bias might have occurred. We presume that IPs with an overall more positive attitude towards the usefulness of eHealth, would have been more likely to respond to our online survey than IPs with a less positive attitude towards the use of technology. This selection bias is also known from other studies investigating physicians and is called “prototypically representative sample” [Citation46].
Taking into account that a higher affinity and experience with the use of eHealth leads to better adherence and adoption of technology [Citation21,Citation47], one would need to be aware of a potential overestimation of the level of adoption when involving IPs in further developing eHealth interventions.
Secondly, we may have overlooked perspectives about the usefulness of eHealth as a result of the multiple-choice format of the survey. To minimize this limitation, we added open ended questions to offer IPs the opportunity to fill in missing suggestions. Analyses of the open-ended questions showed that most of the topics were covered in the survey.
Another limitation of this study may be that we used a broad definition to capture the quantity and complex diversity of interventions based on eHealth. We acknowledge that investigating the vision of IPs with more concrete and specific examples of eHealth interventions might have led to different outcomes due to technology-specific functionalities.
Additionally, we only included the perspectives of IPs and not of other important stakeholders such as persons with disability benefits, other professionals working at the SSI, and policy makers in this survey.
Finally, our approach to combine answering categories “neither agree nor disagree,” “disagree,” and “strongly disagree” might have underestimated the positive results about the vision of IPs regarding the use of eHealth interventions. We argued that by doing so, we are more certain that the participants who “agreed” could be identified as having a positive view towards the use of eHealth.
Recommendations for future research
Combining our results with insights from other important stakeholders, such as persons with a work disability and experts with knowledge about applying eHealth in the medical field, would result in a higher chance of successful development and implementation of eHealth into the daily practice of IPs [Citation48,Citation49]. Moreover, involving a diverse group of stakeholders will improve the acceptance and adoption of eHealth.
Complementary to our findings, we suggest a more in-depth analysis of similarities and differences, not only between the behavior of age groups among IPs themselves, but also between IPs versus their colleagues in adjacent medical fields. Also, identifying other contextual and external factors that influence the use of eHealth interventions in daily practice is important. In addition, efforts should be made to increase knowledge, experience, and training in digital skills for IPs in order to lower the threshold for starting to use eHealth in daily practice. Addressing these factors early in the process of developing interventions using eHealth, enables better understanding of the experiences and wishes of IPs and will lead to a more customized approach and training plan regarding the different levels of eHealth literacy among IPs.
According to the literature, solutions for improving deficits in knowledge and insufficient digital skills and competencies with regard to digitalization also lie in involving healthcare professionals in the decision-making process, combined with education and technological skill training [Citation31,Citation45].
Practical implications
This study shows that the majority of IPs believe eHealth can play a significant role in improving and supporting their work, having both personal benefits and benefits for their clients and organizations. eHealth can support, aid, and improve the work of medical professionals by diminishing the negative impacts that an increasing workload and changing demands of society and clients may have.
This study was conducted in a specific group of medical professionals – insurance physicians – who work within the public domain of insurance at one Dutch organization. Therefore, caution should be taken to extrapolate our results to other rehabilitation professionals working in a different political, juridical context, region or domain.
Despite the promise these technologies hold on paper, however, studies have shown that implementing eHealth interventions in daily practice and routines can take time due to mechanisms of behavioral change. Age (influenced by experience and digital skills) is likely to influence the process of adopting eHealth [Citation25]. Our results suggest that older IPs mainly above the age of 40 may benefit from extra training and education focused on increasing their skills for using eHealth interventions in their work.
Conclusion
This study shows that the majority of IPs have a relatively positive view towards the use of eHealth in their daily work, with younger IPs being generally more positive than their older colleagues. The results of this study can be used as relevant starting points for the development and implementation of interventions based on eHealth in the field of IM, in which age differences should be taken into account.
Disclosure statement
The authors E. Muller and J. v. Rijssen are employed at the SSI. Author J. R. Anema holds a chair in Insurance Medicine on behalf of the SSI. All authors declare that they have no conflict of interest in the analysis and interpretation of the data, in writing the paper, or in the decision to submit the paper for publication.
Additional information
Funding
References
- World Health Assembly, 58. 2005. Fifty-eighth world health assembly, Geneva, 16-25 may 2005: resolutions and decisions: annex. Geneva: World Health Organization.
- Doraiswamy S, Abraham A, Mamtani R, et al. Use of telehealth during the COVID-19 pandemic: scoping review. J Med Internet Res. 2020;22(12):e24087. doi: 10.2196/24087.
