Abstract
Purpose
Self-efficacy and resilience are important for various aspects of rehabilitation outcome after stroke. However, little is known about how these factors are affected and related to communication outcome in stroke survivors with aphasia. The purpose was to investigate self-efficacy and resilience, and associations to language and functional communication, in people with severe post-stroke aphasia.
Materials and methods
37 participants with severe aphasia rated their self-efficacy and resilience, using adapted versions of the existing instruments DLSES and CD-RISC. In addition, linguistic ability, executive function and functional communication were assessed.
Results
Participants rated their self-efficacy and resilience as expected based on reports in the literature; somewhat lower than general populations and at similar levels as clinical populations. There were no association between self-efficacy, resilience and linguistic ability. In the sample as a whole, there were no associations between self-efficacy, resilience and functional communication. However, when results were stratified by executive function, associations emerged in the group with stronger executive function.
Conclusions
People with severe aphasia have decreased self-efficacy and resilience compared to general populations, but not necessarily in proportion to their language impairment. Among participants with relatively spared executive functions there were indications of an association between self-efficacy, resilience and functional communication.
IMPLICATIONS FOR REHABILITATION
The constructs self-efficacy and resilience are related to several outcomes after stroke.
Self-efficacy and resilience can be assessed in many people with severe aphasia, provided that materials and administration procedure are adequately adapted.
There are indications of an association between functional communication and self-efficacy and resilience.
Integrating activities to increase self-efficacy and resilience in aphasia rehabilitation may be beneficial to treatment outcomes regarding functional communication.
Introduction
Approximately one third of stroke patients acquire aphasia [Citation1,Citation2], a language disorder caused by damage to the brain areas responsible for language processing [Citation3]. The term aphasia refers to impairments of expression and comprehension of spoken and written language. In severe aphasia, the residual language abilities are insufficient to meet the communicative needs of the individual, and alternative modes of communication (such as facial expression, gesture, drawing, and communication aids) must be employed [Citation4,Citation5]. To communicate using an insufficient language system is challenging; most people with severe aphasia (PWSA) experience frequent communication breakdowns which may result in frustration and a reluctance to engage in social interactions. Communication problems can cause social isolation and loss of autonomy [Citation6–10].
Functional communication is the process of “getting messages across in a variety of ways ranging from fully formed grammatical sentences to appropriate gestures” [Citation11]. There are considerable individual differences in the functional communication ability of PWSA, and linguistic ability alone does not account for all the variation. Several other factors have been found to play a crucial role for communication success, such as non-verbal cognition [Citation12–14], and the attitudes, skill and knowledge of the communication partner [Citation15]. Thus, when striving to understand and improve functional communication in severe aphasia, it is necessary to explore all potential factors that might be exploited to enhance the individual’s participation in communicative life [Citation16], particularly those that could be targeted in the intervention.
In search of such factors, we can use the model developed by Janice Light and colleagues, describing communicative competence in people who need augmentative and alternative communication [Citation17,Citation18]. According to this model, communicative competence is impacted by individual psychosocial factors such as motivation, attitude, confidence, and resilience. Motivation provides the drive to communicate, the attitude towards alternative means of communication dictates the willingness to use them, the confidence determines the propensity to attempt to communicate in a given situation and the resilience influences whether the individual will persevere with communication attempts despite challenges and failures. The importance of similar personal factors has also been highlighted in the Living with Aphasia: Framework for Outcome Measurement (A-FROM, [Citation19]).
The present study focuses on two of the individual psychosocial factors suggested by Light and colleagues [Citation17,Citation18]; confidence and resilience. We will, however, operationalise confidence as the more specific construct self-efficacy. Light and colleagues [Citation17,Citation18] describe confidence in this context as a person’s “self-assurance that he or she can communicate successfully in the given situation” [Citation18, p.4], that is; an individual’s belief in his/her abilities to succeed in a specific situation. This description is more or less identical to what is encompassed in the construct self-efficacy. This construct also has the advantage of being based within a comprehensive theory, Social Cognitive Theory [Citation20], which may provide suggestions for intervention.
In addition to the potential importance for functional communication, both self-efficacy and resilience have previously been shown to be associated with various outcomes in populations with acquired brain injury. In a systematic review, Korpershoek et al. [Citation21] conclude that self-efficacy is positively related to quality of life in both the short and long term after stroke. Several studies have found associations between self-efficacy and post-stroke depression. For instance, Volz and colleagues [Citation22,Citation23] found signs of early post-stroke depression to be related to a decrease in self-efficacy. In a longitudinal study over five years, they also found indications that decreased self-efficacy may be a driving force for post-stroke depression [Citation23]. Resilience has been shown to be an independent predictor of quality of life after stroke [Citation24]. Such findings further accentuate the need to investigate the constructs self-efficacy and resilience in PWSA, which is a population with a documented high risk of developing post-stroke depression [Citation25–27] and suffer low quality of life [Citation28,Citation29].
Self-efficacy
Self-efficacy, a construct originating from Social Cognitive Theory [Citation20], is defined as “beliefs in one’s capabilities to organize and execute courses of action required to produce given attainments” [Citation30]. It is considered to be activity- or domain specific, rather than a general attribute [Citation30]. Self-efficacy influences motivation and behaviour by determining the goals individuals set for themselves, and the amount of effort they invest to achieve these goals [Citation31]. If a person does not believe it is within their ability to perform a certain behaviour or task, they are unlikely to attempt it [Citation30]. Self-efficacy has been found to be associated with various outcomes after stroke, such as ADL, quality of life, and depression [Citation21,Citation23,Citation32–34], and there is a risk that self-efficacy decreases over time post-stroke [Citation35]. There are indications that interventions designed to increase self-efficacy can have a positive effect on rehabilitation outcome [Citation32,Citation33,Citation36].
To the best of our knowledge there are no studies specifically about self-efficacy and aphasia. There are, however, studies involving closely related concepts. Bakheit et al. [Citation37] investigate self-esteem in people with aphasia, using the Visual Analogue Self-Esteem Scale developed by Brumfitt and Sheeran [Citation38]. Bakheit et al. [Citation37] found that self-esteem does not seem to be related to linguistic ability. Self-esteem is a concept related to “the extent to which one approves of and likes oneself” [Citation38, p. 387], and thus differs from self-efficacy. Babbitt and Cherney [Citation6] propose the construct communication confidence, and developed an instrument for measuring this; the Communication Confidence Rating Scale for Aphasia (CCRSA) [Citation6,Citation39,Citation40]. The CCRSA was used in a study by Plourde et al. [Citation41], and the results suggest that communication confidence can be improved by participation in a group activity. In the way the term confidence is used by Babbitt and Cherney [Citation6], it is more or less synonymous with self-efficacy. Self-management is another construct closely related to self-efficacy, which is just beginning to be studied in the aphasia field [Citation42–44]. Self-management is an established construct in rehabilitation and refers to a patient taking an active part and responsibility in managing life with a chronic condition, and self-efficacy is thought to be a central component of this. However, in a scoping review, Nichol et al. [Citation42] found that structured self-management approaches are rarely used in aphasia rehabilitation.
Resilience
Resilience can be described as “the process of effectively negotiating, adapting to, or managing significant sources of stress or trauma” [Citation45]. Resilience has often been studied in the context of children growing up under challenging conditions [Citation46], while in the adult population resilience is often studied in the context of loss and of traumatic events [Citation47]. Thus, resilience can be studied in relation to both sudden and long-term challenges. In stroke survivors, both temporal aspects are relevant since there is both the sudden event of the stroke and the long-term challenge of living with a chronic condition [Citation48,Citation49].
Strong resilience is associated with successful adjustment, more participation, and less depressive symptoms in several rehabilitation populations, such as spinal cord injury, multiple sclerosis, traumatic brain injury, and stroke [Citation50–52]. In addition, high resilience is reported to be associated with better cognitive function as well as greater recovery of cognitive function in individuals with traumatic brain injury and stroke [Citation53]. In studies of interventions designed to strengthen resilience in various clinical populations, there are indications that it is feasible. However, the research about resilience is somewhat hampered by a lack of consensus regarding the definition of the construct [Citation24,Citation54].
