Abstract
Purpose
Lower limb osteoarthritis (OA) is a prevalent condition that has a profound impact on an individual’s life in several domains, including occupational activities. The objective of this study was to systematically describe and compare work-related outcomes (e.g., employment status, absenteeism, and productivity loss) in individuals with and without lower limb OA.
Materials and methods
Five databases were searched until 17 June 2023. Studies were eligible for inclusion if they compared work-related outcomes between individuals with lower limb OA and healthy controls (e.g., people without OA or the general population).
Results
Seven studies met the inclusion criteria of which two were included in a meta-analysis. Meta-analysis revealed that individuals with OA were less frequently in paid employment than control individuals (odds ratio: 0.25; 95% confidence intervals: 0.12, 0.53). Evidence from single studies indicated greater absenteeism and presenteeism and poorer functional capacity in people with lower limb OA compared to controls.
Conclusions
This systematic review suggests that individuals with lower limb OA have poorer work-related outcomes than those without OA. Low study numbers and lack of consistency in the way work outcomes are defined and measured make accurate quantification of the impact of OA on work challenging.
Prospero: registration number: CRD42020178820.
Implications for Rehabilitation
Individuals with lower limb osteoarthritis (OA) are less frequently in paid employment and experience greater absenteeism and presenteeism and poorer functional capacity than people without OA.
For holistic management of lower limb OA, healthcare providers should have conversations about any difficulties experienced at work and include outcome measures related to work.
Clinicians should work with individuals with lower limb OA and employers to develop interventions to maximize work participation.
Introduction
Osteoarthritis (OA) is one of the leading causes of pain and disability among adults [Citation1]. Worldwide, it is estimated that over 300 million people are affected by OA [Citation2]. Although OA is often considered to be a disease affecting the elderly, it can affect people of all ages [Citation3]. Post-traumatic OA of the knee [Citation4] and ankle [Citation5] develops after joint injury, which commonly occurs at a young age and thus affects people for a considerable portion of their lives. While OA can occur in any joint, it most commonly affects the hip and knee [Citation6]. In fact, hip/knee OA is ranked as the 11th highest contributor to global disability [Citation7].
People with hip [Citation8], knee [Citation8], ankle [Citation9,Citation10], and foot [Citation11] OA typically experience chronic pain, reduced joint mobility, muscle weakness, and difficulties with ambulatory activities, which can limit participation and performance in recreational and occupational activities [Citation12]. A decreased ability to participate in work is concerning. Work is central to an individual’s personal identity and social status, providing financial and emotional security and independence [Citation13,Citation14]. The inability to work is associated with negative health outcomes such as poorer general health, mental health and psychological well‐being, high rates of medical consultation, medication consumption and hospital admission, and increased rates of overall mortality [Citation6,Citation15].
A previous systematic review identified that while research on the impact of OA on work participation is scarce and of low methodological quality, hip, and knee OA has an effect on work participation, including work productivity, sick leave, and work disability, but individuals generally cope with the difficulties experienced [Citation16]. Notably, this study did not compare work-related outcomes between individuals with and without OA. More recently, a 2021 systematic review investigated work-related outcomes in adults aged 16–50 years with all forms of arthritis (e.g., rheumatoid arthritis, systemic lupus erythematosus, and juvenile idiopathic arthritis) [Citation17]. The authors concluded that individuals with arthritis have moderate to high work limitations and a higher work disability, but no differences in absenteeism, compared to healthy populations. While data from the review by Berkovic et al. [Citation17] suggests the presence of serious work limitations in people with arthritis, the effect of lower limb OA on work is difficult to interpret due to the inclusion of individuals with a wide range of arthritic conditions. Further, this review only included participants aged up to 50 years old, which may have underestimated the impact of OA on work-related outcomes due to the progressive nature of the disease. With an increase in the retirement age and people staying in the workforce longer, there is an increasing number of people with OA working [Citation18–20]. Thus, a greater understanding of the impact of lower limb OA on work-related outcomes is needed [Citation21]. This systematic review aimed to compare work-related outcomes among individuals with lower limb OA compared to those without lower limb OA or the general population.
Methods
Protocol and registration
The protocol of this systematic review was registered with the international Prospective Register of Systematic Reviews (#CRD42020178820) [Citation22]. The review was performed according to the Preferred Reporting for Systematic Reviews and Meta-Analyses (PRISMA) criteria [Citation23].
