Abstract
Purpose
Non-weight bearing is often recommended after humeral fractures. This review aims to summarise the extent and nature of the evidence for the feasibility, acceptability, safety, and effects of early weight bearing (EWB) in people with humeral fractures, treated operatively or non-operatively.
Methods
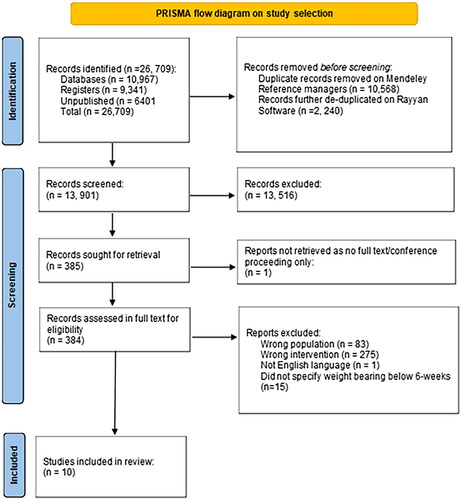
Data sources identified published (PUBMED, EMBASE, CINAHL) and unpublished (ClinicalTrials.gov, CENTRAL, NIHR Open Research, OpenGrey) literature. Independent data extraction was conducted by two reviewers.
Results
13 901 records were retrieved. Ten studies, involving 515 post-operative patients and 351 healthcare professionals, were included. EWB was found to be feasible in nine studies. There was limited evidence regarding adherence to EWB. Trauma and orthopaedic surgeons reported that EWB was acceptable. This depended on surgery type and whether it was a post-operative polytrauma case. No acceptability data was reported from patients’ perspectives. Only one study reported two patients who developed unsatisfactory outcomes from excessive post-operative EWB. Positive effects of EWB were reported on disability level, pain, shoulder and elbow motion, and union.
Conclusion
There is some evidence for the feasibility, safety, and effectiveness of post-operative EWB after humeral fractures. There was limited data on the acceptability of EWB. Heterogeneous study designs, and variations in EWB protocols limit conclusions.
IMPLICATIONS FOR REHABILITATION
There is some evidence to support the feasibility, safety, and effectiveness of early weight bearing following operative management of humeral fractures.
Early weight bearing after some humeral fractures is acceptable to some subspecialities of orthopaedic surgeons but is not universally accepted.
Rehabilitation professionals should discuss the option of early weight bearing after operative management of humeral fracture with patients and their multidisciplinary team.
Introduction
Humeral fractures are debilitating injuries that impact quality of life, particularly among older adults [Citation1,Citation2]. The global annual incidence of humeral fractures is increasing and currently represents 6–8% of all fractures in adults [Citation3–5]. Humeral fractures can be classified based on their location within the bone as: proximal humerus, humeral shaft, and distal humerus [Citation6–9]. These fractures can be stabilised operatively or nonoperatively. Nonoperative approaches are now standard of care for non-complex fractures and in older people [Citation10–13]. However, rehabilitation after humeral fracture remains contentious. Typically, after injury, whether treated either operatively or non-operatively, a period of non-weight bearing (NWB) is prescribed. Recently, early weight bearing (EWB) is recognised as an underused rehabilitation treatment that has shown favourable outcomes [Citation14,Citation15].
At cellular level, bone healing after a fracture occurs in the presence of suitable external mechanical loading and local interfragmentary motion (strain) between fracture fragments [Citation16–19]. By the second week post fracture, granulation tissue formation provides provisional stability before further bony bridging callus formation, leading to clinical union [Citation20]. The adaptation of fractured bones to functional loading via EWB is integral to secondary healing but is underused in clinical practice [Citation21,Citation22]. This cautious approach to EWB may be because, during acute healing, a strategy is required that balances the benefits of EWB as mechanical stimulation with the potential risks of displacement in unstable fractures [Citation20]. Excessive WB, beyond the therapeutic bandwidth of osteosynthesis, could potentially delay healing or cause non-union [Citation23,Citation24]. However, extended NWB is also associated with detrimental physiological and systemic complications and in older people could lead to loss of independence [Citation25–30].
According to the British Orthopaedic Association Standards for Trauma and Orthopaedics (BOAST), all surgery in patients with frailty should be performed to allow full WB for activities of daily living within 36 hours of admission [Citation31,Citation32]. Traditionally, in humeral fractures, a minimum of six-weeks of non-weight bearing is regarded as the gold standard to promote healing, although this duration can vary and extend up to 12-weeks [Citation33–35]. In the management of lower limb fractures, EWB has demonstrated numerous advantages and is now routinely applied; however, this is not yet the case after humeral fractures [Citation36–39]. Additionally, it is recognised that the major stressors on the humerus are rotational force, which are different from the primary stressors of lower limbs – which are axial (force acting in the direction parallel to the axis of a bone) and bending forces during full weight bearing [Citation40–42]. This evidence suggests that EWB following humeral fractures could be safer than weight bearing after a lower limb fracture.
No current or ongoing systematic or scoping reviews are being conducted on this topic [Citation43]. The aim of this scoping review was to identify and summarise the existing research evidence on the feasibility, acceptability, safety, and effects of EWB in humeral fractures treated operatively or non-operatively.
Methods
This scoping review was informed by the Joanna Briggs Institute for conducting scoping reviews and reporting, using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Extension for scoping reviews [Citation44,Citation45]. The protocol was initially created on the Open Science Framework on 22 November 2022. Registration of the final protocol was 24 March 2023 (https://osf.io/zkad9/).
Search strategy
Following piloting of the search strategy on PubMed and CINAHL Plus, seven electronic databases were searched for published or unpublished reports from 01 January 2000 to 20 March 2023 (). A systematic search strategy was designed that expanded the terms “humerus,” “weight bearing,” “fracture,” “operative,” “non-operative,” “rehabilitation” (Supplementary Data 1). The reference list of the studies included in the review were screened for additional potentially eligible records.
Table 1. Source of electronic databases.
Eligibility criteria
Eligibility criteria were characterised as participants, concepts, context, study types and outcomes ().
Table 2. Eligibility criteria.