Hunting Pompon et al. [Citation55] assessed resilience in a study of chronic stress in aphasia and found that lower levels of resilience were associated with higher levels of stress. Cangi et al. [Citation56] found that higher resilience scores were associated with less depression in a small sample of people with aphasia. In a qualitative study, Moss et al. [Citation57] found connections between resilience and psychosocial adjustment to stroke and aphasia. However, little is known about whether there is a relationship between resilience and functional outcome in aphasia [Citation58].
Self-efficacy and resilience are distinct but interconnected constructs. Self-efficacy has been described as a defining attribute of resilience. With a strong self-efficacy for a certain activity, the individual is likely to persevere longer in the face of adversity [Citation59].
Measurement of self-efficacy and resilience
Assessment of highly subjective constructs, such as self-efficacy and resilience, is challenging in PWSA, due to the communication impairment. In addition, when considering concepts representing the individuals’ own views about themselves and their lives, there is no objective “truth” against which to validate the responses [Citation60]. Even though impaired language comprehension is a major barrier, several recent studies have shown that with proper adaptation of material and administration procedure, people with aphasia can provide reliable responses to self-report instruments [Citation61–63]. However, these studies frequently include all severity levels of aphasia, which means there are few participants with severe aphasia. For example, in the study of a minimum level of language comprehension required for a quality-of-life questionnaire [Citation62] the lowest reported language comprehension score, even though low, was above scores that might be expected with some PWSA. Thus, when focusing on severe aphasia, special care needs to be taken regarding the adaptation of instruments.
Furthermore, cognition is crucial to the forming of self-efficacy beliefs and resilience [Citation30,Citation64]. Self-efficacy beliefs are based on several sources of information; the individual’s own experience, vicarious experience, evaluations of contextual factors, and estimations of task demands. The forming of self-efficacy beliefs rests on perception, memory, and cognitive processing of this information. Individuals with impairments of such functions may have difficulty forming adequate and realistic self-efficacy beliefs [Citation30]. Parker et al. [Citation65] demonstrate that correlations between health-related self-efficacy and functional independence are stronger in stroke survivors with mild or no cognitive impairment, as opposed to those with moderate to severe cognitive impairment. These results are assumed to reflect that individuals with more intact cognitive functioning can form more realistic self-efficacy beliefs [Citation65], and as a consequence there is a stronger association between self-efficacy and functioning in that group. Parsons et al. [Citation64] propose a cognitive model of resilience in which executive control is a crucial part. Similar to self-efficacy, resilience is likely to be dependent on executive control and cognitive flexibility.
In conclusion, self-efficacy and resilience are related to a number of outcomes in stroke and other populations with brain injury, and there are indications that self-efficacy and resilience can be specifically targeted in intervention. Unfortunately, we have little knowledge about these constructs in PWSA. There is, based on the model by Light and colleagues [Citation17,Citation18], reason to assume that self-efficacy and resilience have an impact on functional communication. Thus, the study of these factors in the aphasia population is highly warranted. Simultaneously, the challenges of measurement must be taken into consideration and explored.
Aim
The aim of the present study was to gather knowledge about the psychosocial factors self-efficacy and resilience, and their relation to linguistic ability and functional communication, in people with severe post-stroke aphasia. The specific research questions were:
How do people with severe post-stroke aphasia rate their self-efficacy and resilience, and is there an association between the two?
Is there an association between linguistic ability and self-reported self-efficacy or resilience in people with severe post-stroke aphasia?
Is there an association between functional communication and self-reported self-efficacy or resilience in people with severe post stroke aphasia?
Does executive function influence the relationship between functional communication and self-efficacy and/or resilience?
Method
We performed an exploratory, cross-sectional study. Linguistic ability, functional communication, executive function, self-efficacy and resilience were assessed in a sample of people with severe post-stroke aphasia.
Participants
The study was conducted in Sweden. PWSA were recruited via speech-language pathologists, the Aphasia Association, and a Folk high school which organises courses for people with aphasia. This study was part of a larger project and the procedure for recruitment and informed consent has been described in detail in Olsson et al. [Citation12]. The study was approved by the Regional Ethical Review Board of Uppsala, Dnr 2017/183.
The inclusion criteria were:
Severe aphasia (≤2 on Aphasia Severity Rating Scale from The Boston Diagnostic Aphasia Examination [Citation66]) secondary to stroke, at least 6 months post onset.
Comprehensive Aphasia Test language comprehension score ≥ 32 (see further description below).
Adequate vision, hearing and cognitive function to complete the Comprehensive Aphasia Test.
No reported history of cognitive disorder pre-stroke
Access to a significant other (family member, friend or professional care giver) who was willing to complete a questionnaire about communicative effectiveness.
Material
Linguistic ability
Comprehensive aphasia Test (CAT)
Linguistic ability was assessed with the Swedish adaptation of the Comprehensive Aphasia Test (CAT) [Citation67]. The language battery in CAT covers comprehension and production of spoken and written language. In the results section two composite scores will be presented; the total score for the entire language battery as a measure of general linguistic ability, and the language comprehension score, since it is of particular interest for the inclusion of participants, as will be described below.
Executive function
Cognitive linguistic quick Test (CLQT)
Executive functions were assessed as a measure of cognitive functions involved in forming self-efficacy beliefs and resilience [Citation30,Citation64,Citation65].
CLQT [Citation68] is a test battery intended for screening of cognition and language. It is developed to be used in populations with communication disorders and to be administered by speech-language pathologists. Test-retest reliability has been shown to be good. For this study, four CLQT-tasks targeting executive functions while posing minimal linguistic demands were selected: Symbol cancellation, Symbol trails, Mazes, and Design generation. These tasks cover executive functions such as attention, inhibition, working memory, planning, mental flexibility, anticipating problems, ability to vary responses, and self-monitoring [Citation68,Citation69].
Functional communication
Scenario test
The Scenario Test uses a role play format to assess functional communication ability in severe aphasia [Citation70]. The investigator acts as a benevolent communication partner. All modes of communication (speech, writing, drawings, gestures, communication aids etc.) are accepted. Maximum score is possible to obtain for a skilled communicator even in the absence of verbal output. The Scenario Test has been evaluated and found to have good validity and reliability [Citation70].
Communicative effectiveness index (CETI)
CETI is a questionnaire completed by a significant other and is designed to assess the communicative effectiveness of the person with aphasia [Citation71]. The CETI uses 100 mm visual analogue scales, where the significant other is asked to indicate the performance of the PWA in 16 everyday communicative situations or actions. The end points of the scale are “Not able at all” and “As able as before the stroke”.
Self-efficacy
Daily living self-efficacy scale (DLSES)
DLSES is a 12-item questionnaire developed to measure self-efficacy in stroke survivors [Citation72,Citation73]. It comprises two subscales: self-efficacy for psychosocial functioning (DLSES PS, 8 items, of which at least 5 represent activities that are highly dependent on communication) and self-efficacy for activities of daily living (DLSES ADL, 4 items). The DLSES has good psychometric properties among stroke survivors and normal controls [Citation72,Citation73]. It is designed as a questionnaire with a Likert scale of 10-unit intervals from 0 (=cannot do at all) to 100 (=highly certain can do). A mean score is calculated for the entire instrument and for the two subscales. The questionnaire is intended to be completed independently by the stroke survivor. This format for administration excludes a large proportion of stroke survivors with aphasia. Therefore, for this study the questionnaire and administration procedure were adapted to the needs of PWSA [Citation60,Citation74]. The items were translated into Swedish by the first author (with permission from A. Maujean). The translation was reviewed by the second and third author in addition to a naïve assessor, and adjusted accordingly. A visual support for the Likert scale was created to facilitate response by pointing. Pictures to illustrate the content of each item were created using a Swedish online picture resource [Citation75]. For an example from the adapted DLSES material, see . Descriptions, rephrasings and examples to further clarify the intention of the items were prepared, to be used as needed during administration in order to optimise comprehension of the items.
Figure 1. Example from adapted version of DLSES, here in original English wording (pictures from www.bildstod.se).