Selection criteria
Studies were eligible for inclusion if they: included a population of working-age individuals (18–75 years) with OA affecting the hip, knee, ankle, and/or foot; included a comparator group of individuals without lower limb OA (e.g., people without OA or the general population); and reported work-related outcomes (e.g., employment status, absenteeism, presenteeism, productivity, and functional capacity) separately from other outcomes. Lower limb OA could be self-reported, clinically determined, or radiographically determined. For studies with mixed populations (e.g., upper and lower limb OA), studies were included if greater than 50% of the sample were people with lower limb OA, or data for lower limb OA participants were reported separately. Treatment studies were eligible for inclusion if baseline data on work-related outcomes was reported and compared to a control group. Non-English language studies, single case reports, qualitative studies, animal studies, abstracts from meetings and conferences, and review articles were excluded.
Literature search
A systematic literature search was conducted across five databases (PubMed, EMBASE, CINAHL, Web of Science, and Cochrane) from the date of database inception until 17 June 2023. Search terms were developed in consultation with a medical librarian. Three concepts were combined to identify relevant studies. The first concept of terms referred to the disease of interest (e.g., osteoarthritis) and its synonyms. The second concept of terms related to the hip, knee, ankle, and foot and included other anatomical terms used to refer to these joints, and the third concept of terms related to work (e.g., absenteeism) and synonyms for work (e.g., occupation). Supplementary Appendix 1 provides a detailed search strategy.
Screening
Two authors (YSA and RM) independently performed the search. All identified citations were uploaded into EndNote V.X9 and duplicates were removed. Search results were imported into Covidence (Veritas Health Innovation Ltd, Melbourne, Australia) for screening. Pairs of two authors (YSA, RM, MLP, HZ) independently reviewed the title and abstract screening. Full-text screening was performed by pairs of two authors (YSA, MLP, HZ), and any disagreements were resolved by a third senior author (MDS or VJ). Reference lists of all eligible studies were searched for additional titles.
Data extraction
The following data was extracted from all included studies: authors, year, country of publication, selection criteria, sample size, participant characteristics (e.g., age, sex, OA joint), and work-related outcomes. Data were extracted by one reviewer (YSA) and independently audited by a second reviewer (VJ).
Methodological quality assessment
A quality assessment of all eligible studies was completed using the epidemiological appraisal instrument (EAI), which has been shown to be a valid and reliable tool for the assessment of observational studies [Citation24]. This instrument comprises 43 items grouped into five sections: reporting, subject selection, measurement quality, data analysis, and generalization of results. Each item was scored as either “Yes” (score = 2), “Partial” (score = 1), “No” (score = 0), “Unable to determine” (score = 0), or “not applicable” (item removed from scoring). An overall score was derived as an average score across all applicable items (range = 0–2). Two authors (YSA and MLP), independently evaluated the methodological quality of the included studies. Scores were compared for agreement, and disagreements were resolved through discussion with a third investigator (MDS).
Data and statistical analysis
The Kappa (ĸ) statistic (95% confidence intervals (CI)) was calculated to determine the agreement between the two assessors for screening and methodological quality rating. The ĸ statistic was interpreted as: 0.00–0.20 = slight agreement, 0.21–0.40 = fair agreement, 0.41–0.60 = moderate agreement, 0.61–0.80 = substantial agreement, and 0.81–1.00 = almost perfect agreement [Citation25]. Statistical analysis was undertaken in SPSS (Version 26, IBM Corporation, Armonk, NY, USA).
Homogeneous studies were considered for meta-analyses in RevMan 5.4 (Cochrane Collaboration, Nordic Cochrane Center, Copenhagen, Denmark). We considered the graphic display of results, direction of effects, population characteristics and the I2 statistics (as an estimate of heterogeneity) when determining suitability for meta-analysis [Citation26,Citation27]. Effect sizes (odds ratios or standardized mean difference) and 95% confidence intervals (CI) were calculated for dichotomous or continuous outcomes respectively, and data presented in a forest plot. A narrative synthesis of results of studies that could not be included in meta-analyses was undertaken.
