Abstract
Purpose
A large proportion of people die in the years following dysvascular partial foot amputation (PFA) or transtibial amputation (TTA) given the long-term consequences of peripheral vascular disease and/or diabetes. A critical appraisal of recent research is needed to understand the underlying cause of variation and synthesise data for use in consultations about amputation surgery and patient-facing resources. This systematic review aimed to describe proportionate mortality following dysvascular PFA and to compare this between PFA and TTA.
Materials and methods
The review protocol was registered in PROSPERO (CRD42023399161). Peer-reviewed studies of original research were included if they: were published in English between 1 January 2016, and 12 April 2024, included discrete cohorts with PFA, or PFA and TTA, and measured proportionate mortality following dysvascular amputation.
Results
Seventeen studies were included in the review. Following dysvascular PFA, proportionate mortality increased from 30 days (2.1%) to 1-year (13.9%), 3-years (30.1%), and 5-years (42.2%). One study compared proportionate mortality 1-year after dysvascular PFA and TTA, showing a higher relative risk of dying after TTA (RR 1.51).
Conclusions
Proportionate mortality has not changed in recent years. These results are comparable to a previous systematic review that included studies published before 31 December 2015.
It is important to ensure data describing mortality in the years following dysvascular partial foot or transtibial amputation is up to date and accurate.
Evidence about proportionate mortality has not changed in recent years and the results are comparable to previous systematic reviews.
Data describing mortality outcomes can be used in decision aids that support conversations about the choice of amputation level.
Implications for rehabilitation
Introduction
Dysvascular partial foot amputation (PFA) or transtibial amputation (TTA) is a common sequel to the long-term complications of peripheral vascular disease (PVD) and/or diabetes that leads to a reduction of blood supply to a body part and complications such as ulceration, skin breakdown, and infection [Citation1–3].
Many people who undergo dysvascular PFA or TTA are older and have multiple comorbidities such as renal disease, or coronary heart disease [Citation1,Citation4]. As such, a large proportion of people die in the years following dysvascular PFA or TTA [Citation3]. For example, based on a systematic review that included studies published until the 31 December 2015 [Citation5], the proportion of people that died following dysvascular PFA increased from 30 days (2.8%, 95%CI 2.2–3.6) to 1-year (17.3%, 95%CI 14.6–20.2), 3-years (30.6%, 95%CI 23.0–38.7), and 5-years (41.2%, 95%CI 32.6–50.1). In comparison, those people who underwent TTA had a significantly greater relative risk (RR) of dying at 30 days (RR 2.6, 95%CI 1.6–4.1, p < 0.001), 1-year (RR 1.5, 95%CI 1.4–1.6, p < 0.001), and 5-years (RR 1.3, 95%CI 1.2–1.5, p < 0.001); noting there were no data comparing the RR of dying 3-years after PFA or TTA [Citation5]. The greater RR of dying following TTA was thought to reflect that people considered suitable candidates for TTA likely had more advanced systemic disease which made PFA unsuitable [Citation6–8].
In recent years, some studies have reported that the proportion of people who died in the years following dysvascular PFA and TTA has declined [Citation9–11]. By contrast, others suggest that proportionate mortality has increased [Citation7,Citation12–16]. To understand the variation between these studies, a critical appraisal is necessary to understand how different methodologies and populations may have influenced these results. Only then can we determine whether proportionate mortality following dysvascular PFA has changed in recent years and how the RR compares to TTA.
Accurate and up-to-date evidence about proportionate mortality following dysvascular PFA, and how this compares to TTA, is important given these data are used to counsel people about the likely outcomes of these different surgeries, and thereby help inform difficult decisions about the choice of amputation level [Citation5,Citation17–27]. These data are also incorporated into patient-facing resources, such as decision aids, that present unbiased information about the treatment options (e.g., PFA vs. TTA) and the likely outcomes of each (e.g., proportionate mortality over time) [Citation5,Citation17–27]. Given this background, the aims of this systematic review were to:
Describe proportionate mortality following dysvascular PFA.
Compare proportionate mortality between dysvascular PFA and TTA.
Methods
This systematic review used the same methods as reported in the published protocol [Citation28] and related peer reviewed research [Citation5] and as such, a summary of the methods is reported here. This systematic review was registered with PROSPERO (CRD42023399161) and is reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [Citation29] including a copy of the PRISMA checklist (Additional File 1).
Search strategy
A systematic search of the literature was conducted using MEDLINE, EMBASE, PsycINFO, AMED, CINAHL, ProQuest Nursing and Allied Health, and Web of Science. A list of search terms related to the amputation level and mortality, along with their synonyms and acronyms, were used in conjunction with wildcards and Boolean operators as part of a title, abstract, and keyword search. As the restriction of non-English studies does not seem to alter the outcome of systematic reviews and meta-analyses, the search was limited to the English language [Citation30,Citation31]. Searches were limited to studies published between 1 January 2016 and 12 April 2024, given a preceding systematic review included studies published to 31 December 2015 [Citation5]. In keeping with the PRISMA guidelines [Citation29], an illustrative search is presented for one database () with the remaining searches included in Additional File 2. The search strategy was rigorously developed and tested as detailed in the systematic review protocol [Citation28].
