Abstract
Purpose
Persons with post-COVID condition are a growing population requiring support returning to everyday life. Energy management education (EME) is a group self-management intervention based on energy conservation and management strategies delivered by occupational therapists. Data on the effectiveness of EME in persons with long COVID-related fatigue still need to be provided. This study aims to investigate procedural and methodological parameters to plan a future study analyzing the effectiveness of EME in individuals with post-COVID-19 conditions.
Materials and Methods
A pre-post design was used. The procedural data was collected regarding eligibility, reasons for participation decline, dropout, and follow-up rates. Changes in self-efficacy in using energy management strategies, fatigue impact, competency in daily activities, and quality of life were collected three times. Implemented behavior strategies at five months from EME were documented.
Results
During five months, 17 of 30 eligible participants were included in the study. No dropouts were registered during the intervention period. The follow-up response rate was 70%. The effect size was large in three out of four outcomes post-intervention, with a tendency to increase at follow-up.
Conclusions
This study demonstrated the feasibility of study procedures and reported promising effect sizes for EME that should be further researched.
IMPLICATIONS FOR REHABILITATION
Persons with post-COVID condition are a growing population requiring support returning to everyday life.
Energy management education (EME) is a group self-management intervention feasible in persons with long COVID-related fatigue.
The data showed a large effect size in fatigue impact, self-efficacy in performing energy management strategies, and competency in daily activities.
Introduction
Post-coronavirus disease 2019 (COVID-19) condition, also known as long COVID, occurs in individuals with a history of probable or confirmed SARS-CoV-2 infection, usually three months from the onset of COVID-19 [Citation1]. Symptoms last for at least two months and cannot be explained by an alternative diagnosis [Citation1].
Current long COVID prevalence estimates range from 7.5% to 41% in non-hospitalized adults, 2.3–53% in mixed adult samples, and 37.6% in hospitalized adults [Citation2]. Long COVID is a remitting and relapsing condition with a prolonged course preventing the return to previous life routines, work, and performance levels, causing significant distress and disability to the individual [Citation3]. Fatigue is a multidimensional symptom with a high prevalence in long COVID; experienced mostly as severe, it impacts cognition, extended activities of daily living, and social activities [Citation4].
The primary goal of occupational therapy (OT) in persons with fatigue is to enable participation in daily activities through behavior changes and to support occupational performance in all significant life areas in favor of self-determination, well-being, and health [Citation5]. OTs teach the use of energy conservation strategies. In the last decade, there has been a trend towards using the term “energy management” instead of “energy conservation” because “energy management” is considered a more comprehensive, positive, and empowering term. OTs apply self-management education to target energy management in daily routines and habits. This complex intervention positively affects different outcome dimensions, e.g., fatigue impact, self-efficacy, or quality of life in persons with chronic disease-related fatigue like multiple sclerosis [Citation6] or cancer survivors [Citation7].
OTs in Switzerland have used the energy management approach since the beginning of the pandemic, first with post-acute COVID-19, and then with post-COVID conditions. They base their intervention mainly on the Energy Management Education (EME) [Citation8] treatment protocol and its materials available in the local languages. EME is a structured, evidence-based [Citation9,Citation10] intervention protocol developed and evaluated between 2016 and 2018 for persons with multiple sclerosis-related fatigue and subsequently adapted for persons with chronic disease-related fatigue (Version 2.0). In persons with MS, EME showed promising effects on self-efficacy in performing energy management strategies and quality of life [Citation11,Citation12]. According to the experiences of nine OTs who implemented EME 2.0 in different healthcare institutions in Switzerland, the protocol was deemed feasible and appropriate. However, there is a need for optimization to address the specific needs of individuals with long COVID-related fatigue [Citation13]. The OTs reported that participants with long COVID who underwent EME showed an increased understanding of factors that influence fatigue. Furthermore, some participants shared positive changes in their ability to manage daily responsibilities and routines, leading to an increase in their self-confidence [Citation13].
International guidelines recommend OT for individuals with long COVID-related fatigue [Citation14,Citation15]. However, there is a lack of data on the effectiveness, efficiency, and cost-effectiveness of complex interventions like EME. Additionally, the outcomes of rehabilitation programs that are specifically designed for this emerging population need to be evaluated. Clinical trials should investigate whether self-management education improves energy management abilities and induces behavior changes, leading to a reduced impact of fatigue on daily life for former EME participants compared to those with long COVID who did not participate in manualized OT-based self-management education at the same stage of the condition.
