Abstract
Purpose
Therapeutic group interventions are commonly provided in acquired brain injury (ABI) inpatient rehabilitation settings, but little is known about the extent of therapeutic groups run for community-dwellers with ABI. This paper seeks to review current literature concerning the nature of therapeutic groups run for community-dwellers with ABI and the involvement of occupational therapists.
Materials & Methods
A scoping review was conducted with systematic searching of relevant databases guided by Arksey and O’Malley’s framework. Studies were included if they reported on therapeutic groups for community-dwellers with ABI. Articles were collated and summarised with key findings presented in narrative form with accompanying tables.
Results
Seventy articles met inclusion. Groups are used as therapeutic change agents for community-dwellers with ABI and target a diverse range of participation barriers. Participants valued group programs that established safe environments, a sense of belonging, growth opportunities and social connections. Group accessibility needs to be improved, with better funding avenues available for service providers, as well as greater consumer involvement in group design and facilitation.
Conclusions
Groups are a valuable therapeutic modality supporting community-dwellers with ABI. Further research is warranted into the use of groups by occupational therapists working with community-dwellers with ABI.
Therapeutic groups can support the development of social connections, community participation and help community-dwellers with ABI re-establish a positive self-identity.
Conducting groups in community settings and involving consumers in group design and facilitation may enhance the group experience for participants.
Occupational Therapists should be involved in the design and delivery of occupation-based and participation focused group-based programs.
IMPLICATIONS FOR REHABILITATION
Introduction
Acquired brain injury (ABI) is a significant global health issue and leading cause of death and lifelong disability [Citation1,Citation2]. Acquired brain injury refers to brain injury acquired after birth not attributed to a congenital or degenerative disease, of which stroke and traumatic brain injury (TBI) are the two foremost causes [Citation3]. Worldwide, it is estimated over 100 million people have ongoing impacts from ABI [Citation2], and each year an estimated one in five hundred people experience an ABI [Citation4,Citation5]. The impact of brain injury is unique to each individual but commonly includes physical, cognitive-behavioural and psycho-social changes which can lead to significant functional impairments, activity limitations and participation restrictions [Citation6].
Inpatient ABI rehabilitation is routinely provided during the acute stages of recovery with therapy focusing on remediation of affected body function domains [Citation7], and maximizing functional performance of basic and instrumental activities of daily living [Citation8]. Therapeutic group work is commonly used as a modality through which to address therapy goals and promote social interaction for inpatients as they adjust to their newly acquired disability [Citation9]. Group facilitation is considered a core skill of occupational therapy and affords clinicians the opportunity to target a variety of goals within a social, naturalistic context [Citation10]. Permanent effects of ABI are not always resolved upon hospital discharge however, and many community-dwelling people with ABI may require ongoing support as they adjust and compensate for changed circumstances [Citation3]. Therapy priorities also evolve during this time, from a focus on remediation and discharge deadlines, to returning to community living and the accompanying roles, routines, occupations and relationships that importantly provide meaning and identity [Citation11].
This shift in priorities, signposted by the significant move from hospital to home, is recognised as a critical period in the rehabilitation journey, and marks the end of the intense inpatient stage and the beginning of outpatient services and the community reintegration process [Citation12]. The discharge milestone, while initially perceived as an important and positive turning point for families, can also be a challenging time of adjustment, particularly as returning to previously held roles may be difficult and ongoing care required from family members more intense than anticipated [Citation13]. The loss of previously valued social connections with both work colleagues and friends [Citation14], as well as reduced formal and informal social supports [Citation15] are possibly the most significant challenges facing community-dwelling individuals with ABI. This isolation can be amplified by the loss of accompanying meaningful life roles including employment and leisure activities [Citation16]. In addition to losing previous roles and relationships, the persistent interpersonal and communication skill deficits commonly experienced by individuals with ABI, can make it difficult to establish new friendships and social connections post injury, contributing further to the reduced quality of life commonly reported by individuals with ABI [Citation16,Citation17].
Community-based therapeutic groups can offer opportunities to build social connections, reengagement, and social participation within local communities [Citation18]. Group membership in both old (pre-injury) and new (post-injury) social groups has been found to positively impact the health and wellbeing of group members navigating significant life transitions [Citation19]. Group membership can also play a valuable role in supporting post-traumatic growth in community-dwellers with ABI, as they come to terms with the extent of ongoing problems and forge a new self-identity post-injury [Citation20]. Community ABI group membership has been shown to facilitate social reintegration, improve perceived life satisfaction and quality of life, as well as support and enhance community participation [Citation21]. Leisure activities, commonly impacted by ABI, can also be positively explored and supported in group-based formats [Citation22], with several studies linking leisure participation with improved confidence, skill acquisition, self-esteem and mood [Citation23].
While supporting engagement in meaningful occupations and promoting community participation is considered core business for occupational therapists, little is known about the extent of occupational therapy involvement in designing and facilitating therapeutic groups for community-dwellers with ABI [Citation24]. Facilitators and barriers to group programs being offered by services or taken up by community-dwellers with ABI, are also not well understood. Whilst there is a body of evidence exploring the effectiveness, barriers, and facilitators of groups in inpatient settings for people with ABI [Citation8,Citation25] less is known about community-based groups. Given the potential for community-based therapeutic groups to address the long-term sequelae of ABI, understanding current practice, as well as barriers and facilitators could inform and enhance practice in this area.
The objective of the scoping review is to explore what is known about the characteristics of current therapeutic groups run for community-dwelling adults with acquired brain injury and the involvement of occupational therapists in the implementation of these groups.
Materials and methods
Several systematic approaches to reviewing health research evidence have emerged in recent decades. Systematic reviews are popular choices when the research question is clearly defined, and the ideal study design required to answer the question can be anticipated. In comparison, scoping reviews are useful approaches when the research question is broader and might be answered through a range of study designs [Citation26,Citation27]. Given the intention of this review is to explore the broad characteristics of therapeutic groups, a scoping review was chosen as the appropriate methodological approach [Citation26,Citation28]. This scoping review followed Arksey and O’Malley’s five step framework [Citation26] and included further methodology recommendations proposed by Tricco et al. [Citation29] and Peters et al. [Citation30]. The protocol was registered at Open Science Framework (OSF) prior to data extraction and can be accessed at https://osf.io/9va2x/. The optional consultation stage was also followed.
Stage 1: Identifying the research question/s
The four key questions guiding the scoping review were:
What types of therapeutic groups are currently run for community-dwellers with ABI?
What are the key characteristics of these groups?
What are the barriers and facilitators that impact the provision and uptake of therapeutic groups for community-dwellers with ABI?
Which therapeutic groups have an occupational therapist involved in their implementation?
Stage 2: Identifying relevant studies
Search terms were developed through identification of terms commonly used to describe therapeutic groups, as well as consultation with a research librarian and a consumer with a lived experience of brain injury.
On May 20th, 2022, CK searched for recent peer-reviewed articles in CINAHL, MEDLINE, PsycINFO, Scopus, Web of Science and Embase databases. The search terms used for the population (brain injury), context (community-dwelling) and concept (therapeutic groups) in CINAHL database are provided in Supplemental Material.
Stage 3: Study selection
Qualitative, quantitative, and mixed methodology studies that reported on therapeutic groups for community-dwellers with ABI, were reviewed and eligible for inclusion if they were peer reviewed and published between January 1st, 2012, and the day of the search (May 20th, 2022). Limiting the search to a ten-year period allowed for studies to reflect current practice. Studies were excluded if they were conference abstracts, single case studies, protocols, posters, or dissertations.
Additional inclusion criteria required:
Group members to be community-dwellers at the time of participation in the group, and more than 50% of group members to have an ABI diagnosis.
Group members to have a mean age between 18 and 65.
Groups to have a therapeutic focus; that is, the group was designed to improve the health and wellbeing of group members and address goals of participation or occupational engagement [Citation31]. Group interventions with an impairment remediation focus and absence of a participatory or occupation goal, were not included in the review, nor were group interventions with a clear alignment with the remit of a different allied health professional, such as a lower limb exercise group.
Groups to be the primary modality (≥ 50%) used for therapeutic interventions. Accepted groups included face-to-face groups, as well as online groups involving interaction via a web-based or social media platform.