Table 1. Example search for CINAHL database.
To ensure relevant publications were not overlooked, studies that met the inclusion criteria were hand-searched. A forward citation search was performed using Google Scholar to find studies not yet indexed in the aforementioned databases [Citation28].
Selection process
The following criteria were used to determine inclusion:
Peer-reviewed studies.
Studies published in the English language.
Studies published between 1 January 2016 and 12 April 2024.
For the first aim – studies must include cohorts with dysvascular PFA, irrespective of the level of PFA.
For the second aim – studies must include separate cohorts with dysvascular PFA and TTA
Studies that measure proportionate mortality (or present data on survival from which proportionate mortality can be calculated) regardless of the time point at which it was measured following amputation.
Studies that group together people with different levels of lower limb amputation (e.g., PFA and TTA) or causes (e.g., trauma and PVD) were excluded, along with editorials, letters, conference abstracts, and opinion pieces. The International Standards Organisation (ISO) definitions of PFA and TTA were used and therefore, all levels of PFA (including toe amputation) were included [Citation32]. In keeping with the ISO definition, ankle disarticulation (i.e., Syme amputation) was not considered a PFA and as such, studies regarding this amputation level were excluded [Citation32]. Given the ambiguity of terms such as “minor” or “major” amputation, we have not used those terms, except when reporting the results of other studies where those collective nouns were used. In those instances, we have described the level of amputation included using ISO terms.
Search results were exported directly to an EndNote 20 (Clarivate, Philadelphia, PA) library and duplicates removed. The primary investigator (Z.W.) screened the search results based on a review of the title, abstract, or full-text study as necessary. An additional opinion was sought from a second investigator (M.D.) in cases of doubt, with disagreements resolved through discussion until consensus.
Data collection process
Based on the Cochrane Consumers and Communication Review Group’s data extraction template, [Citation33] data from included studies were systematically recorded in an Excel (Microsoft Corporation Inc., Redmond, WA) spreadsheet including: socio-demographic, methodological, proportionate mortality, and quality appraisal details (Additional File 3). This spreadsheet was developed, tested, and used in a previous systematic review [Citation5].
For each of the included studies, data were initially extracted by one investigator (either E.R. or Z.W.) before being independently verified by a second investigator (either M.D. or E.R.). Inconsistencies in data entry were resolved through discussion until consensus. If additional information or clarification was required, the authors of the original research were contacted via email with one follow-up a week later, as needed.
Study risk of bias assessment
The McMaster Critical Review Forms were used to assess methodological quality and identify sources of bias [Citation34]. The appraisal tool was appropriate for use with a wide variety of study designs and included guidelines to reduce the likelihood of errors [Citation35–37]. Results from the McMaster Critical Review Form were recorded in the Excel spreadsheet with detailed comments to support checklist items (Additional File 3).
Statistical analyses
Random effects proportionate meta-analyses (StatsDirect, Wirral, UK) were conducted to synthesise proportionate mortality at discrete time points following amputation. All studies were included in the proportionate meta-analyses as preserving information regarding the heterogeneity of results was important to explore underlying causes of variation and uncertainty in the point estimates reported [Citation38,Citation39]. Results were reported using a forest plot along with the point estimates and 95% confidence intervals. Relative risk meta-analyses were also undertaken to compare the RR of mortality between the PFA and TTA cohorts. Heterogeneity of the results between studies was quantified using the I2 statistic and explored using the findings of the risk of bias assessment. Meta-analyses were accompanied by a narrative review to explain the variations between studies using the findings from the risk of bias and extracted data.
Results
Study selection
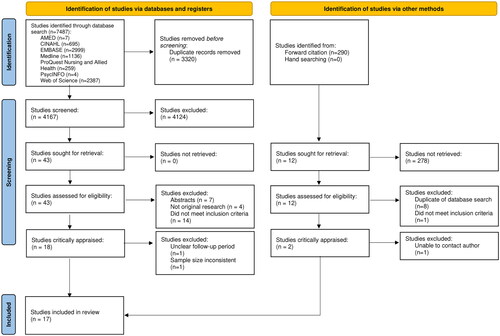
The database search yielded 7487 studies (). Once duplicates were removed, 3320 studies were screened against the inclusion criteria based on the title and abstract. Forty-three full-text studies were examined, of which 18 met the inclusion criteria. The forward citation search yielded two additional studies that both met the inclusion criteria. Of the 20 studies that met the inclusion criteria, two were excluded due to significant methodological or reporting issues including: inconsistent description of number of people included [Citation9] or the time period over which data were collected [Citation40]. One study was excluded given “minor” amputations were not operationally defined and we were unable to confirm the included amputation levels after efforts to contact the authors [Citation41]. Therefore, 17 studies were included in this review ().