The primary aim of this study was to assess the feasibility of a study protocol for a future trial by gathering data on (1) the number of eligible persons during a specific timeframe, the recruitment, and the successful inclusion of participants; (2) the time needed for data collection administration, as well as the follow-up and response rates. The secondary aims were to explore the changes in relevant outcome dimensions, estimate the intervention’s effect size, and increase our knowledge about the implemented energy management strategies two months after the intervention.
Materials and methods
This feasibility study had a pre-post design with four data collection time points (baseline, BL, week 0; post-intervention, T1, week 7; follow-up, T2, week 15, online survey, T3, week 24). Since March 2021, the Rehabilitation Center, REHAB, in Basel, Switzerland, has provided an inter-professional consultation and a day-hospital treatment program for persons with long COVID. Persons, after having had COVID-19, can register for consultation as early as four weeks after infection. Based on the symptom cluster and the rehabilitation goals, the inter-professional team creates a 6–9-week treatment plan tailored to the individual patient. EME version 2.0 is the OT standard intervention of the rehabilitation program. Other rehabilitation interventions are physiotherapy and consultations by different health professionals (e.g., cardiologists, pulmonologists, psychologists, and social workers). On average, six persons with long COVID start with EME every month. Five OTs at REHAB Basel are trained in conducting EME and have experience treating patients with fatigue in other underlying conditions. None of them had participated in the focus group discussion about the feasibility of EME in persons with long COVID held by the authors in the summer of 2021 [Citation13].
Ethical approval was obtained (9 November 2021) from the local research ethics committee (Ethikkommission Nordwest- und Zentralschweiz, Project ID: 2021–02055) and the study was conducted in accordance to the principles of the Declaration of Helsinki.
Participants
The aim was to include a sample of 15–18 participants who had completed at least five of seven EME sessions. This sample size allowed for the feasibility assessment without causing unnecessary inconvenience to patients or utilizing excessive time resources of professionals.
We included participants who signed informed consent, were aged ≥18 years, screened and diagnosed with post-COVID-19 syndrome [Citation14] at the consultation for persons with long COVID at REHAB Basel, and who were eligible for the EME group. This included those with the ability to understand and speak German, confirmed experience of living with fatigue (Fatigue Severity Scale [FSS], cut off >4) [Citation16], no major depression (Beck depression inventory [BDI]-FS cut-off <8) [Citation17], no major cognitive impairments (Montreal cognitive assessment [MoCA] cut-off ≥ 26) [Citation18], and those motivated to participate in EME after being provided with the information by the OT (duration, frequency, and aim).
We excluded those who were not eligible for the EME group, with any insufficient comprehension of spoken German for the research project information and self-filled questionnaires. The EME participants were informed of their eligibility at the end of lesson one by the OT, who provided an information leaflet and the assessment booklet. Those who signed the informed consent and filled in the assessment booklet before lesson two were included.
Intervention
EME teaches participants to manage their available energy and to achieve a satisfying and meaningful daily routine despite fatigue. Participants understand the factors influencing their energy levels and the skills to manage their energy using behavioral strategies (e.g., pacing, planning, prioritizing activities, optimizing the environment, and adopting ergonomic behaviors). Subsequently, they identify and implement tailored behavior modifications and adapt their habits and routines accordingly. According to Wang, predictors of engagement in energy self-management behaviors include self-efficacy, outcome expectations, and knowledge about factors that influence symptoms [Citation19].
EME was delivered once a week by a trained OT. The intervention started with an individual session lasting 45 - 60 min, followed by five group sessions with a maximum of five participants (each session lasting 90 min). After the group sessions, there was another individual session lasting 45 min. The intervention concluded with a booster mail sent eight weeks after the seventh session (refer to ).
Table 1. Description of energy management education (EME).
The EME manual provides detailed content and suggestions on how to lead the intervention. The EME workbook for participants provides information and working tools used during and between the lessons.
