Abstract
Purpose
Communication difficulties are highly prevalent in the stroke population, with implications for patient experience, safety and outcomes. This study explores the experiences of people with aphasia and family members regarding healthcare communication in acute and subacute stroke settings.
Methods and materials
A phenomenological approach was used to understand participants’ experiences. Participants took part in a focus group and data were analysed using an inductive thematic approach.
Results
For individuals with aphasia (n = 4) and family members (n = 2), five themes were generated: “aphasia makes it hard to communicate,” “hospital staff focus on the patient’s medical status only,” “people with aphasia do not get the help they need to improve,” “staff lack the skills to communicate with people with aphasia,” and “staff are crucial to improving healthcare communication.”
Conclusions
The stroke team has expertise in the medical management of stroke but struggle to communicate with patients with aphasia. Patients’ experience of healthcare communication is often one-way and limited to following instructions, with missed opportunities to discuss core topics such as prognosis, rehabilitation, and person-specific needs. Patients and families assert that all members of the stroke healthcare team should be able to adapt communication to accommodate patients.
Implications for Rehabilitation
Person-centred care is not a reality for many patients with aphasia.
Many healthcare conversations, including informal assessments and discussing prognosis, are not accessible for people with aphasia.
Consequently, for people with aphasia, healthcare in hospital is characterised by confusion and exclusion.
Staff are crucial to improving healthcare communication; when appropriate strategies were used, these were not only effective but very meaningful to patients.
Introduction
Within most Western countries, person-centred care is recognised as an essential component of healthcare services [Citation1–5]. This philosophy advocates for patients to be involved in healthcare decision-making, for care to be individualised to specific patient needs and for patients to have access to care that works for them [Citation6,Citation7]. Effective communication is embedded within person-centredness [Citation8–11] and is considered to be a marker of quality: it influences patient satisfaction [Citation12–14], is linked to patient safety incidents [Citation15, Citation16], and may contribute to health outcomes [Citation17]. In Australia, facilitating effective communication between service providers, patients, and their families is enshrined as a standard for safe and quality care [Citation18].
Despite the recognised influence of communication on safe and quality care, patients’ communication needs continue to go unmet [Citation19]. Communication breakdown is one of the most common causes of sentinel events in healthcare [Citation20]. Patients with communication disabilities are particularly vulnerable: they experience difficulty communicating their healthcare needs [Citation21–23] and accessing the care they need [Citation24], have poorer health outcomes [Citation24] and are at higher risk of experiencing a preventable adverse event in hospital [Citation25]. This is particularly relevant to stroke services: as many as 55% of patients on acute stroke wards may struggle to communicate their healthcare needs [Citation23]. Aphasia is a common consequence of stroke, affecting approximately one third of patients with stroke in hospital [Citation26]. People with aphasia are vulnerable to distressing adverse events in hospital, report difficulty interacting with their medical teams, experience negative emotions relating to communication such as frustration and disappointment, and feel disempowered when healthcare workers lack sufficient knowledge about and training in aphasia [Citation27].
Given the nature of aphasia, healthcare communication and involvement in clinical decision-making are vulnerable areas for patients with aphasia. Information provided by healthcare workers is often not designed to be accessible and family members report they receive inadequate emotional support for the adjustment to living with a person with aphasia [Citation28]. Unsurprisingly, people with aphasia report dissatisfaction with health services [Citation29]. From the perspective of staff, nurses have reported not budgeting time for unexpected communication initiated by patients [Citation30]. Furthermore, evidence suggests that staff avoid or limit communication with patients with aphasia, partly due to concerns of lack of time but also due to a fear they will not be able to understand the patient [Citation31,Citation32]. When they do interact with patients with aphasia, they prefer to stick to topics relating to their specific discipline, focus on basic needs, or speak with family members instead [Citation31]. Yet, when interactions are task-focused and the topic is controlled by the staff member, these encounters are unlikely to be therapeutic or individual, particularly for patients with communication difficulties who will struggle to redirect the conversation [Citation33,Citation34].
Healthcare workers play a key role in enabling effective communication for people with communication disabilities [Citation35]. Staff want to help patients with aphasia but often lack the time, skills, resources, and support from management and hospital organisational systems [Citation31,Citation32]. Direct observation of clinical interactions between healthcare workers and people with aphasia indicate asymmetrical conversations: nurses on a stroke rehabilitation ward caring for patients with aphasia or dysarthria were observed to control the timing, topic and flow of the conversation to the extent that patients had little input other than to respond to closed questions [Citation34]. Despite the study taking place on a specialist rehabilitation ward, the topic of conversation typically focused on physical care tasks and there was no evidence of conversations about the patient’s goals or individual concerns [Citation34]. Similar findings have been reported elsewhere: nurses’ interactions were observed to be warm and respectful but primarily focused on physical care and there were qualitative and quantitative difference in how nurses interacted with patients with and without aphasia [Citation36]. For example, clinical interactions between nurses and patients with aphasia may follow a simple question-answer pattern, with limited opportunities for the patient to introduce or expand on the topic [Citation36].
There is a disconnect between the widely accepted and lauded philosophy of person-centred care and the unmet needs of people with aphasia and their family members. This study formed part of a broader project to design an mHealth (mobile health) application to support healthcare communication between people with aphasia and healthcare workers during hospital admission. Interest in the use of mobile technology to support healthcare communication is emerging [Citation37–39] and may offer solutions to the problem of healthcare communication between healthcare workers and those with communication disability. For example, nurses have suggested that mobile technology may assist them to personalise care for people with communication disabilities [Citation40]. While there is an increasing trend of mHealth technology within healthcare systems [Citation41], efficacy evidence is still limited [Citation42]. To inform the development of the application, focus groups were held with individuals with lived experience: people with aphasia, family members and healthcare workers. Findings related to healthcare workers have been reported elsewhere [Citation31]. The aim of the current study is to explore the experiences of individuals with aphasia and their family members regarding healthcare communication within inpatient-settings.
Materials and methods
Ethics
Ethics approval was obtained from La Trobe University Human Ethics Committee (HEC16-080) and St Vincent’s Hospital Melbourne (LNR HREC ref: LNR/16/SVHM/238).
Study design
The study adopted a phenomenological approach within a social constructivist paradigm. The phenomenological methodology allowed us to explore the individuals’ perspectives of healthcare communication in order to develop a deeper understanding of their experiences. A social constructivist paradigm was used because it reflected our assumption that all knowledge, including participants’ and researchers’ realities, is constructed through interaction [Citation43]. We assumed interaction would help to articulate and identify patients’ and family members’ beliefs about communicating with health professionals, and our knowledge of those beliefs. Data were collected via a semi-structured focus group and analysed using an inductive thematic analysis. The study is reported in line with the consolidated criteria for reporting qualitative research (COREQ) checklist [Citation44].