Results
Selection of studies
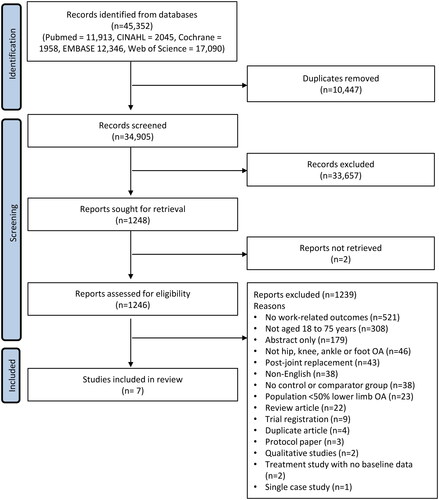
A total of 45 352 studies were identified from five databases, of which 10 477 duplicates were removed. Title and abstracts of the 34 905 remaining studies were screened, followed by a screening of 1246 full-text articles. Seven studies were eligible for inclusion in the review, and of those, two studies were ultimately included in the meta-analysis (). A manual reference list search of included studies did not reveal any additional eligible studies. Agreement between assessors for title/abstract screening and full-text screening was almost perfect (ĸ statistic (95% CI): 0.90 (0.81, 1.00) and 0.96 (0.81, 1.00), respectively).
Study characteristics
Study characteristics are detailed in . The seven included studies had a total of 4151 hip and knee OA participants (1574 participants with knee OA, 1494 with hip OA, 407 with both hip and knee, and 676 participants whose affected joint was not stated) and 14 767 control participants. All studies included participants with hip and/or knee OA, with no studies of individuals with foot or ankle OA. One study included a mixed population of OA locations, with 89% of participants having hip or knee OA [Citation33]. One treatment study was included in the review with baseline data (pre-total joint replacement surgery) for people with hip and knee OA compared to a reference population [Citation34]. Diagnostic criteria for OA varied between studies (). Job characteristics were reported in one study as either white-collar (e.g., professional, administrative, or support-type occupations) or blue-collar (e.g., trade or labor occupations) [Citation33], while another study stated that the majority of participants were farmers or had been engaged in farming [Citation31]. The other five studies did not indicate participant occupation [Citation28–30, Citation32, Citation34]. Work-related outcomes investigated were employment status [Citation28,Citation29,Citation31–33], absenteeism (time absent away from work) [Citation33,Citation34], presenteeism (reduced performance while at work) [Citation33], and physical capacity to work [Citation30].
Table 1. Characteristics of included studies.
Methodological quality assessment
Overall agreement between the two authors on the methodological quality of included studies was almost perfect (ĸ statistic (95% CI): 0.84 (0.81, 1.00)). Agreement was reached on 268 out of 301 EAI items (absolute agreement: 89%), with consensus reached on the remaining items. The total EAI scores for the included studies ranged from 0.75 to 1.15 out of a possible score of 2 (). The methodological quality assessment revealed that descriptions of the research objectives, study design, statistical methods, and key findings were addressed in all included studies [Citation28–34]. Four studies [Citation31–34], adequately reported the source of the participant population, and three studies [Citation31, Citation33,Citation34], included a control group that was comparable to the OA group in terms of the source of population and recruitment method. No studies accounted for the history of symptoms in analyses or reported sample size calculation, participant loss after entry, or the validity and reliability of the work-related outcome measures.
Table 2. Results from the quality assessment of included studies (n = 7) using the Epidemiological Appraisal Instrument.
Meta-analysis
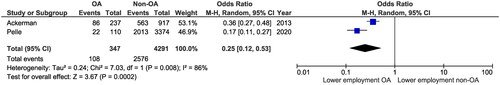
Due to variability in outcomes and the way work status was defined in the studies in this review, only two studies could be included in a meta-analysis. Two studies compared the percentage of individuals with lower limb OA (n = 347) and controls (n = 2576) who were in paid employment [Citation28, Citation32]. The odds of being in paid employment were lower in individuals with lower limb OA compared to controls without OA (pooled odds ratio (95% confidence intervals): 0.25 (0.12, 0.53); I2:87%; p < 0.001) ().
Narrative synthesis of individual studies
Employment status
Employment status was the most frequently explored work outcome, investigated in four studies (n = 4; 57%) [Citation28,Citation29, Citation31, Citation33]. It was measured as the proportion of participants who were: working (paid or unpaid employment status not stated) [Citation31], working in part time employment [Citation33], retired [Citation28], and employed in paid work (defined as ≥8 h work/week for the OA group and ≥12 h work/week for the control group) [Citation29].
Studies reported that individuals with OA were less likely to be working [Citation31], less likely to be working full-time (and more likely to be working part-time) [Citation33], and more likely to be retired [Citation28] than controls without OA/pain (). In contrast, Bieleman et al. [Citation29] reported similar rates of paid employment in individuals with hip and knee pain and/or stiffness and the general Dutch population when data was stratified by age, sex, and education level (). One study reported that workers with lower limb OA were more likely to hold jobs characterized by low demand and high control (as assessed with the Karasek job demand control measure [Citation35]) than healthy controls () [Citation33].