Data collection
Data was collected on patient eligibility and enrollment and completion of study procedures. To document screening of the inclusion and exclusion criteria, willingness to participate, or reasons for refusal, a case report form was completed for each eligible individual. It further documented the number of sessions that each patient had completed and the handing over, return, and needed recalls of the assessment booklets at BL, T1, and T2. In addition, the case report form allowed to register suggestions about the feasibility of the procedures, e.g., duration or support needed while filling out the assessment booklet. The sent calls recalls, and responses to the online survey at T3 were registered by the software program [Citation20].
Four self-reported questionnaires were used to documented different outcomes of interest at BL (week 0), post-intervention (week 7), and follow-up (week 15).
The perceived self-efficacy in performing energy management strategies is an intermediate outcome of EME. It informs about the change in confidence in performing the learned strategies. The Self-Efficacy for Performing Energy Conservation Strategies Assessment (SEPECSA) [Citation21] is a self-reported questionnaire that reports the mean scores of the perceived confidence in performing 14 different energy management strategies (1 = low confidence, 10 = high confidence). It is a valid and reliable instrument and has a minimal clinically important difference of 0.92 [Citation22].
The modified fatigue impact scale (MFIS) [Citation23] is a valid and reliable instrument that measures the impact of physical and mental fatigue on daily routines. It contains 21 items, which score from 0 (never) to 4 (almost always), thus ranging from 0 to 84. The minimal clinically important difference reported is 13.8 [Citation24]. Factors that influence the impact of fatigue on daily life are, e.g., fatigue intensity, knowledge, and ability to modify fatigue influence factors, and engagement in energy-managing behaviors.
The Occupational Self-Assessment (OSA) [Citation25] focuses on the perceived competency to perform 21 daily tasks, which scores from 1 (I have a lot of problems) to 4 (I do extremely well). The raw data are converted to interval levels (0–100). For persons living with long COVID-related fatigue, retaking control over daily tasks is a relevant person-centered outcome.
The Medical Outcome Study 36-item Short Form Health Survey [Citation26] was used to document health-related quality of life. The eight subscales were transformed into a Physical Component Scale (PCS) and a Mental Component Scale (MCS), according to the standard procedures and with weighting coefficients from the Swiss general population [Citation27]. Higher scores indicate a better health-related quality of life.
At week 24, the online survey, Behavior Change in Energy Management – Survey (BCEM-S), was administered. This survey based on existing literature [Citation28–30] invited the study participants to answer eight questions to document change in energy self-management behavior, the effectiveness of stable strategies and the difficulty to implement them (visual analogical scale 0–10), and the reasons for nonuse.
Statistical methods
Data were analyzed using IBM SPSS statistics for Windows version 28.0 [Citation31]. A descriptive statistic was performed for the sociodemographic characteristics of the study sample, the case report forms, and the online survey data. The outcome data were tested for normality using the Shapiro–Wilk test of normality. Then, a one-way repeated measures analysis of variance for within-subject differences and a post hoc test were performed. As effect size, we used partial eta squared (partial η2). For the sample size calculation, the mean differences between BL–T1 and the pooled standard deviations were used with a power 90% and a significant level of 0.05 [Citation32].
Results
Recruitment and response rate
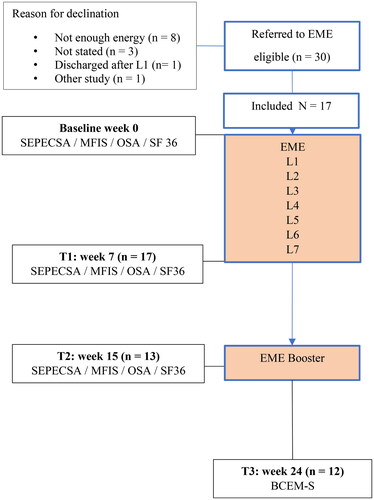
Between February and June 2022, 17 out of 30 eligible EME participants with long COVID could be included in the study (recruitment rate: 56.6%). At T1 (lesson 7), all study participants completed the assessment booklet (drop-out rate: 0%). At T2, two months after lesson 7, the assessments were sent by post, and 13/17 returned filled (76.5%). Five months after the EME started, 70% (12/17) of the study participants had completed the online survey ().