Participants
Participants were recruited via purposive sampling (see for eligibility criteria). Information was disseminated through newsletters and email distribution via the Stroke Foundation, the Stroke Association of Victoria and Aphasia Victoria. Individuals who expressed interest were provided with participant information sheets in line with aphasia-friendly formatting recommendations [Citation45–47]. Written informed consent was obtained before data collection commenced.
Table 1. Eligibility criteria for recruited participants.
Four individuals with aphasia and two family members were recruited and participated in the study. Time post-stroke ranged from 3 to 7.5 years (). Demographic data were not collected for family members. No participants refused participation or dropped out of the study.
Table 2. Demographic information of the participants with aphasia.
Table 3. Topic guide.
Data collection
The research team collaborated to generate the focus group questions (). These key questions were designed to allow sufficient time for discussion with individuals with aphasia, as well as exploring potentially conflicting experiences amongst participants. Probe questions were subsequently used to further explore participants’ responses to the key questions.
A semi-structured focus group took place in November 2016 at La Trobe University, facilitated by the first author and a research assistant who took field notes. The duration of the focus group was two hours including breaks and was audio- and video-recorded to capture verbal and nonverbal communication. The participants knew each other either from participating in previous research studies or through community events to promote awareness of aphasia. This meant that introductions were minimal (i.e. introducing members of the research team) and led to a very convivial atmosphere. The facilitator’s role was to help the group to establish ground rules for the interaction, ask questions, use supportive conversation techniques, ensure that individual participants had the opportunity to contribute to the discussion, and to time-manage the interaction. Supported conversation techniques included writing key words, drawing, and using gesture to assist participants to understand and follow the discussion, and to express their thoughts and opinions. The facilitator made frequent use of verification techniques [Citation48] to check she had correctly understood the responses of the participants with aphasia. During the focus group, participants frequently responded to each other to express agreement, disagreement or a different perspective.
Characteristics of the facilitator and relationship with the participants
The first author facilitated the focus group; she is a female researcher who holds a PhD in relation to aphasia and previously worked as a speech pathologist in hospital-based and community multidisciplinary teams. The facilitator/first author had previously met two of the participants with aphasia and one of the family members. The participants knew the study formed part of a broader study to develop a mHealth app to support healthcare communication; as part of that study, they were invited to share their experiences of hospital care following their stroke. The facilitator/first author’s assumptions were that individuals with aphasia and families would report negative experiences of communication in acute settings, possibly more positive experience of subacute and rehabilitation setting, but report an overall dissatisfaction with healthcare communication. In order to reduce potential research bias, the facilitator asked open questions, which had been developed in collaboration with other members of the research team (). Questions were carefully worded to limit the potential to lead participants to respond in a certain way. Steps to reduce potential bias were taken during data analysis: firstly, the first and second authors completed data analysis together (the second author had not been involved in designing the focus group questions or in data collection). Secondly, developing themes and subthemes were discussed with other members of the research team (the third and last authors) as a form of peer checking.
Data analysis
The video recording of the focus group was transcribed verbatim by a research assistant who is familiar with aphasia and who received transcription training from the first author (this included using a transcription template, a key for transcribing nonverbal communication, and checking by the first author). The written transcript was analysed following an inductive, semantic thematic approach described by Braun and Clarke [Citation49]. This analytical method was chosen to allow for investigation of the participants’ realities. In this way, we had confidence that the resulting themes were data-driven [Citation49,Citation50]. Data from individuals with aphasia and from family members were analysed together, given that participants had all attended the same focus group.
Similar to the analytical method detailed in a related study [Citation31], the first and second authors completed multiple readings of the transcript to identify relevant data and generate descriptive codes (Phase 1, according to Braun and Clarke). Related codes were clustered together (Phase 2) to create possible sub-themes and themes (Phase 3). These preliminary themes were reviewed with the third and last authors (Phase 4); questions and disagreements were documented and resolved through discussion to reach consensus on the final sub-themes and themes (Phase 5). Finally, all co-authors were involved in preparation of the manuscript to ensure participants’ experiences were presented with transparency and honesty.
Trustworthiness
Trustworthiness of the analysis included consideration of credibility, transferability, dependability and confirmability [Citation51]. A process of continual peer review and peer debriefing throughout all stages of analysis was important in establishing the dependability of the data. Confirmability was established through documentation of decisions relating to how data were coded. Team meetings were used to discuss possible sub-themes and themes as a form of peer review: the result of these discussions was consensus on the nature and wording of sub-themes and themes as well as decisions on whether a theme was relevant or distal to the research question. An audit trail of decisions and changes was maintained to show the evolution of the analysis. Purposive sampling of individuals with lived experience (that is, people with aphasia and their family members with experience of receiving hospital-based care post-stroke) contributed to the transferability and credibility of the data collected and analysed. Participants’ views and experiences are frequently reported verbatim in the results, in order to respectfully preserve their voices and to allow readers to draw their own conclusions. Occasionally, quotes are abbreviated (indicated by three full-stops, [Citation52]) to remove repetition or errors that might impede the reader’s understanding. At all times, care was taken not to deviate from the speaker’s intended message. Quotes were selected by the first author and reviewed by all co-authors.