Table 3. Summary of results of individual studies.
Absenteeism
Absenteeism in individuals with hip and knee OA compared to controls was reported in two studies (28%) [Citation33,Citation34], with data collected via telephone interview (the Caremark Work and Health Interview) [Citation33] and retrospective analysis of data from the Swedish Social Insurance Agency [Citation34]. Ricci et al. [Citation33] collected absenteeism due to “any health reason” in the last two weeks, quantified in hours lost per worker per week [Citation36], and estimated absenteeism due to “arthritis or joint pain” for the hip and knee OA group as the difference from that reported by the control group. Stigmar et al. [Citation34] reported absenteeism as the number of days absent from work per month due to “any health-related reason” at intervals of 12, 6, and 3 months before joint replacement surgery.
Workers with hip and/or knee OA were more likely to miss work than controls and had more absenteeism (hours lost per worker per week) than controls for “any health-related reason” () [Citation33]. Absenteeism due to “arthritis or joint pain” in those with hip and/or knee OA was calculated at 0.57 h per worker per week [Citation33]. Male and female workers with hip and knee OA undergoing joint replacement surgery took a greater number of sick leave days per month than controls at all timepoints (3, 6, and 12 months) in the year prior to surgery, with absenteeism increasing as time to surgery decreased () [Citation34].
Presenteeism
Presenteeism, defined as reduced performance while at work, was reported in one study [Citation33]. The telephone-based Caremark Work and Health Interview questionnaire was used to quantify presenteeism in hours lost per week in the last two weeks due to “any health-related reason” and due to “arthritis”. Workers with hip and/or knee OA were more likely to report reduced work performance due to “any health-related reason” than controls, but groups did not differ in the hours lost at work per worker per week () [Citation33].
Functional capacity at work
One study compared the functional capacity to perform physical job demands between male and female workers with hip and knee pain and/or stiffness and healthy workers [Citation30]. Functional capacity was measured using six tests of the work-well systems functional capacity evaluation [Citation37]: lifting low (e.g., from table to floor), lifting overhead, two-handed carrying, overhead working (e.g., postural tolerance of overhead working), dynamic bending (e.g., repetitive bending), and repetitive side reaching (e.g., fast repetitive side movement). Male OA participants performed poorer than healthy male workers on lifting low, two-handed carry, and dynamic bending, and female OA participants performed poorer than their healthy working counterparts on all six tests ().
Discussion
This systematic review aimed to compare work-related outcomes between individuals with lower limb OA and controls. The literature in this area is limited, with only seven studies identified, and the heterogeneity of outcome measures meant that only two studies could be included in a meta-analysis. Data from a meta-analysis indicate that individuals with lower limb OA are less likely to be in paid employment than healthy controls without OA. Evidence from single studies showed that individuals with lower limb OA were more likely to be in part-time employment or retired, have more work hours lost due to absenteeism, report reduced work performance, and have lower functional capacity compared to controls. There were mixed findings from individual studies on the proportion of people with and without lower limb OA who were working.
Employment status was the most commonly investigated work outcome in the studies included in this review. Our meta-analysis revealed that fewer individuals with hip and knee OA were in paid employment than individuals without OA. A systematic review by Bieleman et al. [Citation16] found that hip and knee OA had a mildly negative effect on work participation; however, as this review did not compare employment status between people with and without OA, results cannot be directly compared with our data. Further, a recent systematic review on work-related outcomes in young to middle-aged adults with arthritis reported lower employment rates in those with arthritis compared to healthy populations [Citation17]. The population in this study differs from our review in that it consists of individuals with a range of types of arthritis, including rheumatoid arthritis, systemic lupus erythematosus, and juvenile idiopathic arthritis.
There is mixed evidence from single studies on employment status in people with and without lower limb OA. Lin et al. [Citation31] reported that individuals with OA were less likely to be working (paid or unpaid employment not stated), whereas Bieleman et al. [Citation29] reported similar paid employment rates between groups. Differences in findings may be due to different methodologies. Bieleman et al. [Citation29] controlled for potential confounding factors, such as age, sex, and education level, and used a more conservative definition of paid work in the OA group (≥8 h of work per week) compared to the control group (≥12 h of work per week). Employment data from individual studies also identified that people with hip and knee OA were more likely than controls to be employed part-time [Citation33], work in jobs with low demand and high control [Citation33], or be retired [Citation28]. However, the higher reported retirement rate among individuals with hip and knee OA should be interpreted with caution, as control participants were younger (median age: 55 years) than OA participants (median age: 66 years) [Citation28]. The lack of a consistent definition of employment status and differences between OA and comparator groups make it difficult to accurately quantify the impact of OA on work.
