Abstract
Purpose
Hypermobile Ehlers-Danlos Syndrome (hEDS) and hypermobility spectrum disorder (HSD) are painful, chronic and multi-systemic conditions. No online pain management programs for hEDS/HSD currently exist. We aimed to develop one by exploring what people with hEDS/HSD want in such programs.
Materials and methods
A Delphi was conducted via online surveys of stakeholders: participants with hEDS/HSD and healthcare professionals (HCP). In survey 1, participants were asked if a hEDS/HSD-specific online pain management program was important, listing up to 20 topics important to know about pain. In survey 2, participants rated the importance of those topics. Consensus was set as ≥75% rating of at least “important”. Using topics that reached consensus, the online program was developed. Usability testing was performed using the Systems Usability Scale (SUS).
Results
396 hEDS/HSD and 29 HCP completed survey 1; 151 hEDS/HSD and 12 HCP completed survey 2. 81% of hEDS/HSD and 69% of HCP rated a hEDS/HSD-specific program as at least “important”. Thirty-five topics reached consensus to guide content for the HOPE program (Hypermobile Online Pain managemEnt). SUS score was 82.5, corresponding to “high acceptability”.
Conclusions
A hEDS/HSD-specific online pain management program is important to stakeholders. Utilising a Delphi approach to incorporate stakeholder input, an evidence-informed and user appropriate program was developed.
IMPLICATIONS FOR REHABILITATION
Pain is one of the most common and impactful symptom affecting those with Hypermobile Ehlers-Danlos Syndrome (hEDS) and hypermobility spectrum disorder (HSD).
Online pain management programs are effective in other chronic conditions such as Fibromyalgia and Rheumatoid Arthritis, but there are no programs specific for hEDS/HSD.
People with hEDS or HSD and healthcare professionals with experience in these conditions feel that an online pain management program specific to their condition is important; consensus revealed thirty-five key topics important to these stakeholders.
The first hEDS/HSD-specific online pain management program, called HOPE, was developed with stakeholder input and usability tested, ready for clinical trial testing.
Introduction
Ehlers-Danlos Syndromes (EDS) are a group of heritable connective tissue conditions. Chronic pain is reported in up to 90% in these groups [Citation1,Citation2], approximately three times more than general population-based estimates [Citation3]. Pain mechanisms in EDS are complex and enigmatic, including a combination of nociceptive, neuropathic and nociplastic pain [Citation4]. The interplay between these pain mechanisms in EDS are unique, as multiple mechanisms often contribute to each pain episode (e.g. recurrent acute on chronic injuries), and numerous body systems are simultaneously involved (e.g. musculoskeletal, autonomic, neurological, gastrointestinal). Given this unique complexity, people with EDS struggle to understand and manage their pain [Citation5]. There is evidence to support that EDS-specific multidisciplinary pain management programs are effective [Citation6–8]. However, the ones empirically tested are mostly in-person and are not easily accessible. To the authors knowledge, there are only two studies looking at online treatment for people with EDS that included pain outcome measures [Citation9,Citation10]. However, these two studies used very specific psychology interventions (one using Positive Psychology Interventions and the other using meditation). There is a need for readily accessible EDS-specific pain management strategies that adopt multidisciplinary or a wider biopsychosocial approach.
Online pain management programs are easily accessible and significantly improve pain intensity, health-related quality of life and depression in chronic, widespread musculoskeletal conditions [Citation11]. These programs are generic [Citation12,Citation13] or condition-specific [Citation14,Citation15]. They include pain education (e.g. pain neuroscience or condition-specific pain education) and/or management strategies (e.g. cognitive, behavioural or coping strategies, symptom management or problem-solving skills). However, their effects have not been explored in EDS and there are no EDS-specific programs incorporating comprehensive stakeholder input currently available [Citation11].
While EDS clinical guidelines recommend pain management strategies [Citation16,Citation17], these guidelines omit the views of people with EDS. There is one qualitative study using focus group interviews of patients and researchers that provide stakeholder recommendations for self-management interventions. Participants wanted tailored education about the condition, pain control and self-help strategies [Citation18]. Engagement with stakeholders, namely those with lived experience and healthcare professionals or researchers with relevant clinical expertise, will enrich the content development of EDS-specific online pain management programs [Citation19]. Using an online, anonymous, Delphi method permits consensus-building and equal opportunity for each participant to provide feedback [Citation20]. Stakeholder involvement through consensus building aligns the program content to current needs, facilitating program engagement and relevance [Citation21], especially since EDS subgroups are clinically different and have unique pain management needs.
Hypermobile-EDS (hEDS) is the most common subgroup of EDS. The diagnosis of hEDS is based on the 2017 EDS International Classification [Citation22]. Another hypermobility condition presenting similarly to hEDS but not fitting the diagnostic criteria is hypermobility spectrum disorder (HSD). This diagnosis is made after ruling out differential diagnoses, including hEDS. Population studies suggest that their collective prevalence may be as high as 1 in 500 [Citation23]. Therefore, we have chosen to focus on hEDS and HSD.
The aims of this study were threefold: 1) collect opinion and determine consensus from stakeholders about topics they consider important for a hEDS/HSD-specific online pain management program, 2) develop an online pain management program, and 3) alpha-test the program for usability.
Methods
Overview
This study comprised of three stages to address the three aims. The first stage included two online surveys - the first survey to collect stakeholder opinion and a follow-up survey for consensus making. The second stage involved the development of the online pain management program. The third stage was an alpha-testing of the website. The project was approved by Macquarie University’s human research ethics committee (reference number 520221219241862).
