Abstract
Purpose
To identify articles that evaluated the efficacy of tele-rehabilitation after total hip replacement and to provide a reference for clinical decision-making and continuous improvement of rehabilitation exercise intervention strategies for clinical medical staff.
Methods
Embase, PubMed, Web of Science, Medline, China National Knowledge Network and Google Scholar databases were searched for randomized controlled trials of tele-rehabilitation after total hip replacement from inception to March 4, 2023. The two researchers used the PEDro scale to assess the methodological quality of the included studies. Two researchers used the PEDro scale to assess the methodological quality of the included studies.
Results
Ten studies with 632 participants were analysed.Compared to face-to-face rehabilitation, Internet-based telerehabilitation showed better outcomes in Get-up and go test (SMD −0.54, 95% CI −0.79 to −0.29). telerehabilitation showed no significant difference in outcomes of other functional tests and functional questionnaires.
Conclusion
In this systematic review and meta-analysis, internet-based tele-rehabilitation and face-to-face rehabilitation had the same effect on patients after total hip replacement, and compliance was higher in the tele-rehabilitation group, but attention should be devoted to standardizing this form of rehabilitation to avoid adverse events. In addition, the number and quality of included studies in this study are limited, and the outcome indicators and intervention means have not been unified. More high-quality studies are needed to verify these conclusions to better evaluate the effectiveness and advantages of telerehabilitation.
With the development of science and technology, remote rehabilitation technology will be applied to various fields of rehabilitation, providing personalized and extensive rehabilitation services.
The application of tele-rehabilitation technology to postoperative rehabilitation after total hip arthroplasty is feasible and can reduce the workload of healthcare professionals to a certain extent.
This review evaluated the randomized controlled trials of telerehabilitation after total hip arthroplasty, and the results showed that the clinical efficacy of telerehabilitation after total hip arthroplasty was not inferior to that of traditional rehabilitation.
Implications for rehabilitation
China’s population aging trend is inevitable, the prevalence rate of osteoporosis and osteoarthritis is increasing every year, and all types of Hip Diseases can easily occur [Citation1,Citation2]. Hip fracture is common in elderly patients with osteoporosis, with high morbidity and disability, and is expected to occur in more than 6.26 million patients by 2050 [Citation3]. Hip fracture and osteoarthritis not only reduce the quality of life of patients but also endanger life in severe cases [Citation4]. Total hip replacement (THA) is an effective treatment for hip fracture and osteoarthritis that can effectively relieve pain and improve function. However, the rehabilitation process after total hip replacement is complicated and the rehabilitation cycle is long, which greatly increases the work burden of medical staff. Moreover, most patients are older and have poor compliance, which has become a major problem in orthopedic rehabilitation [Citation5].
In recent years, advances in electronic communication technology and the emergence of COVID-19 have accelerated the development of “Internet + Medical treatment”. “Internet + medical treatment” has become an emerging medical service model that alleviates the difficulty of medical consultation to a certain extent and provides a new idea for orthopedic postoperative rehabilitation [Citation6]. Telemedicine mainly uses network communication technology, wearable devices or various Telemedicine platforms to build a communication platform between orthopedic surgeons and their patients to provide more direct and specific guidance for patient rehabilitation. It can provide remote real-time feedback and guide the rehabilitation process of patients, achieving an effect that cannot be achieved by traditional follow-up methods [Citation7,Citation8] and thus ensuring the continuity of rehabilitation treatment from hospital to home [Citation9], providing a new way of rehabilitation after orthopedic surgery.
A number of studies have used the Knee Joint Injury and Osteoarthritis Scale, Visual Analog Scale and other indicators to evaluate the rehabilitation effect of patients after knee joint replacement, and they have found that the effects of telemedicine are not inferior to those of traditional rehabilitation methods [Citation10,Citation11]. Mariana et al. conducted 12 weeks of tele-rehabilitation instruction for patients with hip fractures and showed that patients who received tele-rehabilitation instruction had higher scores on functional independence measures and functional activity tests [Citation12]. Alon et al. [Citation13] considered tele-rehabilitation as a supplement to standard physical therapy and conducted a tele-rehabilitation study on patients undergoing hip surgery. The results showed that the tele-rehabilitation group showed continuous improvement in all outcome indicators during follow-up, with greater improvement in the 2-min walking test (86.1%) and walking speed (65.6%). In contrast, no significant changes were observed in the control group during follow-up.