Results
We generated five major themes and four subthemes:
Aphasia makes it hard to communicate;
Hospital staff focus on the patient’s medical status only;
Patients with aphasia do not get the help they need to improve;
Staff lack the skills to communicate with people with aphasia; and
Communicating with the healthcare team was a negative experience
Staff did not help patients with aphasia to communicate
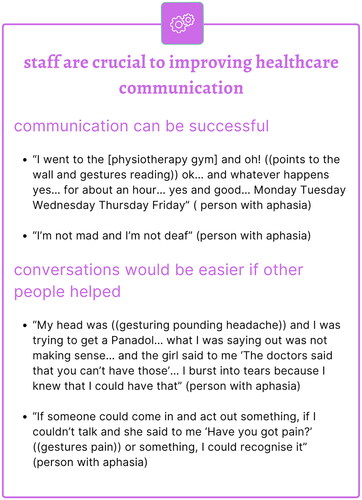
Staff are crucial to improving healthcare communication
Communication can be successful
Conversations would be easier if other people helped
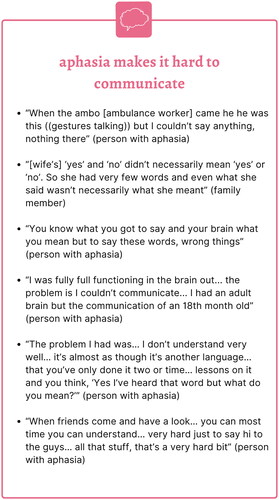
Major theme 1: aphasia makes it hard to communicate
The shock regarding the immediacy and totality of the disability associated with aphasia was evident: problematic, difficult healthcare communication started with the ambulance worker and prevailed throughout the hospital pathway: “When the ambo [ambulance worker] came he he was this ((gestures talking)) but I couldn’t say anything, nothing there” (person with aphasia_f4). In the acute phase, error production was high: “[wife’s] ‘yes’ and ‘no’ didn’t necessarily mean ‘yes’ or ‘no’. So she had very few words and even what she said wasn’t necessarily what she meant” (family member of person with aphasia_f4). These errors made it challenging to involve the patient with aphasia in healthcare discussions and decisions. There was a distressing discrepancy between persevered internal ability and impaired expressive output: “You know what you got to say and your brain what you mean but to say these words, wrong things” (person with aphasia_m1). As one participant with aphasia put it, “I was fully full functioning in the brain out… the problem is I couldn’t communicate… I had an adult brain but the communication of an 18th month old” (person with aphasia_f3). Comprehension also presented challenges to everyday communication, which further undermined self-efficacy for some participants: “The problem I had was… I don’t understand very well… it’s almost as though it’s another language… that you’ve only done it two or time… lessons on it and you think, ‘Yes I’ve heard that word but what do you mean?’” (person with aphasia_f3). Participants recalled that communication difficulties also impacted communication with those who were most familiar to them: “When friends come and have a look… you can most time you can understand… very hard just to say hi to the guys… all that stuff, that’s a very hard bit” (person with aphasia_m1). The inability to communicate left people feeling infantile, frustrated and disconnected. The expressive and receptive symptoms of aphasia had powerful and distressing impacts on participants’ attempts to connect with those around them. With the benefit of time and recovery, participants could communicate the strangeness of the early stages of aphasia ().
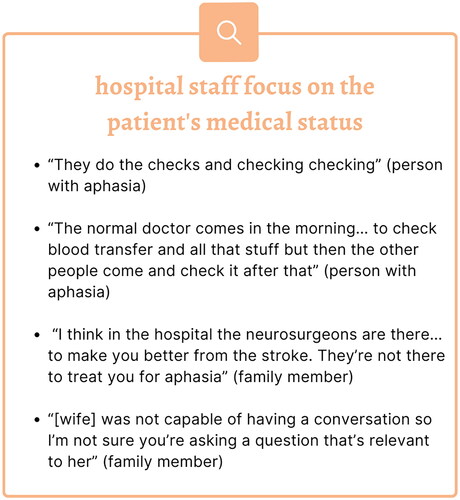
Major theme 2: hospital staff focus on the patient’s medical status only
Participants perceived that the main business of staff in the hospital was to manage the medical status of the patient and this did not include engaging in effective communication with the patient (“They do the checks and checking checking” and “the normal doctor comes in the morning… to check blood transfer and all that stuff but then the other people come and check it after that,” person with aphasia_m1). It is unclear whether these multiple checks represented clinical thoroughness or were redundant, but the need of such checks was perhaps not explained or understood. For one family member, the lack of communication between patients with aphasia and the medical team reflected the reality of hospital life. In hospital, particularly in the acute setting, medical matters dominate; as a family member said “I think in the hospital the neurosurgeons are there… to make you better from the stroke. They’re not there to treat you for aphasia” (family member of person with aphasia_f4). When discussing the experience of individuals with aphasia communicating with the healthcare team, this family member did not see it as a priority to involve the individual with aphasia in communication, “[wife] was not capable of having a conversation so I’m not sure you’re asking a question that’s relevant to her” (family member of person with aphasia_f4). While this did not reflect the opinions of the other participants in the group, it does serve to highlight that some patients or family members have different expectations about communication with the healthcare team in hospital.
All participants described conversations with healthcare providers as centred on the patient’s medical status, although there were some differences in their expectations about whether the patient with aphasia should be included in these conversations or not. There was an acceptance that stroke is a medical emergency and that a medical response is necessary; but for some participants, over-medicalisation led to a singular focus on medical tests, without seeing the patient as a whole ().
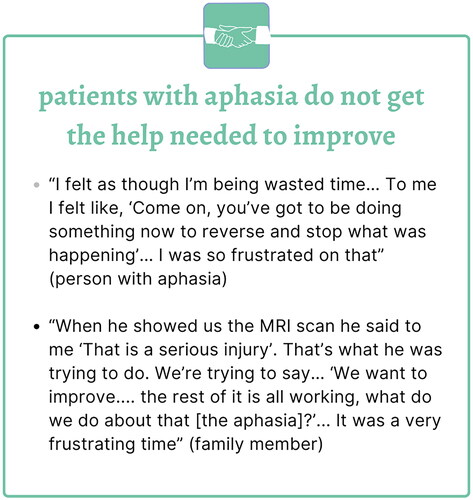
Major theme 3: patients with aphasia do not get the help they need to improve
Participants felt that they did not get enough help to improve. Once the medical emergency of limiting the damage caused by the stroke had been achieved, participants felt there was a reduced urgency to address the residual consequences of the stroke. The participants felt strongly that more action was needed in the days and weeks following the stroke, which led to feelings of impatience and frustration: “I felt as though I’m being wasted time… To me I felt like, ‘Come on, you’ve got to be doing something now to reverse and stop what was happening’… I was so frustrated on that” (person with aphasia_f3). Patients and family members were keen to work to improve the situation, yet they felt this approach was not shared with some of the healthcare team. As a result, patients and families felt frustrated that they were not given suggestions and advice on how to improve. One family member described how the specialist showed them a scan of the stroke and used this to rule out the possibility of improvement: “When he showed us the MRI scan he said to me ‘That is a serious injury’. That’s what he was trying to do. We’re trying to say… ‘We want to improve…. the rest of it is all working, what do we do about that [the aphasia]?’… It was a very frustrating time” (family member of person with aphasia_f3). Participants had busy lives, roles, ambitions and plans they longed to return to. Yet there was a sense of competing beliefs and goals between the healthcare team and the participants. Turning to some professionals for a robust recovery plan led to disappointment and frustration, with test results used as a reason to scale down hope and expectation. What may be viewed by healthcare staff as resource management or delivering prognostic information, was received by participants as the healthcare team not being on the same page as them ().