Figure 1. Study flowchart. EME: Energy Management Education; L: Lesson; SEPECSA: Self-efficacy for Performing Energy Conservation Strategies Assessment; MFIS: Modified Fatigue Impact Scale; OSA: Occupational Self-Assessment; SF36: Medical Outcome Study 36-item Short Form Health Survey; BCEM-S: Behavior Change in Energy Management – Survey.
Time requirements and study procedures
The time required to inform study candidates about the study was about five minutes. The distribution and collection of the assessment at T1 required an average of five minutes (range 1–15 min). For T2 and T3 (including two reminders), the time required was ten minutes per person. In general, filling in the assessments on paper was feasible and took 20–30 min, while the online survey had a median duration of 7 min. It was suggested to have a presence to answer queries for participants with language uncertainties and to allow study participants to fill in the assessments online if they preferred the online format over the paper format.
Participants
The sample size of this study was 17 (11 females and 6 males) with a mean age of 44.1 years. The time range between COVID-19 infection and EME start was broad (range, 2–18.5 months). Sixteen out of 17 study participants had a high fatigue impact (MFIS >39) [Citation33] at baseline. For detailed sociodemographic characteristics, see .
Table 2. Sociodemographic characteristics of the study participants.
Outcomes and treatment effect size
Changes in outcome measures were compared among subjects at baseline, post-intervention, and follow-up (). The results of the perceived self-efficacy to perform energy conservation strategies (SEPECSA) were statistically significant. The main increase was between BL and T1 (mean difference: 1.731) with a tendency to further increase at T2. In 12 out of 17 study participants, the improvement reached the minimal clinically important difference (Supplementary Figure 1). The fatigue impact (MFIS) decreased at T1 and T2. The difference between BL and T2 was statistically significant, without, however, reaching a minimal clinically important difference [Citation24]. The number of study participants with a high fatigue impact decreased (14/17) at T1 compared to BL and remained stable at T2. The perceived competency in performing daily activities (OSA) increased statistically significantly between BL and T2. The Physical Component Scale (PCS) of the health-related quality of life (SF36) showed a statistically significant increase between T1 and T2. In the Mental Component Scale (MCS) no statistically significant changes were registered. The effect size (partial η2) was large in three of four outcome measures (>0.14) ().
Table 3. Outcome data for self-efficacy, fatigue impact, competency in ADL, and QoL.
Implemented energy management strategies
The range of strategies used by the study participants before starting EME was 1–11 (median: 3). Two months after the end of EME the range was 1–12 (median: 4) ().
Figure 2. Energy management strategies in use before and after EME. EME: Energy Management Education.
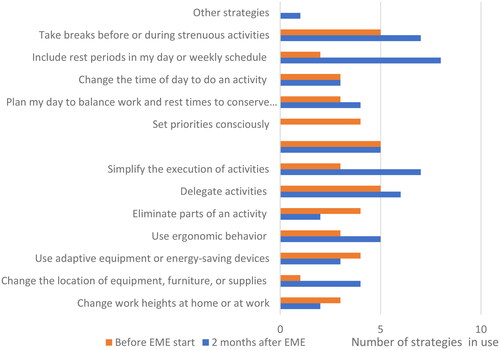
Participants rated “changing the time of day to do an activity,” “taking breaks before or during strenuous activities,” and “including rest periods in my day or weekly schedule” as the most effective strategies. No strategy in use was rated to be less effective than 7.14. (SD: 1.12). The simplest strategies to implement were “change work heights at home or work”, “set priorities consciously,” and “eliminate parts of an activity,” while the most challenging were “delegate activities change,” “communicate needs to others,” and “balance work and rest times.”. The most frequent reason for not having implemented a strategy was a “lack of moral support” and “conviction that a strategy would not have made a real difference.” (Supplementary Tables 1 and 2).
Discussion
The main objectives of this feasibility study were to gather data for planning a main study that investigates the effectiveness of EME on various outcomes of interest for individuals with long COVID. Over a period of five months, 17 out of 30 eligible subjects agreed to participate in the study. The procedural issues were found to be feasible. The effect size was significant in three out of four outcomes after the intervention, and it further increased during the follow-up period. As a result, a relatively small sample size would be needed for a 90% powered RCT.