Based on data from two single studies, individuals with hip and knee OA have greater absenteeism from work than controls [Citation33,Citation34]. Workers with OA took over twice as much sick leave than controls for “any health-related reason” [Citation33,Citation34], with absenteeism due to “arthritis” estimated to be 0.57 hours per worker per week [Citation33]. Data from the study by Stigmar et al. [Citation34], identified an increase in sick leave with closer proximity to joint replacement surgery, suggesting that the severity or progression of hip and knee OA is associated with greater hours of sick leave. Greater absenteeism in individuals with hip and knee OA is supported by a systematic review that found an association between chronic knee pain and absenteeism [Citation38]. It should be noted that, as it is common for workers not to disclose a health issue due to concerns about job security [Citation39], it may be difficult to obtain a precise estimate of absenteeism attributable to OA. Furthermore, comorbid health conditions are more common among individuals with OA than those without OA [Citation40], and as such, absenteeism among workers with OA may be high due to both OA and other comorbidities. Thus, future studies should include measures of comorbid conditions to disentangle the impact of OA on work from that of other health conditions.
Workers with hip and knee OA were more likely to report reduced work performance (presenteeism) than workers without hip and/or knee OA or back pain, but hours of lost productive work time did not differ between groups [Citation33]. It was estimated that health-related lost productive time in workers with hip and/or knee OA costs United States employers $22.8 billion per year, which is $15.96 billion per year more than that in workers without hip and/or knee OA or back pain [Citation33]. This suggests that productivity in people with lower limb OA is a serious concern for both individuals and society. A recent qualitative study found that individuals with OA commonly lost time at work due to leaving early, arriving late, taking extra breaks, and being unable to take on extra responsibilities [Citation41]. As presenteeism is multi-dimensional and is influenced by a number of job-related factors, such as physical and psychosocial characteristics of work [Citation42], future research is needed to better understand the relative contribution of these factors.
In the study by Bieleman et al. [Citation30], the capacity to perform physically demanding tasks was poorer in workers with hip and knee OA compared to healthy workers. In addition, those with OA were found to have difficulty performing physical work, especially work that involved lifting objects to the floor, carrying objects, and repetitive bending. These findings are supported by a recent survey of employed senior workers with lower limb pain showing that the combination of physical work demands and lower limb pain is associated with limited ability to perform work [Citation43]. Performance of physical work was especially reduced in female workers with hip and knee OA [Citation30]. Considering all functional capacity tests performed, 20–40% of the younger women with OA (45–54 years) and 25–65% of the older women with OA (55–65 years) demonstrated functional capacities that could be considered insufficient to meet the lowest category of physical job demands (e.g., sedentary work) as described by the dictionary of occupational titles [Citation44]. A consequence may be the need for females with hip and knee OA to change jobs or leave the workforce due to an inability to meet the job demands, as was suggested by a recent study in eldercare workers with moderate to high musculoskeletal pain [Citation45]. Further research is needed to understand the effects of lower limb OA on current and future employment in this population.
This systematic review synthesized data from seven studies to compare work-related outcomes in individuals with lower limb OA compared to controls. This provides novel and important information on the impact of lower limb OA on work and differs from previous systematic reviews that have considered all locations and forms of arthritis together (e.g., rheumatoid arthritis, systemic lupus erythematosus, and juvenile idiopathic arthritis) [Citation17], and have not compared work-related outcomes between OA and controls [Citation16]. However, there are limitations that must be considered. At the review level, data pooling and comparison between studies were limited due to variable methodology, outcome measures, and timeframes for data collection. While the two studies included in the meta-analysis had similar findings, the same direction of effect, and relatively small confidence intervals that did not overlap, heterogeneity (based on the I2 statistic) was high [Citation26]. This may be because of the small numbers of individuals with OA and differences in sample sizes between studies (n = 22 [34] vs. n = 86 [Citation28]). Selection criteria for participants with OA varied between studies in the review and included radiographic [Citation31] or clinical [Citation32] diagnoses of OA, self-reported diagnoses [Citation28–30, Citation33], and participants who were scheduled for joint replacement surgery. [Citation34]. The diversity of study selection criteria and stages of OA is likely to influence the level of disability and workability, which makes comparing findings between studies difficult.