Study characteristics
The majority of included studies reported outcomes from countries with well-developed healthcare systems including the USA [Citation11,Citation12,Citation42,Citation43], Malta [Citation44], China [Citation45,Citation46], Italy [Citation13], Denmark [Citation47], UK [Citation15,Citation48], and Spain [Citation49].
Given the inclusion criteria, all the included studies reported proportionate mortality following dysvascular PFA [Citation11–15,Citation42–53]. One study also presented proportionate mortality for separate PFA and TTA cohorts [Citation53]. The time points at which proportionate mortality was reported have been summarised in .
Table 2. Summary of study designs and outcomes of included studies.
The majority of the included studies were retrospective cohort designs () from single-centres [Citation12,Citation13,Citation15,Citation42–47,Citation49,Citation52] and as such, they generally contained smaller samples when compared to studies of hospital network [Citation11,Citation51] or national-level [Citation14,Citation48,Citation53] data sets ().
Table 3. Summary demographic characteristics of included studies.
Most studies reported proportionate mortality for a discrete level of PFA such as: transmetatarsal [Citation12,Citation15,Citation42,Citation46,Citation53], toe [Citation44,Citation45,Citation50], Chopart [Citation13], or partial first ray [Citation50]. Two studies grouped toe and ray amputations together [Citation11,Citation52]. Five studies did not stratify their data by level of PFA and instead described the cohort using the collective noun “minor amputation” [Citation14,Citation43,Citation47–49,Citation51] which included different levels of PFA. While some studies also included people with TTA [Citation14,Citation43,Citation49,Citation51–53], most grouped people with TTA into a single “major amputation” cohort along with people living with transfemoral amputation; the exception reported proportionate mortality for the TTA-only cohort [Citation53] in keeping with the inclusion criteria. None of the included studies were designed to compare proportionate mortality between cohorts based on level of amputation.
Given the population of interest, the participants in the included studies were typically older males living with diabetes and other comorbidities ().
Quality appraisal/risk of bias
There were several recurrent issues that impacted both the internal and external validity of the included studies. Each of these issues has been discussed in the paragraphs that follow.
While most studies reported age, sex, and the presence of diabetes, more detailed information about the participants was often poorly reported which made it difficult to generalise these findings to the wider population of people living with dysvascular PFA or TTA. For example, sociodemographic factors such as race/ethnicity, or the presence of common comorbidities known to affect mortality (e.g., the presence of coronary arterial disease) were inconsistently reported (). Similarly, the type of diabetes was often not reported despite the fact that proportionate mortality differs for cohorts with type 1 and type 2 diabetes [Citation47,Citation54].
Cointervention likely affected all included studies given the healthcare required to manage comorbid conditions such as end stage renal disease or coronary heart disease (). Looking specifically at coronary heart disease as an illustrative example, common interventions such as smoking cessation, or the use of beta blockers to manage hypertension, are known to affect mortality outcomes.
There were several issues with the design of studies that reduced confidence in the proportionate mortality reported. Ten studies retrospectively measured mortality in a discrete time window (e.g., 5-year post-amputation) and used that data to estimate proportionate mortality from Kaplan–Meier’s analyses [Citation13,Citation14,Citation42,Citation43,Citation45–49,Citation51]. Given this approach, these studies likely included many data points that underpinned the 1-year proportionate mortality estimate, and comparatively few data points for the 5-year mortality estimate, increasing uncertainty. None of these studies reported an a priori sample size calculation to justify the number of participants required for the Kaplan–Meier analysis at these different time points, nor did they report confidence intervals alongside the Kaplan–Meier estimates to showcase uncertainty of the estimated proportionate mortality in the years after amputation as participants were censored (i.e., died, or lost to follow up and removed from the analysis).
Proportionate mortality
Given the inclusion criteria, all included studies reported either all-cause proportionate mortality (or survival from which mortality could be calculated) and included additional information regarding a discrete time point at which mortality was measured (e.g., 1-year after amputation).
Proportionate mortality was reported either by count of the sample that had died at each time point [Citation11,Citation12,Citation15,Citation44,Citation50,Citation52,Citation53] or by using a Kaplan–Meier analysis to generate an estimate [Citation13,Citation14,Citation42,Citation43,Citation45–49,Citation51]. All studies reported proportionate mortality at 1-, 3-, or 5-years post-amputation [Citation11–15,Citation42–53]. There were also isolated data for other time points post-amputation including: 30 days [Citation12]; 1-, 3-, 6-, and 9-months [Citation15,Citation44,Citation46]; or 2-, 4-, 6-, 7-, and 8-years [Citation13,Citation14,Citation42,Citation43,Citation51].
Consistent with the method we adopted from a previous systematic review [Citation5], we reported proportionate mortality for 30 days, and 1-, 3-, and 5-years post-amputation.