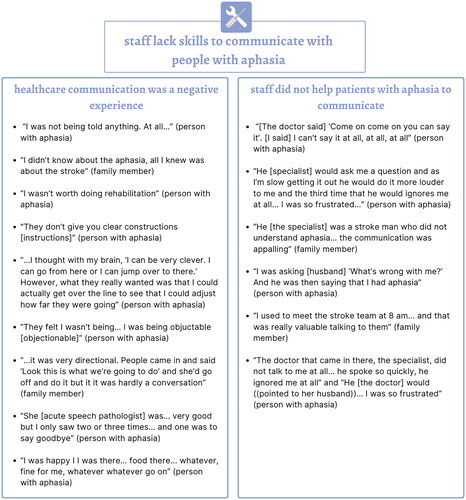
Major theme 4: staff lack the skills to communicate with people with aphasia
Despite some participants accepting that conversations would focus on their medical status and that they would not be included in these conversations (as described in Theme 2 above), others expected that staff would need to communicate with the patient with aphasia and that they would have the knowledge and skills to do so. However this was not the reality of participants’ experiences. Participants described a range of negative experiences communicating with the healthcare team and staff using ineffective strategies when attempting to help.
Communicating with the healthcare team was a negative experience
The healthcare team has expertise in stroke, but participants often had negative experiences communicating with them. There was a lack of information immediately post-stroke: “I was not being told anything. At all…” (person with aphasia_f3); “I didn’t know about the aphasia, all I knew was about the stroke” (family member of person with aphasia_f3). There was a sense that health professionals did not understand aphasia. One experience that was common to participants involved a medical professional pointing to his/her watch, without any explanation, in an attempt to elicit naming from the individual with aphasia. This resulted in confusion, as the individuals with aphasia were unsure what was required of them, i.e. was the correct answer “watch” or to provide the time? Yet their responses carried significant weight regarding prognosis and planning of services. When one participant failed to respond to the doctor’s impromptu language test, the doctor interpreted this as an indication that rehabilitation was not appropriate: “I wasn’t worth doing rehabilitation” (person with aphasia_f3).
Communication difficulties also arose in allied health intervention sessions: “they don’t give you clear constructions [instructions]” (person with aphasia_f3). An example of this related to the occupational therapist asking the participant to make a cup of tea for her husband, which she refused to do. She was unable to explain the reason for her refusal was that the only household chore her husband did was making her a cup of tea and she did not want him to discontinue this. Furthermore, during a physiotherapy session, the participant was asked to jump over a line but she wanted to show that she could do more: “…I thought with my brain ((points to head)), ‘I can be very clever. I can go from here or I can jump over to there.’ However, what they really wanted was that I could actually get over the line to see that I could adjust how far they were going” (person with aphasia_f3). In both situations, whether having a reasonable objection to the task or trying to over-deliver, the participant reflected that her behaviour was interpreted negatively: “They felt I wasn’t being… I was being objuctable [objectionable]” (person with aphasia_f3). Communication with the healthcare team was not collaborative and was often limited to patients following instructions and complying with tests. One family member recalled that communication with the person with aphasia was necessarily one-sided but that this was not a problem: “…it was very directional. People came in and said ‘Look this is what we’re going to do’ and she’d go off and do it but it it was hardly a conversation” (family member of person with aphasia_f4). Speech pathologists were often not available in the acute phase to support communication: “She [acute speech pathologist] was… very good but I only saw two or three times… and one was to say goodbye” (person with aphasia_f3). Only one participant with aphasia felt that her needs were met in hospital and seemed happy to take the role of a passive patient: “I was happy I I was there… food there… whatever, fine for me, whatever whatever go on” (person with aphasia_f4).
Staff did not help patients with aphasia to communicate
Participants recalled both difficulty communicating with health professionals and reduced opportunities to communicate, particularly with the doctors. Staff adapted their communication in ways that were not effective or facilitative. For example, one participant recalled the doctor coaxing her to encourage her to talk, but this was not an effective strategy: “[The doctor said] ‘Come on come on you can say it’. [I said] I can’t say it at all, at all, at all” (person with aphasia_f2). A participant with a comprehension deficit had experiences of members of the health team speaking more loudly to her: “He [specialist] would ask me a question and as I’m slow getting it out he would do it more louder to me and the third time that he would ignores me at all… I was so frustrated…” (person with aphasia_f3). Participants identified a distinction between knowledge and skill to manage stroke, and knowledge and skills to engage with someone with aphasia caused by the stroke: “He [the specialist] was a stroke man who did not understand aphasia… the communication was appalling” (family member of person with aphasia_f3).
Family members became an important conduit in the communication process: “I was asking [husband] ‘What’s wrong with me?’ And he was then saying that I had aphasia” (person with aphasia_f3). Family members became the main contact point between the patient with aphasia and the health team; this worked well as a method of getting information: “I used to meet the stroke team at 8 am… and that was really valuable talking to them” (family member of person with aphasia_f4). However, for participants with aphasia, being excluded from the communication chain led to frustration (“The doctor that came in there, the specialist, did not talk to me at all… he spoke so quickly, he ignored me at all” and “He [the doctor] would ((pointed to her husband))… I was so frustrated,” person with aphasia_f3).
There was an absence of evidence of person-centred care in participants’ recalls of their hospital experiences. Doctors in particular seemed to struggle to implement effective strategies to mitigate at least some of the symptoms of aphasia. In some cases, family members seem to replace patients as the focus of education and decision-making ().
Major theme 5: staff are crucial to improving healthcare communication
Communication can be successful
Participants did experience instances of effective communication, facilitated by environmental props or non-verbal communication. One participant with aphasia recalled how useful it was to see the therapy timetable displayed on the wall of the rehabilitation gym: “I went to the [physiotherapy gym] and oh! ((points to the wall and gestures reading)) ok… and whatever happens yes… for about an hour… yes and good… Monday Tuesday Wednesday Thursday Friday” (person with aphasia_f4). Furthermore, when staff attended to non-verbal communication, participants found they were able to express preferences and choices. For example, when the hospital catering staff visited the wards to offer hot drinks, one participant with aphasia recalled being able to point to, rather than verbalise, their preference for tea or coffee. Another participant with limited verbal output practised typing on her iPad so that she could communicate with the healthcare team. She was motivated to do this as she was frustrated with not receiving adequate support to communicate with the doctor. She recalled typing, “I’m not mad and I’m not deaf” (person with aphasia_f3) on her iPad and going to the specialist’s office to show him. None of the participants recalled any of the healthcare team using additional communication strategies such as writing, gesture, or verification strategies.
