Abstract
Purpose
To identify research priorities related to COVID rehabilitation from the perspectives of persons with lived experiences, clinicians, researchers, community organization and policy representatives.
Materials & Methods
We conducted five international consultations to identify key issues and research priorities in COVID rehabilitation using (i) web-based questionnaires, (ii) synchronous discussions, and (iii) content analysis of COVID rehabilitation research conference presentations. We collated responses and notes and then analyzed data using content analytical techniques.
Results
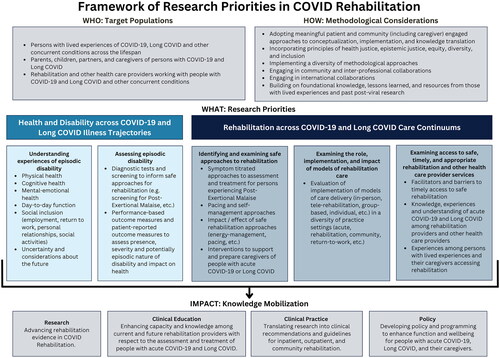
The Framework of Research Priorities in COVID Rehabilitation includes five priorities that span health and disability across COVID-19 and Long COVID illness trajectories: (1) understanding experiences of episodic disability; (2) assessing episodic disability; (3) identifying and examining safe approaches to rehabilitation; (4) examining the role, implementation, and impact of models of rehabilitation care; and (5) examining access to safe, timely and appropriate rehabilitation and other health care provider services. The Framework identifies target populations, methodological considerations, and highlights the importance of integrated knowledge translation and exchange in advancing scientific evidence, clinical education, practice, and COVID rehabilitation policy.
Conclusions
This Framework provides a foundation to advance COVID, disability and rehabilitation research to advance the health and well-being of persons with COVID-19, Long COVID, and their caregivers.
Persons with COVID-19 or Long COVID and their caregivers may experience multi-dimensional forms of disability spanning physical, cognitive, emotional health challenges, difficulties with daily function, and social inclusion, which individually and/or collectively may be unpredictable, episodic and/or chronic in nature.
Rehabilitation has a role in preventing or mitigating disability and enhancing health outcomes for persons with COVID-19, Long COVID and their caregivers.
The Framework of Research Priorities COVID Rehabilitation includes five overlapping research priorities spanning health and disability across COVID trajectories: (1) understanding experiences of episodic disability; (2) assessing episodic disability; (3) identifying and examining safe approaches to rehabilitation; (4) examining the role, implementation, and impact of models of rehabilitation care; and (5) examining access to safe, timely and appropriate rehabilitation and other health care provider services.
The research priorities in the Framework represent a comprehensive approach to examine disability and rehabilitation across COVID illness trajectories and the broad continuums of rehabilitation care to provide a coordinated and collaborative approach to advancing evidence in COVID disability and rehabilitation.
This Framework provides a foundation for international and interdisciplinary collaborations, to advance COVID disability and rehabilitation research to enhance health outcomes of persons with COVID-19, Long COVID, and their caregivers.
Implications for rehabilitation
Introduction
Globally, an estimated 770 million individuals have experienced acute COVID-19 [Citation1]. In Canada, there have been over 4.6 million confirmed cases of COVID-19 and over 54,498 deaths as of October 24, 2023 [Citation2]. In Canada, the average cost per COVID-19 hospital admission was $24,000 CAD, approximately 3 times greater than the cost of an average hospital admission [Citation3]. Approximately 17-30% of people with a confirmed diagnosis of COVID-19 experience long-term symptoms with the most common fatigue, post-exertional malaise (PEM), respiratory issues, cognitive dysfunction, and general weakness [Citation4,Citation5]. The terms Long COVID or Post-COVID Condition (PCC) or Post-acute sequelae of SARS-CoV2 (PASC) have been used to describe when these symptoms are experienced for a persistent and prolonged period, 12 weeks after the acute infectious period and lasting for at least two months [Citation6,Citation7].
An estimated 144 million individuals are living with Long COVID globally [Citation8–11]. A systematic review involving 50 studies indicated a pooled prevalence of 43% of persons living with Long COVID globally, with 53% among hospitalized, and 34% among non-hospitalized patients [Citation12]. Systematic review evidence examining symptoms among individuals after COVID-19 reported that 38-72% lived with ≥1 symptom for at least two months from COVID-19 onset and up to 54% lived with persistent symptoms for six or more months [Citation13–17]. Among the estimated 1.9 million (2.9%) people living with Long COVID in the UK, 79% reported their symptoms negatively impacted their daily activities [Citation11]. Weakness or tiredness was the most commonly reported symptom (60%), followed by shortness of breath (48%), muscle ache (42%), difficulty concentrating (37%), and joint pain (34%) [Citation18]. Post-exertional malaise (PEM) or post-exertional symptom exacerbation (PESE), defined as the worsening or relapse of symptoms following exertion, such as physical or cognitive activity [Citation18–21] is a hallmark symptom of myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). PEM is also experienced by persons living with Long COVID [Citation20–24], whereby an estimated half of persons with Long COVID fulfill ME/CFS criteria [Citation22] further highlighting the health challenges experienced among the population.