Regarding the procedural uncertainties, the data showed a sufficiently high recruitment rate (53%) and follow-up rates (76% and 70%). The inclusion and exclusion criteria and the screening tools were feasible and allowed to identify, during the five months, 30 eligible subjects. Unsurprisingly, the most common reason for declining participation was the high level of fatigue. To avoid an unbalanced study sample in future research, stratification by fatigue level can be used. Regarding gender and age, the study sample exhibited typical sociodemographic characteristics of individuals with long COVID (higher prevalence among females and middle-aged individuals) [Citation34]. However, the time since COVID infection onset varied widely (interquartile range: 7.5–16 months). This parameter is expected to decrease in the future in Switzerland as more specific rehabilitation opportunities become available for individuals with long COVID, and physicians refer patients more promptly. Individuals with long COVID, including former EME participants, emphasized the importance of structured information about fatigue, post-exertional malaise, helpful behavior strategies, and peer exchange experiences to avoid feeling isolated from the early stages of the condition [Citation13]. In the main study, in addition to the paper form, a digital data collection system should be implemented at all time points, using SF-12 instead of SF-36, and onsite support should be provided to individuals with any queries. This will help reduce the number of error-prone procedures and the time required.
Regarding changes in the outcome dimensions, the data revealed a significant effect size in perceived self-efficacy in performing energy conservation strategies, fatigue impact, and competencies in daily activities. The selection of outcome instruments that reflect various aspects of managing fatigue in daily life has proven to be appropriate, as they demonstrated sufficient sensitivity to capture changes. However, it is important to note that the course of long COVID and its primary symptom remains unclear due to the lack of solid longitudinal studies [Citation35,Citation36]. Additionally, it is worth considering that EME was part of an interdisciplinary rehabilitation program, and the reported changes, particularly in fatigue, may be a cumulative effect of the entire program.
The fact that the level of self-efficacy continues to increase after the intervention may be attributed to the regular use of the strategies. This finding aligns with the results of the online survey and other self-management education studies conducted with individuals with chronic conditions [Citation37]. To address the remaining methodological uncertainty, it is reasonable to consider studies conducted with other populations that have examined the effects of EME. In a feasibility study with individuals suffering from multiple sclerosis (MS), the BL score of self-efficacy was 1.45 higher than that of the sample of the present study [Citation11]. The main reason for this could be the MS sufferers’ long experience with fatigue (mean disease onset, 13.9 years) and their pre-existing competence in using strategies in daily life. In contrast, the self-efficacy score at the end of EME was similar in both study populations (long COVID: 7.4; MS: 7.8). This comparison of data may help explain the large increase in the intermediate score in this study.
The online survey that documented the implemented energy management strategies and the behavior change was feasible, and the clarity of the question and consistency of the response categories were given. The results reported are in line with the data reported from a sample of persons with MS after an OT group intervention for fatigue management [Citation29]. In a future study, the survey should be maintained, as the investigated aspects can add a deeper understanding of the factors that transform behaviors into regular habits and routines. That knowledge can support OTs during the delivery of EME and the empowerment of the participants.
Limitations and strengths
The results lack a control group, and the clinical conditions and future study design may differ from this feasibility study. Additionally, there was a lack of documentation regarding treatment fidelity and information about the intensity of other interventions. However, despite these limitations, various aspects of feasibility were investigated, which will help in developing a solid study plan.
Conclusion
Persons with long COVID are a growing population challenging the healthcare system to support them with efficient treatment on the way back to everyday life. EME, an evidence-based self-management education delivered by specially trained OTs, aims to address the impact of fatigue experienced by individuals with long COVID in everyday life routines. This feasibility study provided valuable data for planning a clinical trial to investigate the effectiveness of EME on relevant outcomes. The eligibility criteria were practical in a clinical context, and the recruitment procedures were seamlessly integrated into routine care without excessive time demands. Questionnaires were completed in all parts, and the follow-up rate was satisfactory. The data revealed significant effect sizes in fatigue impact, self-efficacy in performing energy management strategies, and competency in daily activities. In a future study, fatigue impact could serve as the primary outcome measure and guide the calculation of the required study population. The study procedures demonstrated feasibility and the reported promising effect sizes of EME warrant further investigation.