Conversations would be easier if other people helped
Participants felt communication would be improved if health professionals used strategies to support the patient’s comprehension and response. In the acute and sub-acute phases of stroke recovery, patients with aphasia might not have the cognitive flexibility to realise that their verbal output is problematic and that they need to switch to another means of communication. As one participant with aphasia put it, in the early days and weeks post-stroke, she was unable to problem-solve to try out different ways to let the nurse know she had a headache: “My head was ((gesturing pounding headache)) and I was trying to get a Panadol… what I was saying out was not making sense… and the girl said to me ‘The doctors said that you can’t have those’… I burst into tears because I knew that I could have that” (person with aphasia_f3). She suggested the nurse should have used gesture and offered choices to which the patient with aphasia could then respond: “If someone could come in and act out something, if I couldn’t talk and she said to me ‘Have you got pain?’ ((gestures pain)) or something, I could recognise it.” This participant with aphasia described this strategy as “charades” and saw it as the responsibility of the entire healthcare team to consistently use such strategies ().
Discussion
The current study investigated the experiences of individuals with aphasia and their family members regarding healthcare communication following a stroke. We generated five themes relating to the difficulty of engaging in healthcare communication with aphasia, unmet needs, lack of accessible communication opportunities, possibilities for improvement, and understanding the realities of the hospital environment. This study adds to the evidence base by giving voice to individuals with a range of aphasia types and severity and their family members.
It seems uncontroversial to state that aphasia can present serious challenges to effective healthcare communication [Citation31,Citation32,Citation53,Citation54] and findings from the current study re-enforce this. Participants in the current study expressed frustration, disappointment and concern regarding the lack of accessible communication within the hospital environment. Moreover, participants perceived this as a systemic lack of interest or ability to include them in healthcare-related communication. Nurses have reported valuing task-oriented communication that relates to their workload (for example, assessment, providing care, discussing discharge processes) rather than communication related to rapport-building [Citation30]. Yet in the current study, participants’ frustration was not related to communication as a ‘soft’ skill in relation to rapport-building; rather, patients’ needs were often unaddressed due to poor healthcare communication and lack of ways to mitigate the effects of aphasia. For example, pain management needs went unaddressed, patients were unaware they had aphasia and what that meant, and family members had to act as key advocates and conduits for communication with the treating healthcare team. Participants reported staff do not know how to help people with aphasia and either use inappropriate compensatory strategies (talking too loud, encouraging the person with aphasia to talk when it was not possible) or simply ignoring the patient with aphasia. Regarding doctors on the ward, participants in the current study had constrasting perspectives. Some expressed dissatisfaction that experienced stroke doctors did not know how to communicate with patients with aphasia, while a contrasting view was that it may be unrealistic to expect doctors to be skilled in communicating with patients with aphasia. However, the latter does not align with the expectations of the medical profession itself and regulatory bodies (e.g. [Citation18,Citation55]).
A novel finding from the current study relates to the potentially problematic nature of informal assessment used by health professionals. At times, the healthcare team gave instructions or requests that were unclear to patients, such as the doctor pointing to his/her watch or the physiotherapist asking the patient to jump over a line. When patients did not understand the purpose of the assessment, this was a source of not only frustration but also concern that opinions regarding eligibility for rehabilitation were being formed in a non-transparent way. Information needs were routinely not addressed in a tailored way. For example, formulating and delivering information about prognosis is complex [Citation56,Citation57] but participants in this study recalled the information being received as a shock and not within the context of an accessible, open, two-way conversation. Even when health professionals attempted to embed an assessment task in an everyday activity, such as the occupational therapist asking the patient to make a cup of tea for her husband, the patient’s own daily routines will influence whether this is an acceptable task or not. Such misunderstandings could lead to patients being viewed as non-compliant [Citation58]. For one couple with aphasia, there was a sense that the scan data of the brain lesion was a key determinant in whether the patient had rehabilitation potential and that the family member had to fight to advocate for access to rehabilitation.
Interestingly, the role of the speech pathologist was not a predominant theme in any of the participants’ experiences. Admittedly the focus group questions were not designed to specifically probe experiences of working with the speech pathologist; nonetheless the absence of the impact of the role is noteworthy. The literature suggests the role of the speech pathologist shifts throughout the stroke pathway, for example, in the acute phase of care, this role focuses mainly on dysphagia management [Citation59]. This aligns with the perceptions of participants in the current study that priority is given to managing medical status while other needs are neglected, such as those relating to education, engagement, and contributing to decision-making. There is a sense that the acute speech pathology service is restricted to screening and assessment [Citation59] and/or education and strategies rather than individual therapy [Citation31]. As argued elsewhere in the literature, there is potential to fundamentally redefine the role of hospital-based speech pathologists to focus on establishing healthcare communication, that is, working with staff and patients to establish at least a basic communication system in order to manage essential basic transactional and interactional needs [Citation21,Citation60,Citation61]. Interestingly, in the current study, the professional identity of an individual healthcare worker did not appear to influence participants’ expectations or experiences; on the whole, individuals with aphasia agreed that the healthcare team should have the knowledge and skills needed to adjust communicate for someone with aphasia. The lack of speech pathology service was not a source of complaint for participants in the current study; that is, patients’ dissatisfaction did not specifically relate to a lack of speech pathology intervention, but more the lack of accessible information and conversations with the wider team.
Findings from the current study highlight the discrepancy between the experiences and expectations of the stroke pathway by individuals with aphasia and their family members and by the treating healthcare team. Participants expressed alarm, impatience, distress and a sense of urgency. There was a sense of time being wasted in the early days and weeks post-stroke, with patients and family members lacking guidance or counselling. This is not something that has been reported by health professionals (e.g. [Citation31,Citation53]), who are trained in, and exposed on a daily basis, to medical emergencies. Nonetheless, staff want to help and feel distressed when they feel restricted by lack of time, resources, training or skills [Citation31]. Healthcare workers are operating in a non-optimal environment (time not available for staff-patient interaction, lack of access to readily available materials) and feel insufficiently skilled to interact with patients with aphasia; this leads to staff dreading, limiting or avoiding talking with patients with aphasia and to patients experiencing poorer quality of care and dissatisfaction with the service they received [Citation31,Citation53,Citation62]. What is missing is protected time in the clinical environment to tailor information and healthcare conversations to the individual patient. Sundin and Jansson [Citation63] describe “understanding and being understood” as a basic foundation within care (p.107). They elaborate that caring is an interaction, a dialogue between the patient and care giver, where they work together to create action. Participants in the current study did not appear to recall being included in a meaningful dialogue with the healthcare team.