Collectively, the health-related consequences of COVID-19 and Long COVID may be referred to as “disability”, broadly defined as any physical, cognitive, mental and emotional health challenges, activity limitations, uncertainty about the future, and challenges to social participation [Citation23]. Disability among persons with COVID-19 and Long COVID can be experienced as dynamic and episodic in nature, characterized by relapsing or remitting fluctuations in the presence and severity of health-related challenges over time [Citation24–27]. The multi-dimensional and potentially episodic nature of disability experienced by people living with COVID-19 and Long COVID, can adversely impact daily function, return to employment, family life, relationships, and ability to care for others [Citation20,Citation28–30]. Caregivers are essential to the health and wellbeing of persons living with COVID-19 and Long COVID [Citation31–33]. The context of the COVID-19 pandemic, including public health measures, decreased support from formal care providers, and the possibility of contracting COVID-19, further increased demands on caregivers of persons living with COVID-19 and Long COVID [Citation31–33].
Rehabilitation, broadly defined as interventions targeted to address impairments or contextual factors to improve functional capacity [Citation34], has a role in preventing and addressing disability, and enhancing and maintaining health outcomes across the continuum of care (e.g., hospitals, rehabilitation centres, and community clinics) among persons with COVID-19, Long COVID and their caregivers [Citation33,Citation35,Citation36]. Evidence including guidelines on COVID-19 and Long COVID rehabilitation is emerging at a rapid rate [Citation37–39]. The response among people with Long COVID and other post-infectious illnesses to the COVID-19 pandemic has been instrumental in setting and building on foundational research in areas of other post-infectious conditions, to inform education and increase the safety of COVID rehabilitation [Citation40]. However, further research is required to enhance understanding of safe rehabilitation of post-infectious and complex chronic conditions, such as Long COVID, and knowledge translation should be targeted to increase the capacity of rehabilitation professionals (including physiotherapists, occupational therapists, and speech-language pathologists) to deliver care to this population [Citation41]. Developing a robust community-engaged research agenda involving disability and rehabilitation is essential to inform a coordinated response and evidence to support; appropriate, safe, timely and effective rehabilitation strategies, interventions and interprofessional models of care in the context of COVID rehabilitation.
The Rehabilitation Science Research Network for COVID (the Network) was established in the Temerty Faculty of Medicine at the University of Toronto in 2022 to advance evidence in the field of rehabilitation to optimize assessments, interventions and models of care delivery to prevent or mitigate disability and optimize health and well-being among persons with COVID-19, Long COVID, and their caregivers [Citation42]. The Network is guided by an international Advisory Committee (AC), comprised of ∼25 persons with lived experiences, clinicians, researchers, trainees, and policy representatives across the rehabilitation continuum of care [Citation43]. The AC guides the strategic directions of the Network, which are to establish partnerships and collaborations while identifying emerging issues and priorities to advance evidence in the field. Hence, we aimed to identify research priorities in COVID rehabilitation from the perspectives of people with lived experiences, their caregivers, clinicians, researchers, representatives from community organizations and policy representatives.
Materials and Methods
The Network conducted a series of key informant consultations with people with lived experiences, researchers, clinicians, and representatives from community organizations with an interest in COVID and Long COVID rehabilitation. Our approach was informed by past experiences identifying research priorities in rehabilitation among persons living with chronic and episodic conditions [Citation44,Citation45]. We conducted five distinct consultations from June 2022 to April 2023 with the following key informants: (1) AC Members of the Network; (2) Attendees at a symposium focused on COVID rehabilitation research collaboration at the 2022 American Congress of Rehabilitation Medicine (ACRM) conference in Chicago, Illinois; (3) Attendees at a presentation on the Network at the Rehabilitation Sciences Institute Leadership Rehab Rounds, University of Toronto; (4) Members of the Network; and (5) Registrants of the International Forum on COVID Rehabilitation Research. We asked about demographic and personal characteristics using a self-administered, web-based questionnaire with members of the Rehabilitation Science Research Network for COVID and registrants of the International Forum (Supplementary file 1).