Source of evidence selection
All records were imported into Mendeley reference management software (v2.93.0) and duplicates were removed [Citation47], before being imported into Rayyan reference management [Citation48]. Title and abstracts and then full-text were screened independently by at least two of four reviewers [JHG, SW, JR and GB]. Any discrepancies were resolved through discussions. In cases of uncertainty, the opinion of a third reviewer [LB, AT, DN] was sought to reach a consensus [Citation49].
Data extraction and charting
A data extraction template was adapted from the Joanna Briggs Institute System for the Unified Management, Assessment, and Review of Information, a priori and piloted with five articles [Citation50]. Key study characteristics collected included participant’s characteristic, study’s characteristics, characteristic of humeral fractures and its management, WB protocol and parameters, outcomes of EWB in feasibility, acceptability, safety, and effects. One reviewer [JHG] extracted data from all included studies. A second reviewer [GB] independently extracted data from 50% of the included studies and any discrepancies were discussed. Finally, the third reviewer [DN] cross-checked 10% of the extracted data for accuracy by comparing it against the full-text articles. If necessary, the reviewers contacted the corresponding authors of included studies to clarify any missing or additional data.
Data synthesis and analysis
Study characteristics and outcomes of interest were summarised using descriptive statistics (e.g., percentages, mean, standard deviation and range) and narratively to describe the nature and extent of the evidence for each outcome of interest. The outcomes specific to address the research question of this study underwent quantitative analysis to identify the existing literature gaps.
Results
Study identification
A total of 26 709 citations were identified. After duplicates were removed, 13 901 records were retrieved and full texts of 385 articles were screened. 10 studies were included in the final analysis ( and Supplementary Data 2).
Studies included and participants characteristics
Studies included three retrospective cohort studies [Citation51–53], two case series [Citation54,Citation55], two cross sectional surveys [Citation56,Citation57], one commentary article [Citation58], one retrospective case series [Citation59], and one prospective case series [Citation60] ().
Table 3. Study and participant characteristics .
Most of the studies (eight studies, 80%) were conducted in the United State of America [Citation51,Citation52,Citation54–59], with one study each conducted in Europe (Poland) [Citation53] and, South America (Brazil) [Citation60]. Six studies reported retrospective longitudinal data. The mean study duration was 93.5 weeks (range 3.0–456.0 weeks) [Citation51,Citation53–55,Citation59,Citation60].
Nine studies included a total of 515 patients with humeral fractures and 351 healthcare professionals [136 trauma and orthopaedic surgeons, 172 shoulder surgeons]) [Citation51–57,Citation59,Citation60]. The mean patient age was 39.3 years (range 22 to 92 years) (6 studies, 284 patients) [Citation51,Citation52,Citation54,Citation55,Citation59,Citation60]. Sixty-seven % patients were males (report in only four studies, 270 patients) [Citation51,Citation52,Citation55,Citation60].
Five studies reported patient comorbidities including rotator cuff injuries, other sites of fractures, congenital genetic diseases, required assistive walking aids, osteoporosis, cardiac disease, traumatic amputation, prolonged unconsciousness, and unspecified mental disturbance [Citation52–55,Citation59]. Five studies did not report patient comorbidities [Citation51,Citation56–58,Citation60].
Fracture classifications and management
Three studies focused on fractures of the humeral shaft [Citation51,Citation52,Citation57], and four studies investigated distal humeral fractures [Citation55,Citation58–60]. Two studies investigated proximal humeral fractures [Citation53,Citation56]. One study investigated management of proximal metadiaphyseal humeral fractures which is an infrequent severe fracture involving both the proximal and humeral shaft () [Citation54].
Table 4. Feasibility, acceptability, safety and effects of fractures and weight bearing related management.
All studies included patients who were managed operatively following their humeral fractures (). Two studies did not specify the operative approach [Citation57,Citation58]. Six studies used open reduction and internal fixation (ORIF) which included screws, plates, neutralisation devices, and external fixation then planned conversion to ORIF [Citation51,Citation53,Citation54,Citation56,Citation60,Citation61]. Three studies employed arthroplasty techniques, that including of shoulder arthroplasty, total elbow arthroplasty and elbow hemiarthroplasty [Citation55,Citation56,Citation59]. One study explored the preference of EWB after shoulder arthroplasty or ORIF among shoulder, and trauma and orthopaedic surgeons [Citation56]. However, there was a lack of detailed information about the reason surgeons preferred EWB after shoulder arthroplasty versus ORIF. No studies discussed the use of EWB after intramedullary nailing. Only one study that used different type of ORIF reported no relationship between nonunion and postoperative WB status [Citation51].
Only two studies discussed nonoperative approaches as a possible first line treatment following midshaft and distal humeral fractures, including splinting, commercial or functional bracing [Citation57,Citation58]. One study specifically advocated for operative treatment over non-operative management, particularly in younger patients with distal humeral fractures [Citation58].
Five studies provided information on post-operative rehabilitation [Citation52,Citation54,Citation56,Citation59,Citation60]. This included the use of a sling [Citation54,Citation59], no sling nor orthotic [Citation60], patient education [Citation56], outpatient follow-up [Citation56], unspecified physiotherapy programme [Citation54], and home exercise programme [Citation56]. Four studies detailed mobilisation exercises [Citation52,Citation56,Citation59,Citation60], but these varied in the timing of commencement and type of starting point, ranging from passive range of motion (ROM), active assisted ROM, and active ROM before strengthening exercises [Citation52,Citation56,Citation59,Citation60].
These three studies used validated outcome measures including the Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaire [Citation62], Patient Rated Elbow Evaluation (PREE) [Citation63], and Mayo Elbow Performance Score (MEPS) [Citation54,Citation59,Citation60,Citation64]. Whereas, the other seven studies reported non standardised outcome measures.
Early weight bearing protocol in humeral fractures
Two common postoperative EWB protocols were identified. Eight studies investigated WB immediately after surgery [Citation51,Citation52,Citation54–56,Citation58–60]. One study mentioned EWB without specifying a timeframe [Citation57], whilst another study did not specify the terminology of EWB but advised patients to use their arm but “avoid overloading the extremity postoperatively” which was categorised as EWB () [Citation53]. In two studies that used immediate WB protocols, patients were further instructed to “weight bear as tolerated” [Citation51,Citation59]. Only one study provided more specific instructions, allowing arm use for daily activities but restricting lifting to 10-pound or less [Citation54]. However, the timeframe for EWB was not explicitly defined in any included studies.