- Punia V, Nasr G, Zagorski V, et al. Evidence of a rapid shift in outpatient practice during the COVID-19 pandemic using telemedicine. Telemed J E Health. 2020;26(10):1301–1303. doi: 10.1089/tmj.2020.0150.
- Oh H, Rizo C, Enkin M, et al. What is eHealth (3): a systematic review of published definitions. J Med Internet Res. 2005;7(1):e1. doi: 10.2196/jmir.7.1.e1.
- Eysenbach G. What is e-health? J Med Internet Res. 2001;3(2):E20. doi: 10.2196/jmir.3.2.e20.
- Tenforde AS, Hefner JE, Kodish-Wachs JE, et al. Telehealth in physical medicine and rehabilitation: a narrative review. Pm R. 2017;9(5s):S51–S58. doi: 10.1016/j.pmrj.2017.02.013.
- Galiano-Castillo N, Cantarero-Villanueva I, Fernández-Lao C, et al. Telehealth system: a randomized controlled trial evaluating the impact of an internet-based exercise intervention on quality of life, pain, muscle strength, and fatigue in breast cancer survivors. Cancer. 2016;122(20):3166–3174. doi: 10.1002/cncr.30172.
- Andersson G. Internet-Delivered psychological treatments. Annu Rev Clin Psychol. 2016;12:157–179. doi: 10.1146/annurev-clinpsy-021815-093006.
- Andersson G, Titov N. Advantages and limitations of internet-based interventions for common mental disorders. World Psychiatry. 2014;13(1):4–11. doi: 10.1002/wps.20083.
- Barak A, Hen L, Boniel-Nissim M, et al. A comprehensive review and a meta-analysis of the effectiveness of internet-based psychotherapeutic interventions. J Technol Hum Serv. 2008;26(2–4):109–160. doi: 10.1080/15228830802094429.
- Ball MJ, Lillis J. E-health: transforming the physician/patient relationship. Int J Med Inform. 2001;61(1):1–10. doi: 10.1016/s1386-5056(00)00130-1.
- Samoocha D, Bruinvels DJ, Elbers NA, et al. Effectiveness of web-based interventions on patient empowerment: a systematic review and meta-analysis. J Med Internet Res. 2010;12(2):e23. doi: 10.2196/jmir.1286.
- Elbert NJ, van Os-Medendorp H, van Renselaar W, et al. Effectiveness and cost-effectiveness of ehealth interventions in somatic diseases: a systematic review of systematic reviews and meta-analyses. J Med Internet Res. 2014;16(4):e110. doi: 10.2196/jmir.2790.
- de la Torre-Díez I, López-Coronado M, Vaca C, et al. Cost-utility and cost-effectiveness studies of telemedicine, electronic, and mobile health systems in the literature: a systematic review. Telemed J E Health. 2015;21(2):81–85. doi: 10.1089/tmj.2014.0053.
- Gajarawala SN, Pelkowski JN. Telehealth benefits and barriers. J Nurse Pract. 2021;17(2):218–221. doi: 10.1016/j.nurpra.2020.09.013.
- Donelan K, Barreto EA, Sossong S, et al. Patient and clinician experiences with telehealth for patient follow-up care. Am J Managed Care. 2019;25(1):40–44.
- Kruse CS, Krowski N, Rodriguez B, et al. Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ Open. 2017;7(8):e016242. doi: 10.1136/bmjopen-2017-016242.
- OECD. The looming crisis in the health workforce. 2008. Available from: https://www.oecd-ilibrary.org/social-issues-migration-health/the-looming-crisis-in-the-health-workforce_9789264050440-en
- Xyrichis A, Iliopoulou K, Mackintosh NJ, et al. Healthcare stakeholders’ perceptions and experiences of factors affecting the implementation of critical care telemedicine (CCT): qualitative evidence synthesis. Cochrane Database Syst Rev. 2021;2:CD012876.
- OECD. Systems EOoH, policies. The Netherlands: Country Health Profile; 2019.
- Ruiz Morilla MD, Sans M, Casasa A, et al. Implementing technology in healthcare: insights from physicians. BMC Med Inform Decis Mak. 2017;17(1):92. doi: 10.1186/s12911-017-0489-2.
- Ross J, Stevenson F, Lau R, et al. Factors that influence the implementation of e-health: a systematic review of systematic reviews (an update). Implement Sci. 2016;11(1):146.