We used a combination of data collection methods and sources to gather perspectives on research priorities that included: web-based questionnaires asking key informants new and emerging issues and research priorities in COVID, Long COVID, disability and rehabilitation; large group facilitated discussion, and an environmental scan of research presented on COVID and rehabilitation at the ACRM [Citation46]. Specifically, in the web-based questionnaires, we asked the following two questions: “In your opinion, what are 2 new and emerging issues in the field of acute COVID or Long COVID, disability and rehabilitation?”; and 2) “In your opinion, what are 2–3 key research priorities in the area of acute COVID or Long COVID, disability and rehabilitation that are essential for moving the field forward?” In the large group facilitated discussions, we dedicated time across consultations to interactive discussions regarding research priorities in the field of COVID rehabilitation. In the environmental scan, we documented research priorities articulated and addressed by the poster and oral presentations and took detailed notes at the oral presentations at the ACRM conference. See for a detailed description of the characteristics of each consultation, key informant group, and data sources.
Table 1. Key informant consultations & data sources to establish research priorities in COVID rehabilitation.
We reviewed the need for ethics approval with the University of Toronto Health Services Research Ethics Board, who confirmed that given the consultative process involving the membership intake survey, meetings, and Forum, this consultation did not require ethics approval.
Data analysis
Three team members (KKO, KMD, JC) reviewed the responses and discussion notes collated from the data sources from the above consultations. We analyzed the data using content analytical techniques [Citation47]. We developed a list of priority areas for COVID rehabilitation research organized into the Framework of Research Priorities in COVID Rehabilitation. The core analytical team (KKO, JC, KMD) met four times to discuss the content analysis findings and refine the Framework. We presented a preliminary draft of the Framework to the AC of the Rehabilitation Science Research Network for COVID along with the original data sources across the five consultations in April 2023 for review. We then refined the Framework to establish the current Framework of research priorities.
Results
Summary of consultations
We conducted five consultations on COVID rehabilitation research priorities with approximately 450 key informants with an interest in COVID rehabilitation research in 22 countries, spanning seven continents.
Rehabilitation Science Research Network for COVID Advisory Committee
Seventeen AC members completed a web-based survey questionnaire about new and emerging issues and research priorities in advance of the first AC meeting (October 2022). Fifteen AC members also attended the AC meeting, including persons with lived experiences with Long COVID and their caregivers (33%; n = 5), members from Temerty Faculty of Medicine including the Rehabilitation Sciences Sector and Rehabilitation Sciences Institute (33%; n = 5), clinicians and researchers with expertise in COVID rehabilitation (27%; n = 4), and one representative from a community health service organization (7%; n = 1). Most AC members who attended the meeting were from Canada (86%; n = 13).
American Congress of Rehabilitation Medicine (ACRM) conference symposium attendees
Thirteen key informants attended the ACRM symposium from Canada, Germany, the United Kingdom, and the United States. Attendees included people with Long COVID, rehabilitation clinicians (physiotherapists, speech-language pathologists), other healthcare providers (physiatrists, neuropsychologists), researchers, and trainees interested in COVID rehabilitation. Of the 30 posters and 30 oral presentations reviewed in the COVID-19 track of the conference, 25 (83%) posters and 17 (57%) oral presentations considered most relevant to the Network scope of COVID rehabilitation were included in the environmental scan.
Leadership rehab rounds, rehabilitation sciences sector, University of Toronto attendees
Seventy individuals attended the Leadership Rehab Rounds including faculty, staff, and trainees in the Rehabilitation Sciences Sector at the University of Toronto; clinicians, trainees, and researchers from affiliated clinical sites; and people living with Long COVID.
Rehabilitation Science Research Network for COVID membership
As of April 30, 2023, there were 60 responses to the Network’s membership intake survey. Of the 60 members, 9 (15%) had lived experiences with Long COVID, 12 (20%) had lived experiences with acute COVID-19, and 17 (28%) had lived experiences as a caregiver for someone with acute COVID-19 and/or Long COVID. See for characteristics of the members of the Network.
Table 2. Characteristics of members of the rehabilitation science research network for COVID and registrants for the International forum on COVID rehabilitation research.
International Forum on COVID Rehabilitation Research registrants & attendees
There were 297 registrants for the International Forum on COVID Rehabilitation Research. Of the 297 registrants, 291 (98%) responded to questions about their lived experiences with acute COVID, Long COVID, and as a caregiver to people with acute COVID and/or Long COVID. There were 59 (20%) registrants with lived experiences of Long COVID, 41 (14%) with lived experiences with acute COVID, and 32 (11%) with lived experiences as a caregiver for someone with acute COVID and/or Long COVID. See for characteristics of Forum registrants. A total of 160 people attended the Forum (125 online; 35 in-person) from 16 countries, spanning 5 continents.