The average number of group members to be more than two.
Levac et al. [Citation27] recommend scoping reviews involve teams that adopt transparent and replicable processes. In this scoping review, title and abstracts of all articles were independently reviewed by two members of the research team to determine eligibility. Differences in ratings were discussed in team meetings and resolved by consensus or by the decision of a third reviewer.
Stage 4: Charting the data
The data collection form was developed by CK in response to the scoping review questions and further refined following feedback from the research team.
The form was pilot tested in Covidence and further changes made during the early stages of data extraction as per Levac et al.’s [Citation27] recommendations. The data collection form listing items uploaded and used in Covidence is included in Supplemental Material. Collected data were exported to an Excel spreadsheet once all articles were reviewed.
Stage five: Collating, summarising, and reporting results
It is not the purpose of scoping reviews to appraise the levels of evidence for these studies [Citation32] therefore the reported effectiveness of interventions delivered within those programs has not been reported. Descriptive data were collated and formatted within the Excel spreadsheet. Key findings are presented in narrative form with accompanying tables and figures. In keeping with Levac et al.’s [Citation27] recommendations, a qualitative analysis was undertaken of all qualitative studies to complement the descriptive data. The qualitative analysis involved CK familiarising herself with the articles to identify passages of text which discussed the experiences of group participants, family members and group facilitators. From this first review, initial concepts were generated. These concepts were recorded in a table format and further revised upon reviewing quotes and concepts from the complete data set. During this stage, several patterns emerged, which were further refined and developed into three key themes. An example of the theme development process is provided in .
Table 1. Example of theme development process for one theme.
Optional stage: consultation
Arksey and O’Malley suggest consumer consultation can provide additional insights into a research topic [Citation26]. For this scoping review, two consumers with a lived experience of ABI were consulted on proposed search terms for stage 2. Based on their recommendations, eight additional terms were included in the final search strategy. The scoping review findings were also shared with the consumers and they were invited to respond to the findings and advise which points should be highlighted in the discussion section. Final discussion points in the scoping review were clarified based on their recommendations.
Results
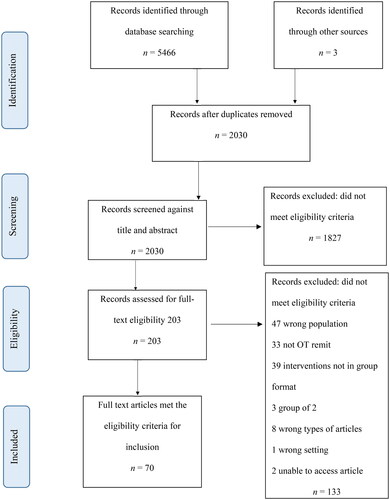
The article search and review process is outlined in .
The initial search retrieved 5469 articles. Following the removal of 3439 duplicate articles, a further 1827 articles were excluded based on title and abstract review, leaving 203 articles. Upon completion of the full text review, a total of seventy articles met the inclusion criteria for data extraction.
Key group characteristics extracted from the included articles are presented in . Additional tabled information relating to group focus, group activities and outcome measures can be found in Supplemental Material.
Table 2. Study and group characteristics.
Study designs
Study designs varied. Of the 70 included studies, 24 were randomised control trials, 16 were pre-post study designs, 14 were qualitative studies, and the remaining articles included case reports (n = 7), feasibility studies (n = 3), cohort studies (n = 3), retrospective studies (n = 2), and cross-sectional design (n = 1). Many studies (n = 49) quantitatively measured group effectiveness in some way, including pre-post group intervention outcomes without concurrent controls (n = 21), comparison of active group versus waitlist outcomes (n = 12) and comparison of active group versus alternative intervention (including different group interventions or traditional rehabilitation services) outcomes (n = 13). Three studies explored a 3-way comparison of two different group interventions to the control group [Citation47,Citation65,Citation93]. Apart from one study [Citation61], all articles that reported gender demographics had mixed gender groups for both control and intervention groups. Data for participants’ age included both mean age and range.
Types of groups
The therapeutic issues that group interventions targeted were varied. Of the seventy articles, 19 described interventions that targeted specific brain injury impairment including groups that addressed physical ABI impairments (n = 4), groups that focused on cognitive issues such as memory or executive functioning impairments (n = 9), and groups developed specifically for people with aphasia (PWA) or communication difficulties (n = 7).
A further 17 articles described programs that were rehabilitative in nature; they tended to be intense programs following closely on from a participant’s inpatient stay, multidisciplinary in their design and delivery, or with a wholistic focus on facilitating ongoing functional improvement or providing support for the adjustment to community living post ABI. Several articles described groups that sought to provide peer and social support (n = 5) or address mental health challenges experienced by people following ABI (n = 4), or were health promoting/self-management groups manualised for people with ABI (n = 9).
The final 18 articles described groups that had a focus on community participation; they included intervention groups that targeted community mobility (n = 2) or used leisure as both a therapeutic means and end (n = 8), as well as groups that explored the specific benefits of yoga (n = 6) and tai chi (n = 2).
Group participants
Of the 70 articles, 33 articles described groups for people who had experienced a stroke, 17 articles described groups exclusively for people with TBI, and the remaining 20 articles described groups for people with ABI (n = 16) or mixed groups with the predominant health condition being an ABI. When gender data were provided by articles, participants were classified either as male or female; there were no identified non-binary participants reported in the 70 studies, and only one article reported having a single sex group [Citation61]. The reviewed articles did not identify gender or sex considerations as a significant variable in their results or discussions, although most articles had a higher proportion of male participants to female participants, with the notable exception being a modified yoga group [Citation50]. Several groups (n = 19) included caregivers in one or more of the group sessions. Eight articles reported on groups in which caregivers/family members were invited to attend sessions as participants in their own right, while three articles reported that family members were invited to observe sessions to support learning, provide encouragement and assist with completion of homework tasks outside of the group sessions [Citation38,Citation43,Citation52]. Two articles reported that family members were invited to attend the final session, which included a graduation ceremony or group performance to celebrate the completion of the program [Citation72,Citation84].
Group size
Seventy one percent (50/70) of articles provided details about group size, most of which had three to nine participants. Groups that addressed specific ABI impairment areas such as upper limb, aphasia and memory tended to provide therapy to groups of three to eight people. Several studies discussed the challenges of attrition for both control and intervention groups, even for groups of reasonably short duration. Articles about peer/social support groups described groups that were open in nature and did not provide specific details about group sizes. When groups included educational sessions led by an external expert, they tended to be larger in size, and followed a lecture style format. Other groups which reported larger group sizes included leisure groups such as choir singing [Citation84], sport exploration [Citation70] and yoga [Citation50].
Group dosage/duration
There was considerable variety in the delivery of groups across the studies. Of the 61 articles that reported on the number of sessions provided, many groups (n = 31) seemed to provide somewhere between 6 and 12 sessions to group members, and commonly (n = 33) provided one session a week. Eighteen articles described groups held between two to four times a week, while some of the intensive programs included commitments from participants of four to five days each week (n = 8); these groups tended to expect participants to attend for several hours within a day. Three groups indicated they ran once a fortnight and one group ran once a month, while 17 articles described intense group experiences that ran for a long time (over six months) and expected participant attendance multiple times (more than three times a week) during the week for several months. Several of the self-management groups (n = 6) changed the group dosage within the group regime, usually meeting more regularly in the commencement stage of the group program, and then transitioning to booster style “top up” sessions that met less frequently.
Group sessions typically lasted between 60 and 150 min in length (n = 44) with a break at the turn of the hour. Longer group sessions commonly included morning tea or lunch in the group session. As mentioned, the intense group programs typically expected participant involvement for half to one full day over several days a week. This dosage tended to be required in the multidisciplinary outpatient clinics during the early stages of community re-entry.
Group setting
Medical-based settings were the most common environment for group programs to be run in. Of the 70 articles, 19 described groups that were run within a community neuro-rehabilitative setting with five groups conducted within a community hospital or an acute hospital’s outpatient facilities. Eight groups were conducted in university and research clinics, while other groups were conducted in community-based centres. Groups that utilised leisure as an intervention were more often conducted in communal areas such community sports centres, yoga studios, and wellness centres, and six groups described community outings as being part of their final group sessions. Three groups described a virtual reality platform or Facebook forum as the group intervention setting [Citation44,Citation66,Citation78]. Several studies did not provide details of the group setting beyond their occurring in the community.