Participants and recruitment
Stage 1: Delphi surveys 1 and 2
Inclusion criteria stipulated that hEDS/HSD participants be 18 years or older, diagnosed with hEDS/HSD (or previously known as Joint Hypermobility Syndrome/EDS-hypermobile type) by a medical doctor. We excluded participants who did not have access or adequate skills to navigate the internet and/or computer, who were unable to provide informed consent online and who were not able to read and/or communicate adequately in English. We also included healthcare professionals (HCP) with at least five years of experience treating individuals with hEDS/HSD and/or conducting hEDS/HSD-related research. We sought 20 participants from each group of stakeholders. Participants were recruited through advertisements on Facebook groups, the Ehlers-Danlos Society page and their social media pages, emails to HCP and clinics/hospitals in the HCP directory available on the EDS Society webpage, and online search of medical researchers of hEDS/HSD whose contact details were publicly available.
Stage 2
No participants were involved in stage 2 as this stage was focused on program development.
Stage 3
Inclusion criteria for usability testers were final year or recent (within 4-years) graduates from physiotherapy or medicine from the university. We sought five participants through advertisements on their online university community announcement page. We chose this sample of convenience as respondents to other online studies of hEDS and HSD participants are often younger and educated, with 52% to 81% reporting at least university level education [Citation24–26].
Procedures
The modified Delphi method was guided by recommendations from Conducting and Reporting Delphi Studies [Citation27] using an online survey (). Similar approaches have been used in other health conditions [Citation28–30]. Two or three rounds of consensus-making have been recommended, so we chose two rounds due to time and resources available [Citation31]. Three of the authors (EI, LN and CC) have previous experience with the utilization of the Delphi technique in clinical research. Both rounds of anonymized surveys were tested by all authors before they were made available to consenting participants. At the end of survey 1, participants were given the option to take part in survey 2 and their email addresses were collected on a separate link so that all responses were anonymous. We analyzed only the surveys of participants who completed and submitted their responses to each survey. Stage 1 surveys were conducted on LimeSurvey [Citation32] and stage 3 on Research Electronic Data Capture (REDCap) [Citation33,Citation34] as technical functions in REDCap were better suited for this survey.
Figure 1. Flowchart of Delphi process. HCP = Healthcare professional, hEDS = hypermobile Ehlers-Danlos Syndrome, HSD = Hypermobility Spectrum Disorder.
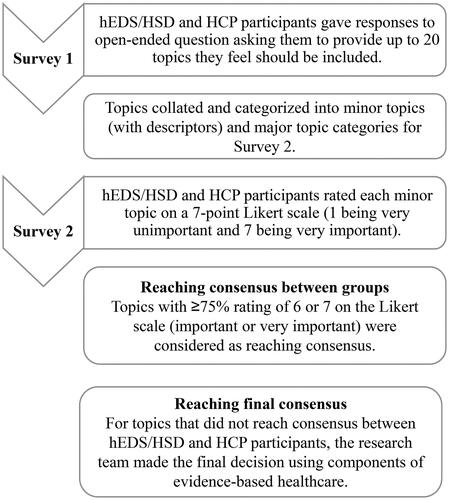
Stage 1: Delphi surveys 1 and 2
Survey 1
This survey asked participants to: i) list up to 20 of the most important, but not necessarily in order of importance, topics/information that people with hEDS/HSD should know about their pain to aid self-management (see supplement A); ii) rate the importance of a condition-specific program on a 7-point Likert scale (very important to very unimportant); and iii) provide their opinion on program parameters including: length of the program, frequency, the importance of online HCP contact as part of the program and how regular it should be (Supplement A). Additionally, only hEDS/HSD participants were asked to rate the importance of including quizzes, real-life case examples and online discussion forums. Responses were collated using Microsoft Excel (Version 16.79.2, United States). Responses were individually analyzed by two authors (MTC and either EI, LN or CC) who grouped them into minor topics using single concepts, and any disagreements in grouping were resolved by discussion. The authors then discussed the naming of each minor topic and came up with questions to elaborate on each concept to help participants understand each minor topic. The authors grouped related minor topics into major topics to allow a clearer presentation in survey 2 (Supplement A). Consensus by the authors was reached on all topics before presenting the list of topics to participants in survey 2.
Survey 2
Participants were asked to rate the importance of each minor topic using a 7-point Likert scale (very important to very unimportant). A priori consensus was set as ≥75% of participants rating a minor topic at least as “important” (i.e., 6 or 7 on the Likert scale) for that minor topic to be placed into consideration for inclusion in the program. Reminder emails were sent to both groups of participants before the closing date of survey 2. Where there was a lack of concordance in topics to be included between groups according to the a priori consensus level, the authors made the final decision on whether to include the topic.
Stage 2: Program development
To create the content for the program, Hypermobile Online Pain ManagemEnt (HOPE), the authors used topics that reached consensus through the Delphi surveys. All content was written and edited by MTC, EI, LN and CC. MTC and CC are practicing Physiotherapists and researchers in hEDS/HSD. Specific content review was provided by a rheumatologist with expertise in hEDS/HSD. The authors also sought external advice for certain topics that required medical expertise. The program was built on the WordPress platform, with the LearnDash (Liquid Web, 2023) Learning Management System (LMS) plugin. WordPress was chosen based on the availability of local expertise and resources. The website was managed by Macquarie University’s Research Data and Software (RDS) team. Due to the sensitive nature of the website, login with 2-factor authentication for security was required.