Proportionate mortality following dysvascular PFA
For 30 day mortality, one study [Citation12] reported that 2.1% (no confidence interval) of individuals died within 30 days after PFA (specifically, transmetatarsal amputation). Given this baseline, proportionate mortality increased from 1-year (13.9%, 95%CI 11.6–16.3), 3-years (30.1%, 95%CI 25.1–35.4), and 5-years (42.2%, 95%CI 36.0–48.5) following PFA (). There was considerable heterogeneity in the results between studies (I2 >80%, p < 0.01). While the heterogeneity between studies did not detract from the precision of the point estimate 1-year post-PFA, uncertainty increased over time (). Studies that contributed most to the heterogeneity received less weighting in the random-effects meta-analysis and thereby had less influence on the point estimate.
Figure 2. Proportionate mortality at 1-, 3-, and 5-years after partial foot amputation (random effects meta-analysis).
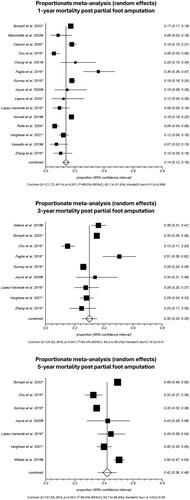
As measures of proportionate mortality do not control for variations in the sample, such as older age or the presence of comorbidities, these were a source of variation in the results between studies. For example, in the study by Faglia et al. [Citation13] proportionate mortality at 1-year post-amputation was relatively high (36.0%, 95%CI 26.0–47.0%) compared to other studies (); likely because the sample was older (71.4 ± 9.3 years), had diabetes for many years (19.3 ± 10.9 years), included a large proportion with failed previous amputations (42.5%), had significant wounds characterised by exposure of the bone or joint with infection and ischaemia (69.9%, Texas wound classification D3), and required emergency surgery due to gangrene or osteomyelitis (65.9%). As such, it is not surprising that proportionate mortality was greater when compared to other studies with more representative samples. By contrast, Chu et al. [Citation45] reported a much lower proportionate mortality at 1-year post-amputation (6.0%, 95%CI 3.0–9.0%, ). While participants in this investigation were similar in age (69.27 ± 9.39 years) to Faglia et al. [Citation13], it is likely they had less advanced systemic disease given that the time with diabetes was shorter (weighted mean 12.8 ± 7.3 years) and that toe- or metatarsophalangeal-amputation was clinically indicated [Citation45].
No studies reported proportionate mortality stratified by different levels of PFA.
Proportionate mortality following dysvascular PFA compared to TTA
One study reported proportionate mortality 1-year after PFA (17.7%) and TTA (24.7%) [Citation53]. In comparison to the PFA cohort (specifically, transmetatarsal amputation), the TTA cohort had a significantly greater RR of dying at 1-year post-amputation (RR 1.5, 95%CI 1.4–1.7, p < 0.0001). Personal correspondence with the authors confirmed that the participants in this study [Citation53] were the same as another cohort study [Citation55] with the exception of a very small proportion who were excluded in the later publication [Citation55] due to constraints of the regression modelling. Based on the demographic and health information for the PFA and TTA cohorts [Citation55], it was possible to discern that, while the PFA and TTA cohorts were similar in terms of age (PFA 65.6 ± 10.0, TTA 66.8 ± 10.2 years), proportion with diabetes (PFA 82.9%, TTA 77.8%) and sex (99.1% male for both PFA and TTA), the PFA cohort had a higher proportion of people with normal Ankle Brachial Index compared to the TTA cohort (PFA 47.0%, TTA 39.8%). The PFA sample also had a smaller proportion with chronic obstructive pulmonary disease (PFA 13.3%, TTA 18.1%) and any revascularisation in the past year (PFA 35.8%, TTA 41.9%). Finally, the PFA sample also showed a higher proportion with independent physical function (PFA 65.0%, TTA 56.5%). These data suggest that the individuals in the TTA cohort had worse systemic health at the point of amputation compared to the PFA cohort, which likely contributed to the higher mortality in the years that followed.
Discussion
Given the aim of this systematic review, the following discussion has been subdivided to interpret the proportionate mortality results for 30 days, 1-, 3-, and 5-years following dysvascular PFA, and compare these outcomes between cohorts with PFA and TTA. The final subsections of the discussion focus on the clinical relevance and limitations of this review.
Proportionate mortality following dysvascular PFA
Following PFA, proportionate mortality increased over time from 2.1% (30 days), 13.9% (1-year), 30.1% (3-years), and 42.2% (5-years). These results are similar to other systematic reviews [Citation5,Citation56] that reported proportionate mortality at these same time points (). The similarities in findings between these reviews reflect, to some extent, the similarity of method designs. For example, these systematic reviews [Citation5,Citation56] focused on original research of people with dysvascular amputation and used a random-effects meta-analysis to synthesise data at the same timepoints. These reviews [Citation5,Citation56] also included many of the same original studies, further explaining the similarities given the time periods of included studies overlapped.
