Abstract
Purpose
To determine the course of adherence to physical activity (PA) recommendation in hip/knee osteoarthritis patients before and after hip/knee arthroplasty (THA/TKA). Moreover, we explored predictors for non-adherence 12 months postoperatively.
Materials and methods
Primary THA/TKA were included in a multicenter observational study. Preoperatively and 6/12 months postoperatively, patients reported engagement in moderate-intensity PA in days/week in the past 6 months (PA-recommendation (≥30 min of moderate-intensity ≥5 days/week)). We included predictors stratified by preoperative adherence: sex, age, BMI, comorbidities, smoking, living/working status, season, mental health, HOOS/KOOS subscales before and 6 months postoperatively, and 6-month adherence.
Results
(1005 THA/972 TKA) Preoperatively, 50% of the population adhered. Adherence increased to 59% at 6 and 12 months. After 12 months, most patients remained at their preoperative PA level, 11% of the preoperative adherers decreased, while 20% of the preoperative non-adherers increased their PA level. In all different groups, adherence to the PA recommendation at 6 months was identified as a predictor (OR-range: 0.16–0.29). In addition, BMI was identified as predictor in the THA adherent (OR = 1.07; 95%CI [1.02–1.15]) and TKA non-adherent groups (OR = 1.08; 95%CI [1.03–1.12]). THA non-adherent group not having paid work (OR = 0.53; 95%CI [0.33–0.85]), and in the TKA adherent group, lower KOOS subscale symptoms (OR = 1.03; 95%CI [1.01–1.05]) were associated with non-adherence.
Conclusions
Majority of patients remained at their preoperative PA level. Non-adherence at 6 months was highly predictive for 12-month non-adherence.
Physical activity (PA) is crucial to decrease mortality risk, especially among patients suffering from osteoarthritis, as these patients have the potential to become more physically active after arthroplasty surgery.
We found that physical function and pain improved, but 69% of the patients remained at their preoperative PA level, while 11% decreased and 20% increased their PA levels.
Using this information shortly after surgery, orthopedic surgeons and other health care professionals can address patients at risk for decreased PA levels and provide PA advice.
Implications for rehabilitation
Keywords:
Introduction
Physical inactivity, or sedentary behavior, increases mortality risk by 20–30% compared to active individuals [Citation1,Citation2]. Additionally, the evidence supporting health benefits of physical activity (PA) is irrefutable [Citation3]. To experience health benefits from PA, various national and international guidelines regarding PA recommend at least 150 minutes of moderate to vigorous PA for adults per week [Citation4–6]. In patients with end-stage OA of the lower extremity, achieving and maintaining a sufficient level of PA is particularly difficult, since they often experience severe joint pain, functional impairment, or fear of aggravating symptoms and increasing joint damage [Citation7,Citation8].
Since both total hip and knee arthroplasty (THA and TKA) surgeries aim to relieve pain and decrease functional impairment, these patients should have the ability to become more physically active after surgery and reach a sufficient PA level to enhance their health [Citation9,Citation10]. However, Vissers et al. [Citation9] showed that even though perceived physical function increased, patients do not adopt a more active lifestyle after THA or TKA. Several studies have demonstrated a difference in self-reported and objectively measured PA after surgery. While self-reported PA levels tend to show higher PA levels after surgery, PA levels remain at or below pre-surgical levels when measured objectively [Citation11–20].
Unraveling the differences between pre- and postoperative PA levels is important, not only in the preoperative consultation and indication for surgery process of these elective surgeries, but also to identify patients eligible for interventions aimed at improving PA after surgery.
Previous studies identified risk factors for lower PA levels after THA/TKA: female gender, older age, higher body mass index (BMI), smoking, lower educational level, unemployment, number of comorbidities, OA pain in multiple sites, lower quality of life, sedentary behavior, and preoperative inadequate PA [Citation4,Citation5,Citation11–13,Citation21]. However, most studies only included risk factors either prior to or after surgery, while noting the change in the PA score is essential.
Thus, the primary aim of this study was to assess the prevalence of adherence to the Dutch PA recommendation, preoperatively and 6 and 12 months following primary THA or TKA. Secondly, we explored which patient characteristics (measured prior to surgery and/or at 6 months postoperatively) were associated with non-adherence to the PA recommendation at 12 months. As preoperative PA level is a strong predictor for postoperative PA levels, we stratified our population based on preoperative adherence level. This latter may enable the identification of patients at risk of non-adherence to the PA recommendation after THA or TKA.