Stage 3: Alpha-testing
Feedback about the usability of the website was obtained using the Systems Usability Scale (SUS) [Citation35–37], presented as an online survey using REDCap. Following each question of the SUS, testers who rated items negatively (e.g. strongly disagree) were given an opportunity to provide suggestions on how to improve that aspect of usability. A last question “How can we improve on the user-friendliness of this website” was included to seek any other feedback. Participants were provided with a $50AUD electronic gift card as an appreciation of their time in testing the usability of the website.
Data analysis
Data analysis using Microsoft Excel enabled descriptive analysis for participant demographics (age, gender identity, country), response rates and drop-out rates. Percentages for ratings and consensus results (with their means ± standard deviations) were calculated using Excel. The SUS scoring and analysis were performed using a recommended scoring equation (38), on Excel. Score interpretation was performed based on a curved grading scale for the SUS [Citation37,Citation38].
Results
Stage 1: Delphi survey 1 participant numbers and demographics
Survey 1 for hEDS/HSD participants, planned for six weeks from September to November 2022, was closed after four weeks due to exceeding our planned recruitment number.
Out of 669 hEDS/HSD responses to survey 1, 408 were complete (). Of the 408, 12 did not meet our inclusion criteria of being diagnosed by a medical practitioner, leaving 396 completed and eligible surveys for analysis. Out of 44 HCP responses, 32 were complete (). From these, three were excluded as they did not have at least five years of experience working with hEDS/HSD, leaving 29 completed and eligible surveys for analysis. Participant demographics are shown in .
Figure 2. Participant response rate flowchart. HCP = Healthcare professional, hEDS = hypermobile Ehlers-Danlos Syndrome, HSD = hypermobility spectrum disorder, SD = standard deviation.
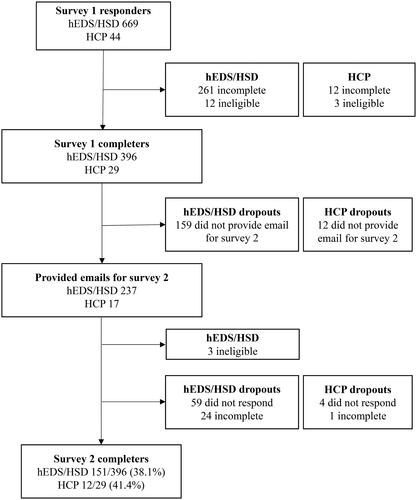
Table 1. HCP and hEDS/HSD participant demographics.
Stage 1: Survey 1 topic results
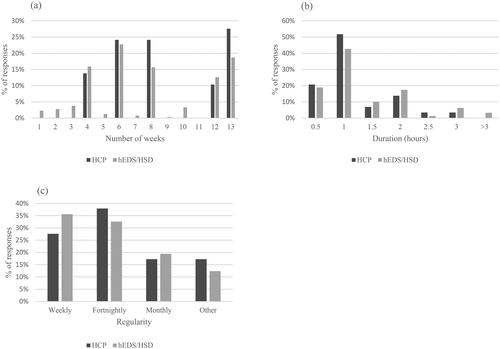
All topics from the participant surveys were collated and summarized into 41 minor topics (Supplement B). Sixty-nine percent of HCP and 81% of hEDS/HSD participants rated an online pain management program for hEDS/HSD as “important” or “very important” (). Overall, most participants felt it should run for 1 h/week (52% HCP and 43% hEDS/HSD) for 6-weeks (24% HCP and 23% hEDS/HSD) (). The majority of participants (69% for both HCP and hEDS/HSD) felt it was “important” or “very important” to have regular online contact with a trained HCP as part of the program (), and this contact should be fortnightly (38% of HCP and 33% of hEDS/HSD) (). In addition, participants with hEDS/HSD rated real-life case examples most highly, followed by online discussion forums, then quizzes (76%, 73% and 30%, respectively rated “important” or “very important) to be a part of the online program ().
Figure 3. (a): Importance of online pain management program. HCP = Healthcare professional, hEDS = hypermobile Ehlers-Danlos Syndrome, HSD = hypermobility spectrum disorder. (b): Importance of online HCP contact as part of program. (c): Importance of other components to program.
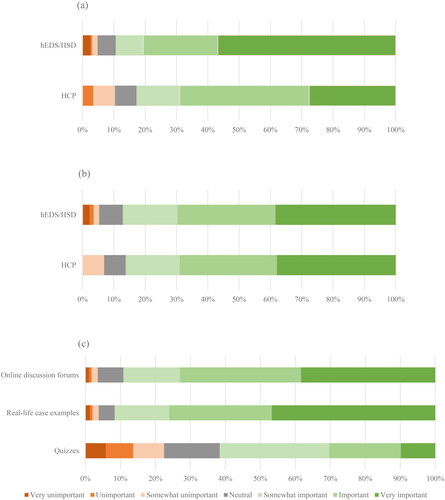
Figure 4. (a): Duration of program. HCP = Healthcare professional, hEDS = hypermobile Ehlers-Danlos Syndrome, HSD = hypermobility spectrum disorder. (b): Time commitment per week. (c): Regularity of online HCP contact.
Stage 1: Delphi survey 2 participant numbers and demographics
Two-hundred and thirty-seven hEDS/HSD participants and 17 HCP provided their email addresses for survey 2 (). 178 hEDS/HSD and 13 HCP participants responded to the email (survey 2 opened for 8 weeks from December 2022 to January 2023). Of these, 154 hEDS/HSD participants and 12 HCP completed the survey. Three hEDS/HSD participants who took part in survey 2 were not diagnosed by a medical practitioner and were excluded; this can be the case since both surveys were anonymous and unlinked. This left 151 hEDS/HSD and 12 HCP completed and eligible responses for analysis ().