Table 4. Proportionate mortality reported in different systematic reviews.
While the findings in this study were very similar to previous systematic reviews [Citation5,Citation56], there were some noteworthy differences. First, in this study, proportionate mortality 30 days after PFA was lower than the 95%CI reported in other systematic reviews (). Given that just one included study reported a 30-day mortality rate [Citation12], we suggest that the results from the previous systematic reviews [Citation5,Citation56] provide a more reliable estimate of 30-day proportionate mortality as they included several studies that allow both a point estimate and 95% confidence intervals to be calculated.
Second, while the point estimates and confidence intervals were similar across these systematic reviews (), we do not have confidence in the 95% confidence interval reported by Yammine et al. [Citation56] at 5-year post-PFA given the point estimate sits outside the confidence interval (44.1, 95%CI 47.1–47.6), and the confidence interval seems narrow given the heterogeneity reported (I2 = 88.7%). Finally, while previous systematic reviews [Citation5,Citation56] have used similar databases, search terms, and inclusion criteria, there were differences in the choice of critical appraisal checklist and, more importantly, how these data were used to explain the underlying causes of variation between studies. One of the strengths of this review was that the results narrative synthesised observations from the critical appraisal (i.e., McMaster appraisal checklist) and extracted data (e.g., patient demographics) to explain variation between studies, such as the impact that older age or comorbid health conditions had on mortality outcomes. The ability to explain the underlying causes of variation between studies is important to engender confidence in the point estimates reported and support clinicians to apply these findings to a diverse population.
Proportionate mortality following dysvascular PFA compared to TTA
Based on the results of the one included study [Citation53] that reported proportionate mortality 1-year after dysvascular PFA (17.7%) and TTA (24.7%), the RR of dying in the first year after TTA was 50% higher than after PFA (RR 1.5, 95%CI 1.4–1.7). This observation was similar to a previous systematic review (RR 1.5, 95%CI 1.4–1.6) that included numerous studies given the time window for inclusion included all indexed studies up to 31 December 2015, and therefore we can have confidence in the finding despite only having one included study [Citation12].
Studies that have used appropriate statistical techniques that control for interactions between factors that confound proportionate mortality (e.g., older age, higher amputation level, presence of comorbid disease such as end-stage renal disease or coronary arterial disease) have reported that amputation level does not independently affect mortality [Citation6–8]. Therefore, the increased RR of dying in the years following TTA (as compared to PFA) may be due to the more advanced systemic disease that made the TTA a preferred amputation surgery, and has little to do with the choice of amputation level per se [Citation6–8].
Given this systematic review used the same method as a previous systematic review [Citation5], together they provide continuous data from the beginning of indexed databases to 12 April 2024. Meta-analyses based on aggregated results show the proportionate mortality after PFA increased over time from 30 days (2.8%, 95%CI 2.2–3.4), to 1-year (15.3%, 95%CI 13.8–17.0), 3-years (30.3%, 95%CI 26.5–34.2), and 5-years (41.5%, 95%CI 35.9–47.2) as depicted in . Similarly, in comparison to the PFA cohort, the TTA cohort had a significantly greater RR of dying at 1-year post-amputation (RR 1.45, 95%CI 1.36–1.54, p < 0.0001).
Figure 3. Updated proportionate mortality at 1-, 3-, and 5-years after partial foot amputation (random effects meta-analysis) including data from this review and preceding review [Citation5].
![Figure 3. Updated proportionate mortality at 1-, 3-, and 5-years after partial foot amputation (random effects meta-analysis) including data from this review and preceding review [Citation5].](/cms/asset/3ce611a4-0ddc-4fa3-8751-5461858022e8/idre_a_2355988_f0003_b.jpg)
Clinical relevance
Proportionate mortality following dysvascular PFA has not changed significantly in recent years given the results of this systematic review are comparable to a previous systematic review that included literature published on 31 December 2015 [Citation5]. Given this finding, the proportionate mortality reported in patient decision aids [Citation5,Citation25,Citation57] is accurate and as such, only a minor revision is necessary to update any supporting references based on this review.
Future research
In recent years, the volume of literature reporting proportionate mortality following dysvascular PFA and PFA/TTA has grown substantially compared to a previous systematic review [Citation5]. However, many of the new studies are from small centres with a small number of participants and do not provide a compelling rationale that would justify further research reporting proportionate mortality. We suggest that further research of isolated healthcare services with small patient numbers will not add value to the already well-developed body of literature on this topic unless there are significant changes in clinical practice that have potential to improve mortality outcomes that warrant publication [Citation58].
While this systematic review focused on proportionate mortality, there are many other outcomes that are also important to help inform difficult decisions about amputation surgery including: mobility, health-related quality of life, delayed wound healing, or the risk of reamputation, among others [Citation5,Citation25,Citation57]. There are opportunities to review literature on these topics to help ensure current evidence has been appraised and synthesised to provide the data needed to inform surgical consultations or patient-facing decision aids.