Taken together, this evidence suggests a relatively inflexible system where patients are expected to fit into a one-size-fits-all model of communication. This has been echoed elsewhere by individuals with aphasia and their carers who report being regarded as “just a number” [Citation53,p.7]. This represents a dehumanising of healthcare, with a reductionist view of the body as a collection of medical symptoms [Citation64–66]. Pound and Jensen [Citation65] highlight the pitfalls of fragmenting the human experience into fixed domains: “Without a more nuanced, inclusive view of human experience, healthcare practitioners may inadvertently operate within artificially narrowed boundaries of the practical, the doable and the visible and therefore be less well equipped to respond with creativity and curiosity” (p.1229). A fragmented approach focusing on “the practical, the doable and the visible” may explain why participants in the current study and elsewhere report dissatisfaction with healthcare services and, on occasion, safety concerns [Citation29,Citation54]. Evidence from the stroke multidisciplinary team suggests that healthcare workers do indeed focus on the practical, doable and visible (e.g. [Citation31]), which likely reflects the organisational environment. Hospital systems are designed for fast-paced judgements and decisions, while internal structures and processes promote efficiency. Models of person-centred care should ensure that care is wrapped around the patient; instead, patients with aphasia report an inflexible experience of care that prioritises physical care tasks (which may require little or no communication with the patient). Patients whose injuries require adjusted communication are vulnerable to being poorly treated as a result of a ruthlessly efficient and overburdened system. As a result, these patients are at increased risk of adverse events and falls [Citation25,Citation67,Citation68]. Roter and Hall [Citation69] argue that medical care has two fundamental ingredients: the first is the expert knowledge of the clinician and patient, the second is communication. The absence, then, of effective communication could result in reduced quality of care and poorer health outcomes. Given the increasing presence and acceptance of eHealth and mHealth platforms, future clinical research could harness the potential utility of technology to allow healthcare professionals to access resources and advice in real time to help them to engage patients with aphasia in healthcare-related discussions. In order to affect meaningful change within the hospital system, technological innovation should be developed with input from consumers including patients and staff, and embedded within centralised team processes.
The current study found that individuals with aphasia and family members think the healthcare team should have the skills to communicate with patients with communication disorders and be prepared to change their usual communication style to accommodate these patients, as echoed elsewhere in the literature [Citation62]. What might be a solution to this impasse? Providing care to patients with communication difficulties is challenging [Citation24] and requires a different approach to planning care for patients without communication difficulties. Instead of focusing on aphasia as a symptom of stroke and as a target for therapy later in the care pathway, aphasia could be viewed as an immediate obstacle to providing person-centred care. This obstacle could be mitigated by optimising the immediate environment so as to compensate for the language impairment, e.g. assessment of healthcare communication [Citation70]. Providing training and tools is obvious, but on its own, unlikely to lead to behavioural and cultural change on the ward. Hemsley and Balandin [Citation71] caution that we need to consider the multiple barriers to uptake of communication tools in hospitals, as well as the need for comprehensive evaluation of any such interventions in order to persuade hospital services of the need for investment. Systemic interventions are called for in order to shift the hospital and ward culture towards an “institutional culture of partnership” [Citation34,p.544). Hospital policies and procedures should be developed so that communication-vulnerable patients are identified on admission [Citation61] and consideration given to how practical care tasks can be balanced with time for clinician-patient interaction [Citation34]. O’Halloran, Grohn, et al. [Citation61] recommend embedding the prioritisation and value of communication in staff recruitment and promotion. For existing staff, ongoing education and training should be delivered in a variety of formats, including formal training as well as on-the-job training via shadowing and case conferences. Such training should include not only communication strategies but also staff’s roles in creating opportunities for communication [Citation61]. Ultimately, healthcare communication is a central and key part of delivering person-centred care. For all patients, and particularly those with communication disability, any threats to healthcare communication should be viewed as relevant to all healthcare professionals, with implementation of system-level solutions required to move the needle on patient experience and safety.
Limitations
The current study presents data from a small number of participants within one metropolitan area in Australia, collected for the purposes of guiding the development of a mHealth application in November 2016. Despite the window of time between data collection and publication, unfortunately there is nothing to suggest that the experiences of individuals with aphasia and their family members have improved, particularly following the COVID pandemic and its impact on healthcare. Therefore, we suggest the findings of the study may continue to reflect hospital experiences for some individuals with aphasia and their families. Individuals living with aphasia from different linguistic and cultural backgrounds, as well as from regional and remote areas, are likely to have different experiences of receiving post-stroke care; their inclusion would have strengthened the relevance of the findings. We acknowledge that those participants who consented to join the study may hold particularly strong feelings about post-stroke healthcare communication. However, the participant with severe aphasia and her husband consistently reported feeling happy with the level of communication, representing a contrasting but nonetheless valid view.
See Appendix 1 for an aphasia-friendly summary of this paper. A draft of this summary was shared with the participants and their feedback incorporated in the final version.
Supplemental Material
Download PDF (415.8 KB)Supplemental Material
Download MS Word (1.4 MB)Acknowledgements
The authors warmly thank the participants who generously shared their experiences and time; efforts have been made to relay these experiences honestly and respectfully. Special thanks to research assistants Chiara Scarpelli who took field notes during the focus group and to Hien My Pham who spent many hours transcribing the data. The authors acknowledge funding support from La Trobe University’s Building Healthy Communities Research Focus Area.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Australian Commission on Safety and Quality in Health Care (ACSQHC). Patient-centred care: improving quality and safety through partnerships with patients and consumers. Sydney, Australia; 2011.
- Eklund JH, Holmström IK, Kumlin T, et al. “Same same or different?” A review of reviews of person-centered and patient-centered care. Patient Educ Couns. 2019;102(1):3–11. doi:10.1016/j.pec.2018.08.029.
- Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century: a new health system for the 21st century. USA: National Academies Press; 2001. http://ebookcentral.proquest.com/lib/latrobe/detail.action?docID=3375215.
- National Health Service. Creating a patientled NHS – delivering the NHS improvement plan. UK: NHS Confederation Briefing; 2005.
- US Department of Health and Human Services. Personalized health care: pioneers, partnerships, progress. Washington (DC): US Department of Health and Human Services; 2008.
- Davis K, Schoenbaum SC, Audet A. A 2020 vision of patient-centred primary care. J Gen Intern Med. 2005;20(10):953–957. doi:10.1111/j.1525-1497.2005.0178.x.
- Robinson JH, Callister LC, Berry JA, et al. Patient-centered care and adherence: definitions and applications to improve outcomes. J Am Acad Nurse Pract. 2008;20(12):600–607. doi:10.1111/j.1745-7599.2008.00360.x.
- Bensing JM, Verhaak PFM, van Dulmen AM, et al. Communication: the royal pathway to patient-centered medicine. Patient Educ Couns. 2000;39(1):1–3. doi:10.1016/S0738-3991(99)00107-X.
- Kitson A, Marshall A, Bassett K, et al. What are the core elements of patient-centred care? A narrative review and synthesis of the literature from health policy, medicine and nursing: core elements of patient-centred care. J Adv Nurs. 2013;69(1):4–15. doi:10.1111/j.1365-2648.2012.06064.x.