Stage 1: Survey 2 consensus results
Of the 41 minor topics from Survey 1, 27 reached consensus in both groups. Nine minor topics did not reach consensus between groups (Supplement B). The authors discussed each of these nine topics based on the three components of evidence-based healthcare: the preferences of hEDS/HSD participants, the current best evidence on the management of pain, and the clinical expertise of the authors in managing pain patients with hEDS/HSD. Consequently, the authors decided to include eight of those minor topics in the program (Supplement B). “Medical trends for pain and/or injury”, “Surgery for pain and/or injuries and post-surgical care”, “Goal setting and realistic expectations” and “Social engagement” hEDS/HSD [Citation39]. “Cognitive, behavioural and emotional strategies” were included as psychosocial contributors are important to consider in hEDS/HSD and are recommended as clinical recommendations for pain management in EDS [Citation16,Citation17,Citation40]. “Nutrition and dietetics” and “Environmental factors” were included as anecdotal and research evidence that suggests how these may affect the experience of pain and are important to consider when making lifestyle changes [Citation41–45]. Lastly, “Hope and reassurance” was included as a topic because these concepts formed the basis of this online pain management program. Like many other researchers and clinicians working to improve the quality of care for hEDS and HSD, we set out on this research path to change, inform, empower and signal hope [Citation46].
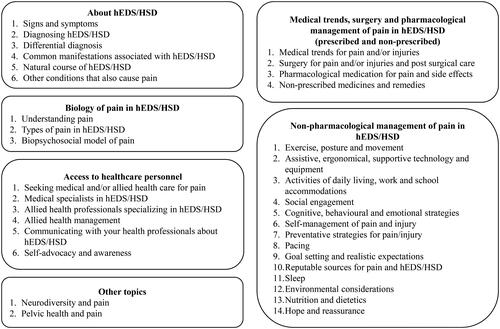
In total, 35 minor topics were included in the program. Topics that were not included are outlined in Supplement B. The authors discussed and categorized the topics into six domains to structure the program in a logical and coherent manner ().
Figure 5. Categorised topics. hEDS = hypermobile Ehlers-Danlos Syndrome, HSD = hypermobility spectrum disorder.
Stage 2: Development results
The six domains of content were divided into 12 modules, and content in each module was tailored to take approximately 30 min to complete. This allowed the program to adhere to the one hour per week, for 6-weeks, that our Delphi participants felt was appropriate. The title of each module and their descriptor is outlined in Supplement B. We used in-built features offered in the LearnDash LMS to build the online HOPE program. Some of the features included were the ability to create distinct modules and enable progress tracking to support learning outcomes. We also included photographs (e.g. kinesiotaping of the shoulder), images (e.g. concept map of the biopsychosocial contributors of pain), and downloadable content (e.g. symptom checker and action plan template) to supplement the online material. There were checkpoints in most modules to promote participant reflection about their pain experiences and content learnt so far, to encourage development of individualized pain self-management strategies and to foster healthy lifestyle and behavioural changes. We also included “take home messages” as a summary at the end of each module to highlight the significance of the content covered in that module.
Stage 3: Alpha test participant numbers and demographics
Five participants were recruited for usability testing. Their demographics are presented in .
Table 2. Usability participant demographics.
Stage 3: Usability test results
The average SUS score was 82.5, corresponding to a 90-95 percentile range and an ‘A’ grade [Citation37,Citation38]. Participant 1 commented that the content was “very very wordy” and participant 3 commented that the “writing is very small making it hard to see at times”. Participant 2 pointed out that they had to click twice on certain buttons to mark a module as complete and to move to the next page. Participant 4 reported that the website used a lot of processing power on Chrome. Accordingly, we reduced word count and adjusted font sizes and recommended which web browsers to use. We created a frequently asked questions page that explained how the navigation buttons worked as the button functions could not be changed due to the limited functionality of Wordpress. Individual scores of each usability participant are presented in Supplement C.
Discussion
Based on a large survey of people with hEDS/HSD and healthcare professionals, an online pain management program specific for hEDS/HSD is important. The topics that they feel people with hEDS/HSD should know about their pain can be captured in six domains that involve: understanding their condition; knowledge about the biology of pain in hEDS/HSD; information about access to healthcare; medical, surgical and pharmacological pain management options; non-pharmacological pain management options; and how neurodiversity and pelvic health relate to pain in hEDS/HSD. Based on these results, we created the first hEDS/HSD-specific online pain management program. Usability testing of this website on a group of participants of comparable age and education level to hEDS/HSD participants in other studies suggests that this online pain management program was highly acceptable in terms of usability [Citation35], providing assurance that it will be usable in similar hEDS/HSD groups.
Key findings
Many of the topics that reached consensus reflected participant desire for pain education, self-management skills and active management strategies. Passive management strategies such as thermotherapies (e.g. heat packs) and complementary or alternative medicine (e.g. Alexander technique, craniosacral therapy) did not reach consensus in either participant groups. These findings strongly echo a recent qualitative study reporting that people with hEDS/HSD want active strategies for their pain [Citation18]. To provide value-based healthcare for people, we need to align management strategies to what stakeholders regard as important [Citation47]. We suggest that healthcare professionals and people with hEDS/HSD should work together as a partnership, and explore high-value health care, including the utilization of EDS-specific and peer-reviewed pain management strategies such as the HOPE program to deliver education and address the biopsychosocial model of pain in its entirety.