In recent years, there has been a growing body of research on telerehabilitation, and the National Quality Forum (NQF) published a report entitled “Creating a framework to support measure development for telehealth”. The number of randomized control trials (RCTs) on the clinical prognosis of telemedicine is limited, the quality of the methodology is variable, and the findings are not completely consistent. The effectiveness and safety of telemedicine intervention are not yet clear [Citation14]. At present, there is still a lack of systematic and comprehensive evaluations of this content, so it is difficult to formally draw a conclusion about the feasibility of tele-rehabilitation. The purpose of this study was to systematically and comprehensively evaluate the effects of tele-rehabilitation training for patients after total hip replacement and to provide references for clinical decision-making and continuous improvement of rehabilitation training intervention strategies for clinical medical staff, broaden the rehabilitation ideas of medical staff, and relieve the workload of medical staff.
Data and methods
Inclusion and exclusion criteria
The PICOS principles were used to determine the inclusion and exclusion criteria [Citation15]. The inclusion criteria were as follows: (1) the subjects (P) were patients ( ≥ 18 years old) who had undergone total hip replacement; (2) the intervention group (I) underwent remote rehabilitation, such as through video telephone/conference, telemedicine system, robot-assisted rehabilitation movement, virtual reality technology, sensors, wearable devices, etc.; (3) the intervention measures of the control group (C) were routine exercise rehabilitation; (4) the main outcome indicators (O) were scores on the Harris Hip Scale (HHS), Hip Disability and Osteoarthritis Outcome Score (HOOS), EuroQol Five Dimensions Questionaire, Get-up and go test (TUG), Concise Health Questionnaire-36 (SF-36), Functional Independence Scale (FIM), etc.; the secondary outcome indicators were patient satisfaction, self-efficacy, compliance; (5) the study design (S) is a randomized controlled trial. The exclusion criteria were as follows: (1) non-Chinese and English literature; (2) duplicate literature; (3) meeting abstracts, reports, plans, etc., for which data could not be extracted or information was incomplete; (4) low-quality literature, that is, a total PEDro score ≤4.
Retrieval strategy
This systematic review was performed in accordance with the Preferred Reporting Project (PRISMA) guidelines for Systematic Review and Meta-analysis to ensure high quality reporting[Citation16]. The protocol for this review was prospectively registered on the PROSPERO Register for Systematic Reviews (CRD42023401395). We searched Embase, PubMed, Web of Science, Medicine, CNKI and Google Scholar databases from inception to March 4, 2023.The combination of subject words and free words was adopted. In addition, the relevant literature was retrieved by the tracking literature method. The key terms used to retrieve studies from the PubMed database are shown in .
Table 1. Search strategies used in pubmed.
Literature screening and data extraction
Literature screening: First, the title and abstract were read, and obviously irrelevant literature was excluded, then, the full texts of the remaining studies were read to assess eligibility. The references of the included literature were manually searched to identify additional eligible studies. ② Data extraction: According to the inclusion and exclusion criteria, two researchers trained in systematic evidence-based knowledge independently conducted the literature retrieval, screening, extraction, summary and classification. In cases of conflicting opinions, the third researcher was consulted to reach a consensus. The following data were extracted: first author, year of publication, country, research object, type of included studies, research topic, number of included original studies, sample size, intervention measures, outcome indicators, etc.
Evaluation of methodological quality and evidence level
Two researchers independently evaluated the methodological quality and evidence level of the included studies. In cases of conflicting opinions, the third researcher was consulted until reaching a consensus. The PEDro scale was used to evaluate the methodological quality of the studies [Citation17]. A study scored as 6 or more is considered having good methodological quality (6–8: good; 9–10: excellent) and scored as 5 or less is considered being of acceptable or poor quality (4–5: acceptable; < 4: poor) [Citation18].
Data analysis method
There were various remote intervention methods and outcome index evaluation tools included in the studies, and there was substantial heterogeneity among the studies. Moreover, some studies did not conduct quantitative synthesis, so a descriptive analysis method was adopted in this study.