Materials and methods
Study design
This study included a subset of patients scheduled for THA or TKA, as a result of OA (October 2013–December 2018), from the ongoing Longitudinal Leiden Orthopaedics Outcomes of Osteo-Arthritis Study (LOAS) (trial ID NTR3348) [Citation22] (level of evidence II). Ethical approval was obtained from the regional Medical Research Ethics Committee (METC) (protocol number: P12.047). Patients treated with primary THA or TKA at one of the seven participating hospitals in the Netherlands were aimed to be included. After obtaining informed consent, patients received a paper or digital LOAS-questionnaire before surgery and at 6 and 12 months after surgery, containing a questionnaire regarding self-reported PA.
Patient selection
Patients were eligible if scheduled for a primary THA or TKA as a result of OA, were 18 years or older, and physically and mentally able to complete questionnaires in Dutch. Patients were excluded if the PA level was missing at any of the time points after surgery.
Assessments
Patients’ baseline characteristics
The following patient characteristics were collected preoperatively: sex, age (years), BMI, current smoking status (yes/no), living arrangements (alone/with others), and work status (paid work; yes/no).
The Dutch recommendation for health enhancing physical activity
The Dutch recommendation for health-enhancing PA (PA recommendation) was used to evaluate patients’ perceived PA. In September 2017, the Dutch Health Council launched new physical activity guidelines [Citation23,Citation24]. According to the new guidelines for adults, a minimum of 150 minutes of moderate-intensity PA/week, divided over several days, is considered health enhancing. Besides, muscle and bone strengthening activities are recommended at least twice a week, and for the elderly, combined with balance exercises. The LOAS-questionnaire included the Dutch PA recommendation based on the guidelines before 2017, which states that at least 30 minutes of moderate-intensity PA/day, for a minimum of 5 days/week, is considered health-enhancing for adults, based on international guidelines [Citation25]. PA of moderate intensity is defined as all kinds of PA with the same intensity as brisk walking or cycling. Prior to surgery and at 6 and 12 months postoperatively, patients answered how often they engaged in PA of such kind (days/week), for at least 30 min per day, in the past 6 months. Patients classified as “adherent” if they reportedly engaged on 5 or more days/week. As a result, patients who were active for more than 150 min/week, but not on 5 or more days/week, were classified as “non-adherent”.
Other assessments
Additionally, patient reported outcome measures (PROMs) were collected using several validated Dutch questionnaires. To gain insight into changes in disease state of patients, the questionnaires were collected prior to surgery and 6 and 12 months postoperatively. Validated Dutch versions of the Hip disability and Knee Injury and Osteoarthritis Outcome Score (HOOS/KOOS) were used to assess hip/knee associated problems (pain, function in daily living (ADL), symptoms, sports and recreation function and quality of life) [Citation26–28], ranging from 0 to 100 (0 representing the worst outcome and 100 representing the best outcome). Patient’s general health and health-related quality of life were evaluated using the Short Form Health Survey (SF-12) [Citation29], calculating summary scores for the physical component summary (PCS) and mental component summary (MCS), with a range from 0 to 100 (higher score indicating better health). To determine the presence of comorbidities before surgery, a comorbidity questionnaire from the Dutch Central Bureau of Statistics (CBS) [Citation30] was used, analyzing whether comorbidities were present in the previous year, categorized into either musculoskeletal or non-musculoskeletal comorbidities.
Statistical analysis
All analyses were stratified by joint (hip/knee) and preoperative adherence level. To determine nonresponse bias, we performed unpaired t-tests (continuous, normally distributed data) and Chi-squared tests (categorical data) to compare patient characteristics between the included and excluded patients. We visualized adherence trajectories over time. Subsequently, we calculated proportions of patients with increased, decreased, or equal PA levels 12 months postoperatively.