At the study level, our quality assessment revealed several limitations in the available literature. No studies accounted for the history of symptoms or severity of OA in analyses, reported sample size calculations, or reported the validity and reliability of the work-related outcome measures. Only three of the seven studies included a control group that was comparable to the OA group (source population and recruitment) [Citation31, Citation33,Citation34], and only one study controlled for potential confounding factors (e.g., age, sex, and education level) in the analysis [Citation29]. No studies investigated work-related outcomes in individuals with foot or ankle OA. Future research on foot and ankle OA and studies on lower limb OA that adjust for confounding factors, including the stage of OA, are needed to better quantify the impact of lower limb OA on work-related outcomes.
The findings of this systematic review indicate that OA can negatively affect work outcomes, but the impact is difficult to accurately quantify. Health care professionals, as one of the key providers of care to people with OA, are ideally placed to support clients’ desire to remain working by enquiring about possible difficulties performing work. A holistic, work-focused approach to care considers outcomes of interest to the individual. This recommendation is consistent with Fan et al. [Citation46] who suggested that core outcomes in OA should include time absent from work, employment status, work productivity, and work interference. While research shows that healthcare professionals have the potential to improve work-related outcomes in individuals with musculoskeletal conditions, there is variability as to whether work is included in patient management [Citation47]. There is also evidence that insufficient communication and collaboration between healthcare professionals and employers is a barrier to work participation [Citation48]. Healthcare professionals and employers should work together with employees with OA to implement suitable and sustainable management plans and refer to vocational specialists as needed.
Conclusion
Our systematic review suggests that individuals with lower limb OA, specifically hip and knee OA, have poorer work-related outcomes (employment status, absenteeism, presenteeism, and physical capacity) than those without lower limb OA. As lower limb OA is common in working-age adults and employment contributes to social, emotional, and financial well-being, there is a need to implement strategies to retain people with lower limb OA in productive employment without negatively impacting their health and determine consistent work outcomes to evaluate this.
Supplemental Material
Download PDF (73.2 KB)Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Vos T, Barber RM, Bell B, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the global burden of disease study 2013. The Lancet. 2015;386(9995):743–800. doi: 10.1016/S0140-6736(15)60692-4.
- Safiri S, Kolahi A-A, Smith E, et al. Global, regional and national burden of osteoarthritis 1990-2017: a systematic analysis of the global burden of disease study 2017. Ann Rheum Dis. 2020;79(6):819–828. doi: 10.1136/annrheumdis-2019-216515.
- Vos T, Abajobir AA, Abate KH, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the global burden of disease study 2016. The Lancet. 2017;390(10100):1211–1259. doi: 10.1016/S0140-6736(17)32154-2.
- Whittaker JL, Woodhouse L, Nettel-Aguirre A, et al. Outcomes associated with early post-traumatic osteoarthritis and other negative health consequences 3–10 years following knee joint injury in youth sport. Osteoarthritis Cartilage. 2015;23(7):1122–1129. doi: 10.1016/j.joca.2015.02.021.
- Brown TD, Johnston RC, Saltzman CL, et al. Posttraumatic osteoarthritis: a first estimate of incidence, prevalence, and burden of disease. J Orthop Trauma. 2006;20(10):739–744. doi: 10.1097/01.bot.0000246468.80635.ef.
- Bennell KL, Hinman RS. A review of the clinical evidence for exercise in osteoarthritis of the hip and knee. J Sci Med Sport. 2011;14(1):4–9. doi: 10.1016/j.jsams.2010.08.002.
- Cross M, Smith E, Hoy D, et al. The global burden of hip and knee osteoarthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis. 2014;73(7):1323–1330. doi: 10.1136/annrheumdis-2013-204763.
- Clynes MA, Jameson KA, Edwards MH, et al. Impact of osteoarthritis on activities of daily living: does joint site matter? Aging Clin Exp Res. 2019;31(8):1049–1056. doi: 10.1007/s40520-019-01163-0.
- Al-Mahrouqi MM, Macdonald DA, Vicenzino B, et al. Physical impairments in adults with ankle osteoarthritis: a systematic review and meta-analysis. J Orthop Sports Phys Ther. 2018;48(6):449–459. doi: 10.2519/jospt.2018.7569.