An important topic that reached consensus needing further exploration is “self-advocacy and awareness”. The fact that 93% of people with hEDS/HSD in this survey felt that self-advocacy for their pain was necessary as a management strategy highlights the medical challenge that people with hEDS/HSD face. This is not a surprising finding, considering growing evidence of the under-recognition and poor medical and allied health management of hEDS and HSD [Citation5,Citation48–50], including reporting of “clinician-associated traumatization” among these groups [Citation51]. There is an old medical saying taught to medical doctors “when you hear hoofbeats, think horses, not zebras”. The zebra represents rarer diseases, so the saying teaches doctors to expect common conditions to avoid misdiagnosis. However, with conditions like hEDS and HSD that are considered less known and have more complex presentations, this saying ironically causes misdiagnosis. The medical community needs to understand that ‘not all hoofbeats mean horses’, and iatrogenic trauma can serve as a barrier to people seeking pain management, leading to negative expectations of future medical care and eventually poorer health outcomes [Citation50]. There is more that the medical and allied health community can do, including active listening [Citation52] and upskilling their own medical knowledge and skillsets to help people who are genuinely seeking to understand and manage their pain.
Cognitive, behavioural and emotional strategies did not reach consensus between groups, despite Cognitive Behavioural Therapy (CBT) being a mainstay medical recommendation for these conditions [Citation17,Citation53]. Our study found more HCP felt it was at least important, compared to hEDS/HSD participants (92% vs 72%). Based on a recent scoping review, there is little research into the use of psychological interventions in hEDS/HSD and not enough high-quality evidence to support their routine use [Citation54]. In a population that has historically felt dismissed and invalidated by healthcare professionals, psychological interventions need to be prescribed with care through genuine acknowledgement of the biological nature of their pain and careful assessment and explanation using the biopsychosocial model of pain, rather than routine prescription, such as not to worsen their loss of trust in the healthcare profession [Citation48,Citation51,Citation55]. More research needs to be done into the feasibility, acceptability and effectiveness of psychological interventions in hEDS/HSD.
Program parameters
Participants with hEDS/HSD expressed that healthcare professional contact, real-life case examples and discussion forums were important as part of an online pain management program while quizzes or practice tasks to confirm understanding were less important. Varying combinations of these four components are usually found in established online pain management programs [Citation12,Citation13]. A study comparing various levels of clinician support in an online pain management program did not find significant differences in pain levels, disability, depression, or anxiety [Citation56]. The challenge with implementing all these components in one program is needing available specialized staff, such as different healthcare professionals involved in pain management, to provide contact, and online forum moderators which will affect cost-effectiveness and the level of automaticity of the program. A long-term study compared various levels of clinician support (no support, optional weekly support, and regular weekly support from a psychologist) in a CBT and transdiagnostic based online pain program [Citation57,Citation58]. Clinical outcome measures including pain intensity, disability, anxiety, and depression were similar between groups, suggesting that no support or optional support could be more cost-effective. However, this finding should be interpreted with caution since their intervention, the Pain Course, has been refined over multiple clinical trials; so their findings may not be translatable to newer and disease-specific pain management courses. Taking their advice into consideration, we acknowledge that these parameters require exploring in future feasibility and effectiveness trials of the HOPE program. Ultimately, health intervention programs must balance the happy medium of maximizing health outcome efficacy with cost-effectiveness for the viability and sustainability of future programs.
Due to the lack of foreseeable sustained funding for our program, we decided to not include healthcare professional contact or discussion forums in this first iteration of our program. Instead, we included reflective checkpoints that encourage participants to consider their own biopsychosocial contributors to their pain and actively engage in creating their own pain self-management action plan. We wanted the program to help participants reflect on their own pain experience and beliefs, build skills for self-efficacy and begin the initial steps to behavioural change [Citation59]. A recent large-scale study (RESTORE) into Cognitive Functional Therapy (CFT) in chronic low back pain used similar strategies [Citation60], and results from the study have showed short- and long-term improvements in pain-related activity limitations. The RESTORE trial adopted individualized approaches conducted in person by trained Physiotherapists. Since the HOPE program is online and is currently not individualized or guided, we chose to use reflective checkpoint questions to incorporate some of the principals of CFT. Guided by this recent evidence, we formed reflective questions encouraging participants to make sense of their pain experiences, set goals and problem-solve with self-management strategies and consider lifestyle or behavioural changes that may be useful for them.
Study limitations
We had excellent hEDS/HSD engagement with hEDS/HSD numbers exceeding our planned numbers in both surveys, but we did not manage to recruit the target number of twenty HCP for the second consensus round of the Delphi survey. We feel that this was to be expected as we exclusively included a very specialized group of healthcare professionals with at least 5-years of experience treating and/or researching hEDS/HSD. Survey 2 spanned from December 2022 to January 2023 which coincided with the holidays, and this may have also affected recruitment. Our lower number may also be indicative of the lack of HCP with experience in hEDS/HSD. Secondly, although we conducted the survey online and advertised through international organisations such as the Ehlers-Danlos Society, our participants were mainly from North America, Europe and Oceania and therefore cannot be generalized to other countries. Another limitation is that our study did not have a balanced gender representation, with more than 80% female gender. However, this is a close representative of the adult hEDS/HSD population, which has a reported gender prevalence of 30% men and 70% women [Citation23].
In summary, people with hEDS/HSD and experienced HCP rated an online hEDS/HSD specific pain management program as important. Overall, stakeholders suggested several topics relevant to the self-management of pain, including topics to increase their knowledge about pain, knowledge about their condition, and current strategies that are available for the management of pain in these conditions. The HOPE program is the first online pain management program designed for people with hEDS/HSD, using key stakeholder input. Future studies will determine if the program is feasible, acceptable, and effective.