To be able to identify patient-related predictors for PA adherence (yes/no) 12 months postoperatively, we performed multiple multivariable logistic regression analyses with backward elimination (level of significance for removing variables in the backward elimination was set at p < 0.20): a model including variables collected both before and 6 months postoperatively, stratified by joint and preoperative adherence. Decisions on the variables to be examined were based on previous studies and our own knowledge about PA after arthroplasty [Citation12,Citation21]. Included variables were: sex, age, BMI, comorbidities, smoking, living and working status, seasons, MCS and HOOS/KOOS scores (both before and 6 months after surgery), and 6-month adherence. Missing values in covariates (assumed to be missing at random (MAR)) were imputed using the multivariate imputation by chained equations (MICE) algorithm in R, while including all other variables available in the model [Citation31]. Imputed data were visually inspected to determine if the data seemed reasonable, and were then pooled to obtain within- and between-imputation variance. The effect estimates were depicted as odds ratios (ORs) with corresponding 95% confidence intervals (lower limit, upper limit). All analyses were performed using R (Version R 3.6.1) (R Foundation for Statistical Computing, Vienna, Austria).
Results
Included patients
One thousand five hundred and ninety-six THA and 1588 TKA patients answered the question regarding PA levels prior to surgery. In total, 1005 (63%) THA and 972 (61%) TKA patients had preoperative and 6 and 12 month postoperative data (). Compared to THA patients without postoperative PA information, the included THA patients were younger, more often female (60% in the group without PA information vs. 65% among included patients), had lower BMI scores, more often had non-musculoskeletal comorbidities (21% in the group without PA information vs. 31% among included patients), were less often smokers (9% in the group without PA information vs. 4% among included patients), and had lower preoperative HOOS and SF-12 scores (Supplementary Table 1).
Figure 1. Flowchart patient selection. Included patients with data at all assessments. THA: total hip arthroplasty; TKA: total knee arthroplasty; OA: osteoarthritis; PA level: physical activity level; FU: follow-up.
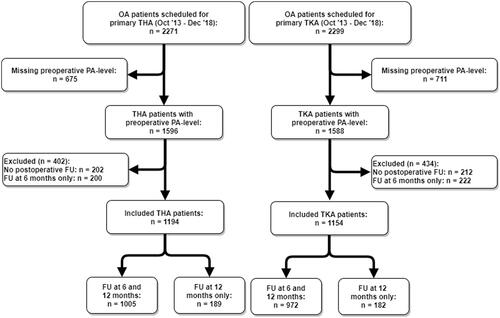
Similar to the THA population, when comparing the TKA patients without postoperative PA information to the included TKA patients, the included TKA patietns were younger and less often smoker (8% in the group without PA information vs. 5% among included patients). Additionally, they more often had no or only musculoskeletal comorbidities, respectively, no musculoskeletal comorbidities: 9% in the group without PA information vs. 13% among included patients, and only musculoskeletal comorbidities: 8% in the group without PA information vs. 10% among included patients. Lastly, they had better KOOS Sports and Recreation Function, MCS and PCS scores. Additionally, the included TKA patients more often had a paid job (19% in the group without PA information vs. 27% among included patients) (Supplementary Table 1).
Preoperative physical activity
Preoperatively, 497 (49%) THA and 465 (48%) TKA patients adhered to the PA recommendation. Adhering THA patients performed 30 minutes of moderate-intensity PA on 6 (SD: 0.9) days/week, compared to 2 (SD: 1.5) days/week in the non-adhering THA patients. Comparison of the adherent and non-adherent THA populations showed lower BMI scores, better HOOS subscales pain, ADL, sport and recreation function, and quality of life scores, MCS and PCS scores, and higher employment percentage (adherent: 27% vs. non-adherent: 22%). Moreover, in the adherent group, the proportion of women was lower (adherent: 57% vs. non-adherent: 64%) ().
Table 1. Preoperative characteristics of patients based on preoperative adherence to the Dutch PA recommendationTable Footnotea.
Overall, we found similar results in the TKA population, with on average lower BMI and better scores on all KOOS subscales and PCS in the adherent population. Additionally, the adherent TKA population consisted of less females (adherent: 59% vs. non-adherent: 66%), compared to the non-adherent group.
When comparing PA in men and women within the adherent THA group, no differences were found (men: 6 (SD: 0.9) days/week; women: 6 (SD: 0.9) days/week), nor within the non-adherent group found (men: 2 (SD: 1.5) days/week; women: 2 (SD: 1.5) days/week).
Outcomes after surgery
PA trajectories
With respect to PA levels prior to surgery, 6 months, and 12 months postoperatively, we identified eight different trajectories over time ( and ). Overall, PA adherence in both the THA and TKA populations increased to 59% 12 months after surgery. Within the THA population, the group adhering to the PA recommendation at 12 months consisted of 65% preoperative adherers and 35% preoperative non-adherers. Furthermore, 11% of patients decreased their PA level, while 22% increased their PA level at 12 months. Almost similar to the THA population, the adherent TKA group at 12 months consisted of 64% preoperative adherers and 36% preoperative non-adherers. Similar changes in adherent levels were found in the TKA population: 11% decreased, while 20% increased their PA level. In total, 69% of THA and TKA patients remained at their preoperative adherence-level.