The feasibility of early weight bearing
The feasibility of EWB was reported in six studies, exploring the facilitators, barriers, and adherence to EWB () [Citation51,Citation53,Citation55,Citation56,Citation58,Citation59]. Two studies highlighted that operative management functioned as a facilitator for EWB [Citation57,Citation58], especially in cases involving polytrauma [Citation51,Citation59]. Setting preoperative rehabilitation goals for prompt postoperative ambulation was also identified as a facilitator.
Three studies focused on barriers to EWB [Citation53,Citation55,Citation56]. These barriers encompassed patient characteristics, surgeon’s experience, fracture characteristics, and the type of operative fixation. Some of these factors affected the patient’s ability to WB immediately and tolerate additional upper limb WB, such as during sit-to-stand or when using walking aids [Citation55,Citation56]. Szczęsny et al. specifically reported the characteristics of two patients with mental and physical incapacity. These patients developed postoperative delirium and had reduced ambulation due to bilateral amputation or the removal of a hip prothesis, which hindered their adherence to post-operative WB instructions [Citation53].
Three studies briefly mentioned patient’s adherence to EWB instructions [Citation51,Citation53,Citation59]. Two retrospective studies queried the patient’s adherence to the prescribed immediate WB protocols [Citation51,Citation59], although no further investigation was completed. Szczęsny et al. reported that two out of 131 patients did not adhere to the postoperative instruction to “avoid overloading,” although it is not clear whether this included the EWB protocols [Citation53].
The acceptability of early weight bearing
No studies investigated the acceptability of EWB from the patients’ perspective. The acceptability of EWB from the orthopaedic surgeon’s perspective was considered in 7 out of 10 studies [Citation51,Citation52,Citation55–58,Citation60]. Some surgeons perceived EWB as acceptable in certain instances, such as polytrauma, older people who required upper limbs to support the use of walking aids or patients who required expedient return to activities of daily living, employment, or an important social role [Citation57–59]. However, there were no standardised postoperative EWB instructions. Instead, five studies emphasised that EWB protocols should be person centred and individualised [Citation51,Citation52,Citation55,Citation58,Citation60] and consider pre-operative planning, the appropriate operative implants, and postoperative rehabilitation.
One study assessed the acceptability of EWB following postoperative proximal humeral fractures among different sub-specialities of orthopaedic surgeons [Citation56]. It reported that a greater proportion of trauma and orthopaedic surgeons considered EWB acceptable after arthroplasty, but not ORIF, compared to shoulder surgeons [Citation56]. Another survey was conducted exclusively amongst trauma and orthopaedic surgeons, and it found that they were more likely to recommend EWB in post-operative humeral shaft fractures and polytrauma cases [Citation57].
The safety of early weight bearing
The safety of EWB in the post-operative management of humeral fractures was reported in only five studies () [Citation51–53,Citation55,Citation60]. One study reported that EWB did not cause non-union in postoperative humeral shaft fractures [Citation51]. Another study reported no adverse effects after EWB in post-operative distal humerus fractures without using slings or orthotics [Citation60]. One study investigating EWB after post-operative comminuted proximal humeral fractures found that only two of 131 patients had secondary destabilisation following EWB [Citation53]. These patients had post-operative delirium and lower limb disability and did not adhere to safety advice. The excessive WB resulted in poor operative outcomes, including humeral tubercles fragmentation and secondary dislocation [Citation53]. It is worth noting that these patients had additional challenges postoperatively, which may have affected their cognitive ability to understand the risk of overloading a severe humeral fracture after surgery [Citation53].
The effects of early weight bearing
Five studies reported the overall positive effects of post-operative EWB following humeral fractures on disability level, pain, shoulder and elbow’s motion and functional outcomes [Citation54,Citation55,Citation58–60]. Five studies reported fracture healing time and extent [Citation51,Citation52,Citation54,Citation55,Citation60]. Three studies did not comment on the effects of EWB [Citation53,Citation56,Citation57].
The studies that used standardised outcome measures such as DASH, PREE, MEPS to measure the effects of EWB all demonstrated improvements in disability levels [Citation54,Citation59,Citation60]. For instance, Wajnsztejn et al. reported that 38% of patients achieved a score of 0 on the DASH scale (indicating the best possible outcome) [Citation60], whilst James et al. reported mean DASH score of 21 (median 12; standard deviation 20) [Citation54], meaning that their patients could be considered clinically indistinguishable from the general population. Stephens et al. rated the improvements as “fair” after EWB, (mean PREE score of 41 points, mean MEPS score of 76.1 points) [Citation59]. Patients reported that their upper limbs’ functional capabilities were generally preserved at 44 months.
Only two studies reported the effect of EWB on pain [Citation54,Citation59]. One study reported that 75% of patients experienced no pain, whilst 25% reported no more than moderate pain measured by the DASH questionnaire [Citation54]. Likewise, in another study, moderate average pain scores were measured by the MEPS [Citation59].
Only three studies reported the effects of EWB on shoulder or elbow motion [Citation54,Citation55,Citation58]. In one case series, three out of four patients achieved a maximum elbow range of motion from 5 to 120 degrees at mean (range) follow up of 47 (12–104) weeks [Citation55]. Two studies used unspecified measures to assess range of motion but mentioned that post-operative upper limb usage for ambulation had improved, and another study reported that 75% of patients were able to lift their arms above their head at mean (range) 132 (52 to 182.5) weeks [Citation54,Citation58].
There was insufficient information to estimate the overall healing time of fractures in two out five studies [Citation51,Citation54,Citation60]. However, James et al. [Citation54] reported uneventful fracture healing in all 18 patients, whilst Langhammer et al. [Citation51] stated that union was achieved in 93% of patients although there was no statistically significant relationship (p = 0.45) between postoperative WB status (EWB versus NWB) and union rate, regardless of the size of fixation plates used. Wajnsztejn et al. [Citation60] defined fracture union as bridged cortices on 2 radiographic planes and absence of union during movement. This study reported that all patients (n = 13) who underwent immediate postoperative WB had fracture healing within 12 weeks. Two other studies reported bony healing on radiography after postoperative EWB [Citation52,Citation55]. Mayer et al. [Citation55] (n = 4) reported initial radiographic healing at 12 weeks, with clinical and full radiographic healing at six months; Suzuki et al. [Citation52] (n = 17) reported radiographic bony union at a mean (range) of time of 11 (8–14) weeks.