Group activities
The therapeutic activities performed within groups were varied and aligned with the group’s purpose. Groups targeting physical impairments typically adopted task specific training in either part or whole practice, while memory groups reported including a range of remedial and internal/external compensatory strategies. Groups that used leisure as either a therapeutic means or end varied in the activities chosen but commonly provided participants with opportunities to engage in and experience the “doing” of leisure activities. Some leisure activities required group work and interaction (e.g., volleyball, canoeing, paddle tennis) while others could be experienced alongside other participants with little to no interaction (e.g., yoga, tai chi, golf). Other groups targeted commonly experienced activity limitations (outdoor walking) and community participation restrictions such as driving cessation and restricted community access. Seven groups utilised technology in the delivery of the group intervention such as virtual reality world EVA park and Facebook (n = 3) or as an intervention tool including use of smart phone apps, computer cognitive retraining and video games (n = 4).
Outcome measures
Reported outcome measures were diverse and included the participants’ experiences, goal achievement, changes in functional performance and daily activities, as well as broader measures of subjective wellbeing, self-efficacy, lifestyle changes, participation in life roles and community mobility. Mood, reintegration to normal living, and quality of life were also measured. Several studies reported using “quality of life” and community participation measurement tools as outcome measures irrespective of the level of the ICF that the group intervention was targeting. Both standardised and non-standardised measures were utilised in quantitative and qualitative studies. Two articles included a cost analysis of their group intervention as an outcome measure [Citation48,Citation56].
The Goal Attainment Scale (GAS) and the Canadian Occupational Performance Measure (COPM) were the two most reported goal setting tools described (n = 9). Whilst 28 articles reported the group intervention addressed individual participant goals only four studies described the goal setting process in detail [Citation42,Citation56,Citation72,Citation83]. Only a handful of studies reported on group member satisfaction or discussed group evaluation from the participants’ perspective [Citation56,Citation58,Citation60].
Perceptions and experiences of participants with ABI
The fourteen qualitative studies were analysed to provide a summary of key participant perspectives and identify emerging recurrent concepts across studies. Participants with ABI were overwhelmingly positive about their experiences and the benefits of group participation, identifying three key elements (or themes) they felt contributed to the transformative effect the group experience had played in their lives. These were a safe environment, a place that provides opportunities for growth and construction of a new self-identity, and a network of ongoing social connections.
The group provided a safe environment
A consistent theme across the qualitative studies highlighted that the groups provided a safe environment for participants which contrasted to the “outside world” in which participants felt defined by their disability. This supportive milieu was seen to be an essential element to the success experienced within the group. Salas et al. [Citation80] highlighted the importance of providing an emotionally safe and predictable milieu; a view shared by many of the studies (n = 10). In Norris et al.’s [Citation35] study, participants indicated that the physical setting of their leisure group, that is, a non-medicalised space within the local community centre, was also a significant factor in establishing a positive therapeutic environment. Donnelly et al. [Citation34] indicated participants found the specific changes made to the yoga studio environment to accommodate the needs or participants with TBI valuable, highlighting the importance of the physical environment, while Caute et al. [Citation44] indicated that the virtual world of EVA Park was perceived by participants to be a safe and welcoming space.
A place that provides opportunities for growth and construction of a new self-identity
Several participants identified that the group format created opportunities for personal growth which they attributed to the group experience and group activities that allowed participants to enjoy each other’s company, experience pleasure, humour and camaraderie, and be challenged on a physical, cognitive and social level [Citation33,Citation35,Citation76,Citation79]. Specifically, participants reported that being “occupied” in group activities allowed them to try new activities and reconnect with old ones [Citation38], challenged their whole body through enjoyable pursuits [Citation76], and provided them with a chance to experience themselves as successful [Citation80].
The concept of participants feeling safe, understood and accepted within the group milieu, leading to confidence to experiment [Citation44], to try new things [Citation36], and practice skills impacted by the brain injury [Citation38], which in turn allowed them the opportunity to construct a new self-identity was identified in a number of studies [Citation20,Citation79,Citation80]. Several studies reported participants felt a new sense of purpose and hope for the future in response to their newfound skills and burgeoning confidence [Citation33,Citation34,Citation91], while Salas et al. reported that participants felt they were provided with a chance to experience themselves as skilled and successful [Citation80]. For example, Salas et al. provided details about the specific benefits of the leisure occupation of pool; an unstructured activity that required cognitive, perceptual, physical, and social skills to be played, yet offered participants the opportunity to reconstruct a new sense of identity[Citation80]. Some participants indicated their success in occupations within the therapeutic setting served as a platform for renewed engagement in occupations and mainstream social groups outside the therapeutic milieu [Citation20,Citation34], as demonstrated by one participant from Donnelly et al.’s [Citation34] study who felt the ABI specific yoga program gave her the confidence to return to a mainstream yoga class; “I have [continued to practice yoga] because I found that I could do it…” p.2486.
A network of ongoing social connection:
Participants overwhelmingly identified the social connections experienced within the group as a significant contributor to the group’s transformative power. Participants frequently reported the group setting normalised their experiences of disability and provided them with a platform to acknowledge their own vulnerabilities and simultaneously learn from the lived experience of others. One participant from Niraj et al.’s [Citation36] article said "I know every person is different but when we are in this room, we are just like one person." p.740.
When asked, most participants were overwhelmingly positive about group co-facilitators with a lived experience of ABI. Participants reported that ABI group co-facilitators contributed significantly to feelings of normality and belonging [Citation80], providing practical advice and sharing of skills and knowledge, as well as offering participants encouragement and hope for the future [Citation91]. Participants’ experience of supporting others was described as a positive group attribute, with one participant from Donnelly et al.’s [Citation34] study stating: "it was empowering to be able to think of myself as a resource in a place where I was damaged." p.2487.
Several studies mentioned that new relationships formed in therapeutic groups developed into important long term social support networks that continued beyond the group milieu, such as group participants in Rotherham et al.’s study who exchanged phone numbers and met up for coffee [Citation79].
The long-term nature of the rehabilitation process was also mentioned by participants across several studies, with participants recognising that lifelong support would be required along their continuum of recovery. For some, this self-awareness also came from participation in the group and the social interactions with others [Citation63].
Barriers and facilitators to community therapeutic groups
Stakeholders reported on the barriers and facilitators of group programs offered by services and taken up by ABI community-dwellers.
Barriers
Some articles reported the group program yielded insignificant participant improvements given the time and resources allocated, although acknowledged that small sample sizes and poorly chosen outcome measures may have also contributed to their limited perceived effectiveness. Barriers to ABI participants joining therapeutic groups were identified in 43 of the 70 studies and included access issues (n = 14), cost (n = 7), group design issues (n = 6), group timing in the participant’s recovery journey (n = 4), communication issues (n = 4) as well as groups not accommodating participants’ unique ABI challenges and not providing appropriate group activities (n = 12). Some group participants reported that their physical, cognitive, and psychological challenges made them reluctant to join the group program, or anxious to participate in group activities they perceived as being too difficult for them [Citation70].
Exploring unmet needs is another way to consider barriers that prevent participants from receiving the services they require. Few articles reported on perceived participant unmet needs, but those articles that did, identified gaps in the provision of timely information, limited involvement of family members and significant others in the community rehabilitation process [Citation37,Citation85], poor support in assisting with successful return to work [Citation42] and a reticence from group facilitators to address participants’ sexuality [Citation100].
From the service provider’s perspective, barriers to implementing group programs included the high cost of setting up and facilitating group programs [Citation48], the required upskilling of therapist facilitators [Citation76], attrition rates minimising group program benefits [Citation86], the failure of funding schemes to routinely fund group interventions [Citation56] and fitting group interventions into the already full timetables of healthcare professionals and facilities [Citation85]. Clinician skill, facilitation competence, and adequate training may also contribute to services not offering group programs that meet participant needs. For example, Poncet et al. [Citation100] found group program therapists felt uncomfortable and unprepared to raise or address sexual health issues, despite participants identifying it as a topic they would like addressed.