Figure 2. Possible postoperative (at 6 and 12 months) physical activity trajectories of total hip arthroplasty patients that either adhered or not-adhered to the physical activity guideline prior to surgery, resulting in eight possible trajectories for adherence at 12 months. aa: All percentages are with respect to preoperatively meeting the PA recommendation. Complete cases: patients with data at both 6 and 12 months postoperative.
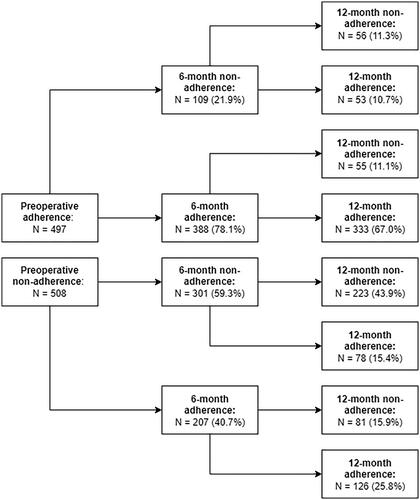
Figure 3. Possible postoperative (at 6 and 12 months) physical activity trajectories of total knee arthroplasty patients that either adhered or not-adhered to the physical activity guideline prior to surgery, resulting in eight possible trajectories for adherence at 12 months. aa: All percentages are with respect to preoperatively meeting the PA recommendation. Complete cases: patients with data at both 6 and 12 months postoperative.
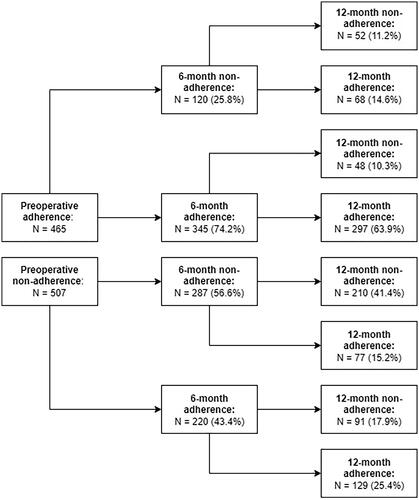
Approximately, 70% of the THA and TKA patients reached their final PA level at 6 months. Additionally, the PA level had changed in 12% of THA and 13% of TKA patients at 12 months, while being consistent at preoperative and 6 months. Furthermore, 13% of THA and 7% of TKA patients switched at 6 months, to return to their preoperative level at 12 months.
Pain and functional outcomes
We did not find significant nor clinical differences in the preoperative adherent and non-adherent THA population when comparing changes in pain (preoperative – 6 month FU; non-adherent: 49 (SD: 22.0), adherent: 47 (SD: 22.5)) and changes in ADL (preoperative – 6 month FU; non-adherent: 43 (SD: 21.6), adherent: 41 (SD: 21.9)). We found similar results in the TKA population: changes in pain (preoperative – 6 month FU; non-adherent: 42 (SD: 23.3)), adherent: 41 (SD: 23.2) and changes in ADL (preoperative – 6 month FU; non-adherent: 36 (SD: 21.5), adherent: 33 (SD: 20.8)).
Identified predictors for adherence to Dutch PA recommendation
In , we depicted the predictors, stratified for THA and TKA, for PA adherence 12 months postoperatively. In all different groups, adherence to the PA recommendation at 6 months was identified as a predictor. In addition, BMI was also identified as predictor in the THA adherent group (OR = 1.07; 95%CI [1.02–1.15]) and TKA non-adherent group (OR = 1.08; 95%CI [1.03–1.12]). In the THA non-adherent group, we also identified not having paid work (OR = 0.53; 95%CI [0.33–0.85]), and in the TKA adherent group, lower KOOS subscale symptoms (OR = 1.03; 95%CI [1.01–1.05]) to be significantly associated with non-adherence.
Table 2. Associated predictors (preoperative and 6 months after surgery) for adherence 12 months after surgery.