- Al-Mahrouqi MM, Vicenzino B, MacDonald DA, et al. Disability, physical impairments, and poor quality of life, rather than radiographic changes, are related to symptoms in individuals with ankle osteoarthritis: a cross-sectional laboratory study. J Orthop Sports Phys Ther. 2020;50(12):711–722. doi: 10.2519/jospt.2020.9376.
- Arnold J, Marshall M, Thomas M, et al. Midfoot osteoarthritis: potential phenotypes and their associations with demographic, symptomatic and clinical characteristics. Osteoarthritis Cartilage. 2019;27(4):659–666. doi: 10.1016/j.joca.2018.12.022.
- Hunter DJ, McDougall JJ, Keefe FJ. The symptoms of osteoarthritis and the genesis of pain. Rheum Dis Clin North Am. 2008;34(3):623–643. doi: 10.1016/j.rdc.2008.05.004.
- Tausig M. Handbook of the sociology of mental health. Berlin: Springer; 2013. The sociology of work and well-being; p. 433–455.
- WHO. International classification of functioning, disability, and health: children & youth version: ICF-CY. Geneva: World Health Organization; 2007.
- Waddell G, Burton AK, Kendall NA. Vocational rehabilitation –What works, for whom, and when? department for work and pensions. London; 2013. https://www.gov.uk/government/publications/vocational-rehabilitation-scientific-evidence-review.
- Bieleman HJ, Bierma-Zeinstra SM, Oosterveld FG, et al. The effect of osteoarthritis of the hip or knee on work participation. J Rheumatol. 2011;38(9):1835–1843. doi: 10.3899/jrheum.101210.
- Berkovic D, Briggs AM, Ayton D, et al. Arthritis-related work outcomes experienced by younger to middle-aged adults: a systematic review. Occup Environ Med. 2021;78(4):225–236. doi: 10.1136/oemed-2020-106640.
- Sharif B, Garner R, Sanmartin C, et al. Risk of work loss due to illness or disability in patients with osteoarthritis: a population-based cohort study. Rheumatology (Oxford). 2016;55(5):861–868. doi: 10.1093/rheumatology/kev428.
- Kenny GP, Yardley JE, Martineau L, et al. Physical work capacity in older adults: implications for the aging worker. Am J Ind Med. 2008;51(8):610–625. doi: 10.1002/ajim.20600.
- Van den Berg T, Elders L, de Zwart B, et al. The effects of work-related and individual factors on the work ability index: a systematic review. Occup Environ Med. 2009;66(4):211–220. doi: 10.1136/oem.2008.039883.
- Laires PA, Canhão H, Rodrigues AM, et al. The impact of osteoarthritis on early exit from work: results from a population-based study. BMC Public Health. 2018;18(1):472. doi: 10.1186/s12889-018-5381-1.
- Alyousef Y. The effect of lower limb osteoarthritis on work-related outcomes: a systematic review. PROSPERO 2020 CRD42020178820. Available from: https://wwwcrdyorkacuk/prospero/display_recordphp?ID=CRD42020178820. 2020.
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–269. doi: 10.7326/0003-4819-151-4-200908180-00135.
- Genaidy A, Lemasters G, Lockey J, et al. An epidemiological appraisal instrument–a tool for evaluation of epidemiological studies. Ergonomics. 2007;50(6):920–960. doi: 10.1080/00140130701237667.
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174.
- Deeks JJ, Higgins JP, Altman DG. Analysing data and undertaking meta‐analyses. In: Higgins JP T, Thomas J, Chandler J, et al., editors. Cochrane handbook for systematic reviews of interventions. UK: The Cochrane Collaboration and John Wiley & Sons Ltd; 2019. p. 241–284.
- Akobeng AK. Understanding systematic reviews and meta-analysis. Arch Dis Child. 2005;90(8):845–848. doi: 10.1136/adc.2004.058230.
- Ackerman IN, Ademi Z, Osborne RH, et al. Comparison of health-related quality of life, work status, and health care utilization and costs according to hip and knee joint disease severity: a national Australian study. Phys Ther. 2013;93(7):889–899. doi: 10.2522/ptj.20120423.
- Bieleman H, Oosterveld F, Oostveen J, et al. Work participation and health status in early osteoarthritis of the hip and/or knee: a comparison between the cohort hip and cohort knee and the osteoarthritis initiative. Arthritis Care Res (Hoboken). 2010;62(5):683–689. doi: 10.1002/acr.20112.