Discussion
This review found that there was some evidence for the feasibility, safety, and effectiveness of EWB in humeral fractures following operative management. EWB after some surgical approaches is acceptable to some orthopaedic surgeons. However, research gaps exist, including the absence of investigations into EWB following non-operative management of humeral fractures, the optimal timeframe for EWB, and the acceptability of EWB in patients, their relatives, and the wider multidisciplinary healthcare team. The study populations included in our review are similar to the age distribution in epidemiological data for humeral fractures, ensuring the generalisability of our findings [Citation3,Citation6,Citation65].
Only six studies examined the facilitators, barriers, and adherence in relation to the feasibility of EWB. Overall, the included studies indicate that setting pre-operative goals [Citation51,Citation57–59], especially in polytrauma cases, can help people’s mobility, consistent with findings of previous studies [Citation10,Citation66,Citation67]. This finding is also evidenced by three studies that compared non-operative and operative fixation in patients with polytrauma and concomitant humeral fractures [Citation68–70]. Our review highlighted that there were four main barriers to post-operative EWB after humeral fracture, this included patient characteristics, surgeon’s experience, fracture characteristics, and the type of operative fixation. These findings are similar to barriers reported in a study of EWB after hip fractures [Citation71]. However, additional barriers to EWB were identified after hip fracture and this may include patient characteristics, increased operative time, pre-holiday surgery and admissions in the first quarter of the year. Patient characteristics, such as post-operative delirium, mental incapacity, and lack of lower limb from amputation are vital safety considerations when implementing EWB after humeral fractures [Citation51,Citation55,Citation58].
Concerns regarding the feasibility and safety of applying EWB post-operatively were raised in two studies [Citation51,Citation59]. Both studies highlighted the risks associated with poor adherence to unexplicit EWB status in some patients [Citation51,Citation59]. These concerns were also raised in people following lower limb fractures, especially in older people [Citation72]. In the non-operative management of displaced lower limb fractures (e.g., pelvic or acetabular fractures) these risks were addressed by adapting the EWB guidelines [Citation73]. One study of post-operative EWB after hip fracture demonstrated that early EWB and mobilisation was feasible and had high adherence (78%) [Citation74]. These EWB protocols were also feasible in patients with cognitive impairment or people with multi-comorbidities [Citation74]. Therefore, post-operative EWB approach should be considered after humeral fractures if accompanied by clear rehabilitation instructions [Citation75].
The acceptability of EWB following humeral fractures has only been investigated from the perspectives of surgeons. Only two included studies found that EWB post-operatively was more acceptable to trauma and orthopaedic surgeons compared to shoulder surgeons [Citation56,Citation57]. This preference was limited to arthroplasty surgery alone [Citation56], perhaps due to the belief that absolute fracture stability is required to allow secondary healing for osteosynthesis. This was further influenced by surgeon’s subspecialty training in shoulder and elbow surgeries [Citation56]. This preference is similar to a national audit of EWB following ankle fracture, where only 21% of operatively managed patients were recommended to EWB by surgeons contrary to clinical guidelines [Citation76,Citation77]. Whereas immediate WB following hip fractures with precautionary measures was successfully implemented as standard of care [Citation78,Citation79]. This provides an example of a successful clinical pathway for EWB that could be mirrored for post-operative humeral fractures. However, it is crucial to establish active collaborations among patients and their relatives and multi-disciplinary professionals to codesign evidence-based protocols and pathways, so they are feasible and acceptable [Citation80].
Adverse events were seldom reported in our included studies. One study supported the application of EWB or immediate post-operative WB protocols following humeral fractures, particularly in people with frailty or polytrauma [Citation53]. This is because humeral fractures can lead to substantial functional impairment and reduced health-related quality of life, that is compounded by NWB restrictions [Citation34,Citation81]. Langhammer et al. [Citation51] found no link between immediate WB protocols and adverse events in post-operative humeral shaft fractures. Biomechanical studies also supported the safety of immediate WB post-operatively in humeral shaft and distal humeral fractures [Citation82–84]. These biomedical studies suggest that the benefits of early rehabilitation and muscle strengthening from an immediate WB approach can enhance the performance of the surgical implants and patient outcomes [Citation67.]
However, it is imperative that WB protocols are adhered to as additional postoperative fractures and secondary dislocation were reported in one study (two patients) following overloading [Citation53]. Secondary displacements of proximal humeral fracture affect over 12.5%–28.8% of cases post-operatively [Citation85,Citation86]. To minimise this risk, Tingstad et al. suggested stratification of post-operative WB protocols following humerus fractures based on the presence of lower limb injury that required restricted WB restriction, rather than humeral fracture pattern or severity [Citation87]. In addition, a multi-professional integrated care model involving biomechanical engineers and rehabilitation clinicians may help mitigate the risk of loading failure in an EWB rehabilitation pathway following a humeral fracture [Citation71,Citation88–91]. The findings from five included studies [Citation51,Citation52,Citation54,Citation55,Citation60]. suggest that EWB has no deleterious effect on the union or malunion rate, which aligns with an early study of EWB in humeral shaft fractures [Citation87]. These findings suggest that promoting independence through immediate or EWB protocols is warranted. Independence in social roles matters more for patient at high mortality risk, which is a stronger predictor of positive outcomes than age alone [Citation92].
Limitations and strengths of this scoping review
This review had several limitations. The small number of included studies, as well as the heterogeneity of patient demographics, operative methods, treatment, and WB protocols mean our findings should be interpreted with caution. These limitations hinder accurate implementation of EWB as part of the functional rehabilitation process, especially distinguishing between the therapeutic effects of primary and secondary bone healing. Additionally, the included retrospective cohort studies and case series, which do not have comparison groups, mean it was not possible to calculate between group effect sizes for each outcome. It was also not possible to stratify outcomes by EWB or immediate WB approaches for different type of humerus fractures, operative or non-operative management. This review, included comprehensive search strategy and followed a standardised framework [Citation43]. Due to funding constraints, it was not possible to assign two reviewers to extract data from all evidence sources. Instead, one reviewer extracted all the data and a second reviewer extracted 50% of the sources. A third reviewer checked the extraction accuracy for 10% of randomly selected evidence sources thus minimising the risk of data inaccuracies [Citation93].