Discussion
We assessed the prevalence of adherence to the Dutch PA recommendation, preoperatively and 6 and 12 months postoperatively, for primary THA or TKA. Secondly, we identified patient-related predictors both before and 6 months after surgery for non-adherence to the Dutch PA recommendation 12 months postoperatively. Although 40% of the preoperative non-adherers became adherers 12 months after surgery, PA adherence decreased in 22% of THA and TKA patients adherent before surgery. The majority of the patients remained at their preoperative PA level. Several patient characteristics were associated with PA adherence 12 months after THA and TKA, but 6-month non-adherence was the most common predictor among all groups and highly predictive for non-adherence at 12 months.
Preoperatively, about 50% of THA and TKA patients adhered to the Dutch PA recommendation, which is comparable, and even slightly higher than the general Dutch population (45% adherence) [Citation32]. Twelve months after surgery, 59% of the THA and TKA populations adhered in our study, which is comparable with, and also slightly higher than two other Dutch studies reporting 51% adherence after THA [Citation33] and 55% adherence after TKA [Citation34]. However, in those studies, adherence to the PA recommendation was measured with the Short QUestionnaire to ASsess Health-enhancing physical activity (SQUASH), which has 11 items and includes questions on multiple activities people perform during a normal week in recent months, compared to the use of a one-item questionnaire in our study. Even though the majority of patients adhered to the Dutch PA recommendation, with even greater numbers than the general Dutch population, there is still a large proportion of patients that remained below the adherence-level or even decreased their PA level. As said before, performing PA at a sufficient level is important to improve overall health status [Citation35].
To the best of our knowledge, this is the first study reporting the proportion of patients with increased, decreased or equal PA levels 12 months after THA/TKA in a larger cohort setting. A small study reported improved PA at 6 months after THA/TKA surgery in 72% of patients, while PA decreased in 10% of patients [Citation11]. In comparison, our results were somewhat less positive at 12 months as the majority of patients that were non-adherent prior to surgery remained at their level (60%), and 11% of patients no longer adhered 12 months postoperative, while they adhered before surgery. Nevertheless, 22% of non-adherent patients increased their PA level. Therefore, THA or TKA could offer preoperative non-adherent patients an opportunity to increase their PA level [Citation36]. Additionally, it is known that PA after THA or TKA has health enhancing benefits on bone quality, better muscle strength and coordination [Citation3,Citation37,Citation38].
With regard to predictors for postoperative PA, Hodges et al. [Citation12] found that inadequate PA before TKA was strongly predictive of inadequate PA 12 months postoperatively. Furthermore, previous studies identified older age, female gender, higher BMI, lower educational level, number of comorbidities, and lower quality of life after surgery to be associated with physical inactivity after surgery [Citation12,Citation21]. After stratification based on preoperative PA adherence, we identified that whether or not patients adhered to the PA recommendation at 6 months to be the only consistent predictor in all groups, with large ORs. None of the models showed a significant effect of pain or function, preoperatively or 6 months after surgery. Thus, improved pain and function does not always result in a more active lifestyle, indicating that possibly a behavioral change is needed to gain a more active lifestyle after surgery.
On average, 40% of all patients did not adhere to the PA recommendation 12 months after surgery. Webber et al. [Citation39] showed that patients are often unaware of the health risks associated with high levels of sedentary behavior, and lack concern and familiarity with increasing PA in order to meet the recommended guidelines. Although PA adherence after surgery is somewhat higher compared to the general population, clinicians could pay more attention to patient education as PA health benefits are substantial in this population. Furthermore, given the pervasive nature of sedentary behavior, there could also be a potential role for behavior change interventions to increase PA after THA/TKA [Citation21]. With our trajectories of patient flow, and identified characteristics of patients at risk of decreased PA level after THA or TKA, orthopedic surgeons and physical therapist may be able to anticipate the behavior of their patients and intervene prior to and 6 months after surgery, to increase PA in these patients.