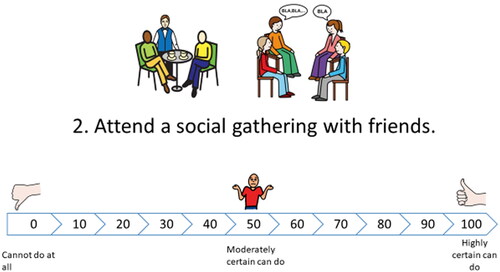
Self-efficacy of communication (SEC)
Several of the items in DLSES concern activities that are likely to be affected by communication disorders, but does not specifically target communication. Thus, five additional items were created for this study, in the same format as the DLSES. The items are listed in , an example is presented in .
Figure 2. Example from SEC, translated from Swedish (pictures from www.bildstod.se).
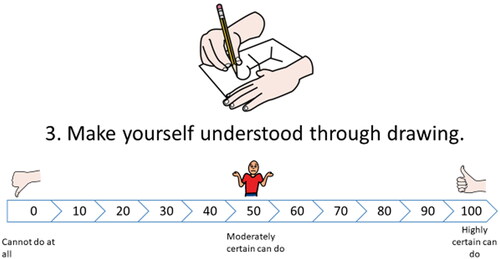
Table 1. SEC items, translated from Swedish.
Resilience
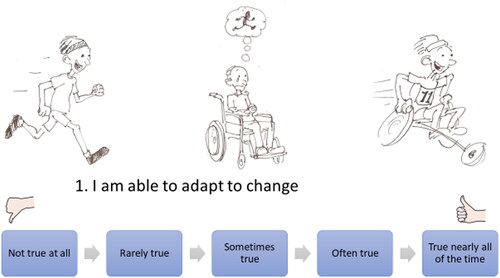
Connor-Davidson resilience scale (CD-RISC)
The CD-RISC [Citation76,Citation77] is a 25 item self-rating scale for adults. It consists of statements that are rated on a five step Likert scale from “not true at all” to “true nearly all the time”, quantified into 0-4 points which are added up to give a total score. A higher score indicates stronger resilience. There is also a shorter, 10-item version, developed based on factor analysis of the original 25-item version [Citation78]. This shorter scale was preferred for the present study in order to reduce the demands on the participants. CD-RISC is considered to be psychometrically sound for use in an older population (over 60) [Citation79]. For the present study, an approved Swedish translation was used. As with DLSES, adaptation of the material was needed. Again, a visual support was created for the assessment. The concepts to be rated in CD-RISC are often complex. An artist was engaged to create illustrations that would convey the general idea and/or an example of the item. The artist and the first author developed the pictures in collaboration. The second and third authors reviewed and approved the pictures. See for an example. As with DLSES, descriptions, rephrasings and examples to clarify the intention of the items were prepared.
Figure 3. Example from adapted CD-RISC, here in original English wording.
Procedure
All assessments were conducted by the first author over 2-4 sessions, depending on the time required and the stamina of the participant. Each session typically lasted about one hour, including small talk and breaks. The distribution of assessments over the sessions differed somewhat between the participants but the overall order remained the same: CAT, DLSES, SEC, CLQT, Scenario Test, CD-RISC. Data for additional studies were collected at the same time, a detailed record of the procedure has been reported in Olsson et al. [Citation12].
The adapted procedure for completion of DLSES, SEC, and CD-RISC was as follows: The overall aim of the particular assessment was explained and the scale steps were read aloud and supported with gestures. For DLSES an example was given, where the investigator rated her self-efficacy for two different activities while briefly accounting for her thought process, to illustrate the end points of the scale. When the procedure was thus established, the page with the item text, picture, and response scale was placed in front of the participant. The investigator read the item text aloud and reinforced the content as needed (pointing to the picture, using gestures, rephrasing, and giving examples). For both DLSES and CD-RISC, the investigator used the prepared descriptions, rephrasings, and examples, but departed from those when deemed necessary in response to the needs of the participant. The clarification of the content of the item was continued until the participant was perceived to have understood the item. The scale steps were repeated as often as needed. All assessments were video recorded.
For each PWSA a significant other (family member, close friend or professional care giver) completed the CETI.
Data analysis
All statistical analyses were performed with IBM SPSS Statistics version 26.
37 participants were included in the final statistical analyses.
Variables were inspected for missing values. For DLSES, there were two participants with one missing value and two participants with two missing values. One participant did not complete SEC, thus for SEC n = 36. A further two participants had one missing value each on SEC. One participant did not complete the CD-RISC, thus for CD-RISC n = 36. For all other participants, the CD-RISC data was complete. It was decided to include the participants with missing values by calculating the means of the existing values.
All variables were analysed with descriptive statistics. Inspection of histograms revealed the non-normal distribution of some of the variables.
Cronbach’s alpha was computed to assess internal consistency for DLSES, SEC, and CD-RISC. Each participant’s response range (highest value minus lowest value) was calculated for DLSES ADL, DLSES PS, SEC, and CD-RISC, and a mean response range is presented for these assessments.
Differences between the excluded and the included groups were analysed with Mann-Whitney U-test.
Associations among self-efficacy, resilience, language and functional communication were investigated with bivariate correlation analyses. The non-parametric Spearman’s rank correlation was not suitable because of the many tied ranks in the data set. Instead, Pearson’s product moment correlation was used. The problem of non-normal distributions for some of the variables were handled by calculating p-values for all correlation coefficients using an approximate randomisation test with 5000 permutations [Citation80].
To explore whether the level of executive function influence the relationship between functional communication and self-efficacy and/or resilience, the participants were stratified by their executive functions represented by the CLQT scores, using a median split. Thus, forming one group with lower scores on CLQT (Low EF) and one group with higher scores on CLQT (High EF), the correlational analysis procedures were then run again, separately in the two groups.
Results
Participants
47 PWSA potentially eligible for inclusion in the present study were identified. The decision process of inclusion and exclusion will be described in some detail, due to the complexity of the issue in this particular population. The process of participant inclusion is presented in . Characteristics of the included 37 participants are presented in .
Figure 4. Process of participant inclusion.
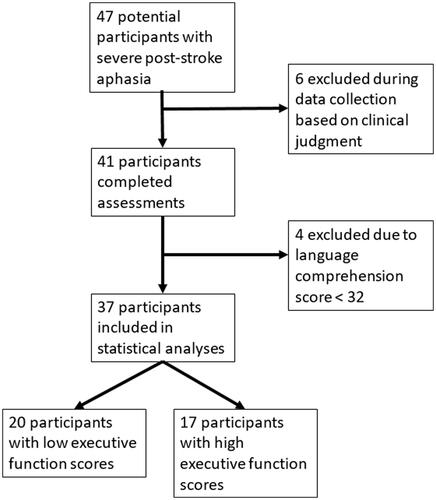
Table 2. Demographics and characteristics of participants (n = 37).
Six individuals were excluded during data collection, based on a decision made by the investigator (CO) not to perform the DLSES, SEC and CD-RISC with these individuals. The decisions were in five of the cases based on clinical judgment of impaired language comprehension and general behaviour during assessments of language and communication. In the sixth case, DLSES was initiated but the questions made the participant upset and was promptly interrupted, and no further attempts to assess psychosocial factors were made. This left 41 potential participants after data collection. However, we were concerned about comprehension of the items by some of the participants with whom the assessments had been completed. Video recordings of the assessments were inspected and 4 participants were identified who frequently displayed behaviours that indicated uncertainty during the self-efficacy and resilience assessments (e.g., pointing to both ends of the scale, pointing to the pictures instead of the scale, expressing uncertainty through gestures and facial expressions). The language comprehension scores for those individuals were all below the lowest reported in previous research about the minimum level of language comprehension required for a quality-of-life questionnaire [Citation62] which also used CAT (the Dutch adaptation) for language assessment. It was decided to use the Raven-Takken et al. [Citation62] study as a guideline and apply the lowest language comprehension score reported there (32 points), as an a posteriori exclusion criterion. In support of the decisions made during data collection, the five potential participants excluded by CO based on clinical judgement also fell below the cut off. All 47 who were assessed were included in other parts of the project [Citation12].