Author contributions
All authors on this paper contributed to the design of the study, data analysis, preparation of the manuscript and have all approved the submitted manuscript. MTC, CC, EI and LN contributed to writing the content of the website. MTC designed and developed the website with assistance from the Macquarie University AAO RDS team.
Supplemental Material
Download Zip (41.3 KB)Acknowledgements
We would like to thank the Ehlers Danlos Society for allowing us to promote our survey on their website and social media, Dr Alan Hakim (Rheumatologist, EDS Society, United Kingdom) and Dr Marina Junqueira Santiago (Senior Lecturer, Macquarie University, Australia) for reviewing parts of our content. We also thank Simon O’Toole and Elizabeth Davies (Australian Astronomical Optics RDS team, Macquarie University, Australia) for assisting us in the website design, construction and maintenance. Lastly, we would especially like to thank all hEDS/HSD and healthcare professional participants who took part and gave us their valuable input in this study. Min Tze Chew holds a research scholarship supported by the Australian Government’s Research Training Program (RTP) for the duration of her PhD candidature at Macquarie University.
Disclosure statement
The authors declare no conflict of interest.
Data availability statement
The authors confirm that the data supporting the findings of this study are available within the article and its supplementary materials. Raw data files related to this study can be found at: Chan, Cliffton; Chew, Min Tze; Ilhan, Emre; Nicholson, Leslie (2024). The raw data files for "An online pain management program for people with hypermobile Ehlers-Danlos syndrome or Hypermobility Spectrum Disorder: a three-staged development process". Macquarie University. Dataset. https://doi.org/10.25949/24892329.v1.
Additional information
Funding
References
- Sacheti A, Szemere J, Bernstein B, et al. Chronic pain is a manifestation of the Ehlers-Danlos syndrome. J Pain Symptom Manage. 1997;14(2):88–93. doi:10.1016/s0885-3924(97)00007-9.
- Voermans NC, Knoop H, Bleijenberg G, et al. Pain in ehlers-danlos syndrome is common, severe, and associated with functional impairment. J Pain Symptom Manage. 2010;40(3):370–378. doi:10.1016/j.jpainsymman.2009.12.026.
- Zimmer Z, Fraser K, Grol-Prokopczyk H, et al. A global study of pain prevalence across 52 countries: examining the role of country-level contextual factors. Pain (Amsterdam). 2022;163(9):1740–1750. doi:10.1097/j.pain.0000000000002557.
- Malfait F, Marlies C, Vroman R, et al. Pain in the Ehlers–Danlos syndromes: mechanisms, models, and challenges. Am J Med Genet C. 2021;187(4):429–445. doi:10.1002/ajmg.c.31950.
- Bennett SE, Walsh N, Moss T, et al. The lived experience of joint hypermobility and Ehlers-Danlos syndromes: a systematic review and thematic synthesis. Phys Ther Rev. 2019;24(1-2):12–28. doi:10.1080/10833196.2019.1590674.
- Bathen T, Hångmann AB, Hoff M, et al. Multidisciplinary treatment of disability in ehlers-danlos syndrome hypermobility type/hypermobility syndrome: a pilot study using a combination of physical and cognitive-behavioral therapy on 12 women. Am J Med Genet A. 2013;161a(12):3005–3011. doi:10.1002/ajmg.a.36060.
- Rahman A, Daniel C, Grahame R. Efficacy of an out-patient pain management programme for people with joint hypermobility syndrome. Clin Rheumatol. 2014;33(11):1665–1669. doi:10.1007/s10067-014-2539-9.
- Revivo G, Amstutz DK, Gagnon CM, et al. Interdisciplinary pain management improves pain and function in pediatric patients with chronic pain associated with joint hypermobility syndrome. Pm R. 2019;11(2):150–157. doi:10.1016/j.pmrj.2018.06.018.
- Kalisch L, Boniwell I, Osin E, et al. Feeling good despite EDS: the effects of a 5-week online positive psychology programme for Ehlers–Danlos-Syndromes patients. J Contemp Psychother. 2022;52(1):79–87. doi:10.1007/s10879-021-09521-8.
- Lattimore P, Harrison F. Pilot study of an online-delivered mindfulness meditation in Ehlers-Danlos syndrome (hEDS): effect on quality-of-life and participant lived experience. Disabil Rehabil. 2022;45(23):3833–3840. doi:10.1080/09638288.2022.2140843.
- Chew MT, Chan C, Kobayashi S, et al. Online pain management programs for chronic, widespread musculoskeletal conditions: a systematic review with meta-analysis. Pain Pract. 2023;23(6):664–683. doi:10.1111/papr.13227.
- Dear BF, Titov N, Perry KN, et al. The pain course: a randomised controlled trial of a clinician-guided internet-delivered cognitive behaviour therapy program for managing chronic pain and emotional well-being. Pain. 2013;154(6):942–950. doi:10.1016/j.pain.2013.03.005.
- Smith J, Faux SG, Gardner T, et al. Reboot online: a randomized controlled trial comparing an online multidisciplinary pain management program with usual care for chronic pain. Pain Med. 2019;20(12):2385–2396. doi:10.1093/pm/pnz208.
- Friesen LN, Hadjistavropoulos HD, Schneider LH, et al. Examination of an internet-delivered cognitive behavioural pain management course for adults with fibromyalgia: a randomized controlled trial. Pain. 2017;158(4):593–604. doi:10.1097/j.pain.0000000000000802.