Framework of Research Priorities in COVID rehabilitation
Synthesis across all data sources provided insight into the “who” (target populations), the “how” (methodological considerations), the “what” (research priorities), and the “impact” (knowledge mobilization) of COVID rehabilitation research. We collated this information to develop the Framework of Research Priorities in COVID Rehabilitation, which includes five research priorities that span health and disability across COVID illness trajectories from acute COVID-19 to Long COVID; and the rehabilitation care continuum from acute to community care. Research priorities (the “what”) include: (1) understanding experiences of episodic disability; (2) assessing episodic disability; (3) identifying and evaluating safe approaches to rehabilitation; (4) examining the role, implementation, and impact of models of rehabilitation care; and (5) examining access to safe, timely and appropriate rehabilitation and other health care provider services. The Framework identifies target populations of interest (the “who”), methodological considerations to address the priorities (the “how”), and the importance of knowledge mobilization (the “impact”) in advancing scientific evidence, clinical education and practice, and COVID rehabilitation policy (). See Supplementary file 2 for the full dataset of sources across the consultations.
In the Framework, the priorities in COVID-19 and Long COVID Rehabilitation are clustered and overlap within and between the two broader priority content areas: (a) health and disability across illness trajectories; and (b) rehabilitation across care continuums. Specific to these conditions, illness trajectories may span from initial COVID infection onward, with Long COVID included at the other end of one illness trajectory. Applicable care continuums encompass points of care that individuals with COVID-19 or Long COVID may access for rehabilitation services, such as primary care, hospitals, rehabilitation hospitals, virtual rehabilitation programs, or community clinics. Additionally, the Framework includes target populations (persons with lived experiences of acute COVID-19, Long COVID and other concurrent conditions across the lifespan; parents, children, partners, and caregivers; rehabilitation and other health providers), and methodological considerations (community-engaged, interdisciplinary, and diversity of approaches while incorporating principles of health justice) for addressing the research priorities. The Framework highlights the importance of knowledge mobilization to transfer and exchange research evidence into future practice, programs, education and policy (). The Framework is intended to serve as a knowledge mobilization tool that may be used by researchers, clinicians, trainees, and members of the community to inform future COVID rehabilitation research.
We discuss the five research priorities followed by the target population, methodological considerations and knowledge mobilization components of the framework.
What: Research priorities
Health and disability across COVID-19 and Long COVID illness trajectories
We identified two specific research priorities: (1) understanding experiences of episodic disability; and (2) assessing episodic disability. Understanding experiences of episodic disability may include exploring the physical, cognitive, and mental-emotional health, day-to-day function, social inclusion (including employment, return to work, personal relationships, and social and recreational activities), and uncertainty experienced by individuals living with COVID-19 and Long COVID and/or their parents, children, partners, and caregivers. Assessing episodic disability may include developing and evaluating diagnostic tests and screening tools to inform safe approaches to rehabilitation (e.g., screening for PESE). It may also include developing and evaluating safe performance-based and patient-reported outcome measures to assess the potentially episodic nature of disability experienced by people with COVID and Long COVID.
Rehabilitation across COVID-19 and Long COVID care continuums
We determined three specific research priorities: (1) identifying and examining safe approaches to rehabilitation; (2) examining the role, implementation, and impact of models of rehabilitation care; and (3) examining access to safe, timely and appropriate rehabilitation and other health care provider services. Key informants identified the importance of developing, implementing, and evaluating safe approaches to rehabilitation for people with COVID-19, Long COVID, and their parents, partners, and caregivers. Examples of safe approaches to rehabilitation identified by key informants as requiring further research included: symptom titrated approaches to assessment and treatment for persons experiencing PEM/PESE; pacing and self-management approaches; and interventions to support and prepare parents, children, partners, and caregivers of persons with COVID-19 or Long COVID. These interventions may include education involving instruction, interventions or programs involving strategies for balancing activity and rest, specifically modifying physical and cognitive activities to prevent PEM/PESE. Key informants also expressed that it was important to develop, implement and evaluate a range of models of rehabilitation care for COVID and Long COVID (in-person, online, individual, and group-based). They stated that health and disability outcomes should be examined when evaluating models of rehabilitation care in acute, rehabilitation, and community settings. Key informants also identified the importance of examining barriers and facilitators to timely access to safe rehabilitation, such as funding, health human resources, and consideration of referral pathways. This priority may also include exploring the knowledge, experiences and understanding of COVID and Long COVID among rehabilitation providers and other healthcare providers, in order to develop and optimize safe approaches and interventions.
Who: Target populations
The Framework includes three target populations to consider in COVID rehabilitation research: (1) persons with lived experiences of COVID-19, Long COVID and other concurrent conditions across the lifespan; (2) parents, children, partners, and caregivers of people with COVID-19 or Long COVID; and (3) rehabilitation and other health care providers working with these populations.