Thus, data from 37 participants were included in the statistical analyses. All participants had Swedish as their primary language.
There were, according to the Mann-Whitney U-test, no statistically significant differences between the excluded and included groups regarding age (U = 122.5, p = 0.105) or time post onset (U = 222.5, p = 0.105). Of the 10 excluded PWSA, 2 (20%) were female. All levels of education were represented. As expected, they had more severe aphasia. Four were classified as ASRS 0, and 6 were classified as ASRS 1. The CAT language score mean was 31 (SD 17.5) and the CAT language comprehension score mean was 25 (SD 10.3) (as compared to 159 (SD 68.6) and 77 (SD 20.4), respectively, for the included participants).
The median split based on CLQT scores resulted in 20 participants in the group with lower scores for executive function (Low EF), and 17 participants in the group with higher executive functions scores (High EF).
Language, executive function and functional communication
Results from CAT, CLQT, Scenario Test and CETI are presented in . Although all participants were classified as having severe aphasia (based on ASRS) there was a wide range in the results regarding functional communication and executive function.
Table 3. Descriptive statistics of participants’ (n = 37) language, executive function and functional communication.
Self-efficacy and resilience
Results of the self-ratings of self-efficacy and resilience are presented in .
Table 4. Results of self-ratings of self-efficacy (DLSES and SEC) and resilience (CD-RISC). Maximum for all DLSES and SEC are 100, maximum for CD-RISC-10 is 40.
The participants’ self-efficacy for psychosocial functions (DLSES PS) was lower than their self-efficacy for ADL (DLSES ADL). The difference was statistically significant (t(36) = 3.68, p = 0.001) with a small effect size (d = 0.45). The self-efficacy for communication (SEC) was lower than the general self-efficacy (DLSES total) but close to the psychosocial self-efficacy.
To limit the number of comparisons the DLSES total score was not included in further analyses.
Cronbach’s alpha and mean response range for the instruments used to measure self-efficacy and resilience are presented in . According to the mean response ranges the participants’ made use of fairly large portions of the scales in the various instruments, indicating that they did not routinely point to the same part of the scale.
Table 5. Cronbach’s α and mean response range for measures of self-efficacy and resilience.
The correlations between the different measures of self-efficacy and resilience are presented in . There were moderate to strong correlations with p-values < .05 among all these measures.
Table 6. Pearson’s correlation coefficients between measures of self-efficacy and resilience.
Associations between linguistic ability, self-efficacy, and resilience
Linguistic ability, as measured with CAT, did not have a statistically significant correlation with the measures of self-efficacy or resilience (DLSES ADL: r = 0.13, p = 0.453, DLSES PS: r = 0.17, p = 0.312, SEC: r = 0.06, p = 0.735, CD-RISC: r = −0.16, p = 0.336).
Associations between functional communication, self-efficacy, and resilience
Functional communication was measured with the Scenario Test and CETI, results are presented in .
The relations between functional communication, self-efficacy, and resilience for the entire sample (n = 37) are presented in .
Table 7. Pearson correlations coefficients between measures of functional communication, self-efficacy and resilience.
The only correlation coefficient with a p-value < 0.05 was found between self-efficacy of communication (SEC) and functional communication as rated by a significant other (CETI). The correlation between SEC and Scenario Test had a p-value relatively close to .05. The relationships between CD-RISC and the two communication measures were characterised by particularly low correlation coefficients and high p-values ().
Influence of executive function
Executive function was measured with four tasks from CLQT, results are presented in . Participants were stratified by CLQT scores into two groups, using median cut.
Mean and standard deviations for DLSES, SEC, and CD-RISC for the two groups are presented in . The Low EF group generally had lower scores on all measures, except on CD-RISC, where the two groups had almost identical results.
Table 8. Mean scores (SD) on all measures for the two groups (Low EF n = 20, and Low EF n = 17).
Bivariate correlations were computed between functional communication (Scenario Test and CETI) on the one hand, and self-efficacy (DLSES, SEC) and resilience (CD-RISC) on the other, separately for the two groups. Results are presented in .
Table 9. Pearson’s correlations between functional communication and psychosocial factors (self-efficacy and resilience), analysis of groups with low and high EF, respectively.
In the Low EF group, no correlations with p-values ≤ 0.05 emerged. In the High EF group, the pattern was quite different. There were significant and strong positive correlations between Scenario Test and both self-efficacy for psychosocial functioning and resilience, as well as between CETI and self-efficacy for communication. In addition, the correlation between Scenario Test and self-efficacy for ADL was moderate and had a p-value close to 0.05.
Discussion
This study aimed to explore the psychosocial factors self-efficacy and resilience in people with severe post-stroke aphasia. Aims also included exploring the relationship with linguistic ability and functional communication. 37 PWSA were included. Existing instruments for assessing self-efficacy and resilience were adapted and administered, in addition to assessments of language, executive functions and functional communication. Internal consistency for the measures of self-efficacy and resilience was good. The levels of self-efficacy and resilience among the participants presented to be as expected; lower than reported for general populations and at approximately the same level as in similar clinical populations (see further details below). The participants demonstrated a wide range of self-efficacy and resilience, which was not clearly related to their linguistic ability. In the sample as a whole, there was no clear evidence of associations between functional communication and self-efficacy and/or resilience. However, when the sample was stratified by executive functions, a different pattern emerged. In the group with more impaired executive functions, there were still no significant associations. In the group with higher executive functions, there were moderate to strong, significant, and close to significant correlations between functional communication and the psychosocial factors self-efficacy and resilience.
Levels of self-efficacy in PWSA
Our results indicate that PWSA as a group report themselves to have lower self-efficacy and resilience than general populations reported in the literature [Citation73,Citation77]. The overall ratings of self-efficacy of the PWSA in the present study were similar to the ratings by stroke patients in the original DLSES study by Maujean et al. [Citation73] (where PWSA were probably excluded since inclusion demanded the absence of cognitive impairment and the data collection procedure included a telephone interview). However, in contrast to that sample, our participants rated their self-efficacy for psychosocial functions (PS) significantly lower than their self-efficacy for ADL (PS 59.5 versus ADL 70.9, in Maujean’s stroke sample PS 64.9 versus ADL 60.5). This result is important since self-efficacy for psychosocial functioning is particularly strongly related to general well-being [Citation72].
The healthy controls of Maujean [Citation72] scored generally higher than our participants (PS 84.5 and ADL 93.0), as did a sample of geriatric subacute rehabilitation patients studied by Harper et al. [Citation31] (PS 75,5, ADL 89.1). Both these populations showed the same pattern as our participants, with a higher score for ADL than for psychosocial functioning.
Since the assessment of self-efficacy for communication, SEC, was constructed specifically for the present study, there is no previous data to compare with. Our participants rated their self-efficacy for communication at a level similar to that of self-efficacy for psychosocial functioning in DLSES. The SEC ratings may seem surprisingly high (mean 56 out of 100), considering all participants had severe aphasia, several of them being functionally non-verbal. In this context, it is important to consider some degree of anosognosia as a possible explanation for unexpectedly optimistic ratings [Citation81]. Anosognosia has been suggested to be associated with executive dysfunction after stroke [Citation82]. On the other hand, it is a known phenomenon in disability research using self-rating of various subjective constructs that people with impairments, as a group, often rate themselves higher than outsiders expect, and frequently above the theoretical mean of the scale used [Citation72,Citation83].
Levels of resilience in PWSA
The mean resilience score among our participants was 28.1, which is slightly lower than for American healthy populations on the 10 item CD-RISC, the scores of which have been reported to fall between 29.0 and 33.5 [Citation77]. A mean score of 32.4 has been reported for a sample of rehabilitation inpatients [Citation84], and a mean of 28.07 for a sample with long-term physical disabilities [Citation85], both studies conducted in the USA. For comparison with a similar group, Hunting Pompon et al. [Citation55] reported a mean of 28.72 on CD-RISC-10 in a sample of 72 people with aphasia (a study conducted in the USA), a result that closely resembles the result found in the present study.