Future research recommendations
Future studies should develop standardised definitions and terminology for immediate and EWB when applied to the management of humeral fractures, build the evidence for the dosage, timeframes, and instructions for applying EWB protocols for both operative and non-operative management of humeral fractures and explore the perspectives of patients and healthcare professional about EWB protocols. While studies that evaluated the effect of post-operative EWB using standardised outcome measures demonstrated improvements in disability and function there is no core outcome set which makes further synthesis difficult [Citation54,Citation59,Citation60]. The development of a core outcome set is needed for research into the effectiveness of EWB after humeral fracture [Citation94,Citation95].
Conclusion
This scoping review revealed that there is some evidence for the feasibility, safety, and effectiveness of EWB in humeral fractures following operative management only. EWB after some surgical approaches are acceptable to some sub-speciality of orthopaedic surgeons, but this is not universal among orthopaedic surgeons. Robust research studies using a core outcome set are warranted to establish effective guidelines and clinical decision tools for the implementation of EWB after humeral fractures.
Author contributions
All authors meet the criteria for authorship as defined by the International Committee of Medical Journal Editors (ICMJE). Lindsay Bearne, Alex Trompeter and Dimitra Nikoletou supervised Jia Hui Gan throughout the study and they were involved in the conceptualisation and design of the research. Jia Hui Gan, Lindsay Bearne, Alex Trompeter, Dimitra Nikoletou, Sam Walters, and Jon Room wrote and published the study protocol. Jia Hui Gan, Sam Walters, Jon Room, and Greg Booth reviewed and retrieved the records. Jia Hui Gan, Greg Booth, and Dimitra Nikoletou conducted data extraction and data analysis. Jia Hui Gan wrote the first draft of the manuscript, which was then reviewed by Dimitra Nikoletou, Alex Trompeter, and Lindsay Bearne. All authors provided critical feedback and approved the final manuscript.
Data set
Supplemental Material
Download Zip (95.5 KB)Acknowledgements
We would like to express our gratitude to Dr Helen Wilson, the orthogeriatrician and joint clinical director for frailty services at the Royal Surrey NHS Foundation Trust for her valuable clinical input to this study. We also acknowledge the support of librarian at the St George’s, University of London, for facilitating open access publishing through their agreement with Taylor & Francis Group and the university.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
Additional information
Funding
References
- Anley C, Vrettos B, Rachuene P, et al. Proximal humerus fractures - part 1: conservative management. South Afr Orthop J. 2019;18(3):63–71.
- Leiblein M, Verboket R, Marzi I, et al. Nonunions of the humerus – treatment concepts and results of the last five years. Chin J Traumatol. 2019;22(4):187–195. doi: 10.1016/j.cjtee.2019.04.002.
- Court-Brown CM, Caesar B. Epidemiology of adult fractures: a review. Int J Care Injured. 2006;37(8):691–697. doi: 10.1016/j.injury.2006.04.130.
- Iglesias-Rodríguez S, Domínguez-Prado DM, García-Reza A, et al. Epidemiology of proximal humerus fractures. J Orthop Surg Res. 2021;16(1):402. doi: 10.1186/s13018-021-02551-x.
- Kim SH, Szabo RM, Marder RA. Epidemiology of humerus fractures in the United States: nationwide emergency department sample, 2008. Arthritis Care Res. 2012;64(3):407–414. doi: 10.1002/acr.21563.
- Bilge O, Dundar ZD, Atılgan N, et al. The epidemiology of adult fractures according to the AO/OTA fracture classification. Ulus Travma Acil Cerrahi Derg. 2022;28:209–216.
- Daoub A, Ferreira PMO, Cheruvu S, et al. Humeral shaft fractures: a literature review on current treatment methods. Open Orthop J. 2022;16(1).
- Hakeem NN, Almaslmani S, Al-Asiri J. Systematic review and Meta-Analysis of patient reported outcome and return to work after surgical vs non-surgical mid shaft humerus fracture. J Orthop Bone Disord. 2022;6(1):000220.
- Martinez-Catalan N. Conservative treatment of proximal humerus fractures: when, how, and what to expect. Curr Rev Musculoskelet Med. 2022;16(2):75–84. doi: 10.1007/s12178-022-09817-9.
- Cosic F, Kirzner N, Edwards E, et al. The translated proximal humerus fracture: a comparison of operative and non-operative management. J Orthop Trauma. 2023;37(9):e341–e348. Available from: http://journals.lww.com/jorthotrauma doi: 10.1097/BOT.0000000000002612.
- Handoll HHG, Elliott J, Thillemann TM, et al. Interventions for treating proximal humeral fractures in adults. Cochrane Database Syst Rev. 2022;2022:1–373.
- Kandemir U, Naclerio EH, McKee MD, et al. Humerus fractures: selecting fixation for a successful outcome. J Orthop Trauma. 2023;6:e259.
- Soler-Peiro M, García-Martínez L, Aguilella L, et al. Conservative treatment of 3-part and 4-part proximal humeral fractures: a systematic review. J Orthop Surg Res. 2020;15(1):347. doi: 10.1186/s13018-020-01880-7.
- Flowers DW, McCallister E, Christopherson R, et al. The safety and effectiveness of early, progressive weight bearing and implant choice after traumatic lower extremity fracture: a systematic review. Bioengineering. 2022;9(12):750. doi: 10.3390/bioengineering9120750.
- Singh S, Rao K, Iyer C, et al. Effect of progressive controlled weight bearing of upper extremity following proximal humeral fracture: randomised control study. Int J Sci Res Publ. 2014;4:1–8.
- Claes LE, Heigele CA. Magnitudes of local stress and strain along bony surfaces predict the course and type of fracture healing. J Biomech. 1999;32(3):255–266. doi: 10.1016/s0021-9290(98)00153-5.
- Claes L, Heigele C, Neidlinger-Wilke C, et al. Effects of mechanical factors on the fracture healing process. Clin Orthop Relat Res. 1998;355(355 Suppl):S132–S147. doi: 10.1097/00003086-199810001-00015.