Supplemental Material
Download Zip (255.9 KB)Acknowledgments
We would like to thank all participants involved in this study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- WHO. Post COVID-19 condition (Long COVID). WwwWhoInt/Europe. 2022. [cited 2022 November 21]. Available from: https://www.who.int/europe/news-room/fact-sheets/item/post-covid-19-condition.
- Nittas V, Gao M, West EA, et al. Long COVID through a public health lens: an umbrella review. Public Health Rev. 2022;43:1604501. doi: 10.3389/phrs.2022.1604501.
- Townsend L, Dyer AH, Jones K, et al. Persistent fatigue following SARS-CoV-2 infection is common and independent of severity of initial infection. PLOS One. 2020;15(11):e0240784. doi: 10.1371/journal.pone.0240784.
- Sivan M, Parkin A, Makower S, et al. Post-COVID syndrome symptoms, functional disability, and clinical severity phenotypes in hospitalized and nonhospitalized individuals: a cross-sectional evaluation from a community COVID rehabilitation service. J Med Virol. 2022;94(4):1419–1427. doi: 10.1002/jmv.27456.
- Taylor RR, Kielhofner GW. An occupational therapy approach to persons with chronic fatigue syndrome: part two, assessment and intervention. Occupational Therapy in Health Care. 2003;17(2):63–87. doi: 10.1300/J003v17n02_05.
- Asano M, Finlayson ML. Meta-Analysis of three different types of fatigue management interventions for people with multiple sclerosis: exercise, education, and medication. Mult Scler Int. 2014;2014:798285. doi: 10.1155/2014/798285.
- Bennett S, Pigott A, Beller EM, et al. Educational interventions for the management of cancer-related fatigue in adults. Cochrane Database Syst Rev. 2016;11(11):CD008144. doi: 10.1002/14651858.CD008144.pub2.
- Hersche R, Weise A, Michel G, et al. Development and preliminary evaluation of a 3-week inpatient energy management education program for people with multiple sclerosis–related fatigue. Int J MS Care. 2019;21(6):265–274. doi: 10.7224/1537-2073.2018-058.
- Mathiowetz V, Matuska KM, Murphy ME. Efficacy of an energy conservation course for persons with multiple sclerosis. Arch Phys Med Rehabil. 2001;82(4):449–456. doi: 10.1053/apmr.2001.22192.
- Packer TL, Brink N, Sauriol A. Managing fatigue: a six-week course for energy conservation. Tucson, Arizona: Therapy Skill Builders; 1995.
- Hersche R, Weise A, Michel G, et al. Three-week inpatient energy management education (IEME) for persons with multiple sclerosis-related fatigue: feasibility of a randomized clinical trial. Mult Scler Relat Disord. 2019;35:26–33. doi: 10.1016/j.msard.2019.06.034.
- Patt N, Kool J, Hersche R, et al. High-intensity interval training and energy management education, compared with moderate continuous training and progressive muscle relaxation, for improving health-related quality of life in persons with multiple sclerosis: study protocol of a randomized controlled superiority trial with six months’ follow-up. BMC Neurol. 2021;21(1):65. doi: 10.1186/s12883-021-02084-0.
- Hersche R, Weise A. Occupational therapy-based energy management education in people with post-COVID-19 condition-related fatigue: results from a focus group discussion. Occup Ther Int. 2022;2022:4590154. doi: 10.1155/2022/4590154.
- NICE Guideline. COVID-19 rapid guideline: managing the long-term effects of COVID-19. London: National Institute for Health and Care Excellence; 2022.
- Royal College of Occupational Therapists. Guidance: a quick guide for occupational therapists - Rehabilitation for people recovering from COVID-19 (2020). London: RCOT. 2020.
- Valko PO, Bassetti CL, Bloch KE, et al. Validation of the fatigue severity scale in a swiss cohort. Sleep. 2008;31(11):1601–1607. doi: 10.1093/sleep/31.11.1601.
- Beck AT, Steer RA, Ball R, et al. Use of the beck anxiety and depression inventories for primary care with medical outpatients. Assessment. 1997;4(3):211–219. doi: 10.1177/107319119700400301.