Limitations
The results of this investigation should be considered in light of a number of limitations.
We acknowledge that proportionate mortality has been reported for other timepoints not included in this review such as 3-, 6-, and 9-months [Citation15,Citation44,Citation46]; or 2-, 4-, 6-, 7-, and 8-years [Citation13,Citation14,Citation42,Citation43,Citation51]. Since we adopted the method of a previous systematic review [Citation12], we used the same timepoints to report the outcomes given they are the most commonly reported, and adequately demonstrate changes in mortality and RR over time. For those wanting to utilise data from other time points, or look at longer term mortality outcomes, these data have been reported in Additional File 3.
Given the multiple timepoints at which proportionate mortality has been reported, the result narratives deliberately use illustrative examples to showcase the risks of bias and the impact on the results, rather than reporting risk of bias for each study. Full details of the risk of bias assessment are included as Additional File 3.
Conclusions
This systematic review highlights that proportionate mortality following dysvascular PFA, or PFA and TTA, has not changed in recent years, despite an increase in new research. As such, outcomes of proportionate mortality reported in a previous systematic review and patient-facing decision aids reflect contemporary evidence.
Supplemental Material
Download Zip (135.6 KB)Acknowledgements
We would like to acknowledge Professor Kate Webster of La Trobe University for producing the meta-analyses in this review.
Disclosure statement
Professor Michael Dillon, Dr Matthew Quigley, and Professor Stefania Fatone were the developers of a patient-facing decision aid (i.e., Amputation Decision Aid) [Citation57]. No financial support was received for the current systematic review. The authors declare no other competing interests.
Data availability statement
The authors confirm that the data supporting the findings of this study are available within the article and its supplementary materials.
Additional information
Funding
References
- Coke LA, Dennison-Himmelfarb C. Peripheral arterial disease prevention in women: awareness and action. J Cardiovasc Nurs. 2019;34(6):427–429. doi: 10.1097/JCN.0000000000000617.
- Varaki ES, Gargiulo GD, Penkala S, et al. Peripheral vascular disease assessment in the lower limb: a review of current and emerging non-invasive diagnostic methods. Biomed Eng Online. 2018;17(1):61. doi: 10.1186/s12938-018-0494-4.
- Dillon M, Quigley M, Fatone S. A systematic review describing incidence rate and prevalence of dysvascular partial foot amputation; how both have changed over time and compare to transtibial amputation. Syst Rev. 2017;6(1):230. doi: 10.1186/s13643-017-0626-0.
- Song P, Rudan D, Zhu Y, et al. Global, regional, and national prevalence and risk factors for peripheral artery disease in 2015: an updated systematic review and analysis. Lancet Glob Health. 2019;7(8):e1020–e1030. doi: 10.1016/S2214-109X(19)30255-4.
- Dillon MP, Quigley M, Fatone S. Outcomes of dysvascular partial foot amputation and how these compare to transtibial amputation: a systematic review for the development of shared decision-making resources. Syst Rev. 2017;6(1):54. doi: 10.1186/s13643-017-0433-7.
- Izumi Y, Satterfield K, Lee S, et al. Mortality of first-time amputees in diabetics: a 10-year observation. Diabetes Res Clin Pract. 2009;83(1):126–131.
- Stern JR, Wong CK, Yerovinkina M, et al. A meta-analysis of long-term mortality and associated risk factors following lower extremity amputation. Ann Vasc Surg. 2017;42:322–327. doi: 10.1016/j.avsg.2016.12.015.
- Tseng C-H, Chong C-K, Tseng C-P, et al. Mortality, causes of death and associated risk factors in a cohort of diabetic patients after lower-extremity amputation: a 6.5-year follow-up study in Taiwan. Atherosclerosis. 2008;197(1):111–117. doi: 10.1016/j.atherosclerosis.2007.02.011.
- Humphrey JA, Kanthasamy S, Coughlin P, et al. Outcome of trans-metatarsal amputations in patients with diabetes mellitus. Foot. 2019;40:22–26.
- Spoden M, Nimptsch U, Mansky T. Amputation rates of the lower limb by amputation level – observational study using German National Hospital Discharge Data from 2005 to 2015. BMC Health Serv Res. 2019;19(1):163. doi: 10.1186/s12913-019-3973-9.
- Rolle NP, Kawaji Q, Morton C, et al. Risk factors for lower extremity minor amputation conversion to major amputation. Ann Vasc Surg. 2024;104:166–173. doi: 10.1016/j.avsg.2023.12.066.
- Adams B, Edlinger J, Ritterman WM, et al. Three-year morbidity and mortality rates after nontraumatic transmetatarsal amputation. J Foot Ankle Surg. 2018;57(5):967–971.