Facilitators
In contrast, just over half of the included studies (n = 37) identified factors that supported the successful implementation of group programs. Factors identified by participants included improving access to the group for potential participants (n = 7), minimising costs or offering the group program for free (n = 8), involving volunteers and people with a lived experience of ABI as group facilitators (n = 6), allowing for more participant choice as to when group programs were scheduled (n = 5), offering enjoyable therapeutic activities that had been suitably modified to accommodate the needs of people within ABI friendly environments (n = 5), including family members in the group program (n = 8) and promoting social connections amongst group members that extend beyond the group program [Citation63,Citation84]. Participant perceived benefits from engagement in the group program can also be interpreted as a potential facilitator of future group program uptake [Citation34].
From the service provider’s perspective, factors which made it easier to implement group programs included receiving organisation and funding support to adequately plan and deliver a group program with the necessary resources and staff [Citation87], providing detailed preparatory training to facilitators close to the start of the intervention itself [Citation85] and affording adequate time for facilitators to debrief with each other at the completion of each group session [Citation76]. The timing of the group treatment period and the general readiness of the participant to re-engage in social activity were also significant factors impacting a group’s success [Citation56,Citation77]. Technology and social platforms were used to remind and promote participant desired behaviours in several studies with mixed success [Citation51,Citation56,Citation78]. It should be noted that student-resourced group programs were described in six articles, allowing for those groups to have high participant to facilitator ratios [Citation20,Citation21,Citation42,Citation72,Citation90,Citation99].
Group facilitators
Groups were delivered by a range of health disciplines including occupational therapists (n = 16), neuropsychologists (n = 15), speech pathologists (n = 10), allied health students (n = 6), physiotherapists (n = 4), exercise instructors (n = 4), as well as yoga and tai chi instructors (n = 6). Five studies were facilitated by volunteers with lived experience of brain injury (n = 5). Eight articles did not provide details about the background or profession of group facilitators. Reports on facilitator training varied; some facilitators received one-or-two-day’s training, while others were provided with instruction manuals. Of the 70 articles, 32 did not discuss what training was provided to facilitators.
Discussion
This scoping review was conducted to identify the types and characteristics of therapeutic groups currently run for community-dwellers with ABI. Barriers and facilitators were identified to inform implementation of therapeutic groups for community-dwellers with ABI. A specific focus on the occupational therapist’s role was then explored.
Surprisingly several groups appeared to replicate an inpatient rehabilitative experience in both the activities performed within the group and in the chosen group setting. From an ICF framework perspective, traditional style rehabilitation groups which target body function impairments and activity limitations accounted for 36 of the 70 reported groups, despite recent calls for rehabilitation services to set goals at the participation level of the ICF, or to contextualise them as involvement in a life situation [Citation101]. There is evidence that barriers in the social and physical environments of people with ABI can have a greater impact on successful return to community living than a person’s specific impairment issues [Citation102]. This suggests that greater scrutiny should be applied to the physical setting of the group as well as greater consideration of participant experiences of the group milieu.
Thirty-one of the group programs for community-dwelling participants were set in medical environments and university research clinics in contrast to community and health promoting centres (such as gyms, swimming pools and yoga studios). For group programs delivered outside of a medical, traditional therapeutic or hospital environment, the location choice was identified as an attractive feature of the group program, and interpreted by group members as a sign of their recovery and return to ‘normal occupations’ beyond the sick role [Citation34,Citation35,Citation90]. Interestingly, group participants of virtual world environments expressed similar views, reporting that in the virtual environment, they were less defined by their disabilities [Citation44]. Norris et al.’s participants also indicated they appreciated the performing of de-medicalised interventions; namely leisure and exercise occupations in group sessions, with de-medicalised facilitators such as gym and exercise instructors leading the programs rather than therapists [Citation35]. These views offer insight into the recovery journey of community-dwellers with ABI and suggest that chosen environments, activities and group facilitators should be considered in light of how they might affect a person’s recovery process and construction of identity. It may be valuable to access community-based settings for group programs for community-dwellers with ABI that better connect them to their local communities and normalise their ongoing community reintegration experience.
Environmental accommodations must also be considered. Chauhan et al.’s [Citation45] modified yoga program highlights how essential environment accommodations can be in setting up a group member’s successful participation in community occupations. The therapy role in group planning therefore, should always consider environmental adaptations in response to the unique needs of group participants, especially when therapy groups are being facilitated in community contexts and communal spaces.
Group facilitators are also key contributors to the group milieu. As so many articles indicated that participants valued the inclusion of group facilitators with a lived experience of brain injury, health care professionals should consider creating opportunities to co-design and co-facilitate groups with people with brain injury. This finding is consistent with current recognition that health services are more likely to address client need if the target population is involved in the design and delivery of health services[Citation103]. Health organisations, researchers, and therapists wishing to offer person-centred therapeutic groups should be embedding consumer involvement into every tier of their planning process. Payment of consumers with a lived experience of brain injury rather than utilising their willingness to volunteer, is also in keeping with current policies on consumer involvement [Citation104] and provides ABI survivors with another avenue into meaningful employment. This service shift may require funding bodies to incorporate consumer consultancy costs into their planning budget as well as flexibly exploring opportunities to employ users of their services in group-facilitation roles.
The qualitative review of articles highlighted key features of groups that participants perceived as beneficial. Group programs offered something very valuable that individual sessions did not, but this was contingent on both good design and facilitation of groups. This review suggests that groups need to create safe, inclusive environments before the full benefits of the group can be realised; a process that may take some time to develop. Most group programs reported in this review ran 6–12 weekly sessions, and this might not be enough time for the necessary group dynamic groundwork to be established. Given group dynamics appear to serve as a key ingredient in group-based interventions, future research is needed to explore the necessary duration to develop a safe and positive group environment with this population.
Notably participants reported on the central role their group membership played in the healing process following on from a difficult moment in their lives. Post-traumatic growth, described as the positive changes experienced following a traumatic event [Citation105], is considered an ideal long-term goal in the recovery journey, and involves people finding a means to accept and reframe their trauma as an impetus for personal growth [Citation106]. From participant responses, this process was supported by the social connections and comparisons with group members on their own recovery journey [Citation90], as well as the practical group activities that afforded them the opportunity to construct a new self-identity that was familiar, yet something new [Citation63]. Overwhelmingly it was the intrapersonal and interpersonal connections with other group members that was identified as the catalyst for this positive change. This may be sobering news for therapists who believe their therapeutic alliance is the key to group success. This scoping review suggests establishing a safe environment, influencing the group milieu and norms, and generating opportunities for people to engage in meaningful, enjoyable activities that build on skills and construct new social identities are important responsibilities of the facilitator, but these too can be shared with group members, to create a collectively co-designed group.
The scoping review reported on barriers and facilitating factors that make it easier or harder for group programs to be offered by services and taken up by community-dwellers with ABI. Barriers and facilitators were also explored more broadly in terms of participation, that being understood as attendance and involvement in life situations [Citation107]. Participants indicated access was the most significant barrier impacting their joining and staying in a group. Accessibility was impacted by too few groups being offered in their local communities (availability) or offered in settings that were too far from home that made it too effortful or costly to attend. Affordability was mentioned in several studies as a reason for participants not joining groups as were group programs not accommodating the needs of potential group members with activity choices, and group programs covering topics that participants did not feel ready to address (acceptability).
Affordability, accessibility, availability, accommodability and acceptability are recognised as environmental barriers that restrict community participation, making it both difficult for participants to “turn up” (attend), and stifling the development of accommodations and acceptances that would potentially improve involvement for everyone [Citation107,Citation108]. Irrespective of the type of group intervention, the multi-layered components of accessibility must be better considered when planning and delivering group programs. Groups continue to be developed with decisions made arguably in the best logistical interests of group providers and the limited resources available, rather than the specific needs of individuals, as evidenced by group programs set in medical environments instead of local community contexts, and content decisions made without consumer involvement. Participant friendly groups need to be affordable, accessible, available at a time and location easy to reach, and provide activities that are the right fit for participants at their stage in the recovery journey. Ensuring mechanisms for participant feedback are in place and allowing for some group agility to change content and activities in response to participant feedback is another recommendation for group developers.