In a recent study, Velickovic et al. [Citation86] evaluated the psychometric properties of the 25-item version of the CD-RISC in a Swedish population, which would be a relevant comparison to our Swedish sample. Since Velickovic et al. [Citation86] used the more extensive version of CD-RISC, direct comparisons cannot be made. However, the 10 items of the version used in the present study is a subset of the 25-item version, and an item mean can be calculated and used for an approximate comparison. Thus, in Velickovic et al.’s [Citation86] Swedish sample, the item mean is 3.14, while in our sample of PWSA it was 2.81, hence our participants rated their resilience as lower but not dramatically so.
In conclusion, self-rated levels of self-efficacy and resilience among our participants match findings reported in the literature; somewhat lower than reported for general populations but at similar levels as in comparable populations.
Since self-efficacy and resilience are considered to be related, but not synonymous, constructs [Citation87], the moderate correlations found between DLSES and CD-RISC were expected.
Several studies in recent years have demonstrated that it is possible for people with aphasia to perform self-ratings of various constructs of a subjective nature (e.g., quality of life [Citation62], life participation [Citation61], post-traumatic growth [Citation63]). The results from the present study point in the same direction; assessment of psychosocial factors such as self-efficacy and resilience is possible with a large part of the aphasia population. This is indicated by the good internal consistency as well as the convergence between our results and previous research.
Associations between linguistic ability, self-efficacy, and resilience
In our results, there were no statistically significant correlations between linguistic ability and self-efficacy or resilience. We have not been able to find any previous studies investigating associations between these specific variables. However, there are studies involving closely related concepts. Chiou and Yu [Citation61] found no relationship between linguistic ability and communicative confidence. Bakheit et al. [Citation37] reported no relationship between aphasia severity and self-esteem. Kuroda and Kuroda [Citation88] found that the severity of language impairment in people with aphasia does not necessarily relate to psychological status. Thus, our findings concur with previous research.
Associations between functional communication, self-efficacy, and resilience
According to the model presented by Light and colleagues [Citation18], the psychosocial factors confidence/self-efficacy and resilience are crucial to communicative competence for people with complex communication needs. If that is indeed so, these factors ought to be specifically considered in the design of communication intervention. In this study, we explored whether we could find evidence to support the associations suggested by Light and colleagues [Citation17,Citation18].
The first analysis, involving the whole sample, did not clearly demonstrate such associations (). A possible explanation for this is revealed by the second set of correlation analyses (). In these, the participants were stratified by their cognitive functions, similar to the procedure used by Parker et al. [Citation65]. The reasoning behind this procedure was that self-efficacy beliefs are not built on the performance or outcome of an activity per se, but on the information about one’s capabilities conveyed via the cognitive processing of that performance or outcome. This means that adequate self-efficacy beliefs are dependent on cognitive abilities [Citation30]. As demonstrated by the CLQT results, many of the participants had cognitive impairments. The results of the second set of correlation analyses clearly showed that there were generally stronger correlations between functional communication and the psychosocial factors self-efficacy and resilience among the participants with more intact executive functions, than among the participants with more impaired executive functions. Although tentative, the results follow a pattern that echo the findings of Parker et al. [Citation65]. These are the results of exploratory research and must be interpreted with caution, but may indicate a line of further inquiry regarding communication and psychosocial factors in aphasia.
However, it is important to discuss other possible explanations for the lack of associations in the sample as a whole, since it offers an opportunity to reflect on several interesting issues regarding functional communication in aphasia. To begin with; in what ways are self-efficacy and resilience likely to affect communication? According to Light and McNaughton [Citation18], confidence/self-efficacy “determines the individual’s propensity to act – in other words, to attempt to communicate in any given situation” (p. 4). Resilience “influences whether or not the individual perseveres with communication despite the many challenges and potential failures encountered” (p. 5). Thus, self-efficacy and resilience might primarily impact the PWSA’s choices regarding what situations they engage in, and also their behaviour during social encounters (e. g. attempting to join in a conversation versus keeping silent, insisting on speaking for themselves versus allowing a partner to speak in their place). Such aspects are probably not very well captured by the instruments we used to measure functional communication in this study. In the Scenario Test, the focus is on the independence with which the requested message is conveyed. The investigator puts the PWSA in hypothetical situations and there is limited opportunity to choose whether to communicate. CETI is an instrument that comes closer to the everyday communication of the participant. However, relying on the ratings of a significant other, it captures mainly the communication that actually takes place and, just like the Scenario Test, focuses on whether the person with aphasia is able to perform certain communicative activities, not to what extent he or she chooses to do so or feels a need to avoid them. Thus, upon closer inspection, CETI is perhaps not well suited to capture the aspects of communication that may be associated with self-efficacy and resilience.
Another possible association between functional communication and psychosocial factors is that the self-efficacy and resilience of the PWSA may affect their behavior in a way, that in turn influences the communication partner’s attitudes and behavior. Most people who are not used to interacting with people with aphasia experience insecurity in such encounters, and may even try to avoid them. A strong sense of self-efficacy and/or resilience on the part of the PWSA might manifest itself in more initiation of interaction, determination in trying to get the message across, meeting failures with humour, and so on. Thus, self-efficacy and resilience could be related to the social (in Light’s model called socio-relational) skills described as; “demonstrating an interest in others, participating in interactions actively, being responsive to partners, putting partners at ease, and projecting a positive self-image” [Citation17]. The demonstration of such skills may lead to more successful communication through increased engagement and cooperation from the communication partner. By this route, self-efficacy and resilience could lead to increased participation in social situations, even without a direct impact on the aspects of functional communication captured by the Scenario Test and CETI.
Methodological considerations and limitations
Being an exploratory investigation, this study has obvious limitations. The main issue when using self-rating instruments with PWSA is to make as sure as possible that the items are presented in such a way that they can be understood and responded to in spite of the language impairments. This demands adaptation of the questionnaire and of the administration procedure [Citation74]. The administration of DLSES, SEC and CD-RISC was not strictly standardized; the investigator did not give verbatim identical instructions to all participants. The use of prepared descriptions and examples to clarify the items was an attempt to standardize the procedure to a certain extent, but departures were made when deemed necessary. This entails a risk of bias and a compromised reliability, since the evaluator may affect the responses, for instance through the unconscious display of preference or expectation. However, identical instructions in this population lead to varying opportunities to understand instructions and items, due to individual differences in language comprehension. Thus, when administering assessments (other than language assessments) to PWSA, a choice must be made between a strictly standardised procedure resulting in varying comprehension, or a more flexible approach aiming for optimal comprehension for all participants, at the cost of slightly varying the administration procedure. For this study, the latter strategy was chosen.
The results and experiences from the data collection allow us to make some observations about the measurement of self-efficacy and resilience in PWSA. Of the original 47 potential participants, 37 were included in the analysis. The investigator conducting the assessments (first author CO) made decisions about exclusion of potential participants during data collection. These decisions had to be made on the spot during the data collection session. To refrain from administering DLSES, SEC and CD-RISC to these participants was considered important not only to avoid invalid data, but foremost due to ethical considerations. To administer questionnaires about self-efficacy and resilience to persons who would struggle to understand the content and purpose of the questions was not considered ethical. This method for exclusion during data collection was inevitably influenced by the subjective judgement of CO.
Before data analysis, another four participants were excluded based on language comprehension scores. The decision to use a language comprehension cut off was founded on an inspection of the video recorded assessments, in combination with data reported in previous research about the minimum level of language comprehension required for a quality-of-life questionnaire [Citation62]. Thus, in this study the exclusion criterion of having a language comprehension score <32 was applied generally, but only after data collection was completed and data were reviewed. This is a somewhat unorthodox method, and is a reflection of the complexity of assessment in, and research about, severe aphasia. There is a great need for increased knowledge about this population, and the delicate balance between ethical issues and the endeavour to include people with severe aphasia in research, as well as the methodological challenges, needs to be acknowledged and discussed within the fields of stroke and aphasia research.