Results
Literature screening process and results
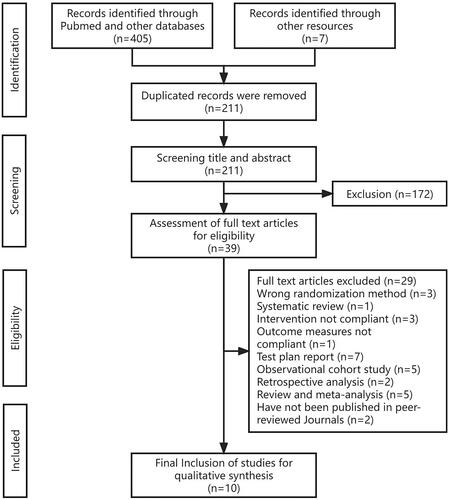
Initially, 412 records were found. After eliminating duplicates and screening, 39 (9.5%) studies were selected for full-text review. Of these, 29 (74.4%) were excluded after review and 10 (25.6%) were finally reviewed in detail (.). All 10 studies were randomized controlled trials.
Characteristics of studies
Ten studies were included in this review. The studies were conducted in China (n = 4), Australia (n = 2), the Denmark (n = 1), Germany (n = 1), Italy (n = 1) and Israel (n = 1). eight studies focused on total hip arthroplasty, two on total knee arthroplasty and total hip arthroplasty. A total of 695 arthroplasty patients (632 THAs and 63 TKAs) were recruited in these studies. Their mean age was 66.6 years, and the majority were females (58.7%). The characteristics of the included studies are presented in supplementary document 1
Evaluation of the quality of evidence included in the study
Two reviewers (A.G., W.C.) independently assessed the methodological quality of the included trials by applying the PEDro scale [Citation28]. The PEDro scale is an 11-item scale assessing eligibility criteria, random allocation, concealed allocation, similarity at baseline, participant blinding, therapist blinding, assessor blinding, >85% retention, intention-to-treat analysis, between-group statistical comparisons and point measures, and measures of variability. Each item is rated as 0 or 1, and the total score ranges from 0-11. The PEDro scale has been shown to be valid as a measure of methodological quality of clinical trials. The results showed that 7 studies were of "Good" quality, and 3 studies were of “Excellent” quality (.).
Table 2. Summary of PEDro scores for included studies.
Outcome measures of the selected studies
In this review, the effectiveness of tele-rehabilitation for THA patients was evaluated mainly by functional tests and functional scales, including the TUG test, the walking test, the HOOS score and the HHS score. In addition, the secondary outcome measures included satisfaction, compliance, and self-efficacy scores.
Functional test
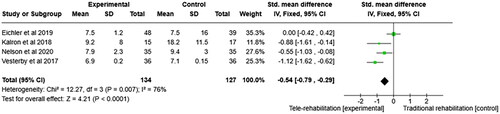
Five studies measured hip function. The meta-analysis revealed that the experimental group performed better than the control group in TUG tests at the completion of the intervention (SMD −0.54, 95% CI −0.79 to −0.29, p < 0.05, four RCTs, 261 participants, I2 = 76%) (.). In other functional assessments, including the Chair Rise Test [Citation13,Citation20], Hip muscle strength [Citation21,Citation24,Citation25] and Stair Ascend Test [Citation21,Citation24], no significant difference was detected between the two groups. However, in one study, the tele-rehabilitation group showed greater improvements on the walking test[Citation13]. One study could not be analyzed because the data were not available [Citation24].
Functional questionnaire
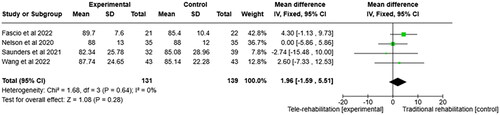
In this review, the functional assessments included HOOS, the HHS, the Oxford Hip Score and WOMAC score. The results of the meta-analysis showed that there was no significant difference in the HOOS score between the experimental group and the control group at the end of the intervention (SMD 1.96, 95% CI −1.59 to 5.51, p > 0.05, four RCTs, 270 participants, I2 = 0%) (). Other studies used the HHS score [Citation25,Citation26], the Oxford Hip score [Citation19] and WOMAC score [Citation20] and there were no significant differences between the two groups.