- Bartholomew LK, Parcel GS, Kok G, et al. Planning health promotion programs: an intervention mapping approach. New York: John Wiley & Sons; 2011.
- Dalum P, Schaalma H, Kok G. The development of an adolescent smoking cessation intervention–an intervention mapping approach to planning. Health Educ Res. 2012;27(1):172–181. doi: 10.1093/her/cyr044.
- Tennant B, Stellefson M, Dodd V, et al. eHealth literacy and web 2.0 health information seeking behaviors among baby boomers and older adults. J Med Internet Res. 2015;17(3):e70. doi: 10.2196/jmir.3992.
- Kuek A, Hakkennes S. Healthcare staff digital literacy levels and their attitudes towards information systems. Health Informatics J. 2020;26(1):592–612. doi: 10.1177/1460458219839613.
- Fleuren MA, Paulussen TG, Van Dommelen P, et al. Towards a measurement instrument for determinants of innovations. Int J Qual Health Care. 2014;26(5):501–510. doi: 10.1093/intqhc/mzu060.
- Blank G, Groselj D. Dimensions of internet use: amount, variety, and types. Inform Commun Soc. 2014;17(4):417–435. doi: 10.1080/1369118X.2014.889189.
- Antheunis ML, Tates K, Nieboer TE. “Patients’ and health professionals’” use of social media in health care: motives, barriers and expectations. Patient Educ Couns. 2013;92(3):426–431. doi: 10.1016/j.pec.2013.06.020.
- Han KJ, Subramanian R, Cameron GT. Listen before you leap: Sri Lankan health professionals’ perspectives on m-health. Health Informatics J. 2019;25(3):858–866. doi: 10.1177/1460458217725903.
- Feijt MA, de Kort YA, Bongers IM, et al. Perceived drivers and barriers to the adoption of emental health by psychologists: the construction of the levels of adoption of emental health model. J Med Internet Res. 2018;20(4):e153. doi: 10.2196/jmir.9485.
- Perle JG, Langsam LC, Randel A, et al. Attitudes toward psychological telehealth: current and future clinical psychologists’ opinions of internet-based interventions. J Clin Psychol. 2013;69(1):100–113. doi: 10.1002/jclp.21912.
- Vigerland S, Ljótsson B, Gustafsson F, et al. Attitudes towards the use of computerized cognitive behavior therapy (cCBT) with children and adolescents: a survey among Swedish mental health professionals. Internet Interventions. 2014;1(3):111–117. doi: 10.1016/j.invent.2014.06.002.
- van der Vaart R, Witting M, Riper H, et al. Blending online therapy into regular face-to-face therapy for depression: content, ratio and preconditions according to patients and therapists using a Delphi study. BMC Psychiatry. 2014;14:355. doi: 10.1186/s12888-014-0355-z.
- Boonstra A, Broekhuis M. Barriers to the acceptance of electronic medical records by physicians from systematic review to taxonomy and interventions. BMC Health Serv Res. 2010;10:231. doi: 10.1186/1472-6963-10-231.
- Langarizadeh M, Tabatabaei MS, Tavakol K, et al. Telemental health care, an effective alternative to conventional mental care: a systematic review. Acta Inform Med. 2017;25(4):240–246. doi: 10.5455/aim.2017.25.240-246.
- Davis MM, Freeman M, Kaye J, et al. A systematic review of clinician and staff views on the acceptability of incorporating remote monitoring technology into primary care. Telemed J E Health. 2014;20(5):428–438. doi: 10.1089/tmj.2013.0166.
- Hennemann S, Beutel ME, Zwerenz R. Ready for eHealth? Health professionals’ acceptance and adoption of eHealth interventions in inpatient routine care. J Health Commun. 2017;22(3):274–284. doi: 10.1080/10810730.2017.1284286.
- Chesser A, Burke A, Reyes J, et al. Navigating the digital divide: a systematic review of eHealth literacy in underserved populations in the United States. Inform Health Soc Care. 2016;41(1):1–19. doi: 10.3109/17538157.2014.948171.
- Naszay M, Stockinger A, Jungwirth D, et al. Digital age and the public eHealth perspective: prevailing health app use among Austrian internet users. Inform Health Soc Care. 2018;43(4):390–400. doi: 10.1080/17538157.2017.1399131.
- Wilkowska W, Ziefle M. Privacy and data security in E-health: requirements from the user’s perspective. Health Informatics J. 2012;18(3):191–201. doi: 10.1177/1460458212442933.