Another limitation is that the instruments used to measure self-efficacy and resilience were not validated for this specific population. DLSES is developed for stroke survivors, but has not been previously used with stroke survivors with severe aphasia. In addition, the instrument was translated and adapted with visual support by the authors of this study, while SEC was developed specifically for the study. CD-RISC already existed in a Swedish version, but it was adapted with visual support.
Resilience was measured as a mainly internal personal attribute, in keeping with the description of resilience in the model of communication competence by Light and colleagues [Citation17,Citation18]. However, resilience may also be considered to include external environmental and social resources [Citation58,Citation89]. It may be considered that the failure to include this broader view of resilience is a limitation of the present study.
Future directions
Since it has been shown that self-efficacy and resilience are related to various outcomes in stroke rehabilitation [Citation21,Citation23,Citation32,Citation33,Citation50,Citation53,Citation72,Citation90], and possibly functional communication, it seems clear that gaining knowledge about these factors in people with aphasia is important.
There are several instruments for measuring self-efficacy and resilience, and it is not certain that the instruments used in this study are the most suitable for people with aphasia. After the data collection for this study, the University of Washington Resilience Scale (UWRS) was published by Amtmann et al. [Citation91], using stakeholder engagement and modern psychometric methods. UWRS is currently being adapted for use with people with aphasia (R. Hunting Pompon, personal communication, June 14, 2023), and may prove to be more suitable for the aphasia population. For continued use of DLSES and CD-RISC in clinic or research, a thorough evaluation with people with aphasia is needed.
It is also necessary to further explore the possible associations in PWSA between functional communication and the psychosocial factors suggested by Light et al. [Citation18]. There are several possibilities; using measures targeting other aspects of communicative behaviour than the ones employed here, or using more communication-specific measures of self-efficacy and resilience and similar constructs, such as CCRSE [Citation39,Citation40].
It might be fruitful to think about ways of strengthening the self-efficacy and resilience of PWSA. Social Cognitive Theory predicts that self-efficacy has an impact on behavior and performance and that self-efficacy beliefs can be affected through intervention [Citation30]. Activities to systematically enhance self-efficacy and resilience could be integrated into aphasia interventions, thereby adding more tools to improve the functioning and well-being of people with aphasia. It is, in fact, likely that such processes are at work in aphasia group therapy programs, even if self-efficacy or resilience are not explicitly targeted. Many group interventions give opportunity for mastery experience, vicarious experience, and the receiving and giving of social support [Citation92]. It is possible that the enhancement of self-efficacy and resilience is one of the mechanisms behind the positive outcome of group interventions, that has sometimes proven difficult to quantify [Citation93]. Increased communication confidence has been shown to be an outcome of aphasia group participation [Citation41], thereby proving that it is possible to improve confidence. Whether this also has a positive effect directly on functional communication remains to be examined. Perhaps, with further research, the effect of self-efficacy and resilience on communication could be better understood, and, if proven important, systematic strategies to build self-efficacy and resilience could be put to more structured use. Enhancement of self-efficacy and resilience cannot replace interventions targeting language and communication. But, as eloquently put by Bandura: “self-belief does not necessarily ensure success, but self-disbelief assuredly spawns failure” [Citation30].
Conclusions
This study was an exploration of self-efficacy and resilience in the population of PWSA, and of the associations between these constructs and linguistic and cognitive ability as well as functional communication.
The results indicated that assessment of self-efficacy and resilience is, with proper adaptation, possible in a majority of PWSA. Since it proved necessary to adopt a language comprehension cut off for inclusion it cannot be claimed that assessment of self-efficacy and resilience can be performed with all PWSA.
PWSA as a group had decreased self-efficacy and resilience compared to general populations reported in the literature. We found no association between self-efficacy or resilience and linguistic ability. The same was true for functional communication, when analysing the sample as a whole. However, in the part of the sample who had more intact executive functions, associations between functional communication and the various measures of self-efficacy and resilience could be demonstrated. Although many questions remain unanswered, we believe this study has provided a contribution to the knowledge about self-efficacy and resilience and has demonstrated these constructs to be worthy of further investigation in aphasia research.
Acknowledgements
The authors wish to thank the participants and their significant others for their time, effort and patience.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Flowers HL, Skoretz SA, Silver FL, et al. Poststroke aphasia frequency, recovery, and outcomes: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2016;97(12):2188–2201.e8. doi: 10.1016/j.apmr.2016.03.006.
- Grönberg A, Henriksson I, Stenman M, et al. Incidence of aphasia in ischemic stroke. Neuroepidemiology. 2022;56(3):174–182. doi: 10.1159/000524206.
- Papathanasiou I, Coppens P, Davidson B. Aphasia and related neurogenic communication disorders: basic concepts, management, and efficacy. In: Papathanasiou I, Coppens P, editors. Aphasia and related neurogenic communication disorders. 2nd ed. Burlington (MA): Jones & Bartlett Learning; 2017. p. 3–12.
- King JM. Communication supports. In: Simmons-Mackie N, King JM, Beukelman D, editors. Supporting communication for adults with acute and chronic aphasia. Baltimore (MD): Paul H. Brookes Pub; 2013. p. 51–72.
- Lasker JP, Garrett KL, Fox LE. Severe aphasia. In: Beukelman D, Garrett KL, Yorkston KM, editors. Augmentative communication strategies for adults with acute or chronic medical conditions. Baltimore (MD): Paul H. Brookes Publishing Co; 2007. p. 163–206.
- Babbitt E, Cherney L. Communication confidence in persons with aphasia. Top Stroke Rehabil. 2010;17(3):214–223. doi: 10.1310/tsr1703-214.
- Cruice M, Worrall L, Hickson L. Quantifying aphasic people’s social lives in the context of non-aphasic peers. Aphasiology. 2006;20(12):1210–1225. doi: 10.1080/02687030600790136.
- Northcott S, Hilari K. Why do people lose their friends after a stroke? Int J Lang Commun Disord. 2011;46(5):524–534. doi: 10.1111/j.1460-6984.2011.00079.x.
- Parr S. Living with severe aphasia: tracking social exclusion. Aphasiology. 2007;21(1):98–123. doi: 10.1080/02687030600798337.
- Darrigrand B, Dutheil S, Michelet V, et al. Communication impairment and activity limitation in stroke patients with severe aphasia. Disabil Rehabil. 2011;33(13–14):1169–1178. doi: 10.3109/09638288.2010.524271.
- Holland AL. Observing functional communication of aphasic adults. J Speech Hear Disord. 1982;47(1):50–56. doi: 10.1044/jshd.4701.50.
- Olsson C, Arvidsson P, Blom Johansson M. Relations between executive function, language, and functional communication in severe aphasia. Aphasiology. 2019;33(7):821–845. doi: 10.1080/02687038.2019.1602813.
- Ramsberger G, Rende B. Measuring transactional success in the conversation of people with aphasia. Aphasiology. 2002;16(3):337–353. doi: 10.1080/02687040143000636.
- Schumacher R, Bruehl S, Halai AD, et al. The verbal, nonverbal and structural bases of functional communication abilities in aphasia. Brain Commun. 2020;2(2):fcaa118.
- Simmons-Mackie N, Raymer A, Cherney LR. Communication partner training in aphasia: an updated systematic review. Arch Phys Med Rehabil. 2016;97(12):2202–2221.e8. doi: 10.1016/j.apmr.2016.03.023.
- Simmons-Mackie N. Frameworks for managing communication support for people with aphasia. In: Simmons-Mackie N, King JM, Beukelman D, editors. Supporting communication for adults with acute and chronic aphasia. Baltimore (MD): Paul H. Brookes Pub; 2013. p. 11–50.
- Light JC, Beukelman DR, Reichle J. Communicative competence for individuals who use AAC from theory to effective practice. Baltimore (MD):Paul H. Brookes Publishing Co.; 2003.
- Light J, McNaughton D. Communicative competence for individuals who require augmentative and alternative communication: a new definition for a new era of communication? Augment Altern Commun. 2014;30(1):1–18. doi: 10.3109/07434618.2014.885080.