- Stinson JN, Lalloo C, Hundert AS, et al. Teens taking charge: a randomized controlled trial of a Web-Based self-management program with telephone support for adolescents with juvenile idiopathic arthritis. J Med Internet Res. 2020;22(7):e16234. doi:10.2196/16234.
- Baeza-Velasco C, Bulbena A, Polanco-Carrasco R, et al. Cognitive, emotional, and behavioral considerations for chronic pain management in the Ehlers–Danlos syndrome hypermobility-type: a narrative review. Disabil Rehabil. 2019;41(9):1110–1118. doi:10.1080/09638288.2017.1419294.
- Chopra P, Tinkle B, Hamonet C, et al. Pain management in the Ehlers–Danlos syndromes. Am J Med Genet C Semin Med Genet. 2017;175(1):212–219. doi:10.1002/ajmg.c.31554.
- Bennett SE, Walsh N, Moss T, et al. Developing a self-management intervention to manage hypermobility spectrum disorders (HSD) and hypermobile Ehlers-Danlos syndrome (hEDS): an analysis informed by behaviour change theory. Disabil Rehabil. 2022;44(18):5231–5240. doi:10.1080/09638288.2021.1933618.
- Holzer KJ, Veasley C, Kerns RD, et al. Partnering with patients in clinical trials of pain treatments: a narrative review. Pain (Amsterdam). 2022;163(10):1862–1873. doi:10.1097/j.pain.0000000000002600.
- Hsu C-C, Sandford BA. The delphi technique: making sense of consensus. Pract Assess Res Eval. 2007;12:10.
- Forsythe LP, Carman KL, Szydlowski V, et al. Patient engagement in research: early findings from the Patient-Centered outcomes research institute. Health Aff (Millwood). 2019;38(3):359–367. doi:10.1377/hlthaff.2018.05067.
- Malfait F, Francomano C, Byers P, et al. The 2017 international classification of the ehlers–Danlos syndromes [. ]Am J Med Genet C Semin Med Genet. 2017;175(1):8–26. doi:10.1002/ajmg.c.31552.
- Demmler JC, Atkinson MD, Reinhold EJ, et al. Diagnosed prevalence of Ehlers-Danlos syndrome and hypermobility spectrum disorder in Wales, UK: a national electronic cohort study and case–control comparison. BMJ Open. 2019;9(11):e031365. doi:10.1136/bmjopen-2019-031365.
- Murray B, Yashar BM, Uhlmann WR, et al. Ehlers-Danlos syndrome, hypermobility type: a characterization of the patients’ lived experience. Am J Med Genet A. 2013;161A(12):2981–2988. doi:10.1002/ajmg.a.36293.
- Simmonds JV, Herbland A, Hakim A, et al. Exercise beliefs and behaviours of individuals with joint hypermobility syndrome/Ehlers-Danlos syndrome - hypermobility type. Disabil Rehabil. 2019;41(4):445–455. doi:10.1080/09638288.2017.1398278.
- Teran-Wodzinski P, Kumar A. Clinical characteristics of patients with hypermobile type Ehlers–Danlos syndrome (hEDS) and generalized hypermobility spectrum disorders (G-HSD): an online survey. Rheumatol Int. 2023;43(10):1935–1945. doi:10.1007/s00296-023-05378-3.
- Jünger S, Payne SA, Brine J, et al. Guidance on conducting and REporting DElphi studies (CREDES) in palliative care: recommendations based on a methodological systematic review. Palliat Med. 2017;31(8):684–706. doi:10.1177/0269216317690685.
- French SD, Nielsen M, Hall L, et al. Essential key messages about diagnosis, imaging, and self-care for people with low back pain: a modified delphi study of consumer and expert opinions. Pain (Amsterdam). 2019;160(12):2787–2797. doi:10.1097/j.pain.0000000000001663.
- Moore E, Braithwaite FA, Stanton TR, et al. What do I need to know? Essential educational concepts for complex regional pain syndrome. Eur J Pain. 2022;26(7):1481–1498. doi:10.1002/ejp.1976.
- Sharpe L, Jones E, Ashton-James CE, et al. Necessary components of psychological treatment in pain management programs: a delphi study. Eur J Pain. 2020;24(6):1160–1168. doi:10.1002/ejp.1561.
- Hasson F, Keeney S, McKenna H. Research guidelines for the delphi survey technique. J Adv Nurs. 2000;32(4):1008–1015. doi:10.1046/j.1365-2648.2000.t01-1-01567.x.
- LimeSurvey GmbH. LimeSurvey: an Open Source survey tool. LimeSurvey GmbH; 2012. http://www.limesurvey.org
- Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. doi:10.1016/j.jbi.2019.103208.
- Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi:10.1016/j.jbi.2008.08.010.
- Bangor A, Kortum PT, Miller JT. An empirical evaluation of the system usability scale. Int J Human-Comput Interact. 2008;24(6):574–594. doi:10.1080/10447310802205776.
- Brooke J. Sus: a “quick and dirty’usability. Usability Eval Industry. 1996;189(3):189–194.
- Lewis JR. The system usability scale: past, present, and future. Int J Human-Comput Interact. 2018;34(7):577–590. doi:10.1080/10447318.2018.1455307.
- Lewis JR, Sauro J. Item benchmarks for the system usability scale. J. Usability Studies. 2018;13(3):158–167.
- Clark NL, Johnson M, Rangan A, et al. The biopsychosocial impact of hypermobility spectrum disorders in adults: a scoping review. Rheumatol Int. 2023;43(6):985–1014. doi:10.1007/s00296-023-05298-2.