- McCormack B, McCance T. Development of a framework for person-centred nursing. J Adv Nurs. 2006;56(5):472–479. doi:10.1111/j.1365-2648.2006.04042.x.
- Picker Institute. Eight dimensions of patient-centred care. UK: PIcker Institute; 2008.
- DiMatteo MR, Taranta A, Friedman HS, et al. Predicting patient satisfaction from physicians’ nonverbal communication skills. Med Care. 1980;18(4):376–387. doi:10.1097/00005650-198004000-00003.
- Jackson JL, Chamberlin J, Kroenke K. Predictors of patient satisfaction. Soc Sci Med. 2001;52(4):609–620. doi:10.1016/S0277-9536(00)00164-7.
- Lee S, Groß SE, Pfaff H, et al. Waiting time, communication quality, and patient satisfaction: an analysis of moderating influences on the relationship between perceived waiting time and the satisfaction of breast cancer patients during their inpatient stay. Patient Educ Couns. 2020;103(4):819–825. doi:10.1016/j.pec.2019.11.018.
- Burgener AM. Enhancing communication to improve patient safety and to increase patient satisfaction. Health Care Manag (Frederick). 2020;39(3):128–132. doi:10.1097/HCM.0000000000000165.
- Leonard M, Graham S, Bonacum D. The human factor: the critical importance of effective teamwork and communication in providing safe care. Qual Saf Health Care. 2004;13(suppl_1):i85–i90. doi:10.1136/qshc.2004.010033.
- Street RL, Makoul G, Arora NK, et al. How does communication heal? Pathways linking clinician–patient communication to health outcomes. Patient Educ Couns. 2009;74(3):295–301. doi:10.1016/j.pec.2008.11.015.
- Australian Commission on Safety and Quality in Health Care (ACSQHC). Sydney (Australia): National Safety and Quality Health Service Standards; 2017.
- Patak L, Wilson-Stronks A, Costello J, et al. Improving patient-Provider communication: a call to action. J Nurs Adm. 2009;39(9):372–376. doi:10.1097/NNA.0b013e3181b414ca.
- The Joint Commission. Advancing effective communication, cultural competence, and patient-and family-centered care: a roadmap for hospitals. United States: The Joint Commission.
- Hemsley B, Balandin S, Togher L. Creating a communicative environment in hospital for adults with developmental disability and complex communication needs. ACQuiring Knowledge in Speech, Language & Hearing. 2010;12(3):108–111.
- Murphy J. Perceptions of communication between people with communication disability and general practice staff. Health Expect. 2006;9(1):49–59. doi:10.1111/j.1369-7625.2006.00366.x.
- O’Halloran R, Worrall L, Hickson L. Stroke patients communicating their healthcare needs in hospital: a study within the ICF framework. Int J Lang Commun Disord. 2012;47(2):130–143. doi:10.1111/j.1460-6984.2011.00077.x.
- Stransky ML, Jensen KM, Morris M. Adults with communication disabilities experience poorer health and healthcare outcomes compared to persons without communication disabilities. J Gen Intern Med. 2018;33(12):2147–2155. doi:10.1007/s11606-018-4625-1.
- Bartlett G, Blais R, Tamblyn R, et al. Impact of patient communication problems on the risk of preventable adverse events in acute care settings. CMAJ. 2008;178(12):1555–1562. doi:10.1503/cmaj.070690.
- Flowers HLP, Skoretz SAP, Silver FLMD, et al. Poststroke aphasia frequency, recovery, and outcomes: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2015;97(12):2188–2201.e8. doi:10.1016/j.apmr.2016.03.006.
- Manning M, MacFarlane A, Hickey A, et al. Perspectives of people with aphasia post-stroke towards personal recovery and living successfully: a systematic review and thematic synthesis. PLoS One. 2019;14(3):e0214200-e0214200. doi:10.1371/journal.pone.0214200.
- van Rijssen M, Isaksen J, Vandenborre D, et al. Ways to improve communication and support in healthcare centres according to people with aphasia and their relatives: a Dutch perspective. Aphasiology. 2021;37(1):69–82. doi:10.1080/02687038.2021.1988505.
- Tomkins B, Siyambalapitiya S, Worrall L. What do people with aphasia think about their health care? Factors influencing satisfaction and dissatisfaction. Aphasiology. 2013;27(8):972–991. doi:10.1080/02687038.2013.811211.
- Chan EA, Jones A, Fung S, et al. Nurses’ perception of time availability in patient communication in Hong Kong. J Clin Nurs. 2011;21(7–8):1168–1177. doi:10.1111/j.1365-2702.2011.03841.x.
- Carragher M, Steel G, O’Halloran R, et al. Aphasia disrupts usual care: the stroke team’s perceptions of delivering healthcare to patients with aphasia. Disabil Rehabil. 2020;43(21):3003–3014. doi:10.1080/09638288.2020.1722264.
- van Rijssen MN, Veldkamp M, Bryon E, et al. How do healthcare professionals experience communication with people with aphasia and what content should communication partner training entail? Disabil Rehabil. 2022;44(14):3671–3678. doi:10.1080/09638288.2021.1878561.
- Bright FAS, Reeves B. Creating therapeutic relationships through communication: a qualitative metasynthesis from the perspectives of people with communication impairment after stroke. Disabil Rehabil. 2022;44(12):2670–2682. doi:10.1080/09638288.2020.1849419.
- Gordon C, Ellis-Hill C, Ashburn A. The use of conversational analysis: nurse-patient interaction in communication disability after stroke. J Adv Nurs. 2009;65(3):544–553. doi:10.1111/j.1365-2648.2008.04917.x.
- O’Halloran R, Worrall L, Hickson L. Environmental factors that influence communciation between patients and their healthcare providers in acute hospital stroke units: an observational study. Int J Lang Commun Disord. 2011;46(1):30–47. doi:10.3109/13682821003660380.
- Hersh D, Godecke E, Armstrong E, et al. “Ward talk”: nurse’ interaction with people with and without aphasia in the very early period poststroke. Aphasiology. 2016;30(5):609–628. doi:10.1080/02687038.2014.933520.
- Elko S, Velez JA, Corwin M, et al. Rethinking patient–provider care through visual communication. Visual Communication. 2020;21(1):176–192. doi:10.1177/1470357220915605.
- Smith S. Hospital Talk (Version 1.1). 2016. https://itunes.apple.com/au/app/hospital-talk/id1131978841?mt=8.
- Strubbia C, Levack WMM, Grainger R, et al. Use of an iPad app (aid for decision-making in occupational choice) for collaborative goal setting in interprofessional rehabilitation: qualitative descriptive study. JMIR Rehabil Assist Technol. 2021;8(4):e33027. doi:10.2196/33027.