- Kenwright J, Gardner T. Mechanical influences on tibial fractures healing. Clin Orthop Relat Res. 1998;355(355 Suppl):S179–S190. doi: 10.1097/00003086-199810001-00019.
- Perren SM. Physical and biological aspects of fracture healing with special reference to internal fixation. Clin Orthop Relat Res. 1979;138(138):175–196.
- Sheen RJ, Mabrouk A, Garla VV. Fracture healing overview [Internet]. Treasure Island (FL): StatPearls; 2023 [updated 2023 Apr 8; cited 2023 Jun 20]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK551678/
- Buckwalter JA, Grodzinsky AJ. Loading of healing bone, fibrous tissue, and muscle: implications for orthopaedic practice. J Am Acad Orthop Surg. 1999;7(5):291–299. doi: 10.5435/00124635-199909000-00002.
- Rueff-Barroso CR, Milagres D, Juliana D V, et al. Bone healing in rats submitted to weight-bearing and non-weight-bearing exercises. Med Sci Monit. 2008;14:BR231–BR236.
- Augat P, Simon U, Liedert A, et al. Mechanics and mechano-biology of fracture healing in normal and osteoporotic bone. Int Osteoporos Found Natl Osteoporos Found. 2005;16:S36–43.
- Meys G, Kalmet PHS, Sanduleanu S, et al. A protocol for permissive weight-bearing during allied health therapy in surgically treated fractures of the pelvis and lower extremities. J Rehabil Med. 2019;51(4):290–297. doi: 10.2340/16501977-2532.
- Bretherton CP, Claireaux HA, Achten J, et al. Protocol for the weight-bearing in ankle fractures (WAX) trial: a multicentre prospective non-inferiority trial of early versus delayed weight-bearing after operatively managed ankle fracture. BMC Musculoskelet Disord. 2021;22(1):672. doi: 10.1186/s12891-021-04560-7.
- Hodgson SA, Mawson SJ, Stanley D. Rehabilitation after two-part fractures of the neck of the humerus. J Bone Joint Surg Br. 2003;85(3):419–422. doi: 10.1302/0301-620x.85b3.13458.
- Khojaly R, Mac Niocaill R, Shahab M, et al. Is postoperative non-weight-bearing necessary? INWN study protocol for a pragmatic randomised multicentre trial of operatively treated ankle fracture. Trials. 2021;22(1):369. doi: 10.1186/s13063-021-05319-0.
- Kumar S, Sonar U, Singh I. Fragility fractures in the upper limb: proximal and distal humerus. Br J Hosp Med. 2018;79(3):148–150. doi: 10.12968/hmed.2018.79.3.148.
- Trompeter A. A call to arms: it’s time to bear weight!. Bone Joint J. 2020;102-B(4):403–406. doi: 10.1302/0301-620X.102B4.BJJ-2019-1482.R1.
- Warren J, Sundaram K, Anis H, et al. The association between weight-bearing status and early complications in hip fractures. Eur J Orthop Surg Traumatol. 2019;29(7):1419–1427. doi: 10.1007/s00590-019-02453-z.
- British Orthopaedic Association Trauma Committee. British Orthopaedic Association’s Standards for Trauma (BOAST): care of the older or frail patient with orthopaedic injuries. Injury. 2020;51(7):1419–1421. doi: 10.1016/j.injury.2020.06.005.
- Sacks B, Mughal HN, Ahluwalia A, et al. The BOAST recommendations for care of the older or frail orthopaedic trauma patient. Br J Hosp Med. 2020;81(7):1–8. doi: 10.12968/hmed.2020.0028.
- Ağır İ, Tunçer N, Küçükdurmaz F, et al. Functional comparison of immediate and late weight bearing after ankle bimalleolar fracture surgery. Open Orthop J. 2015;9(1):188–190. doi: 10.2174/1874325001509010188.
- Budharaju A, Hones KM, Hao KA, et al. Rehabilitation protocols in proximal humerus fracture management: a systematic review. Shoulder Elbow. 2023:17585732231182374.
- Passias BJ, Korpi FP, Chu AK, et al. Safety of early weight bearing following fixation of bimalleolar ankle fractures. Cureus. 2020;12(4):e7557. doi: 10.7759/cureus.7557.
- Anderson TB, Duong H. Weight bearing [Internet]. NCBI Bookshelf. A Service of the National Library of Medicine, National Institutes of Health. StatPearls. Treasure Island (FL): StatPearls Publishing; 2022 [cited 2022 Oct 7]. Available from: https://pubmed.ncbi.nlm.nih.gov/31855400/
- Myers DM, Pulido SH, Forsting S, et al. Effect of early weight bearing on outcomes after open reduction and internal fixation of trimalleolar ankle fractures. Journal of. Orthopedics. 2021;44(3):160–165. doi: 10.3928/01477447-20210104-04.
- National Clinical Guideline Centre (The Section on Surgical Procedures Has Been Updated by the 2023 Update). The management of hip fracture in adults update information [Internet]. 2011. Available from: https://www.nice.org.uk/guidance/cg124
- Sernandez H, Riehl J, Fogel J. Do early weight-bearing and range of motion affect outcomes in operatively treated ankle fractures: a systematic review and meta-analysis. J Orthop Trauma. 2021;35(8):408–413. doi: 10.1097/BOT.0000000000002046.
- Ambrósio J, Quental C, Pilarczyk B, et al. Multibody biomechanical models of the upper limb. 2011 symposium on human body dynamics. Procedia IUTAM. 2011;2:4–17. doi: 10.1016/j.piutam.2011.04.002.
- Lu S, Wu J, Xu S, et al. Medial approach to treat humeral mid-shaft fractures: a retrospective study. J Orthop Surg Res. 2016;11:32. doi: 10.1186/s13018-016-0366-1.
- Pidhorz L. Acute and chronic humeral shaft fractures in adults. Orthop Traumatol Surg Res. 2015;101(1 Suppl):S41–S49. doi: 10.1016/j.otsr.2014.07.034.
- Peters MDJ, Godfrey C, McInerney P, et al. Best practice guidance and reporting items for the development of scoping review protocols. JBI Evid Synth. 2022;20(4):953–968. doi: 10.11124/JBIES-21-00242.
- Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–473. doi: 10.7326/M18-0850.
- Peters MDJ, Marnie C, Colquhoun H, et al. Scoping reviews: reinforcing and advancing the methodology and application. Syst Rev. 2021;10(1):263. doi: 10.1186/s13643-021-01821-3.
- Hoppe DJ, Bhandari M. Evidence-based orthopaedics: a brief history symposium. Indian J Orthop. 2008;42:1–7.
- Guimarães NS, Ferreira AJF, Ribeiro Silva RdC, et al. Deduplicating records in systematic reviews: there are free, accurate automated ways to do so. J Clin Epidemiol. 2022;152:110–115. doi: 10.1016/j.jclinepi.2022.10.009.
- Ouzzani M, Hammady H, Fedorowicz Z, et al. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210. doi: 10.1186/s13643-016-0384-4.
- Khalil H, Peters MD, Tricco AC, et al. Conducting high quality scoping reviews-challenges and solutions. J Clin Epidemiol. 2021;130:156–160. doi: 10.1016/j.jclinepi.2020.10.009.
- Piper C. System for the unified management, assessment, and review of information (SUMARI). J Med Libr Assoc. 2019;107:634–636.
- Langhammer CG, Rotunno G, Sebastian C, et al. Small-fragment plate fixation of humeral shaft fractures. Orthopedics. 2023;46(4):198–204. doi: 10.3928/01477447-20230224-02.
- Suzuki T, Hak DJ, Stahel PF, et al. Safety and efficacy of conversion from external fixation to plate fixation in humeral shaft fractures. J Orthop Trauma. 2003;24(7):414–419. doi: 10.1097/BOT.0b013e3181c673a6.
- Szczęsny G, Ratajczak K, Fijewski G, et al. Failures of operative treatment of comminuted fractures of proximal humerus in own material. Ortop Traumatol Rehabil. 2018;20(4):271–284. doi: 10.5604/01.3001.0012.6461.
- James IB, Farrell DJ, Evans AR, et al. Open reconstruction of complex proximal metadiaphyseal fragility fractures of the humerus. Geriatr Orthop Surg Rehabil. 2014;5(1):9–13. doi: 10.1177/2151458514520701.
- Mayer R, Choo A, Zuelzer D. Distal humerus fractures in the elderly: when to fix and when to replace? J Orthop Trauma. 2021;35(Suppl 5):S11–S15. doi: 10.1097/BOT.0000000000002231.
- Patch DA, Reed LA, Hao KA, et al. Understanding postoperative rehabilitation preferences in operatively managed proximal humerus fractures: do trauma and shoulder surgeons differ? J Shoulder Elbow Surg. 2022;31(5):1106–1114. doi: 10.1016/j.jse.2021.12.045.
- Sharareh B, Perkins C. Variation in management of humeral and clavicular shaft fractures amongst fellowship trained orthopedic traumatologists. BMC Musculoskelet Disord. 2020;21(1):618. doi: 10.1186/s12891-020-03639-x.
- Ayoub MS, Tarkin IS. Best care paradigm to optimize functionality after extra-articular distal humeral fractures in the young patient. J Clin Orthop Trauma. 2018;9S:(Suppl 1):S116–S122. doi: 10.1016/j.jcot.2018.02.002.
- Stephens J, Kohrs B, Bushnell L, et al. Distal humerus fractures managed with elbow hemiarthroplasty. J Shoulder Elb Arthroplast. 2020;4:1–6.
- Wajnsztejn A, de Albuquerque DD, Espinola I, et al. Submuscular double bridge plating for complex distal fractures of the humerus: an alternative, safe, and efficient treatment method. Eur J Orthop Surg Traumatol. 2017;27(8):1069–1074. doi: 10.1007/s00590-017-1987-8.
- Suzuki T, Hak DJ, Stahel PF, et al. Safety and efficacy of conversion from external fixation to plate fixation in humeral shaft fractures [Internet]. J Orthop Trauma. 2010;24(7):414–419.
- Beaton DE, Katz JN, Fossel AH, et al. Measuring the whole or the parts? Validity, reliability, and responsiveness of the disabilities of the arm, shoulder and hand outcome measure in different regions of the upper extremity. J Hand Ther. 2001;14(2):128–142. doi: 10.1016/S0894-1130(01)80043-0.
- Vincent J, MacDermid JC. The patient-rated elbow evaluation (PREE). J Physiother. 2012;58(4):274. doi: 10.1016/S1836-9553(12)70134-0.
- Cusick MC, Bonnaig NS, Azar FM, et al. Accuracy and reliability of the Mayo elbow performance score. J Hand Surg Am. 2014;39(6):1146–1150. doi: 10.1016/j.jhsa.2014.01.041.
- Walters JM, Ahmadi S. High-Energy proximal humerus fractures in geriatric patients: a review. Geriatr Orthop Surg Rehabil. 2020;11:2151459320971568. doi: 10.1177/2151459320971568.
- Handoll H, Brealey S, Rangan A, et al. The ProFHer (PROximal fracture of the humerus: evaluation by randomisation) trial – a pragmatic multicentre randomized controlled trial evaluating the clinical effectiveness and cost-effectiveness of surgical compared with non-surgical treatment for proximal fracture of the humerus in adults. Health Technol Assess. 2015;19(24):1–280. doi: 10.3310/hta19240.
- Cunningham B, Tangtiphaiboontana J, Basmajian H, et al. Immediate weight-bearing as tolerated has improved outcomes compared to non-weight-bearing after surgical stabilisation of midshaft clavicle fractures trauma in polytrauma patients. J Orthop Rehabil. 2018;25:16–20.
- Dielwart C, Harmer L, Thompson J, et al. Management of closed diaphyseal humerus fractures in patients with injury severity score ≥17. J Orthop Trauma. 2017;31(4):220–224. doi: 10.1097/BOT.0000000000000768.
- Lee MJ, Ng J, Kok TWK, et al. Does the surgical treatment of concomitant upper limb fractures affect the outcomes of hip fractures in the elderly population? Arch Orthop Trauma Surg. 2023;143(1):353–358. doi: 10.1007/s00402-021-04328-7.