Poncet et al.’s [Citation100] study also highlighted that some client priorities such as sexuality are not raised or addressed by therapists. Lynch and Fortune [Citation109] argue that sexuality is an inherent aspect of a person’s identity and should be better acknowledged and addressed by health professions. More work needs to be done to provide participants with opportunities to raise deeply personal goals that may become more important upon return to community living. Allowing consumer choice about education sessions to be covered by “guest speakers”, may provide an avenue for addressing unmet needs. While the reviewed articles didn’t raise gender or sex as a significant factor in their results, greater research may be warranted to ensure the appropriate gender mix is considered for group programs wishing to address sexuality.
This scoping review found service providers also face significant barriers to providing group programs; namely high costs and insufficient time to upskill facilitators and design and run groups under current funding systems. This is concerning, given the overwhelming benefits that can be experienced through well designed group programs. Several articles reported on group programs that mitigated some of these barriers by using volunteers and allied health students as group facilitators.
Six studies reported allied health students as group facilitators, allowing for higher facilitator-participant ratios in those group programs, as well as sufficient time allocated for both the planning of person/centred group activities and debriefing before and after implementing group sessions. Student-resourced service delivery models have emerged as an innovative placement model in which students learn professional skills and competencies while delivering part or all of the services to consumers [Citation110].
Student-resourced service delivery models have been used to great effect in providing well planned, person-centred groups in inpatient settings with ABI patients [Citation111]. For effective person-centred, student-resourced group programs to run in community settings with community-dwellers with ABI, work needs to be done to clarify funding pathways for such groups, and for partnerships to be established between universities seeking placement opportunities for their students and local community ABI service providers. Chinchai et al.’s [Citation46] intensive training of village health volunteers provides another example of creatively maximising resources to provide a meaningful community rehabilitative service.
Interprofessional co-facilitation of groups was strongly represented in articles reviewed (n = 20). Interprofessional collaboration allows groups to address several therapeutic goals in a group context, and potentially broaden the outcomes of group success [Citation112]. More specifically, this scoping review explored occupational therapy involvement in group design and facilitation, as well as occupation-centred practice principles utilised in the group context. Sixteen of the 70 articles described occupational therapy involvement in group design and facilitation, and 41 of the 70 articles explicitly described occupations contextually used in the group to address participant and group goals. Several participants indicated opportunities for growth came from involvement in therapeutic occupations within the group context. The collective participant narratives of experiencing transformative change through “doing occupation” supports what the profession of occupational therapy holds to be true; engagement in occupation is therapeutic [Citation10], and occupation-centred practice can bring substantial health and wellbeing benefits to individuals beyond a mere change in occupational performance.
This group context for considering occupation-centred practice aligns well with Nilsson et al.’s description of meaningful group occupation as being both activities which promote experiences of creativity and joy, and activities of transformation that extend existing skills and build capacity [Citation113]. Occupation-centred practice, that is, using meaningful occupations in the therapeutic process, is considered a cornerstone of occupational therapy practice and was a key feature in over half of the reported group programs, yet occupational therapy facilitation accounted for less than 23% of group facilitators. This poor representation begs the question; why aren’t more occupational therapists facilitating groups for community-dwellers with ABI? Further research into the perspectives of occupational therapists providing services to community-dwellers with ABI and perspectives of community-dwellers with ABI is recommended.
Limitations
This scoping review was limited by inconsistent terms used in articles to describe therapeutic groups. The decision to exclude groups designed for participants over 65 was made to avoid groups designed for older people with mild cognitive impairment and early-stage dementia, however it may have led to the exclusion of relevant articles. Excluding articles that discussed groups with only two participants, may have also led to the missing of relevant studies. Several retrieved articles did not report on key features the scoping review wished to explore. This may have confounded the key features which were discussed. The appraisal of qualitative studies recognised that several researchers were also involved in implementing the group program and consequently, there is significant risk of reporting bias. The study designs of retrieved articles were also not appraised, and while this is in keeping with recommended scoping review processes, it means that any conclusions reached within this review should be treated conservatively by readers.
Conclusions
This scoping review was conducted to map the characteristics of therapeutic groups currently run for community-dwellers with ABI. Seventy articles met the inclusion criteria, providing details of diverse groups delivered across the world that respond to the needs of community-dwellers in the chronic stage of ABI recovery. Interdisciplinary groups with a focus on improving participation are apparent. Participants reported the group milieu and therapeutic activities to be transformative in helping them adjust to community living post ABI. Challenges to accessing group programs include limited availability of groups and lack of accommodation of participants’ immediate needs. Service providers also have difficulty finding avenues to fund and adequately resource groups. Occupational therapists are under-represented in the reviewed studies despite their valuable contribution to occupation-centred practice, community participation and group facilitation in the community context. Recommendations of this scoping review include providing group programs outside of medical environments in authentic community settings and employing consumers to be part of group design and group facilitation. Student resourced group programs may offer opportunities for more group programs to be run. Further research into experiences of community-based ABI occupational therapists and group programs is warranted.
Authors contributions
The first author (CK) was responsible for writing the manuscript. All authors were involved in the third, fourth and fifth stage of the scoping review process. The second, third and fifth, authors were involved in editing the manuscript.
Supplemental Material
Download PDF (365.6 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Lucchesi LR, Agrawal S, Ahmadi A, et al. Global, regional, and national burden of traumatic brain injury and spinal cord injury, 1990–2016: a systematic analysis for the global burden of disease study 2016. Lancet Neurol. 2019;18(1):56–87. doi: 10.1016/S1474-4422(18)30415-0.
- Mitchell E, Ahern E, Saha S, et al. The value of nonpharmacological interventions for people with an acquired brain injury: a systematic review of economic evaluations. Value Health. 2022;25(10):1778–1790. doi: 10.1016/j.jval.2022.03.014.
- Domensino A-F, van Haastregt JCM, van Heugten CM. One-year follow-up results of a community-based treatment programme for people with acquired brain injury in the chronic phase. Disabil Rehabil. 2020;42(21):3106–3111. doi: 10.1080/09638288.2019.1582719.
- Maas AIR, Diaz-Arrastia R, Dreier JP, et al. Traumatic brain injury: integrated approaches to improve prevention, clinical care, and research. Lancet Neurol. 2017;16(12):987.
- Johnson CO, Nguyen M, Roth GA, et al. Global, regional, and national burden of stroke, 1990–2016: a systematic analysis for the global burden of disease study 2016. Lancet Neurol. 2019;18(5):439–458. doi: 10.1016/S1474-4422(19)30034-1.
- Goverover Y, Genova H, Smith A, et al. Changes in activity participation following traumatic brain injury. Neuropsychol Rehabil. 2017;27(4):472–485. 2017/05/19doi: 10.1080/09602011.2016.1168746.
- Perna R, Loughan AR, Talka K. Executive functioning and adaptive living skills after acquired brain injury. Appl Neuropsychol Adult. 2012;19(4):263–271. doi: 10.1080/09084282.2012.670147.
- Spalding K, Gustafsson L, Di Tommaso A. Occupation-based group programs in the inpatient hospital rehabilitation setting: a scoping review. Disabil Rehabil. 2022;44(10):2138–2148. doi: 10.1080/09638288.2020.1813818.
- Hammond FM, Barrett R, Dijkers MP, et al. Group therapy use and its impact on the outcomes of inpatient rehabilitation after traumatic brain injury: data from traumatic brain injury-practice based evidence project. Arch Phys Med Rehabil. 2015;96(8 Suppl):S282–92 e5. doi: 10.1016/j.apmr.2014.11.029.
- Kielhofner G. Conceptual foundations of occupational therapy practice, 4th ed. Philadelphia: F.A. Davis Co.; 2009.
- Sansonetti D, Nicks RJ, Unsworth C. Barriers and enablers to aligning rehabilitation goals to patient life roles following acquired brain injury. Aust Occup Ther J. 2018;65(6):512–522. doi: 10.1111/1440-1630.12492.
- Turner B, Ownsworth T, Cornwell P, et al. Reengagement in meaningful occupations during the transition from hospital to home for people with acquired brain injury and their family caregivers. Am J Occup Ther. 2009;63(5):609–620. doi: 10.5014/ajot.63.5.609.