Strengths and limitations
This study has several strengths. First, it is a large, multicenter cohort study, assessing PA prior to surgery and 6 and 12 months after surgery. By including preoperative PA, we could assess predictors for non-adherence for preoperative adherers and non-adherers. Limitations of the present study include the risk of bias: the PA level was assessed using a one-item question on PA behavior during the last 6 months. First, this is reasonably a long period, which could have resulted in recall bias. As a result, PA could have been influenced by seasons during this period. Nevertheless, season did not remain in the model after backward elimination, thereby indicating that it did not significantly affect the results in this study. Furthermore, the use of self-reported PA has been shown to differ from objectively measured PA, as patient tend to overestimate their PA levels [Citation11–20]. However, the use of objective measures (e.g., accelerometers) for PA levels in such a large population and both prior to and after surgery was not deemed feasible for the current study. Regarding subjective measurement instruments on PA, the literature reports that the validity of single-item questionnaires shows notable similarities to device-based measures and multiple-item measures for PA [Citation40,Citation41]. In that sense, the assessment method used can be considered a strength. Moreover, previous studies show that single-item questions are valuable measurements in older adults and adolescents, as well as in settings where resources and time are limited [Citation41]. Additionally, patients might have several reasons to refuse answering the PA recommendation question, resulting in the introduction of self-selection. To evaluate this risk of bias, we compared characteristics of the included patients and excluded population, but we expect that no self-selection was introduced, as differences were not clinically relevant. Furthermore, we did not include all previously identified predictors for postoperative PA level, such as educational level (this information was not recorded) and physical therapy (PT). The latter was excluded as 95% of our population used postoperative PT [Citation42]. Lastly, due to the cutoff point (adherence = PA ≥ 5 days/week), misclassification may have occurred, as a patient’s PA level fluctuates over time around 5 days/week, they could be included in the adherent group prior to surgery, while being included in the non-adherent group after surgery, indicating a decreased PA level. Within the new guideline of the Dutch recommendation for health enhancing PA, the cut-off point of five days has been amended to “a minimum of 150 min of moderate-intensity PA/week, divided over several days” thereby some participants in our study may adhere to the new recommendation but are classified as non-adheres in our current study. As such the numbers reported could be an underestimation of the new Dutch recommendation for health enhancing PA.
We presented trajectories of patient flow and identified predictors associated with adherence 12 months postoperatively. Non-adherence to the PA recommendation at 6 months was found to be highly predictive for non-adherence at 12 months.
Ethical approval
The Medical Ethics Committee of the LUMC approved the study P12.047 “Longitudinal Leiden Orthopaedics Outcomes of Osteoarthritis Study (LOAS)”. The nature of the study, the interests of involved subjects and article 3 of the Law Medical-Scientific Research with Human Subjects were taken into consideration and resulted in a positive judgement of the execution of the study.
Supplemental Table
Download PDF (69.2 KB)Acknowledgements
We would like to acknowledge the members of the LOAS study group in addition to the authors: W.J. Marijnissen, Albert Schweitzer Hospital, Dordrecht; PJ Damen, Waterland Hospital, Purmerend; HMJ van der Linden and BL Kaptein, Leiden University Medical Center, Leiden; SHM Verdegaal, Alrijne Hospital, Leiderdorp; HH Kaptijn, LangeLand Hospital, Zoetermeer; SBW Vehmeijer, Reinier de Graaf Hospital, Delft; R Onstenk, Groene Hart Hospital, Gouda: the Netherlands for the provision of patients and general support.
Disclosure statement
The authors report no conflicts of interest.
Data availability statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Additional information
Funding
References
- World Health Organization. Physical activity; 2018 . Available from: https://www.who.int/news-room/fact-sheets/detail/physical-activity
- Lavie CJ, Ozemek C, Carbone S, et al. Sedentary behavior, exercise, and cardiovascular health. Circ Res. 2019;124(5):799–815. doi: 10.1161/CIRCRESAHA.118.312669.
- Warburton DER, Bredin SSD. Health benefits of physical activity: a systematic review of current systematic reviews. Curr Opin Cardiol. 2017;32(5):541–556. doi: 10.1097/HCO.0000000000000437.
- Chang AH, Song J, Lee J, et al. Proportion and associated factors of meeting the 2018 physical activity guidelines for Americans in adults with or at risk for knee osteoarthritis. Osteoarthritis Cartilage. 2020;28(6):774–781. doi: 10.1016/j.joca.2020.03.007.
- Ernstgard A, PirouziFard M, Thorstensson CA. Health enhancing physical activity in patients with hip or knee osteoarthritis – an observational intervention study. BMC Musculoskelet Disord. 2017;18(1):42. doi: 10.1186/s12891-017-1394-7.
- Herbolsheimer F, Schaap LA, Edwards MH, et al. Physical activity patterns among older adults with and without knee osteoarthritis in six European countries. Arthritis Care Res. 2016;68(2):228–236. doi: 10.1002/acr.22669.