- Bieleman H, Van Ittersum M, Groothoff J, et al. Functional capacity of people with early osteoarthritis: a comparison between subjects from the cohort hip and cohort knee (CHECK) and healthy ageing workers. Int Arch Occup Environ Health. 2010;83(8):913–921. doi: 10.1007/s00420-010-0541-3.
- Ling J, Fransen M, Kang X, et al. Marked disability and high use of nonsteroidal antiinflammatory drugs associated with knee osteoarthritis in rural China: a cross-sectional population-based survey. Arthritis Res Ther. 2010;12(6):1–7.
- Pelle T, Claassen AA, Meessen JM, et al. Comparison of physical activity among different subsets of patients with knee or hip osteoarthritis and the general population. Rheumatol Int. 2020;40(3):383–392. doi: 10.1007/s00296-019-04507-1.
- Ricci JA, Stewart WF, Chee E, et al. Pain exacerbation as a major source of lost productive time in US workers with arthritis. Arthritis Rheum. 2005;53(5):673–681. doi: 10.1002/art.21453.
- Stigmar K, Dahlberg LE, Zhou C, et al. Sick leave in Sweden before and after total joint replacement in hip and knee osteoarthritis patients. Acta Orthop. 2017;88(2):152–157. doi: 10.1080/17453674.2016.1269051.
- Karasek R, Brisson C, Kawakami N, et al. The Job Content Questionnaire (JCQ): an instrument for internationally comparative assessments of psychosocial job characteristics. J Occup Health Psychol. 1998;3(4):322–355. doi: 10.1037//1076-8998.3.4.322.
- Stewart WF, Ricci JA, Leotta C, et al. Validation of the work and health interview. Pharmacoeconomics. 2004;22(17):1127–1140. doi: 10.2165/00019053-200422170-00003.
- Gross DP, Battié MC. Reliability of safe maximum lifting determinations of a functional capacity evaluation. Phys Therapy. 2002;82(4):364–371. doi: 10.1093/ptj/82.4.364.
- Agaliotis M, Mackey MG, Jan S, et al. Burden of reduced work productivity among people with chronic knee pain: a systematic review. Occup Environ Med. 2014;71(9):651–659. doi: 10.1136/oemed-2013-101997.
- Wilton RD. Disability disclosure in the workplace. Just Lour. 2006. doi: 10.25071/1705-1436.107.
- Marshall DA, Liu X, Barnabe C, et al. Existing comorbidities in people with osteoarthritis: a retrospective analysis of a population-based cohort in Alberta, Canada. BMJ Open. 2019;9(11):e033334. doi: 10.1136/bmjopen-2019-033334.
- Ching A, Prior Y. Exploring the perceptions of how living with osteoarthritis affects employed people’s work productivity. Musculoskelet Care. 2023;21(3):683–693. doi: 10.1002/msc.1739.
- Alavinia SM, Molenaar D, Burdorf A. Productivity loss in the workforce: associations with health, work demands, and individual characteristics. Am J Ind Med. 2009;52(1):49–56. doi: 10.1002/ajim.20648.
- Skovlund SV, Bláfoss R, Sundstrup E, et al. Joint association of physical work demands and leg pain intensity for work limitations due to pain in senior workers: cross-sectional study. BMC Public Health. 2020;20(1):1–10. doi: 10.1186/s12889-020-09860-6.
- Reich RB. Selected characteristics of occupations defined in the revised dictionary of occupational titles. Washington, DC: U.S. Department of Labor; 1993.
- Bláfoss R, Vinstrup J, Skovlund SV, et al. Musculoskeletal pain intensity in different body regions and risk of disability pension among female eldercare workers: prospective cohort study with 11-year register follow-up. BMC Musculoskelet Disord. 2021;22(1):771. doi: 10.1186/s12891-021-04655-1.
- Fan X, Straube S. Reporting on work-related low back pain: data sources, discrepancies and the art of discovering truths. Pain Manag. 2016;6(6):553–559. doi: 10.2217/pmt.16.8.
- Xie Y, Hutting N, Bartys S, et al. Interventions to promote work‐focused care by healthcare providers for individuals with musculoskeletal conditions a scoping review. J Occup Rehabil. 2021;31(4):840–865. doi: 10.1007/s10926-021-09971-w.
- Bartys S, Frederiksen P, Bendix T, et al. System influences on work disability due to low back pain: an international evidence synthesis. Health Policy. 2017;121(8):903–912. doi: 10.1016/j.healthpol.2017.05.011.