- Sharpe B, Hemsley B. Improving nurse–patient communication with patients with communication impairments: hospital nurses’ views on the feasibility of using mobile communication technologies. Appl Nurs Res. 2016;30:228–236. doi:10.1016/j.apnr.2015.11.012.
- Asadzadeh A, Kalankesh LR. A scope of mobile health solutions in COVID-19 pandemics. Inform Med Unlocked. 2021;23:100558. doi:10.1016/j.imu.2021.100558.
- Marcolino MS, Oliveira JAQ, D’Agostino M, et al. The impact of mHealth interventions: systematic review of systematic reviews. JMIR Mhealth Uhealth. 2018;6(1):e23. doi:10.2196/mhealth.8873.
- Crotty MJ. The foundations of social research. 1st ed. Thousand Oaks: SAGE Publications Ltd.; 1998.
- Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–357. doi:10.1093/intqhc/mzm042.
- Brennan A, Worrall L, McKenna K. The relationship between specific features of aphasia-friendly written material and comprehension of written material for people with aphasia: an exploratory study. Aphasiology. 2005;19(8):693–711. doi:10.1080/02687030444000958.
- Rose T, Worrall L, McKenna K. The effectiveness of aphasia-friendly principles for printed health education materials for people with aphasia following stroke. Aphasiology. 2003;17(10):947–963. doi:10.1080/02687030344000319.
- Rose TA, Worrall LE, Hickson LM, et al. Aphasia friendly written health information: content and design characteristics. Int J Speech Lang Pathol. 2011;13(4):335–347. doi:10.3109/17549507.2011.560396.
- Kagan A. Supported conversation for adults with aphasia: methods and resources for training conversation partners. Aphasiology. 1998;12(9):816–830. doi:10.1080/02687039808249575.
- Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology,. 2006;3(2):77–101. doi:10.1191/1478088706qp063oa.
- Patton MQ. Qualitative evaluation and research methods. 2nd ed. Newbury Park (CA): Sage; 1990.
- Lincoln YS, Guba EG. 1985. Naturalistic inquiry. Thousand Oaks: Sage Publications.
- Braun V, Clarke V. Thematic analysis. In: Cooper H, Camic PM, Long DL, et al, editors. APA handbook of research methods in psychology, Vol. 2. Research designs: quantitative, qualitative, neuropsychological, and biological. Washington (DC): American Psychological Association; 2012. p. 57–71.
- Clancy L, Povey R, Rodham K. “Living in a foreign country”: experiences of staff–patient communication in inpatient stroke settings for people with post-stroke aphasia and those supporting them. Disabil Rehabil. 2018;42(3):324–334. doi:10.1080/09638288.2018.1497716.
- Hemsley B, Werninck M, Worrall L. “That really shouldn’t have happened”: people with aphasia and their spouses narrate adverse events in hospital. Aphasiology. 2013;27(6):706–722. doi:10.1080/02687038.2012.748181.
- Ha JH, Longnecker N. Doctor-patient communication: a review. Ochsner J. 2010;10:38–43.
- Cheng BBY, Ryan BJ, Copland DA, et al. Prognostication in post-stroke aphasia: perspectives of people with aphasia on receiving information about recovery. Neuropsychol Rehabil. 2022;33(5):871–902. doi:10.1080/09602011.2022.2051565.
- Cheng BBY, Worrall L, Copland DA, et al. Prognostication in post-stroke aphasia: how do speech pathologists formulate and deliver information about recovery? Int J Lang Commun Disord. 2020;55(4):520–536. doi:10.1111/1460-6984.12534.
- Sinkfield-Morey T. How using the term ‘non-compliant’ keeps providers from partnering with patients. Creative Nursing. 2018;24(3):178–185. doi:10.1891/1946-6560.24.3.178.
- Foster A, Worrall L, Rose M, et al. ‘I do the best I can’: an in-depth exploration of the aphasia management pathway in the acute hospital setting. Disabil Rehabil. 2016;38(18):1765–1779. doi:10.3109/09638288.2015.1107766.
- McCooey-O’Halloran R, Worrall L, Hickson L. Evaluating the role of speech-language pathology with patients with communication disability in the acute care hospital setting using the ICF. J Med Speech-Language Pathol. 2004;12(2):49–58.
- O’Halloran R, Grohn B, Worrall L. Environmental factors that influence communication for patients with a communication disability in acute hospital stroke units: a qualitative metasynthesis. Arch Phys Med Rehabil. 2012;93(1 Suppl):S77–S85. doi:10.1016/j.apmr.2011.06.039.
- Burns M, Baylor C, Dudgeon B, et al. Asking the stakeholders: perspectives of individuals with aphasia, their family members, and physicians regarding communication in medical interactions. Am J Speech Lang Pathol. 2015;24(3):341–357. doi:10.1044/2015_AJSLP-14-0051.
- Sundin K, Jansson L. Understanding and being understood’ as a creative caring phenomenon - in care of patients with stroke and aphasia. J Clin Nurs. 2003;12(1):107–116. doi:10.1046/j.1365-2702.2003.00676.x.
- Pound C, Duchan J, Penman T, et al. Communication access to organisations: inclusionary practices for people with aphasia. Aphasiology. 2007;21(1):23–38. doi:10.1080/02687030600798212.
- Pound C, Jensen LR. Humanising communication between nursing staff and patients with aphasia: potential contributions of the humanisation values framework. Aphasiology. 2018;32(10):1225–1249. doi:10.1080/02687038.2018.1494817.
- Todres L, Galvin KT, Holloway I. The humanization of healthcare: a value framework for qualitative research. Int J Qual Stud Health Well-Being. 2009;4(2):68–77. doi:10.1080/17482620802646204.
- Hemsley B, Steel J, Worrall L, et al. A systematic review of falls in hospital for patients with communication disability: highlighting an invisible population. J Safety Res. 2019;68:89–105. doi:10.1016/j.jsr.2018.11.004.
- Sullivan R, Harding K. Do patients with severe post-stroke communication difficulties have a higher incidence of falls during inpatient rehabilitation? A retrospective cohort study. Top Stroke Rehabil. 2019;26(4):288–293. doi:10.1080/10749357.2019.1591689.
- Roter DL, Hall JA. 2006). Doctors talking with patients/patients talking with doctors. 2nd ed. Westport (CT): Praeger.
- O’Halloran R, Worrall L, Toffolo D, et al. Inpatient functional communication interview: screening, assessment and intervention. San Diego: Plural Publishing Inc.; 2019.
- Hemsley B, Balandin S. A metasynthesis of patient-provider communication in hospital for patients with severe communication disabilities: informing new translational research. Augment Altern Commun. 2014;30(4):329–343. doi:10.3109/07434618.2014.955614.