- Nuesch E, Dieppe P, Reichenbach S, et al. All cause and disease specific mortality in patients with knee or hip osteoarthritis: population based cohort study. BMJ. 2011;342:d1165. doi: 10.1136/bmj.d1165.
- Fransen M, McConnell S. Land-based exercise for osteoarthritis of the knee: a metaanalysis of randomized controlled trials. J Rheumatol. 2009;36(6):1109–1117. doi: 10.3899/jrheum.090058.
- Vissers MM, Bussmann JB, de Groot IB, et al. Physical functioning four years after total hip and knee arthroplasty. Gait Posture. 2013;38(2):310–315. doi: 10.1016/j.gaitpost.2012.12.007.
- Jüni P, Reichenbach S, Dieppe P. Osteoarthritis: rational approach to treating the individual. Best Pract Res Clin Rheumatol. 2006;20(4):721–740. doi: 10.1016/j.berh.2006.05.002.
- Harding P, Holland AE, Delany C, et al. Do activity levels increase after total hip and knee arthroplasty? Clin Orthop Relat Res. 2014;472(5):1502–1511. doi: 10.1007/s11999-013-3427-3.
- Hodges A, Harmer AR, Dennis S, et al. Prevalence and determinants of physical activity and sedentary behaviour before and up to 12 months after total knee replacement: a longitudinal cohort study. Clin Rehabil. 2018;32(9):1271–1283. doi: 10.1177/0269215518769986.
- Issa K, Jauregui JJ, Given K, et al. A prospective, longitudinal study of patient activity levels following total knee arthroplasty stratified by demographic and comorbid factors. J Knee Surg. 2015;28(4):343–347. doi: 10.1055/s-0034-1388658.
- Pelle T, Claassen AAOM, Meessen JMTA, et al. Patients who underwent total hip or knee arthroplasty are more physically active than the general Dutch population. Rheumatol Int. 2017;40(3):383–392. doi: 10.1007/s00296-016-3598-9.
- Hammett T, Simonian A, Austin M, et al. Changes in physical activity after total hip or knee arthroplasty: a systematic review and meta-analysis of six- and twelve-month outcomes. Arthritis Care Res. 2018;70(6):892–901. doi: 10.1002/acr.23415.
- Arnold JB, Walters JL, Ferrar KE. Does physical activity increase after total hip or knee arthroplasty for osteoarthritis? A systematic review. J Orthop Sports Phys Ther. 2016;46(6):431–442. doi: 10.2519/jospt.2016.6449.
- Paxton RJ, Melanson EL, Stevens-Lapsley JE, et al. Physical activity after total knee arthroplasty: a critical review. World J Orthop. 2015;6(8):614–622. doi: 10.5312/wjo.v6.i8.614.
- Mills K, Falchi B, Duckett C, et al. Minimal change in physical activity after lower limb joint arthroplasty, but the outcome measure may be contributing to the problem: a systematic review and meta-analysis. Physiotherapy. 2019;105(1):35–45. doi: 10.1016/j.physio.2018.04.003.
- Kahn TL, Schwarzkopf R. Does total knee arthroplasty affect physical activity levels? Data from the osteoarthritis initiative. J Arthroplasty. 2015;30(9):1521–1525. doi: 10.1016/j.arth.2015.03.016.
- Jeldi AJ, Deakin AH, Allen DJ, et al. Total hip arthroplasty improves pain and function but not physical activity. J Arthroplasty. 2017;32(7):2191–2198. doi: 10.1016/j.arth.2017.02.002.
- Naylor JM, Pocovi N, Descallar J, et al. Participation in regular physical activity after total knee or hip arthroplasty for osteoarthritis: prevalence, associated factors, and type. Arthritis Care Res. 2019;71(2):207–217. doi: 10.1002/acr.23604.
- Tilbury C, Leichtenberg C, Kaptein B, et al. Feasibility of collecting multiple patient-reported outcome measures alongside the Dutch Arthroplasty Register. J Patient Exp. 2020;7(4):484–492. doi: 10.1177/2374373519853166.