Key informants emphasized that COVID rehabilitation research should include persons of all ages across the lifespan living with COVID-19 and Long COVID. Many identified a paucity of COVID rehabilitation research specific to pediatric and older populations at this time. Additionally, they emphasized the importance of considering concurrent conditions (e.g., ME/CFS, Postural Orthostatic Tachycardia Syndrome (POTS), dementia, pre-existing disabilities) related to COVID rehabilitation research.
See for examples of research questions that illustrate how each of the two priority content areas of research may apply to each target population.
Table 3. Examples of research questions by priority area of research and target population within the Framework of research priorities in COVID rehabilitation.
How: Methodological considerations
Key informants recommended adopting meaningful patient- and community-engaged approaches (including caregivers) at all stages of research, across conceptualization, implementation, and knowledge translation. Collaborative engagement is essential to enhance the relevance and timeliness of research questions to the community. Patient- and community-engaged research can help to raise public awareness about the roles of safe rehabilitation in managing COVID-19 and Long COVID and to promote the integration of rehabilitation into practice.
Key informants also recommended incorporating health justice, epistemic justice, equity, diversity, and inclusion principles into COVID rehabilitation research as social determinants of health, ableism, racism, sexism, transphobia, and other systemic forms of oppression have resulted in inequitable access to care and the exclusion of more marginalized groups and people with lower socioeconomic status from research among individuals with COVID-19, Long COVID, and their parents, children, partners, or caregivers [Citation48].
Key informants recommended that COVID rehabilitation research include diverse methodological approaches (quantitative, qualitative, mixed-methods, co-design) as they may apply to a given research question. Efforts should be made to engage community and inter-professional collaborations; to help capture diverse and unique perspectives and expertise in COVID rehabilitation research. Researchers should consider international research collaborations involving countries where people living with COVID and Long COVID may share similar experiences related to disability and rehabilitation. Finally, COVID rehabilitation research should build on foundational knowledge, lessons learned, and resources from those with lived experiences and past post-infectious research.
Impact: Knowledge mobilization
As knowledge transfer and exchange is a key strategic direction of the Rehabilitation Science Research Network for COVID, key informants highlighted the need for COVID rehabilitation research to emphasize the needs of the community and clinical practice and ensure that research evidence is translated to appropriate clinicians, health providers, educators, and health authorities to advance education, programs, and policy. Knowledge transfer and exchange should be targeted to key populations that include (but are not limited to) people with lived experiences, clinicians, healthcare professional educators, health authorities and ministries, insurers and workers’ compensation boards.
Discussion
The aim of this work was to outline the key research priorities for rehabilitation in the context of COVID-19 and Long COVID. The Framework of Research Priorities in COVID Rehabilitation reflects the perspectives of an international group of persons with lived experiences, researchers, clinicians, representatives from community-based organizations, funders and policy representatives with an interest in COVID and rehabilitation across five consultations. This framework includes focal research areas, targeted research populations, methodological considerations to enhance research, and specific knowledge translation and exchange priorities including clinical education, clinical practice, policy, and future research.
The research priorities in the Framework outline the need for a comprehensive approach to address disability and rehabilitation across COVID illness trajectories and the broad continuums of rehabilitation care. Since the priorities are overlapping constructs, they are not mutually exclusive and should not be addressed in isolation. Rather, the priorities are meant to provide a coordinated and collaborative approach to advancing evidence in the field of COVID-19 and Long COVID disability and rehabilitation. The Framework aligns with the Canadian Task Force for Post-COVID Condition recommendations (March 2023) that outline the importance of standardizing assessments, providing timely and equitable access to person-centered care, and advancing research priority areas in the development of treatment approaches to maximize function and participation of persons living with Long COVID [Citation49]. Furthermore, some of these research priorities align with priorities established in post-infectious conditions (ME/CFS) [Citation50], and other chronic and episodic conditions [Citation44,Citation45,Citation51]. However, the priorities in this Framework are distinct from other research priorities, given they specifically consider priorities for COVID-19 and Long COVID rehabilitation.
Rehabilitation should be safe, disability-focused, goal-oriented, person-centered, focused on function, and tailored to an individual’s goals, abilities, and interests [Citation41]. Rehabilitation is not limited to cardiorespiratory approaches, exercise or physical activity. Exercise can be harmful to persons with PEM or PESE; specifically, graded exercise therapy is not a safe rehabilitation intervention to treat fatigue among people experiencing PEM or PESE [Citation52–54]. Rehabilitation should be person-centered and may include strategies such as self-management, pacing, and accommodation to support return to work [Citation41,Citation55–57]. Rehabilitation should consider pre-existing health conditions that persons may be living with prior to COVID-19 or Long COVID, such as cardiovascular disease, cancer, diabetes, and chronic pain to ensure meaningful and relevant goal setting and approaches to care [Citation58,Citation59]. There is a need to consider a coordinated research response in rehabilitation, between people with lived experiences, clinicians, and researchers, to address disability, optimize safe and effective rehabilitation approaches to care and treatment, and highlight best practices in the field. Opportunities exist to build on successful disability and rehabilitation models from other chronic and episodic illnesses, in the context of COVID rehabilitation research [Citation26,Citation60]. Access to timely, safe, effective, and accessible rehabilitation is a critical area in need of development and highlights the opportunities and importance of partnering with other chronic conditions to foster a “strength in numbers approach” with other chronic and episodic illnesses to advance policy and programming related to COVID rehabilitation such as ME/CFS [Citation61,Citation62].