- Odendaal WA, Anstey Watkins J, Leon N, et al. Health workers’ perceptions and experiences of using mHealth technologies to deliver primary healthcare services: a qualitative evidence synthesis. Cochrane Database Syst Rev. 2020;3:CD011942.
- Wernhart A, Gahbauer S, Haluza D. eHealth and telemedicine: practices and beliefs among healthcare professionals and medical students at a medical university. PLoS One. 2019;14(2):e0213067. doi: 10.1371/journal.pone.0213067.
- Wind TR, Rijkeboer M, Andersson G, et al. The COVID-19 pandemic: the ‘black swan’ for mental health care and a turning point for e-health. Internet Interv. 2020;20:100317. doi: 10.1016/j.invent.2020.100317.
- Guitton MJ. Something good out of something bad: eHealth and telemedicine in the Post-COVID era. Comput Human Behav. 2021;123:106882. doi: 10.1016/j.chb.2021.106882.
- Linden M, Muschalla B, Noack N, et al. Treatment changes in general practice patients with chronic mental disorders following a psychiatric-psychosomatic consultation. Health Serv Res Manag Epidemiol. 2018;5:2333392818758523. doi: 10.1177/2333392818758523.
- Feijt M, de Kort Y, Bongers I, et al. Mental health care goes online: practitioners’ experiences of providing mental health care during the COVID-19 pandemic. Cyberpsychol Behav Soc Netw. 2020;23(12):860–864. doi: 10.1089/cyber.2020.0370.
- Schreiweis B, Pobiruchin M, Strotbaum V, et al. Barriers and facilitators to the implementation of eHealth services: systematic literature analysis. J Med Internet Res. 2019;21(11):e14197. doi: 10.2196/14197.
- Damhus CS, Emme C, Hansen H. Barriers and enablers of COPD telerehabilitation - a frontline staff perspective. Int J Chron Obstruct Pulmon Dis. 2018;13:2473–2482. doi: 10.2147/COPD.S167501.
Appendix A
shows agreement with the statements of all participating IPs (total (agree)), the IPs under 40 (age < 40 years (agree)) and the IPs 40 and older (age ≥ 40 years (agree)). The cut-off age of 40 years was based on previous studies about digital literacy and the specific characteristics of this population (mean age, work experience, educational level) [Citation21,Citation26,Citation28].
Figure A1. Behavioral expectations of IPs with respect to the use of eHealth.
A five-point Likert response scale was provided to specify the level of agreement to each statement, with higher scores indicating elevated agreement. Choices of responses consisted of: “strongly disagree,” “disagree,” “neither agree nor disagree,” “agree,” “strongly agree.” The category “neither agree nor disagree” was added to “disagree.” Differences were analyzed with a Pearson’s chi-squared test and significant differences (p < 0.05) are marked with an asterisk (*).
Figure A2. Facilitators for using eHealth in their work.
shows agreement with the statements of all participating IPs (total (agree)), the IPs under 40 (age < 40 years (agree)) and the IPs 40 and older (age ≥ 40 years (agree)). The cut-off age of 40 years was based on previous studies about digital literacy and the specific characteristics of this population (mean age, work experience, educational level)) [Citation21,Citation26,Citation28].
A five-point Likert response scale was provided to specify the level of agreement to each statement, with higher scores indicating elevated agreement. Choices of responses consisted of: “strongly disagree,” “disagree,” “neither agree nor disagree,” “agree,” “strongly agree.” The category “neither agree nor disagree” was added to “disagree.” Differences were analyzed with a Pearson’s chi-squared test and significant differences (p < 0.05) are marked with an asterisk (*).
Figure A3. Barriers related to the use of eHealth.
shows agreement with the statements of all participating IPs (total (agree)), the IPs under 40 (age < 40 years (agree)) and the IPs 40 and older (age ≥ 40 years (agree)). The cut-off age of 40 years was based on previous studies about digital literacy and the specific characteristics of this population (mean age, work experience, educational level)) [Citation21,Citation26,Citation28].
A five-point Likert response scale was provided to specify the level of agreement to each statement, with higher scores indicating elevated agreement. Choices of responses consisted of: “strongly disagree,” “disagree,” “neither agree nor disagree,” “agree,” “strongly agree.” The category “neither agree nor disagree” was added to “disagree.” Differences were analyzed with a Pearson’s chi-squared test and significant differences (p < 0.05) are marked with an asterisk (*).
Table A1. Questions in the online survey (by section).