- Klein K. De beweegrichtlijnen per september 2017: Kenniscentrum Sport & Bewegen; 2020 [updated 2020 Feb 19]. Available from: https://www.allesoversport.nl/artikel/hoeveel-moet-je-bewegen-volgens-de-beweegrichtlijnen/
- Bernaards C. Nederlandse organisatie voor toegepast-wetenschappelijk onderzoek (TNO). Bewegen in Nederland 2000–2013. Leiden; 2014. Available from: Bewegen in Nederland 2000-2013 (tno.nl)
- Gezondheidsraad. Beweegrichtlijnen; 2017. Available from: https://www.gezondheidsraad.nl/documenten/adviezen/2017/08/22/beweegrichtlijnen-2017
- Roos EM, Toksvig-Larsen S. The Knee Injury and Osteoarthritis Outcome Score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes. 2003;1:17. doi: 10.1186/1477-7525-1-64.
- de Groot IB, Favejee MM, Reijman M, et al. The Dutch version of the Knee Injury and Osteoarthritis Outcome Score: a validation study. Health Qual Life Outcomes. 2008;6:16. doi: 10.1186/1477-7525-6-16.
- Nilsdotter AK, Lohmander LS, Klassbo M, et al. Hip Disability and Osteoarthritis Outcome Score (HOOS) – validity and responsiveness in total hip replacement. BMC Musculoskelet Disord. 2003;4:10. doi: 10.1186/1471-2474-4-10.
- Gandhi SK, Salmon JW, Zhao SZ, et al. Psychometric evaluation of the 12-Item Short-Form Health Survey (SF-12) in osteoarthritis and rheumatoid arthritis clinical trials. Clin Ther. 2001;23(7):1080–1098. doi: 10.1016/s0149-2918(01)80093-x.
- Statistiek CBvd. Gezondheid, leefstijl, zorggebruik; 2000–2009; 2016. Available from: https://opendata.cbs.nl/statline/"/l"/CBS/nl/dataset/03799/table?fromstatweb"
- Buuren S, Groothuis-Oudshoorn K. Mice: multivariate imputation by chained equations in R. J Stat Soft. 2011;45(3):1–68. doi: 10.18637/jss.v045.i03.
- RIVM. Gestandaardiseerde trend voldoen aan beweegrichtlijnen: Volksgezondheidenzorg.info; 2019 [updated 2019 Apr 18; cited 2020 Apr 17]. Available from: https://www.volksgezondheidenzorg.info/onderwerp/bewegen/cijfers-context/trends
- Wagenmakers R, Stevens M, Zijlstra W, et al. Habitual physical activity behavior of patients after primary total hip arthroplasty. Phys Ther. 2008;88(9):1039–1048. doi: 10.2522/ptj.20070375.
- Kersten RF, Stevens M, van Raay JJ, et al. Habitual physical activity after total knee replacement. Phys Ther. 2012;92(9):1109–1116. doi: 10.2522/ptj.20110273.
- Kokkinos P. Physical activity, health benefits, and mortality risk. ISRN Cardiol. 2012;2012:718789. doi: 10.5402/2012/718789.
- Ponzio DY, Rothermel SD, Chiu YF, et al. Does physical activity level influence total hip arthroplasty expectations, satisfaction, and outcomes? J Arthroplasty. 2021;36(8):2850–2857. doi: 10.1016/j.arth.2021.03.052.
- Warburton DE, Gledhill N, Quinney A. Musculoskeletal fitness and health. Can J Appl Physiol. 2001;26(2):217–237. doi: 10.1139/h01-013.
- Kuster MS. Exercise recommendations after total joint replacement: a review of the current literature and proposal of scientifically based guidelines. Sports Med. 2002;32(7):433–445. doi: 10.2165/00007256-200232070-00003.
- Webber SC, Ripat JD, Pachu NS, et al. Exploring physical activity and sedentary behaviour: perspectives of individuals with osteoarthritis and knee arthroplasty. Disabil Rehabil. 2020;42(14):1971–1978. doi: 10.1080/09638288.2018.1543463.
- Bauman AE, Richards JA. Understanding of the single-item physical activity question for population surveillance. J Phys Act Health. 2022;19(10):681–686. doi: 10.1123/jpah.2022-0369.
- O’Halloran P, Kingsley M, Nicholson M, et al. Responsiveness of the single item measure to detect change in physical activity. PLOS One. 2020;15(6):e0234420. doi: 10.1371/journal.pone.0234420.
- Groot L, Latijnhouwers D, Reijman M, et al. Recovery and the use of postoperative physical therapy after total hip or knee replacement. BMC Musculoskelet Disord. 2022;23(1):666. doi: 10.1186/s12891-022-05429-z.