- Nalder E, Fleming J, Cornwell P, et al. Reflections on life: experiences of individuals with brain injury during the transition from hospital to home. Brain Inj. 2013;27(11):1294–1303. doi: 10.3109/02699052.2013.823560.
- Morton MV, Wehman P. Psychosocial and emotional sequelae of individuals with traumatic brain injury: a literature review and recommendations. Brain Inj. 1995;9(1):81–92. doi: 10.3109/02699059509004574.
- Haslam C, Holme A, Haslam SA, et al. Maintaining group memberships: social identity continuity predicts well-being after stroke. Neuropsychol Rehabil. 2008;18(5-6):671–691. 2008/11/01doi: 10.1080/09602010701643449.
- Fleming J, Braithwaite H, Gustafsson L, et al. Participation in leisure activities during brain injury rehabilitation. Brain Inj. 2011;25(9):806–818. 1doi: 10.3109/02699052.2011.585508.
- McLean AM, Jarus T, Hubley AM, et al. Associations between social participation and subjective quality of life for adults with moderate to severe traumatic brain injury. Disabil Rehabil. 2014;36(17):1409–1418. doi: 10.3109/09638288.2013.834986.
- Kinsella EL, Muldoon OT, Fortune DG, et al. Collective influences on individual functioning: multiple group memberships, self-regulation, and depression after acquired brain injury. Neuropsychol Rehabil. 2020;30(6):1059–1073. doi: 10.1080/09602011.2018.1546194.
- Cruwys T, Dingle GA, Haslam C, et al. Social group memberships protect against future depression, alleviate depression symptoms and prevent depression relapse. Soc Sci Med. 2013;98:179–186. doi: 10.1016/j.socscimed.2013.09.013.
- Wilson A, Wills P, Pretorius C, et al. Cognitive rehabilitation groups: a thematic analysis of feasibility and perceived benefits for clients with moderate to severe traumatic brain injury living in the Western Cape. Afr J Disabil. 2015;4(1):175. doi: 10.4102/ajod.v4i1.175.
- Keegan LC, Murdock M, Suger C, et al. Improving natural social interaction: group rehabilitation after traumatic brain injury. Neuropsychol Rehabil. 2020;30(8):1497–1522. doi: 10.1080/09602011.2019.1591464.
- Alves-Stein S, George S, Lannin NA, et al. Implementation of a leisure reintegration programme for people with acquired brain injury in a community rehabilitation programme: a feasibility study. Brain Impairment. 2022;2022:1–13. doi: 10.1017/BrImp.2022.8.
- Poelke G, Ventura MI, Byers AL, et al. Leisure activities and depressive symptoms in older adults with cognitive complaints. Int Psychogeriatr. 2016;28(1):63–69. doi: 10.1017/S1041610215001246.
- Higgins S, Schwartzberg SL, Bedell G, et al. Current practice and perceptions of group work in occupational therapy. Am J Occup Ther. 2015;69(Supplement_1):6911510223p1. doi: 10.5014/ajot.2015.69S1-PO7096.
- Patterson F, Fleming J, Doig E. Group-based delivery of interventions in traumatic brain injury rehabilitation: a scoping review. Disabil Rehabil. 2016;38(20):1961–1986. 2016/09/24doi: 10.3109/09638288.2015.1111436.
- Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. doi: 10.1080/1364557032000119616.
- Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5(1):69–69. doi: 10.1186/1748-5908-5-69.
- Levack W, Tomori K, Takahashi K, et al. Development of an English-language version of a Japanese iPad application to facilitate collaborative goal setting in rehabilitation: a Delphi study and field test. BMJ Open. 2018;8(3):e018908. doi: 10.1136/bmjopen-2017-018908.
- Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–473. doi: 10.7326/M18-0850.
- Peters MDJ, Godfrey C, McInerney P, et al. Best practice guidance and reporting items for the development of scoping review protocols. JBI Evid Synth. 2022;20(4):953–968. doi: 10.11124/JBIES-21-00242.
- Rebeiro GK. & Lauckner, H. Promoting occupational participation with groups. In: Mary E, Gayle R, Egan M, Restall G, editors. Promoting occupational participation: collaborative relationship-focused occupational therapy: 10th Canadian occupational therapy guidelines. Rockland, Ontario: Canadian Association of Occupational Therapists; 2022. p. 169–197.
- Peters MDJ, Marnie C, Tricco AC, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Implement. 2021;19(1):3–10. doi: 10.1097/XEB.0000000000000277.
- Dam SL, Rhind DJA. The perceived benefits of community-based group exercise sessions for survivors of stroke. Int J Ther Rehabil. 2020;27(2):1–14. doi: 10.12968/ijtr.2016.0049.
- Donnelly KZ, Goldberg S, Fournier D. A qualitative study of LoveYourBrain yoga: a group-based yoga with psychoeducation intervention to facilitate community integration for people with traumatic brain injury and their caregivers. Disabil Rehabil. 2020;42(17):2482–2491. doi: 10.1080/09638288.2018.1563638.
- Norris M, Kilbride C, Mohagheghi A, et al. Exercise instructor-led functional training programme for community dwelling stroke survivors: a qualitative study…including commentary by jones TM and dean CM. Int J Ther Rehabil. 2013;20(12):597–605. doi: 10.12968/ijtr.2013.20.12.597.
- Niraj S, Wright S, Powell T. A qualitative study exploring the experiences of mindfulness training in people with acquired brain injury. Neuropsychol Rehabil. 2020;30(4):731–752. doi: 10.1080/09602011.2018.1515086.
- Attard MC, Loupis Y, Togher L, et al. The efficacy of an inter-disciplinary community aphasia group for living well with aphasia. Aphasiology. 2018;32(2):105–138. doi: 10.1080/02687038.2017.1381877.
- Attard MC, Loupis Y, Togher L, et al. Experiences of people with severe aphasia and spouses attending an interdisciplinary community Aphasia group. Disabil Rehabil. 2020;42(10):1382–1396. doi: 10.1080/09638288.2018.1526336.
- Batcho CS, Stoquart G, Thonnard J-L. Brisk walking can promote functional recovery in chronic stroke patients. J Rehabil Med. 2013;45(9):854–859. doi: 10.2340/16501977-1211.
- Bédard M, Felteau M, Marshall S, et al. Mindfulness-based cognitive therapy reduces symptoms of depression in people with a traumatic brain injury: results from a randomized controlled trial. J Head Trauma Rehabil. 2014;29(4):E13–E22. doi: 10.1097/HTR.0b013e3182a615a0.
- Bek J, Brown MR, Jutley-Neilson J, et al. Conductive education as a method of stroke rehabilitation: a single blinded randomised controlled feasibility study. Stroke Res Treatment. 2016;2016:1–6. doi: 10.1155/2016/5391598.
- Bonn MM, Dickey JP, Moran B, et al. Completing an interdisciplinary outpatient intervention improves patient rehabilitation goals following a mild traumatic brain injury. Physiother Theory Pract. 2023;39(2):310–316. doi: 10.1080/09593985.2021.2022046.
- Brenner LA, Braden CA, Bates M, et al. A health and wellness intervention for those with moderate to severe traumatic brain injury: a randomized controlled trial. J Head Trauma Rehabil. 2012;27(6):E57–E68. doi: 10.1097/HTR.0b013e318273414c.
- Caute A, Cruice M, Devane N, et al. Delivering group support for people with aphasia in a virtual world: experiences of service providers. Disabil Rehabil. 2022;44(26):8264–8282. doi: 10.1080/09638288.2021.2011436.
- Chauhan N, Zeller S, Donnelly KZ. Best practices for adapting and delivering community-based yoga for people with traumatic brain injury in the United States and Canada. Int J Yoga Therap. 2020;30(1):89–101. doi: 10.17761/2020-D-19-00055.
- Chinchai P, Sirisatayawong P, Jindakum N. Community integration and quality of life: stroke survivors as recipients of rehabilitation by village health volunteers (VHVs) in Thailand. Occup Ther Health Care. 2020;34(3):277–290. doi: 10.1080/07380577.2020.1773010.
- das Nair R, Lincoln NB. Evaluation of rehabilitation of memory in neurological disabilities (ReMiND): a randomized controlled trial. Clin Rehabil. 2012;26(10):894–903. doi: 10.1177/0269215511435424.