- Kagan A, Simmons-Mackie N, Rowland A, et al. Counting what counts: a framework for capturing real-life outcomes of aphasia intervention. Aphasiology. 2008;22(3):258–280. doi: 10.1080/02687030701282595.
- Bandura A. Social foundations of thought and action: a social cognitive theory. Englewood Cliffs (NJ): Prentice-Hall, Inc; 1986.
- Korpershoek C, van der Bijl J, Hafsteinsdóttir TB. Self-efficacy and its influence on recovery of patients with stroke: a systematic review. J Adv Nurs. 2011;67(9):1876–1894. doi: 10.1111/j.1365-2648.2011.05659.x.
- Volz M, Möbus J, Letsch C, et al. The influence of early depressive symptoms, social support and decreasing self-efficacy on depression 6 months post-stroke. J Affect Disord. 2016;206:252–255. doi: 10.1016/j.jad.2016.07.041.
- Volz M, Voelkle MC, Werheid K. General self-efficacy as a driving factor of post-stroke depression: a longitudinal study. Neuropsychol Rehabil. 2019;29(9):1426–1438. doi: 10.1080/09602011.2017.1418392.
- Liu Z, Zhou X, Zhang W, et al. Factors associated with quality of life early after ischemic stroke: the role of resilience. Top Stroke Rehabil. 2019;26(5):335–341. doi: 10.1080/10749357.2019.1600285.
- Kauhanen ML, Korpelainen JT, Hiltunen P, et al. Aphasia, depression, and non-verbal cognitive impairment in ischaemic stroke. Cerebrovasc Dis. 2000;10(6):455–461. doi: 10.1159/000016107.
- Mitchell AJ, Sheth B, Gill J, et al. Prevalence and predictors of post-stroke mood disorders: a meta-analysis and meta-regression of depression, anxiety and adjustment disorder. Gen Hosp Psychiatry. 2017;47:48–60. doi: 10.1016/j.genhosppsych.2017.04.001.
- Zanella C, Laures-Gore J, Dotson VM, et al. Incidence of post-stroke depression symptoms and potential risk factors in adults with aphasia in a comprehensive stroke center. Top Stroke Rehabil. 2023;30(5):448–458. doi: 10.1080/10749357.2022.2070363.
- Hilari K. The impact of stroke: are people with aphasia different to those without? Disabil Rehabil. 2011;33(3):211–218. doi: 10.3109/09638288.2010.508829.
- Thayabaranathan T, Baker C, Andrew N, et al. Exploring dimensions of quality-of-life in survivors of stroke with communication disabilities – a brief report. Top Stroke Rehabil. 2023;30(6):603–609. doi: 10.1080/10749357.2022.2095087.
- Bandura A. Self-efficacy: the exercise of control. Basingstoke: W. H. Freeman; 1997.
- Harper KJ, Jacques A, Barton A. Validity and reliability of the daily living self-efficacy scale in subacute geriatric rehabilitation. Phys Occup Ther Geriatr. 2020;38(1):31–42. doi: 10.1080/02703181.2019.1675844.
- Jones F, Riazi A. Self-efficacy and self-management after stroke: a systematic review. Disabil Rehabil. 2011;33(10):797–810. doi: 10.3109/09638288.2010.511415.
- Nott M, Wiseman L, Seymour T, et al. Stroke self-management and the role of self-efficacy. Disabil Rehabil. 2019;43(10):1410–1419.
- Torrisi M, De Cola MC, Buda A, et al. Self-efficacy, poststroke depression, and rehabilitation outcomes: is there a correlation? J Stroke Cerebrovasc Dis. 2018;27(11):3208–3211. doi: 10.1016/j.jstrokecerebrovasdis.2018.07.021.
- Wijenberg MLM, van Heugten CM, van Mierlo ML, et al. Psychological factors after stroke: are they stable over time? J Rehabil Med. 2019;51(1):18–25. doi: 10.2340/16501977-2688.
- Cameron JE, Voth J, Jaglal SB, et al. “In this together”: social identification predicts health outcomes (via self-efficacy) in a chronic disease self-management program. Soc Sci Med. 2018;208:172–179. doi: 10.1016/j.socscimed.2018.03.007.
- Bakheit AMO, Barrett L, Wood J. The relationship between the severity of post-stroke aphasia and state self-esteem. Aphasiology. 2004;18(8):759–764. doi: 10.1080/02687030444000372.
- Brumfitt SM, Sheeran P. The development and validation of the visual analogue self-esteem scale (VASES). Br J Clin Psychol. 1999;38(4):387–400. doi: 10.1348/014466599162980.
- Babbitt EM, Heinemann AW, Semik P, et al. Psychometric properties of the communication confidence rating scale for aphasia (CCRSA): phase 2. Aphasiology. 2011;25(6-7):727–735. doi: 10.1080/02687038.2010.537347.
- Cherney LR, Babbitt EM, Semik P, et al. Psychometric properties of the communication confidence rating scale for aphasia (CCRSA): phase 1. Top Stroke Rehabil. 2011;18(4):352–360. doi: 10.1310/tsr1804-352.
- Plourde JMH, Purdy SC, Moore C, et al. Gavel club for people with aphasia: communication confidence and quality of communication life. Aphasiology. 2019;33(1):73–93. doi: 10.1080/02687038.2018.1453043.
- Nichol L, Wallace S, Pitt R, et al. Self-management of aphasia: a scoping review. Aphasiology. 2019;33(8):903–942. doi: 10.1080/02687038.2019.1575065.
- Nichol L, Wallace SJ, Pitt R, et al. People with aphasia share their views on self-management and the role of technology to support self-management of aphasia. Disabil Rehabil. 2022;44(24):7399–7412. doi: 10.1080/09638288.2021.1989501.
- Nichol L, Wallace SJ, Pitt R, et al. Communication partner perspectives of aphasia self-management and the role of technology: an in-depth qualitative exploration. Disabil Rehabil. 2022;44(23):7199–7216. doi: 10.1080/09638288.2021.1988153.
- Windle G. What is resilience? A review and concept analysis. Rev Clin Gerontol. 2011;21(2):152–169. doi: 10.1017/S0959259810000420.
- Scoloveno R. A concept analysis of the phenomenon of resilience. J Nurs Care. 2016;5(4) doi: 10.4172/2167-1168.1000353.
- Bonanno GA. Loss, trauma, and human resilience: have we underestimated the human capacity to thrive after extremely aversive events? Psychol Trauma. 2008;S(1):101–113. doi: 10.1037/1942-9681.S.1.101.
- Pangallo A, Zibarras L, Lewis R, et al. Resilience through the lens of interactionism: a systematic review. Psychol Assess. 2015;27(1):1–20. Mar doi: 10.1037/pas0000024.
- Sarre S, Redlich C, Tinker A, et al. A systematic review of qualitative studies on adjusting after stroke: lessons for the study of resilience. Disabil Rehabil. 2014;36(9):716–726. doi: 10.3109/09638288.2013.814724.
- Neils-Strunjas J, Paul D, Clark AN, et al. Role of resilience in the rehabilitation of adults with acquired brain injury. Brain Inj. 2017;31(2):131–139. doi: 10.1080/02699052.2016.1229032.
- Sherer M, Sander AM, Nick TG, et al. Key dimensions of impairment, self-report, and environmental supports in persons with traumatic brain injury. Rehabil Psychol. 2015;60(2):138–146. May doi: 10.1037/rep0000030.
- Vos L, Poritz JMP, Ngan E, et al. The relationship between resilience, emotional distress, and community participation outcomes following traumatic brain injury. Brain Inj. 2019;33(13-14):1615–1623. doi: 10.1080/02699052.2019.1658132.
- Castor N, El Massioui F. Resilience after a neurological pathology: what impact on the cognitive abilities of patients with brain damage? Neuropsychol Rehabil. 2020;30(5):853–871. doi: 10.1080/09602011.2018.1512873.
- Kim GM, Lim JY, Kim EJ, et al. Resilience of patients with chronic diseases: a systematic review. Health Soc Care Community. 2019;27(4):797–807. Jul doi: 10.1111/hsc.12620.