The Framework of Research Priorities on COVID Rehabilitation is intended to be used as a knowledge mobilization tool and may be used by researchers, clinicians, trainees, and members of the community to inform future COVID rehabilitation research. This Framework can also be used to help individuals prioritize clinical and research efforts or to help guide decisions on funding research in the field.
Community and patient-led and engaged approaches to COVID rehabilitation research are essential to foster timely, meaningful and relevant approaches to rehabilitation research and its application of research evidence about appropriate service planning and delivery. Patient engagement should involve the integration of patient or community partners at all phases of the research process, including conceptualization, implementation, knowledge translation, and shared decision-making between community and research partners. The Patient-Led Research Collaborative (PLRC) score cards provide a foundation for the community and researchers to collaboratively work together to address the priorities and guide the process of a patient group and research partner collaborations [Citation63]. Fostering engagement and connecting clinicians and community members with researchers is critical for moving the field forward. International partnerships and collaborations fostered in other health conditions provide a strong foundation from which to establish a coordinated, relevant and meaningful approach for advancing rehabilitation for people living with COVID and Long COVID. Experiences with COVID and Long COVID, access to services, and experiences with rehabilitation vary across regions (countries, urban vs. rural or remote), sex, gender, and race [Citation64–67]. Therefore, it is important for research across all priority areas to incorporate principles of equity, diversity, inclusion, accessibility, and health justice. Forming partnerships and exchanging knowledge with other informants where individuals experience similar challenges related to COVID disability and rehabilitation is essential to address research priorities in this emerging field.
Our consultations, including persons with lived experiences, researchers, clinicians, trainees and community organization representatives, were a strength in developing the Framework. The Framework was co-constructed with the Advisory Committee and builds on a conceptual framework of episodic disability that considers the multi-dimensional nature of health-related challenges experienced among persons with Long COVID [Citation27]. We embedded this consultation within existing meetings, membership surveys, and knowledge translation events to broaden the international scope of the consultation. Nevertheless, we did not use a formal Delphi or nominal group technique to identify the priorities, nor did we capture the characteristics of key informants in detail across the consultation sessions. Demographic characteristics were limited to Forum registrants and Network members as as we did not formally survey the characteristics of attendees at the conference or rounds presentations. While our consultation was international in scope, our sources were limited primarily to perspectives within high-income countries, which limits the transferability of the priorities to low and middle-income countries. The disparities of Long COVID across different sex, racial, and ethnic groups [Citation68], as well as differences in Long COVID awareness and research within low-income settings [Citation69,Citation70], highlight the need to consider the applicability of the Framework in broader socio-demographic contexts. Although these priorities are meant to be aligned with a rehabilitation lens, addressing them will require collaborative and interprofessional community-engaged approaches involving COVID-19, Long COVID, primary care, and other teams of healthcare providers in collaboration with rehabilitation. Key informants involved in the consultation are involved in numerous research and community-led initiatives to address the impact of living with COVID-19 and Long COVID. Finally, we acknowledge that the field is continually evolving, and new priorities will emerge as more evidence in COVID-19 and Long COVID evolves; hence, this is a living Framework whereby research priorities will continue to evolve with new and emerging priorities as identified by the community.
Conclusion
This Framework of Research Priorities in COVID Rehabilitation provides a foundation for international and multidisciplinary collaborations to advance COVID-19 and Long COVID disability and rehabilitation research to promote the health and well-being of persons with COVID-19, Long COVID, and their caregivers. The Framework may be used by researchers, clinicians, trainees, and members of the community to inform future COVID rehabilitation research.
Supplemental Material
Download Zip (435.4 KB)Acknowledgments
We thank the following for their contributions to this manuscript [*indicates Advisory Committee Member of the Rehabilitation Science Research Network for COVID]: *Darren A. Brown (Chelsea and Westminster NHS Foundation Trust), Simon Décary (University of Sherbrooke), *Jessica DeMars (Breathewell Physio), *Mary Forhan (Department of Occupational Science and Occupational Therapy, University of Toronto), *Patricia Houston (Temerty Faculty of Medicine, University of Toronto), Fiona Jones (Population Health Research Institute, St. George’s University of London), *Pascal van Lieshout (Department of Speech-Language Pathology, University of Toronto), *Nisa Malli (Patient-Led Research Collaborative), *Rosemary Martino (Department of Speech-Language Pathology, University of Toronto), Alyssa Minor (Long COVID Physio), *Elizabeth Racz (Realize), and additional members of the Advisory Committee of the Rehabilitation Science Research Network for COVID. We thank the individuals who were involved in identifying the research priorities in COVID rehabilitation. We thank members of the Rehabilitation Science Research Network for COVID Advisory Committee for the refinement of the Framework. We thank Laura Bassi, Fisiocamera for their role in the refinement of the Framework figure.