- das Nair R, Bradshaw LE, Day FE, et al. Clinical and cost effectiveness of memory rehabilitation following traumatic brain injury: a pragmatic cluster randomized controlled trial. Clin Rehabil. 2019;33(7):1171–1184. doi: 10.1177/0269215519840069.
- Donnelly KZ, Linnea K, Grant DA, et al. The feasibility and impact of a yoga pilot programme on the quality-of-life of adults with acquired brain injury. Brain Inj. 2017;31(2):208–214. doi: 10.1080/02699052.2016.1225988.
- Donnelly KZ, Baker K, Pierce R, et al. A retrospective study on the acceptability, feasibility, and effectiveness of LoveYourBrain Yoga for people with traumatic brain injury and caregivers. Disabil Rehabil. 2021;43(12):1764–1775. doi: 10.1080/09638288.2019.1672109.
- Driver S, Woolsey A. Evaluation of a physical activity behavior change program for individuals with a brain injury. Arch Phys Med Rehabil. 2016;97(9 Suppl):S194–S200. doi: 10.1016/j.apmr.2015.06.023.
- Driver S, Reynolds M, Kramer K. Modifying an evidence-based lifestyle programme for individuals with traumatic brain injury. Brain Inj. 2017;31(12):1612–1616. doi: 10.1080/02699052.2017.1346286.
- Driver S, Reynolds M, Woolsey A, et al. Impact of a community-based healthy lifestyle program on individuals with traumatic brain injury. J Head Trauma Rehabil. 2018;33(6):E49–E58. doi: 10.1097/HTR.0000000000000372.
- English K, Daley B, Cahill L, et al. Characteristics and outcomes of a community upper limb rehabilitation group for adult stroke survivors in Australia: a pre-post cohort study. Occup Ther Health Care. 2022;36(4):440–458. doi: 10.1080/07380577.2021.2012734.
- Evald L. Prospective memory rehabilitation using smartphones in patients with TBI. Disabil Rehabil. 2018;40(19):2250–2259. doi: 10.1080/09638288.2017.1333633.
- George S, Barr C, Berndt A, et al. Effects of the carfreeme traumatic injuries, a community mobility group intervention, to increase community participation for people with traumatic injuries: a randomized controlled trial with crossover. Front Neurol. 2022;13:821195–821195. doi: 10.3389/fneur.2022.821195.
- Gerber GJ, Gargaro J. Participation in a social and recreational day programme increases community integration and reduces family burden of persons with acquired brain injury. Brain Inj. 2015;29(6):722–729. doi: 10.3109/02699052.2015.1004745.
- Givon N, Zeilig G, Weingarden H, et al. Video-games used in a group setting is feasible and effective to improve indicators of physical activity in individuals with chronic stroke: a randomized controlled trial. Clin Rehabil. 2016;30(4):383–392. doi: 10.1177/0269215515584382.
- Harel-Katz H, Adar T, Milman U, et al. Examining the feasibility and effectiveness of a culturally adapted participation-focused stroke self-management program in a day-rehabilitation setting: a randomized pilot study. Top Stroke Rehabil. 2020;27(8):577–589. doi: 10.1080/10749357.2020.1738676.
- Hawley L, Morey C, Sevigny M, et al. Enhancing self-advocacy after traumatic brain injury: a randomized controlled trial. J Head Trauma Rehabil. 2022;37(2):114–124. doi: 10.1097/HTR.0000000000000689.
- Jones JP, Drass JM, Kaimal G. Art therapy for military service members with post-traumatic stress and traumatic brain injury: three case reports highlighting trajectories of treatment and recovery. Arts Psychother. 2019;63:18–30. doi: 10.1016/j.aip.2019.04.004.
- Lee D, Fischer H, Zera S, et al. Examining a participation-focused stroke self-management intervention in a day rehabilitation setting: a quasi-experimental pilot study. Top Stroke Rehabil. 2017;24(8):601–607. doi: 10.1080/10749357.2017.1375222.
- Lexell EM, Alkhed A-K, Olsson K. The group rehabilitation helped me adjust to a new life: experiences shared by persons with an acquired brain injury. Brain Inj. 2013;27(5):529–537. doi: 10.3109/02699052.2013.765598.
- Liu-Ambrose T, Eng JJ. Exercise training and recreational activities to promote executive functions in chronic stroke: a proof-of-concept study. J Stroke Cerebrovasc Dis. 2015;24(1):130–137. doi: 10.1016/j.jstrokecerebrovasdis.2014.08.012.
- Mandehgary Najafabadi M, Azad A, Mehdizadeh H, et al. Improvement of upper limb motor control and function after competitive and noncompetitive volleyball exercises in chronic stroke survivors: a randomized clinical trial. Arch Phys Med Rehabil. 2019;100(3):401–411. doi: 10.1016/j.apmr.2018.10.012.
- Marshall J, Devane N, Talbot R, et al. A randomised trial of social support group intervention for people with aphasia: a novel application of virtual reality. PLoS One. 2020;15(9):e0239715. doi: 10.1371/journal.pone.0239715.
- Mayo NE, Anderson S, Barclay R, et al. Getting on with the rest of your life following stroke: a randomized trial of a complex intervention aimed at enhancing life participation post stroke. Clin Rehabil. 2015;29(12):1198–1211. doi: 10.1177/0269215514565396.
- Miller LA, Radford K. Testing the effectiveness of group-based memory rehabilitation in chronic stroke patients. Neuropsychol Rehabil. 2014;24(5):721–737. doi: 10.1080/09602011.2014.894479.
- Mitchell EJ, Veitch C, Passey M. Efficacy of leisure intervention groups in rehabilitation of people with an acquired brain injury. Disabil Rehabil. 2014;36(17):1474–1482. doi: 10.3109/09638288.2013.845259.
- Nayak P, Mahmood A, Kumaran D S, et al. Adaptive sports for promoting physical activity in community-dwelling adults with stroke: a feasibility study. J Bodyw Mov Ther. 2021;28:341–347. doi: 10.1016/j.jbmt.2021.07.004.
- Nemeth DG, Songy C, Olivier TW. Increasing success in neurocognitively impaired patients through group therapy. Int J Group Psychother. 2015;65(1):125–133. doi: 10.1521/ijgp.2015.65.1.125.
- Nicholas M, Pittmann R, Pennington S, et al. Outcomes of an interprofessional intensive comprehensive aphasia program’s first five years. Top Stroke Rehabil. 2022;29(8):588–604. doi: 10.1080/10749357.2021.1970452.
- Perez-Rodriguez M, Garcia-Gomez S, Coteron J, et al. Physical activity and sport for acquired brain injury (PASABI): a non-randomized controlled trial. Medicina. 2021;57(2):122. doi: 10.3390/medicina57020122.
- Poncet F, Pradat-Diehl P, Lamontagne M-E, et al. Participant and service provider perceptions of an outpatient rehabilitation program for people with acquired brain injury. Ann Phys Rehabil Med. 2017;60(5):334–340. doi: 10.1016/j.rehab.2017.03.010.
- Radford K, Lah S, Thayer Z, et al. Improving memory in outpatients with neurological disorders using a group-based training program. J Int Neuropsychol Soc. 2012;18(4):738–748. doi: 10.1017/S1355617712000379.
- Rand D, Givon N, Avrech Bar M. A video-game group intervention: experiences and perceptions of adults with chronic stroke and their therapists. Can J Occup Ther. 2018;85(2):158–168. doi: 10.1177/0008417417733274.
- Raukola-Lindblom M, Elina V, Riitta V. Recovering social participation – experience with a relational group intervention for traumatic brain injury patients. NeuroRehabilitation. 2020;47(1):55–64. doi: 10.3233/NRE-203083.
- Reynolds M, Driver S, Bennett M. The social network – using social media to support individuals with traumatic brain injury participating in a pilot study weight-loss program. Brain Inj. 2018;32(12):1450–1454. doi: 10.1080/02699052.2018.1496480.
- Rotherham A, Howe T, Tillard G. We just thought that this was Christmas: perceived benefits of participating in aphasia, stroke, and other groups. Aphasiology. 2015;29(8):965–982. doi: 10.1080/02687038.2015.1016887.