- Faglia E, Clerici G, Frykberg R, et al. Outcomes of Chopart amputation in a tertiary referral diabetic foot clinic: data from a consecutive series of 83 hospitalized patients. J Foot Ankle Surg. 2016;55(2):230–234.
- Gurney JK, Stanley J, York S, et al. Risk of lower limb amputation in a national prevalent cohort of patients with diabetes. Diabetologia. 2018;61(3):626–635. doi: 10.1007/s00125-017-4488-8.
- Joyce A, Yates B, Cichero M. Transmetatarsal amputation: a 12 year retrospective case review of outcomes. Foot. 2020;42:101637. doi: 10.1016/j.foot.2019.08.008.
- Thorud JC, Plemmons BD, Buckley CJ, et al. Mortality after nontraumatic major amputation among patients with diabetes and peripheral vascular disease: a systematic review. J Foot Ankle Surg. 2016;55(3):591–599.
- Agoritsas T, Heen AF, Brandt L, et al. Decision aids that really promote shared decision making: the pace quickens. Brit Med J. 2015;350:7624.
- Anderson CB, Kittelson AJ, Wurdeman SR, et al. Understanding decision-making in prosthetic rehabilitation by prosthetists and people with lower limb amputation: a qualitative study. Disabil Rehabil. 2023;45(4):723–732.
- Barry MJ, Edgman-Levitan S. Shared decision making—the pinnacle of patient-centered care. N Engl J Med. 2012;366(9):780–781. doi: 10.1056/NEJMp1109283.
- Bodde MI, Dijkstra PU, Schrier M, et al. Informed decision-making regarding amputation for complex regional pain syndrome type I. J Bone Joint Surg Am. 2014;96A(11):930–934.
- Elwyn G, Frosch D, Thomson R, et al. Shared decision making: a model for clinical practice. J Gen Intern Med. 2012;27(10):1361–1367. doi: 10.1007/s11606-012-2077-6.
- Fried TR. Shared decision making—finding the sweet spot. N Engl J Med. 2016;374(2):104–106. doi: 10.1056/NEJMp1510020.
- Gudbranson E, Galivanche A, Mercier M, et al. Shared decision-making in limb salvage versus amputation: a commentary and review. J Orthoplast Surg. 2022;9:111–115.
- Hoffmann T, Jansen J, Glasziou P. The importance and challenges of shared decision making in older people with multimorbidity. PLoS Med. 2018;15(3):e1002530. doi: 10.1371/journal.pmed.1002530.
- Quigley M, Dillon MP, Fatone S. Development of shared decision-making resources to help inform difficult healthcare decisions: an example focused on dysvascular partial foot and transtibial amputations. Prosthet Orthot Int. 2018;42(4):378–386. doi: 10.1177/0309364617752984.
- Rassin M, Tzevlin V, Malul E, et al. Retrospective study of emerging themes in the decision-making process of patients considering amputation. J Vasc Nurs. 2012;30(2):54–60.
- Schrier E, Dijkstra PU, Zeebregts CJ, et al. Decision making process for amputation in case of therapy resistant complex regional pain syndrome type-I in a Dutch specialist centre. Med Hypotheses. 2018;121:15–20.
- Dillon MP, Fatone S, Quigley M. Describe the outcomes of dysvascular partial foot amputation and how these compare to transtibial amputation: a systematic review protocol for the development of shared decision-making resources. Syst Rev. 2015;4(1):173–173. doi: 10.1186/s13643-015-0161-9.
- Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Brit Med J. 2021;372:71–71.
- Moher D, Pham B, Lawson ML, et al. The inclusion of reports of randomised trials published in languages other than English in systematic reviews. Health Technol Assess. 2003;7(41):1–90. doi: 10.3310/hta7410.
- Morrison A, Polisena J, Husereau D, et al. The effect of English-language restriction on systematic review-based meta-analyses: a systematic review of empirical studies. Int J Technol Assess Health Care. 2012;28(2):138–144. doi: 10.1017/S0266462312000086.
- Schuch CM, Pritham CH. International Standards Organization terminology: application to prosthetics and orthotics. J Prosthet Orthot. 1994;6(1):29–33.
- Cochrane Consumers and Communication Review Group C. Data extraction template; 2013. Available from: http://cccrg.cochrane.org/author-resources
- Law M, Stewart D, Pollock N, et al. Guidelines for critical review form – quantitative studies; 1998. Available from: https://canchild.ca/system/tenon/assets/attachments/000/000/366/original/quantguide.pdf
- Law MC, MacDermid J. Evidence-based rehabilitation: a guide to practice. 3rd ed. Thorofare (NJ): Slack Incorporated; 2014.
- Stern P. A holistic approach to teaching evidence-based practice. Am J Occup Ther. 2005;59(2):157–164. doi: 10.5014/ajot.59.2.157.
- Thomas BH, Ciliska D, Dobbins M, et al. A process for systematically reviewing the literature: providing the research evidence for public health nursing interventions. Worldviews Evid Based Nurs. 2004;1(3):176–184.