Disclosure statement
The authors report there are no competing interests to declare.
Data availability statement
All data sources supporting the results presented in the paper are in Supplementary file 2.
Additional information
Funding
References
- World Health Organization. WHO Coronovirus (COVID-19) Dashboard: World Health Organization. 2023; [cited 2023 August 21]. Available from: https://covid19.who.int/.
- Government of Canada. COVID-19 epidemiology update: summary. 2023. Available from: https://health-infobase.canada.ca/covid-19/#a2.
- Canadian Institute for Health Information. COVID-19 hospitalization and emergency department statistics: canadian Institute for Health Information. 2023; [cited 2023 September 7]. Available from: https://www.cihi.ca/en/covid-19-hospitalization-and-emergency-department-statistics.
- Government of Canada. COVID-19: longer-term symptoms among Canadian adults – Highlights. 2022. Available from: https://health-infobase.canada.ca/covid-19/post-covid-condition/.
- Chen C, Haupert SR, Zimmermann L, et al. Global prevalence of post-coronavirus disease 2019 (COVID-19) condition or long COVID: a meta-analysis and systematic review. J Infect Dis. 2022;226(9):1593–1607. doi: 10.1093/infdis/jiac136.
- Soriano JB, Murthy S, Marshall JC, et al. A clinical case definition of post-COVID-19 condition by a Delphi consensus. Lancet Infect Dis. 2021;22(4):e102–e107. doi: 10.1016/S1473-3099(21)00703-9.
- Chou R, Herman E, Ahmed A, et al. Long COVID definitions and models of care: a scoping review. Ann Intern Med. 2024;177(7):929–940. doi: 10.7326/M24-0677.
- Wulf Hanson S, Abbafati C, Aerts JG, et al. A global systematic analysis of the occurrence, severity, and recovery pattern of long COVID in 2020 and 2021. medRxiv. 2022. doi: 10.1101/2022.05.26.22275532.
- Statistics Canada. Long-term symptoms in Canadian adults who tested positive for COVID-19 or suspected an infection, January 2020 to August 2022. Available from: https://www150.statcan.gc.ca/n1/daily-quotidien/221017/dq221017b-eng.htm.
- Bull-Otterson L, Baca S, Saydah S, et al. Post-COVID conditions among adult COVID0-19 survivors aged 18-64 and ≥65 years – United States, March 2020-November 2021. Morbidity and Mortality Weekly Report (MMWR). 2022;71(21):713–717.
- Office for National Statistics. Prevalence of ongoing symptoms following coronavirus (COVID-19) infection in the UK. 2023; [cited30 March 2023]. Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/prevalenceofongoingsymptomsfollowingcoronaviruscovid19infectionintheuk/30march2023.
- Chen C, Haupert SR, Zimmermann L, et al. Global prevalence of post-coronovirus disease 2019 (COVID-19) condition or Long COVID: a meta-analysis and systematic review. J Infect Dis. 2022;226(9):1593–1667.
- Nasserie T, Hittle M, Goodman SN. Assessment of the Frequency and Variety of Persistent Symptoms Among Patients With COVID-19: a Systematic Review. JAMA Netw Open. 2021;4(5):e2111417. doi: 10.1001/jamanetworkopen.2021.11417.
- Domingo FR, Waddell LA, Cheung AM, et al. Prevalence of long-term effects in individuals diagnosed with COVID-19: an updated living systematic review. medRxiv. 2021. doi: 10.1101/2021.06.03.21258317.
- Michelen M, Manoharan L, Elkheir N, et al. Characterising Long COVID: a living systematic review. BMJ Glob Health. 2021;6(9):e005427. doi: 10.1136/bmjgh-2021-005427.
- Whitaker M, Elliott J, Chadeau-Hyam M, et al. Persistent COVID-19 symptoms in a community study of 606,434 people in England. Nat Commun. 2022;13:1957. doi: 10.1038/s41467-022-29521-z.
- Groff D, Sun A, Ssentongo AE, et al. Short-term and long-term rates of postacute sequelae of SARS-CoV-2 infection: a systematic review. JAMA Netw Open. 2021;4(10):e2128568. doi: 10.1001/jamanetworkopen.2021.28568.