- Ritter V, Lin FC, Miller A, et al. Fixation of humerus shaft fractures in polytrauma patients does not improve short-term outcomes. Injury. 2023;54(2):573–577. doi: 10.1016/j.injury.2022.11.060.
- Turabi RY, Wyatt D, Guerra S, et al. Barriers and facilitators of weight bearing after hip fracture surgery among older adults. A scoping review. Osteoporos Int. 2023;34(7):1193–1205. doi: 10.1007/s00198-023-06735-5.
- Seo H, Lee GJ, Shon HC, et al. Factors affecting compliance with weight-bearing restriction and the amount of weight-bearing in the elderly with femur or pelvic fractures. Ann Rehabil Med. 2020;44(2):109–116. doi: 10.5535/arm.2020.44.2.109.
- Sivapathasuntharam D, Smith G, Master MA, et al. Fragility fractures of the pelvis in the older population. Age Ageing. 2022;51:1–5.
- Barone A, Giusti A, Pizzonia M, et al. Factors associated with an immediate weight-bearing and early ambulation program for older adults after hip fracture repair. Arch Phys Med Rehabil. 2009;90(9):1495–1498. doi: 10.1016/j.apmr.2009.03.013.
- Raza M, Walters S, Richardson C, et al. Weight-bearing in trauma surgery (WiTS) study: a national survey of UK trauma & orthopaedic multidisciplinary health professionals. Injury. 2022;53(2):427–433. doi: 10.1016/j.injury.2021.12.019.
- BONE Collaborative. Weight-bearing in ankle fractures: an audit of UK practice. Foot. 2019;39:28–36. doi: 10.1016/j.foot.2019.02.005.
- National Institute for Health and Care Excellence. Fractures (non-complex): assessment and management NICE guideline [Internet]. 2023 [cited 2023 May 30]. Available from: www.nice.org.uk/guidance/ng38.
- Richardson C, Bretherton CP, Raza M, et al. The fragility fracture postoperative mobilisation multicentre audit. Bone Joint J. 2022;104-B(8):972–979. doi: 10.1302/0301-620X.104B8.BJJ-2022-0074.R1.
- Tarrant SM, Attia J, Balogh ZJ. The influence of weight-bearing status on post-operative mobility and outcomes in geriatric hip fracture. Eur J Trauma Emerg Surg. 2022;48(5):4093–4103. doi: 10.1007/s00068-022-01939-6.
- Owyang D, Bakhsh A, Brewer D, et al. Patient and public involvement within orthopaedic research: a systematic review. J Bone Joint Surg. 2021;103:1–6.
- Kortebein P, Symons TB, Ferrando A, et al. Functional impact of 10 days of bed rest in healthy older adults. J Gerontol A Biol Sci Med Sci. 2008;63(10):1076–1081. doi: 10.1093/gerona/63.10.1076.
- Bledsoe JG, Geraud S, Cannada LK. Immediate weight bearing after fixation of humeral shaft fractures with small fragment hybrid plating: a biomechanical analysis. J Orthop Exp Innov. 2021;2(2):1–9. doi: 10.60118/001c.25328.
- Patel J, Motwani G, Shah H, et al. Outcome after internal fixation of intraarticular distal humerus (AO type B & C) fractures: preliminary results with anatomical distal humerus LCP system. J Clin Orthop Trauma. 2017;8(1):63–67. doi: 10.1016/j.jcot.2017.02.004.
- Varady PA, von Rüden C, Greinwald M, et al. Biomechanical comparison of anatomical plating systems for comminuted distal humeral fractures. Int Orthop. 2017;41(9):1709–1714. doi: 10.1007/s00264-017-3444-z.
- Ji JH, Jeong JJ, Kim YY, et al. Clinical and radiologic outcomes of arthroscopic suture bridge repair for the greater tuberosity fractures of the proximal humerus. Arch Orthop Trauma Surg. 2017;137(1):9–17. doi: 10.1007/s00402-016-2586-6.
- Rangan A, Handoll H, Brealey S, et al. Surgical vs nonsurgical treatment of adults with displaced fractures of the proximal humerus the PROFHER randomized clinical trial. JAMA J Am Med Assoc. 2015;313(10):1037–1047. doi: 10.1001/jama.2015.1629.
- Tingstad EM, Wolinsky PR, Shyr Y, et al. Effect of immediate weightbearing on plated fractures of the humeral shaft background: this study evaluated. J Trauma. 2000;49(2):278–280. doi: 10.1097/00005373-200008000-00014.
- British Geriatrics Society. BGS joining the dots - a blueprint for preventing and managing frailty in older people [Internet]. 2023 [cited 2023 Jun 22]. Available from: https://www.bgs.org.uk/Blueprint
- Donohoe E, Roberts HJ, Miclau T, et al. Management of lower extremity fractures in the elderly: a focus on post-operative rehabilitation. Injury. 2020;51 Suppl 2:S118–S122. doi: 10.1016/j.injury.2020.04.050.
- Lamb LC, Montgomery SC, Wong Won B, et al. A multidisciplinary approach to improve the quality of care for patients with fragility fractures. J Orthop. 2017;14(2):247–251. doi: 10.1016/j.jor.2017.03.004.
- McCartney M, Finnikin S. Evidence and values in the NHS: choosing treatments and interventions well. Br J Gen Pract. 2019;69(678):4–5. doi: 10.3399/bjgp19X700313.
- Schumaier A, Grawe B. Proximal humerus fractures: evaluation and management in the elderly patient. Geriatr Orthop Surg Rehabil. 2018;9:2151458517750516. doi: 10.1177/2151458517750516.
- Pollock D, Peters MDJ, Khalil H, et al. Recommendations for the extraction, analysis, and presentation of results in scoping reviews. JBI Evid Synth. 2023;21(3):520–532. doi: 10.11124/JBIES-22-00123.
- Bergdahl C, Ekholm C, Wennergren D, et al. Epidemiology and patho-anatomical pattern of 2,011 humeral fractures: data from the Swedish fracture register. BMC Musculoskelet Disord. 2016;17:1–10.
- Navarro CM, Brolund A, Ekholm C, et al. Treatment of humerus fractures in the elderly: a systematic review covering effectiveness, safety, economic aspects and evolution of practice. PLoS One. 2018;13(12):e0207815. doi: 10.1371/journal.pone.0207815.