- Higgins JPT, Thomas J, Chandler J, et al. Cochrane handbook for systematic reviews of interventions. Newark (UK): John Wiley & Sons, Incorporated; 2019.
- Mittlböck M, Heinzl H. A simulation study comparing properties of heterogeneity measures in meta-analyses. Stat Med. 2006;25(24):4321–4333. doi: 10.1002/sim.2692.
- Soo BP, Rajbhandari S, Egun A, et al. Survival at 10 years following lower extremity amputations in patients with diabetic foot disease. Endocrine. 2020;69(1):100–106. doi: 10.1007/s12020-020-02292-7.
- Chiang N, Wang J, Marie N, et al. Evaluation of clinical outcomes following minor amputations in Australia – an important consideration for timing of revascularisation. Ann Vasc Surg. 2021;76:389–398. doi: 10.1016/j.avsg.2021.03.050.
- Lepow BD, Zulbaran-Rojas A, Park C, et al. Guillotine transmetatarsal amputations with staged closure promote early ambulation and limb salvage in patients with advanced chronic limb-threatening ischemia. J Endovasc Ther. 2022. doi: 10.1177/15266028221144587.
- Varghese JJ, Estes BA, Martinsen BJ, et al. Predictors of long-term mortality in patients undergoing major or minor lower-extremity amputations. J Crit Limb Ischem. 2021;1(3):110–117.
- Vassallo IM, Gatt A, Cassar K, et al. Healing and mortality rates following toe amputation in type 2 diabetes mellitus. Exp Clin Endocrinol Diabetes. 2021;129(6):438–442. doi: 10.1055/a-0942-1789.
- Chu YJ, Li XW, Wang PH, et al. Clinical outcomes of toe amputation in patients with type 2 diabetes in Tianjin, China. Int Wound J. 2016;13(2):175–181.
- Zhang S, Wang S, Xu L, et al. Clinical outcomes of transmetatarsal amputation in patients with diabetic foot ulcers treated without revascularization. Diabetes Ther. 2019;10(4):1465–1472. doi: 10.1007/s13300-019-0653-z.
- Wilbek TE, Jansen RB, Jørgensen B, et al. The diabetic foot in a multidisciplinary team setting. Number of amputations below ankle level and mortality. Exp Clin Endocrinol Diabetes. 2016;124(9):535–540. doi: 10.1055/s-0042-109260.
- Birmpili P, Li Q, Johal AS, et al. Outcomes after minor lower limb amputation for peripheral arterial disease and diabetes: population-based cohort study. Br J Surg. 2023;110(8):958–965. doi: 10.1093/bjs/znad134.
- López-Valverde ME, Aragón-Sánchez J, López-de-Andrés A, et al. Perioperative and long-term all-cause mortality in patients with diabetes who underwent a lower extremity amputation. Diabetes Res Clin Pract. 2018;141:175–180.
- Blanchette V, Houde L, Armstrong DG, et al. Outcomes of hallux amputation versus partial first ray resection in people with non-healing diabetic foot ulcers: a pragmatic observational cohort study. Int J Low Extrem Wounds. 2022. doi: 10.1177/15347346221122859.
- Cascini S, Agabiti N, Davoli M, et al. Survival and factors predicting mortality after major and minor lower-extremity amputations among patients with diabetes: a population-based study using health information systems. BMJ Open Diabetes Res Care. 2020;8(1):7.
- Chung PM, Chau BKH, Chow ECS, et al. Factors that affect the one-year mortality rate after lower limb amputation in the Hong Kong Chinese population. J Orthop Trauma Rehabil. 2021;28. doi: 10.1177/22104917211056949.
- Norvell DC, Thompson ML, Boyko EJ, et al. Mortality prediction following non-traumatic amputation of the lower extremity. Br J Surg. 2019;106(7):879–888. doi: 10.1002/bjs.11124.
- Quigley M, Morton JI, Lazzarini PA, et al. Trends in diabetes-related foot disease hospitalizations and amputations in Australia, 2010 to 2019. Diabetes Res Clin Pract. 2022;194:110189.
- Norvell DC, Czerniecki JM. Risks and risk factors for ipsilateral re-amputation in the first year following first major unilateral dysvascular amputation. Eur J Vasc Endovasc Surg. 2020;60(4):614–621. doi: 10.1016/j.ejvs.2020.06.026.
- Yammine K, Hayek F, Assi C. A meta-analysis of mortality after minor amputation among patients with diabetes and/or peripheral vascular disease. J Vasc Surg. 2020;72(6):2197–2207.
- Dillon MP, Fatone S, Quigley M. A decision aid for people facing partial foot amputation due to peripheral arterial disease; 2023 [cited 2023 Oct 12]. Available from: http://amputationdecisionaid.com2017
- Taylor Aiken G, Button C. Over researched places: towards a critical and reflexive approach. Abingdon (UK), New York (NY): Routledge; 2022.