Other outcome indicators
Other outcome measures included satisfaction, compliance, quality-of-life scores, joint dislocation rate and self-perceived efficacy. Secondary outcome indicators were not included in the meta-analysis due to a lack of specific data and inconsistent evaluation indicators. Compliance was reported in two studies, all of which showed that compliance with tele-rehabilitation was significantly higher than that with traditional rehabilitation [Citation21,Citation26]. Three studies reported satisfaction, and the results showed no significant differences between the groups [Citation20,Citation21,Citation23]. Several studies reported relevant quality-of-life scores, with some showing no difference between the two groups [Citation19,Citation20,Citation22,Citation23] and others showing that the tele-rehabilitation group was higher than the control group [Citation27]. Wang [Citation25] compared the dislocation rates of artificial joints and found that the tele-rehabilitation group was lower than the traditional rehabilitation group, and the difference was statistically significant. Self-efficacy was assessed and there was no difference between the two groups [Citation23], with the tele-rehabilitation group being higher than the control group [Citation22,Citation27].
Discussion
A total of 10 articles were included in this systematic review and meta-analysis to evaluate the effectiveness of tele-rehabilitation in the recovery of motor function after hip replacement. Four studies [Citation14,Citation26–28] showed that tele-rehabilitation had a significantly better rehabilitation effect than traditional rehabilitation. Other studies [Citation20–25] showed that motor function was improved in both groups, but the difference between groups was not significant. A change above the minimal clinically important difference (MCID) threshold indicates a level of improvement in the outcome can be considered as a promising change in clinical level. According to the developed recommended levels of MCID for HOOS [Citation29], the threshold was set as 8.0–10.0 in this review. Among the studies using HOOS, only the study by Wang [Citation27] introduced MCID. But according to the original data from the studies included, all the four treatment groups from the four studies saw improvements in HOOS that met the criteria of MCID, which can largely prove that the tele-rehabilitation can effectively improve the outcome after surgeries. None of the other outcome measures indicated MCID.
This review generated new knowledge on the effectiveness of internet-based tele-rehabilitation. Compared with the traditional rehabilitation mode, the application of tele-rehabilitation provides convenient conditions for patients to carry out rehabilitation exercise at home. The included research results show that the compliance of the tele-rehabilitation group is significantly higher than that of the traditional rehabilitation group [Citation22,Citation27], and it can save medical resources, reduce patient costs after discharge, and reduce the time burden of therapists and caregivers. However, attention should be given to the standardization of use to avoid the occurrence of adverse events [Citation30,Citation31].
At present, with the rapid development of internet technology, the advantages of telemedicine continue to emerge and are gradually expanding the scope of application. As a product of the rapid development of communication and digital technology, telemedicine is being increasingly used in medical practice [Citation32] and has broad application prospects. In the future, tele-rehabilitation is expected to become an effective substitute for traditional rehabilitation and broaden the scope of rehabilitation services.
This study had some limitations. (1) Only articles published in Chinese or English were included in this review, which may have led to the omission of evidence from articles published in other languages. (2) In some studies, the generation, assignment hiding and blinding methods of random sequences are not clearly described, which may have led to selection and evaluation bias. (3) In some studies, the sample size was small, which may have affected the stability of the results. (4) The intervention measures included in the studies are different, so the best intervention mode of tele-rehabilitation cannot be determined. (5) The outcome indicators included in the studies have different forms, and thus, there was substantial heterogeneity, leading to bias in data analysis.
Conclusion
In this systematic review of meta-analyses, internet-based tele-rehabilitation had no less or even better efficacy for THA patients than face-to-face rehabilitation. The tele-rehabilitation group had a high level of compliance, but attention should be devoted to standardizing this form of rehabilitation to avoid adverse events. In addition, the number and quality of included studies were limited, and the outcome indicators and intervention means have not been unified. More high-quality studies are needed to verify these conclusion to better evaluate the effectiveness and advantages of telerehabilitation.
Authors’ Contributions statement
Zheng Zhou: Conceptualization Methodology.
Xiang Zhou: Literature retrieval.
Na Cui: Data Curation.
Hongjie Huang: Writing - Review & Editing.