- Whalen KC, Crone W. Multidisciplinary approach to treating chronic pain in patients with Ehlers–Danlos syndrome: critically appraised topic. J Pain Res. 2022;15:2893–2904. doi:10.2147/JPR.S377790.
- Castori M, Morlino S, Pascolini G, et al. Gastrointestinal and nutritional issues in joint hypermobility syndrome/Ehlers-Danlos syndrome, hypermobility type. Am J Med Genet C Semin Med Genet. 2015;169C(1):54–75. doi:10.1002/ajmg.c.31431.
- Elma O, Yilmaz ST, Deliens T, et al. Do nutritional factors interact with chronic musculoskeletal pain? A systematic review. J Clin Med. 2020;9(3):702. doi:10.3390/jcm9030702.
- Haack M, Simpson N, Sethna N, et al. Sleep deficiency and chronic pain: potential underlying mechanisms and clinical implications. Neuropsychopharmacology. 2020;45(1):205–216. doi:10.1038/s41386-019-0439-z.
- Momi SK, Fabiane SM, Lachance G, et al. Neuropathic pain as part of chronic widespread pain: environmental and genetic influences. Pain. 2015;156(10):2100–2106. doi:10.1097/j.pain.0000000000000277.
- Palomo-Toucedo IC, Leon-Larios F, Reina-Bueno M, et al. Psychosocial influence of Ehlers-Danlos syndrome in daily life of patients: a qualitative study. Int J Environ Res Public Health. 2020;17(17):6425. doi:10.3390/ijerph17176425.
- Gensemer C, Burks R, Kautz S, et al. Hypermobile Ehlers-Danlos syndromes: complex phenotypes, challenging diagnoses, and poorly understood causes. Dev Dyn. 2021;250(3):318–344. doi:10.1002/dvdy.220.
- Teisberg E, Wallace S, O’Hara S. Defining and implementing value-based health care: a strategic framework. Acad Med. 2020;95(5):682–685. doi:10.1097/ACM.0000000000003122.
- Anderson LK, Lane KR. The diagnostic journey in adults with hypermobile Ehlers-Danlos syndrome and hypermobility spectrum disorders. J Am Assoc Nurse Pract. 2021;34(4):639–648. doi:10.1097/jxx.0000000000000672.
- Bovet C, Carlson M, Taylor M. Quality of life, unmet needs, and iatrogenic injuries in rehabilitation of patients with Ehlers-Danlos syndrome hypermobility type/joint hypermobility syndrome. Am J Med Genet A. 2016;170(8):2044–2051. doi:10.1002/ajmg.a.37774.
- Langhinrichsen-Rohling J, Lewis CL, McCabe S, et al. They’ve been BITTEN: reports of institutional and provider betrayal and links with Ehlers-Danlos syndrome patients’ current symptoms, unmet needs and healthcare expectations. Ther Adv Rare Dis. 2021;2:26330040211022033–26330040211022033. doi:10.1177/26330040211022033.
- Halverson CME, Penwell HL, Francomano CA. Clinician-associated traumatization from difficult medical encounters: results from a qualitative interview study on the Ehlers-Danlos syndromes. SSM Qual Res Health. 2023;3:100237. doi:10.1016/j.ssmqr.2023.100237.
- Baguley SI, Pavlova A, Consedine NS. More than a feeling? What does compassion in healthcare ‘look like’ to patients? Health Expect. 2022;25(4):1691–1702. doi:10.1111/hex.13512.
- Russek LN, Stott P, Simmonds J. Recognizing and effectively managing Hypermobility-Related conditions. Phys Ther. 2019;99(9):1189–1200. doi:10.1093/ptj/pzz078.
- Song JZ, Luong D, Feldman ECH, et al. Psychological interventions for individuals with Ehlers-Danlos syndrome and hypermobility spectrum disorder: a scoping review. Orphanet J Rare Dis. 2023;18(1):254. doi:10.1186/s13023-023-02799-y.
- Berglund B, Nordström G, Lützén K. Living a restricted life with Ehlers-Danlos syndrome (EDS). Int J Nurs Stud. 2000;37(2):111–118. doi:10.1016/S0020-7489(99)00067-X.
- Dear BF, Gandy M, Karin E, et al. The pain course: 12- and 24-Month outcomes from a randomized controlled trial of an Internet-Delivered pain management program provided with different levels of clinician support. J Pain. 2018;19(12):1491–1503. doi:10.1016/j.jpain.2018.07.005.
- Dear BF, Gandy M, Karin E, et al. The pain course: a randomised controlled trial examining an internet-delivered pain management program when provided with different levels of clinician support. Pain (Amsterdam). 2015;156(10):1920–1935. doi:10.1097/j.pain.0000000000000251.
- Dear BF, Karin E, Fogliati R, et al. A cost-effectiveness analysis of an internet-delivered pain management program delivered with different levels of clinician support: results from a randomised controlled trial. J Pain. 2021;22(3):344–358. doi:10.1016/j.jpain.2020.11.003.
- Caneiro JP, Bunzli S, O’Sullivan P. Beliefs about the body and pain: the critical role in musculoskeletal pain management. Braz J Phys Ther. 2021;25(1):17–29. doi:10.1016/j.bjpt.2020.06.003.
- Kent P, Haines T, O’Sullivan P, et al. Cognitive functional therapy with or without movement sensor biofeedback versus usual care for chronic, disabling low back pain (RESTORE): a randomised, controlled, three-arm, parallel group, phase 3, clinical trial. Lancet. 2023;401(10391):1866–1877. doi:10.1016/S0140-6736(23)00441-5.