- Hunting Pompon R, Amtmann D, Bombardier C, et al. Modifying and validating a measure of chronic stress for people with aphasia. J Speech Lang Hear Res. 2018;61(12):2934–2949. doi: 10.1044/2018_JSLHR-L-18-0173.
- Cangi ME, Eroğlu Uzun D, Gürel İN. Speech fluency, depression, and resilience in chronic aphasia. Aphasiology. 2022;37(4):696–713. doi: 10.1080/02687038.2022.2094334.
- Moss B, Northcott S, Behn N, et al. ‘Emotion is of the essence. … number one priority’: a nested qualitative study exploring psychosocial adjustment to stroke and aphasia. Int J Lang Commun Disord. 2021;56(3):594–608. doi: 10.1111/1460-6984.12616.
- Hunting Pompon R, Mach H. Characterizations of resilience in poststroke aphasia: a scoping review and considerations for treatment and research. Top Lang Dis. 2022;42(3):236–251. doi: 10.1097/TLD.0000000000000285.
- Gillespie BM, Chaboyer W, Wallis M. Development of a theoretically derived model of resilience through concept analysis. Contemp Nurse. 2007;25(1–2):124–135. doi: 10.5172/conu.2007.25.1-2.124.
- Cruice M, Worrall L, Hickson L, et al. Measuring quality of life: comparing family members’ and friends’ ratings with those of their aphasic partners. Aphasiology. 2005;19(2):111–129. doi: 10.1080/02687030444000651.
- Chiou HS, Yu VY. Measuring life participation, communicative confidence, language, and cognition in people with aphasia. Perspect ASHA SIGs. 2018;3(2):4–12. doi: 10.1044/persp3.SIG2.4.
- Raven-Takken E, Ter Wal N, Van Ewijk L. What minimum level of language comprehension is required for reliable administration of the SAQOL-39NLg? Aphasiology. 2020;34(6):695–708. doi: 10.1080/02687038.2019.1610152.
- Sherratt S, Worrall L. Posttraumatic growth following aphasia: a prospective cohort study of the first year post-stroke. Aphasiology. 2021;35(3):291–313. doi: 10.1080/02687038.2020.1787945.
- Parsons S, Kruijt A-W, Fox E. A cognitive model of psychological resilience. J Exp Psychopathol. 2016;7(3):296–310. doi: 10.5127/jep.053415.
- Parker HA, Rapport LJ, Williams MW, et al. Functional independence after acquired brain injury: prospective effects of health self-efficacy and cognitive impairment. Rehabil Psychol. 2018;63(4):595–603. doi: 10.1037/rep0000243.
- Goodglass H, Kaplan E, Barresi B. The boston diagnostic aphasia examination. 3rd ed. Philadelphia (PA): Lippincot Williams Wilkins; 2001.
- Swinburn K, Porter G, Howard D. Comprehensive aphasia test (CAT). Hove: Psychology Press; 2004.
- Helm-Estabrooks N. The cognitive linguistic quick test. San Antonio, TX: The Psychological Corporation; 2001.
- Helm-Estabrooks N. Cognition and aphasia: a discussion and a study. J Commun Disord. 2002;35(2):171–186. doi: 10.1016/s0021-9924(02)00063-1.
- van der Meulen I, van de Sandt-Koenderman WM, Duivenvoorden HJ, et al. Measuring verbal and non-verbal communication in aphasia: reliability, validity, and sensitivity to change of the scenario test. Int J Lang Commun Disord. 2010;45(4):424–435. doi: 10.3109/13682820903111952.
- Lomas J, Pickard L, Bester S, et al. The communicative effectiveness index: development and psychometric evaluation of a functional communication measure for adult aphasia. J Speech Hear Disord. 1989;54(1):113–124. doi: 10.1044/jshd.5401.113.
- Maujean FA. An investigation of the relationship between self-efficacy and well-being in stroke survivors. Queensland: Griffith University; 2011.
- Maujean FA, Davis P, Kendall E, et al. The daily living self-efficacy scale: a new measure for assessing self-efficacy in stroke survivors. Disabil Rehabil. 2014;36(6):504–511. doi: 10.3109/09638288.2013.804592.
- Tucker FM, Edwards DF, Mathews LK, et al. Modifying health outcome measures for people with aphasia. Am J Occup Ther. 2012;66(1):42–50. doi: 10.5014/ajot.2012.001255.
- Bildstod.se. [Internet]. Göteborg: Västra Götalandsregionen; 2017 [cited 2017 May 15]. www.bildstod.se
- Connor KM, Davidson JRT. Connor-Davidson resilience scale (CD-RISC). 2001. http://www.cdrisc.com.
- Davidson JRT, Connor KM. Connor-Davidson resilience scale (CD-RISC). 2016. www.cd-risc.com.
- Campbell-Sills L, Stein MB. Psychometric analysis and refinement of the Connor–Davidson resilience scale (CD-RISC): validation of a 10-item measure of resilience. J Trauma Stress. 2007;20(6):1019–1028. doi: 10.1002/jts.20271.
- Cosco TD, Kaushal A, Richards M, et al. Resilience measurement in later life: a systematic review and psychometric analysis. Health Qual Life Outcomes. 2016;14(1):16. doi: 10.1186/s12955-016-0418-6.
- Hayes AF. SPSS procedures for approximate randomization tests. Behav Res Meth Instrum Comput. 1998;30(3):536–543. doi: 10.3758/BF03200687.
- Crosson B, Barco PP, Velozo CA, et al. Awareness and compensation in postacute head injury rehabilitation. J Head Trauma Rehabil. 1989;4(3):46–54.
- Narushima K, Moser DJ, Robinson RG. Correlation between denial of illness and executive function following stroke: a pilot study. J Neuropsychiatry Clin Neurosci. 2008;20(1):96–100. doi: 10.1176/jnp.2008.20.1.96.
- Dunn D. The social psychology of disability. Oxford: Oxford University Press, Incorporated; 2014.
- Dodd Z. Effects of adult romantic attachment and social support on resilience and depression in patients with acquired disabilities [dissertation]. Denton (TX): University of North Texas; 2010.
- Terrill AL, Molton IR, Ehde DM, et al. Resilience, age, and perceived symptoms in persons with long-term physical disabilities. J Health Psychol. 2016;21(5):640–649. doi: 10.1177/1359105314532973.
- Velickovic K, Rahm Hallberg I, Axelsson U, et al. Psychometric properties of the Connor-Davidson resilience scale (CD-RISC) in a non-clinical population in Sweden. Health Qual Life Outcomes. 2020;18(1):132. doi: 10.1186/s12955-020-01383-3.
- Schwarzer R, Warner LM. Percieved self-efficacy and its relationship to resilience. In: Prince-Embury S, Saklofske DH, editors. Resilience in children, adolescents, and adults: translating research into practice. New York (NY): Springer Verlag; 2013.
- Kuroda Y, Kuroda R. The relationship between verbal communication and observed psychological status in aphasia: preliminary findings. Aphasiology. 2005;19(9):849–859. doi: 10.1080/02687030500225951.
- Yan H-Y, Lin H-R. Resilience in stroke patients: a concept analysis. Healthcare. 2022;10(11):2281. doi: 10.3390/healthcare10112281.
- de Graaf JA, Schepers VPM, Nijsse B, et al. The influence of psychological factors and mood on the course of participation up to four years after stroke. Disabil Rehabil. 2022;44(10):1855–1862. doi: 10.1080/09638288.2020.1808089.
- Amtmann D, Bamer AM, Alschuler KN, et al. Development of a resilience item bank and short forms. Rehabil Psychol. 2020;65(2):145–157. doi: 10.1037/rep0000312.
- Elman RJ, Hoover E. Integrating commuication support into aphasia group treatment. In: Simmons-Mackie N, King JM, Beukelman D, editors. Supporting communication for adults with acute and chronic aphasia. Baltimore (MD): Paul H. Brookes publishing; 2013. p. 189–220.
- Hoover E, McFee A, DeDe G. Efficacy of group conversation intervention in individuals with severe profiles of aphasia. Sem Speech Lang. 2020;41(1):71–82.