Fan Yang: Investigation.
Gang Yang: Supervision.
Dingge Liu: Data Curation.
Kaiping Liu: Formal Analysis.
Xin Zhang: Writing - Review & Editing.
Jianquan Wang: Funding Acquisition. Editing.
Patient involvement statement
This document is not applicable
Supplemental Material
Download MS Word (18.1 KB)Disclosure statement
No potential conflict of interest was reported by the authors.
Data availability statement
The authors will supply the relevant data in response to reasonable requests.
Additional information
Funding
References
- Zou Z, Liu W, Cao L, et al. Advances in the occurrence and biotherapy of osteoporosis[J]. Biochem Soc Trans. 2020;48(4):1623–1636. doi: 10.1042/BST20200005.
- Safiri S, Kolahi A, Smith E, et al. Global, regional and national burden of osteoarthritis 1990-2017: a systematic analysis of the Global Burden of Disease Study 2017. Ann Rheum Dis. 2019;79(6):819–828. doi: 10.1136/annrheumdis-2019-216515.
- Lavernia CJ, Iacobelli DA, Brooks L, et al. The cost-utility of total hip arthroplasty: earlier intervention, improved economics. J Arthroplasty. 2015;30(6):945–949. doi: 10.1016/j.arth.2014.12.028.
- Ekhtiari S, Gormley J, Axelrod DE, et al. Total hip arthroplasty versus hemiarthroplasty for displaced femoral neck fracture: a systematic review and meta-analysis of randomized controlled trials. J Bone Joint Surg Am. 2020;102(18):1638–1645. doi: 10.2106/JBJS.20.00226.
- Groot L, Latijnhouwers D, Reijman M, et al. Recovery and the use of postoperative physical therapy after total hip or knee replacement. BMC Musculoskelet Disord. 2022;23(1):666. doi: 10.1186/s12891-022-05429-z.
- Zhang M, Dai D, Hou S, et al. Thinking on the informatization development of China’s healthcare system in the post-COVID-19 era. Intell Med. 2021;1(1):24–28. doi: 10.1016/j.imed.2021.03.004.
- Fleischman AN, Crizer MP, Tarabichi M, et al. 2018 John N. Insall award: recovery of knee flexion with unsupervised home exercise is not inferior to outpatient physical therapy after TKA: a randomized trial. Clin Orthop Relat Res. 2019;477(1):60–69. doi: 10.1097/CORR.0000000000000561.
- Davidovitch RI, Anoushiravani AA, Feng JE, et al. Home health services are not required for select total hip arthroplasty candidates: assessment and supplementation with an electronic recovery application. J Arthroplasty. 2018;33(7S): S49–S55. doi: 10.1016/j.arth.2018.02.048.
- Agostini M, Moja L, Banzi R, et al. Telerehabilitation and recovery of motor function: a systematic review and meta-analysis. J Telemed Telecare. 2015;21(4):202–213. doi: 10.1177/1357633X15572201.
- Bini SA, Mahajan J. Clinical outcomes of remote asynchronous telerehabilitation are equivalent to traditional therapy following total knee arthroplasty: a randomized control study. J Telemed Telecare. 2017;23(2):239–247. doi: 10.1177/1357633X16634518.
- Buhagiar MA, Naylor JM, Harris IA, et al. Effect of inpatient rehabilitation vs a monitored Home-Based program on mobility in patients with total knee arthroplasty. JAMA. 2017;317(10):1037–1046. doi: 10.1001/jama.2017.1224.
- Ortiz-Pina M, Molina-Garcia P, Femia P, et al. Effects of tele-rehabilitation compared with home-based in-person rehabilitation for older adult’s function after hip fracture. Int J Environ Res Public Health. 2021;18(10):5493. doi: 10.3390/ijerph18105493.
- Kalron A, Tawil H, Peleg-Shani S, et al. Effect of telerehabilitation on mobility in people after hip surgery: a pilot feasibility study. Int J Rehabil Res. 2018;41(3):244–250. doi: 10.1097/MRR.0000000000000296.
- Hollander JWMAD. Creating a framework to support measure development for telehealth[J]. Washington, DC: national Quality Forum, 2017.