- McLennan SN, Mathias JL, Brennan LC, et al. Validity of the montreal cognitive assessment (MoCA) as a screening test for mild cognitive impairment (MCI) in a cardiovascular population. J Geriatr Psychiatry Neurol. 2011;24(1):33–38. doi: 10.1177/0891988710390813.
- Wang E, Chang JHC, Plow M. Predictors of fatigue self-management behaviors in adults with multiple sclerosis. NRE. 2022;50(1):75–87. doi: 10.3233/NRE-210179.
- Qualtrics. Qualtrics Software. 2023.
- Liepold A, Mathiowetz V. Reliability and validity of the Self-Efficacy for performing energy conservation strategies assessment for persons with multiple sclerosis. Occup Ther Int. 2005;12(4):234–249. doi: 10.1002/oti.5.
- Van Heest KNL, Mogush AR, Mathiowetz VG. Effects of a one-to-one fatigue management course for people with chronic conditions and fatigue. Am J Occup Ther. 2017;71(4):7104100020p1–7104100020p9. doi: 10.5014/ajot.2017.023440.
- Fisk JD, Ritvo PG, Ross L, et al. Measuring the functional impact of fatigue: initial validation of the fatigue impact scale. Clin Infect Dis. 1994;18(Suppl 1): s 79–83. doi: 10.1093/clinids/18.Supplement_1.S79.
- Kluger BM, Garimella S, Garvan C. Minimal clinically important difference of the modified fatigue impact scale in Parkinson’s disease. Parkinsonism Relat Disord. 2017;43:101–104. doi: 10.1016/j.parkreldis.2017.07.016.
- Kielhofner G, Forsyth K, Kramer J, et al. Developing the occupational self assessment: the use of rasch analysis to assure internal validity, sensitivity and reliability. Br J Occup Ther. 2009;72(3):94–104. doi: 10.1177/030802260907200302.
- Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Med Care. 1992;30(6):473–483.
- Roser K, Mader L, Baenziger J, et al. Health-related quality of life in Switzerland: normative data for the SF-36v2 questionnaire. Qual Life Res. 2019;28(7):1963–1977. doi: 10.1007/s11136-019-02161-5.
- DiClemente RJ, Salazar LF, Crosby RA. Health behavior theory for public health: principles, foundations, and applications. Burlington (MA): Jones & Bartlett Publishers; 2013.
- Matuska K, Mathiowetz V, Finlayson M. Use and perceived effectivness of energy conservation strategies for managing multiples sclerosis fatigue. Am J Occup Ther. 2007;61(1):62–69. doi: 10.5014/ajot.61.1.62.
- Mallik PS, Finlayson M, Mathiowetz V, et al. Psychometric evaluation of the energy conservation strategies survey. Clin Rehabil. 2005;19(5):538–543. doi: 10.1191/0269215505cr789oa.
- IBM Corp. IBM SPSS statistics for windows. New York, USA: IBM SPSS; 2020.
- Dhand NK, Khatkar MS. Statulator: an online statistical calculator. Sample Size Calculator for Comparing Two Independent Means. 2022.
- Flachenecker P, Kümpfel T, Kallmann B, et al. Fatigue in multiple sclerosis: a comparison of different rating scales and correlation to clinical parameters. Mult Scler. 2002;8(6):523–526. doi: 10.1191/1352458502ms839oa.
- Mendes Paranhos AC, Nazareth Dias ÁR, Machado da Silva LC, et al. Sociodemographic characteristics and comorbidities of patients with long COVID and persistent olfactory dysfunction. JAMA Netw Open. 2022;5(9):e2230637. doi: 10.1001/jamanetworkopen.2022.30637.
- Michelen M, Manoharan L, Elkheir N, et al. Characterising long COVID: a living systematic review. BMJ Glob Health. 2021;6(9):e005427. doi: 10.1136/bmjgh-2021-005427.
- Umesh A, Pranay K, Pandey RC, et al. Evidence mapping and review of long-COVID and its underlying pathophysiological mechanism. Infection. 2022;50(5):1053–1066. doi: 10.1007/s15010-022-01835-6.
- Farley H. Promoting self-efficacy in patients with chronic disease beyond traditional education: a literature review. Nurs Open. 2020;7(1):30–41. doi: 10.1002/nop2.382.