- Salas C, Casassus M, Rowlands L, et al. Developing a model of long-term social rehabilitation after traumatic brain injury: the case of the head forward Centre. Disabil Rehabil. 2021;43(23):3405–3416. doi: 10.1080/09638288.2020.1741697.
- Shany-Ur T, Bloch A, Salomon-Shushan T, et al. Efficacy of postacute neuropsychological rehabilitation for patients with acquired brain injuries is maintained in the long-term. J Int Neuropsychol Soc. 2020;26(1):130–141. doi: 10.1017/S1355617719001024.
- Song R, Park M, Jang T, et al. Effects of a tai chi-based stroke rehabilitation program on symptom clusters, physical and cognitive functions, and quality of life: a randomized feasibility study. Int J Environ Res Public Health. 2021;18(10):5453. doi: 10.3390/ijerph18105453.
- Stephens JA, Van Puymbroeck M, Sample PL, et al. Yoga improves balance, mobility, and perceived occupational performance in adults with chronic brain injury: a preliminary investigation. Complement Ther Clin Pract. 2020;40:101172. doi: 10.1016/j.ctcp.2020.101172.
- Tamplin J, Baker FA, Jones B, et al. Stroke a Chord’: the effect of singing in a community choir on mood and social engagement for people living with aphasia following a stroke. NeuroRehabilitation. 2013;32(4):929–941. doi: 10.3233/NRE-130916.
- Tielemans NS, Schepers VPM, Visser-Meily JMA, et al. Process evaluation of the Restore4stroke self-management intervention ‘plan ahead!’: a stroke-specific self-management intervention [article. Clin Rehabil. 2016;30(12):1175–1185. doi: 10.1177/0269215515620255.
- Towfighi A, Cheng EM, Hill VA, et al. Results of a pilot trial of a lifestyle intervention for stroke survivors: healthy eating and lifestyle after stroke. J Stroke Cerebrovascular Diseases. 2020;29(12):105323.
- Vestri A, Peruch F, Marchi S, et al. Individual and group treatment for patients with acquired brain injury in comprehensive rehabilitation. Brain Inj. 2014;28(8):1102–1108. doi: 10.3109/02699052.2014.910698.
- Vikane E, Hellstrøm T, Røe C, et al. Multidisciplinary outpatient treatment in patients with mild traumatic brain injury: a randomised controlled intervention study. Brain Inj. 2017;31(4):475–484. doi: 10.1080/02699052.2017.1280852.
- Visser MM, Heijenbrok-Kal MH, Van’t Spijker A, et al. Problem-solving therapy during outpatient stroke rehabilitation improves coping and health-related quality of life: randomized controlled trial. Stroke. 2016;47(1):135–142. (00392499)doi: 10.1161/STROKEAHA.115.010961.
- White BP. Exploring participant perceptions of a community-based program for people with brain injury. OTJR. 2020;40(4):245–252. doi: 10.1177/1539449220915853.
- Wijekoon S, Wilson W, Gowan N, et al. Experiences of occupational performance in survivors of stroke attending peer support groups. Can J Occup Ther. 2020;87(3):173–181. doi: 10.1177/0008417420905707.
- Withiel TD, Wong D, Ponsford JL, et al. Comparing memory group training and computerized cognitive training for improving memory function following stroke: a phase II randomized controlled trial. J Rehabil Med. 2019;51(5):343–351. doi: 10.2340/16501977-2540.
- Withiel TD, Stolwyk RJ, Ponsford JL, et al. Effectiveness of a manualised group training intervention for memory dysfunction following stroke: a series of single case studies. Disabil Rehabil. 2020;42(21):3033–3042. doi: 10.1080/09638288.2019.1579260.
- Wolf TJ, Baum CM, Lee D, et al. The development of the improving participation after stroke self-management program (IPASS): an exploratory randomized clinical study. Top Stroke Rehabil. 2016;23(4):284–292. doi: 10.1080/10749357.2016.1155278.
- Wong D, Kempnich C, Bradshaw J, et al. Real world implementation of a group-based memory rehabilitation program into stroke services: a knowledge translation evaluation. Top Stroke Rehabil. 2021;28(6):410–421. doi: 10.1080/10749357.2020.1838084.
- Xie G, Rao T, Lin L, et al. Effects of Tai Chi Yunshou exercise on community-based stroke patients: a cluster randomized controlled trial. Eur Rev Aging Phys Act. 2018;15(1):17. doi: 10.1186/s11556-018-0206-x.
- Xu T, Clemson L, O’Loughlin K, et al. Stepping on after stroke falls-prevention programme for community stroke survivors in Singapore: a feasibility study. Br J Occup Ther. 2021;84(6):366–375. doi: 10.1177/0308022620946640.
- Yeates G, Murphy M, Baldwin J, et al. A pilot participant perceptions of a community of acquired brain injury in a community setting. bpscpf. 2015;1(267):46–51. doi: 10.53841/bpscpf.2015.1.267.46.
- Zoerink DA, Carter MJ. A case report of a physical activity intervention for adults with stroke enhancing balance and functional fitness through golf. Ther Recreat J. 2015;49(3):238–252.
- Poncet F, Swaine B, Migeot H, et al. Effectiveness of a multidisciplinary rehabilitation program for persons with acquired brain injury and executive dysfunction. Disabil Rehabil. 2018;40(13):1569–1583. doi: 10.1080/09638288.2017.1300945.
- Rauch A, Scheel-Sailer A. Applying the international classification of functioning, disability and health to rehabilitation goal setting. In: Siegert RJ, Levack WMM, editors. Rehabilitation goal setting: theory, practice and evidence. Baton Rouge, USA: Taylor & Francis Group; 2014. p. 161–180.
- Tracey Karlovits MAM. Coping with community reintegration after severe brain injury: a description of stresses and coping strategies. Brain Injury. 1999;13(11):845–861.
- Greenhalgh T, Robert G, Macfarlane F, et al. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q. 2004;82(4):581–629. doi: 10.1111/j.0887-378X.2004.00325.x.
- Care ACoSaQiH. Safety and Quality Improvement Guide Standard 2: partnering with Consumers. 2012. Available from: https://www.safetyandquality.gov.au/standards/nsqhs-standards/partnering-consumers-standard.
- Lyon I, Fisher P, Gracey F. “Putting a new perspective on life”: a qualitative grounded theory of posttraumatic growth following acquired brain injury. Disabil Rehabil. 202143(22):3225–3233. doi: 10.1080/09638288.2020.1741699.
- Tedeschi RG, Calhoun LG. Posttraumatic growth: conceptual foundations and empirical evidence. Psycholog Inquiry. 2004;15(1):1–18. doi: 10.1207/s15327965pli1501_01.
- Imms C, Granlund M. Participation: are we there yet. Aust Occup Ther J. 2014;61(5):291–292. doi: 10.1111/1440-1630.12166.
- Maxwell G, Alves I, Granlund M. Participation and environmental aspects in education and the ICF and the ICF-CY: findings from a systematic literature review. Dev Neurorehabil. 2012;15(1):63–78. doi: 10.3109/17518423.2011.633108.
- Lynch C, Fortune T. Applying an occupational lens to thinking about and addressing sexuality. Sex Disabil. 2019;37(2):145–159. doi: 10.1007/s11195-019-09566-7.
- Wynne D, Cooper K. Student-led rehabilitation groups and clinics in entry-level health education: a scoping review. JBI Evid Synth. 2021;19(11):2958–2992. doi: 10.11124/JBIES-20-00340.
- Patterson F, Doig E, Fleming J, et al. Student-resourced service delivery of occupational therapy rehabilitation groups: patient, clinician and student perspectives about the ingredients for success. Disabil Rehabil. 2022;44(18):5329–5340. doi: 10.1080/09638288.2021.1922517.
- Waldron-Perrine B, Mudar R, Mashima P, et al. Interprofessional collaboration and communication to facilitate implementation of cognitive rehabilitation in persons with brain injury. J Interprof Care. 2022;36(4):529–537. doi: 10.1080/13561820.2021.1971956.
- Nilsson I, Nygåård L. Geriatric rehabilitation: elderly clients’ experiences of a pre-discharge occupational therapy group programme. Scand J Occup Ther. 2003;10(3):107–117. doi: 10.1080/11038120310016418.