- Amir-Behghadami M, Janati, A, Population. Intervention, comparison, outcomes and study (PICOS) design as a framework to formulate eligibility criteria in systematic reviews. Emerg Med J. 2020;37(6):387–387. doi: 10.1136/emermed-2020-209567.
- Page MJ, Mckenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71.
- Maher CG, Sherrington C, Herbert RD, et al. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83(8):713–721. doi: 10.1093/ptj/83.8.713.
- Foley NC, Teasell RW, Bhogal SK, et al. Stroke rehabilitation Evidence-Based review: methodology. Top Stroke Rehabil. 2003;10(1):1–7. doi: 10.1310/Y6TG-1KQ9-LEDQ-64L8.
- Vesterby MS, Pedersen PU, Laursen M, et al. Telemedicine support shortens length of stay after fast-track hip replacement. Acta Orthop. 2017;88(1):41–47. doi: 10.1080/17453674.2016.1256939.
- Eichler S, Salzwedel A, Rabe S, et al. The effectiveness of telerehabilitation as a supplement to rehabilitation in patients after total knee or hip replacement: randomized controlled trial. JMIR Rehabil Assist Technol. 2019;6(2):e14236. doi: 10.2196/14236.
- Nelson M, Bourke M, Crossley K, et al. Telerehabilitation is non-inferior to usual care following total hip replacement—a randomized controlled non-inferiority trial. Physiotherapy. 2020;107:19–27. doi: 10.1016/j.physio.2019.06.006.
- Fascio E, Vitale JA, Sirtori P, et al. Early virtual-reality-based home rehabilitation after total hip arthroplasty: a randomized controlled trial. J Clin Med. 2022;11(7):1766. doi: 10.3390/jcm11071766.
- Saunders R, Seaman K, Emery L, et al. Comparing an eHealth program (My hip journey) with standard care for total hip arthroplasty: randomized controlled trial. JMIR Rehabil Assist Technol. 2021;8(1):e22944. doi: 10.2196/22944.
- Xiumei T. The comparative study of remote rehabilitation nursing and traditional nursing after total hip replacement in elderly patients with femoral fracture. Genomics and Applied Biology. 2019;38(12):5811–5816.
- Peixia W, Wenying W, Ying Y, et al. Effect of medical alliance combined with video recording guidance on the out-of-hospital rehabilitation of elderly patients undergoing hip replacement[J]. Chin J Modern Nurs. 2021;27(10):1340–1344.
- L G, J X, S Z. Application of remote live broadcast health education in home rehabilitation nursing of patients after hip replacement. Modern Nurse. 2021;27–28.
- Wang Q, Hunter S, Lee RL, et al. The effectiveness of a mobile application-based programme for rehabilitation after total hip or knee arthroplasty: a randomised controlled trial[J]. Int J Nurs Stud. 2023;140:104455. doi: 10.1016/j.ijnurstu.2023.104455.
- Moseley AM, Rahman P, Wells GA, et al. Agreement between the cochrane risk of bias tool and physiotherapy evidence database (PEDro) scale: a meta-epidemiological study of randomized controlled trials of physical therapy interventions[J]. PLoS One. 2019;14(9):e222770. doi: 10.1371/journal.pone.0222770.
- Klemt C, Smith EJ, Tirumala V, et al. Outcomes and risk factors associated with 2-Stage reimplantation requiring an interim spacer exchange for periprosthetic joint infection[J]. J Arthroplasty. 2021;36(3):1094–1100. doi: 10.1016/j.arth.2020.09.012.
- Rosner BI, Gottlieb M, Anderson WN. Effectiveness of an automated digital remote guidance and telemonitoring platform on costs, readmissions, and complications after hip and knee arthroplasties[J]. J Arthroplasty. 2018;33(4):988–996.e4. doi: 10.1016/j.arth.2017.11.036.
- Nelson M, Russell T, Crossley K, et al. Cost-effectiveness of telerehabilitation versus traditional care after total hip replacement: a trial-based economic evaluation[J]. J Telemed Telecare. 2021;27(6):359–366. doi: 10.1177/1357633X19869796.
- Dorsey ER, Topol EJ. State of telehealth[J]. N Engl J Med. 2016;375(2):154–161. doi: 10.1056/NEJMra1601705.