- Office for National Statistics. Self-reported long COVID symptoms, UK. 2023; [cited 10 July 2023]. Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/selfreportedlongcovidsymptomsuk/10july2023#:∼:text=Of%20those%20respondents%20who%20self,and%20joint%20pain%20(34%25).
- Ziauddeen N, Gurdasani D, O’Hara ME, et al. Characteristics and impact of Long Covid: findings from an online survey. PLoS One. 2022;17(3):e0264331. doi: 10.1371/journal.pone.0264331.
- Davis HE, Assaf GS, McCorkell L, et al. Characterizing Long COVID in an international cohort: 7 months of symptoms and their impact. EClinicalMedicine. 2021;38:101019. doi: 10.1016/j.eclinm.2021.101019.
- Humphreys H, Kilby L, Kudiersky N, et al. Long COVID and the role of physical activity: a qualitative study. BMJ Open. 2021;11(3):e047632. doi: 10.1136/bmjopen-2020-047632.
- Grach SL, Seltzer J, Chon, TY, Ganesh R. Diagnosis and management of myalgic encephalomyelitis/chronic fatigue syndrome. Mayo Clin Proc. 2023;98(10): 1544–1551. doi: 10.1016/j.mayocp.2023.07.032.
- O’Brien KK, Bayoumi AM, Strike C, et al. Exploring disability from the perspective of adults living with HIV/AIDS: development of a conceptual framework. Health Qual Life Outcomes. 2008;6(1):76. doi: 10.1186/1477-7525-6-76.
- O’Brien KK, Brown DA, McDuff K, et al. Conceptualising the episodic nature of disability among adults living with Long COVID: a qualitative study. BMJ Glob Health. 2023;8(3):e011276. doi: 10.1136/bmjgh-2022-011276.
- Thomas C, Faghy MA, Owen R, et al. Lived experience of patients with Long COVID: a qualitative study in the UK. BMJ Open. 2023;13(4):e068481. doi: 10.1136/bmjopen-2022-068481.
- Brown DA, O’Brien KK. Conceptualising long COVID as an episodic health condition. BMJ Glob Health. 2021;6(9):e007004. doi: 10.1136/bmjgh-2021-007004.
- O’Brien KK, Brown DA, McDuff K, et al. Conceptual framework of episodic disability in the context of Long COVID: findings from a community-engaged international qualitative study. medRxiv. 2024. doi: 10.1101/2024.05.28.24308048.
- Walker S, Goodfellow H, Pookarnjanamorakot P, et al. Impact of fatigue as the primary determinant of functional limitations among patients with post-COVID-19 syndrome: a cross-sectional observational study. BMJ Open. 2023;13(6):e069217. doi: 10.1136/bmjopen-2022-069217.
- Mazer B, Feldman DE. Functional limitations in individuals with long COVID. Arch Phys Med Rehabil. 2023;104(9):1378–1384. doi: 10.1016/j.apmr.2023.03.004.
- Stelson EA, Dash D, McCorkell L, et al. Return to work with long-COVID: An episodic disability and total worker health® analysis. Soc Sci Med. 2023;338:116336. doi: 10.1016/j.socscimed.2023.116336.
- Muldrew DH, Fee A, Coates V. Impact of the COVID-19 pandemic on family carers in the community: a scoping review. Health Soc Care Community. 2022;30(4):1275–1285. doi: 10.1111/hsc.13677.
- Wasilewski MB, Szigeti Z, Sheppard CL, et al. Patients, caregivers, and healthcare providers’ experiences with COVID care and recovery across the care continuum: a qualitative study. Int J Integr Care. 2023;23(2):27. doi: 10.5334/ijic.6952.
- Wasilewski MB, Szigeti Z, Sheppard CL, et al. “You want them to be partners in therapy, but that’s tricky when they’re not there”: A qualitative study exploring caregiver involvement across the continuum of care during the early COVID pandemic. Clin Rehabil. 2023;38(1):109–118. doi: 10.1177/02692155231191011.
- Negrini S, Selb M, Kiekens C, et al. Rehabilitation definition for research purposes. A global stakeholders’ initiative by Cochrane Rehabilitation. Neurorehabil Neural Repair. 2022;36(7):405–414. doi: 10.1177/15459683221093587.
- Mills J-A, Marks E, Reynolds T, et al. Rehabilitation: essential along the continuum of care. 3rd ed. Washington (DC): The International Bank for Reconstruction and Development / The World Bank; 2017. Chapter 15, Disease control priorities: improving health and reducing poverty.
- Décary S, De Groote W, Arienti C, et al. Scoping review of rehabilitation care models for post COVID-19 condition. Bull World Health Organ. 2022;100(11):676–688. doi: 10.2471/BLT.22.288105.
- World Health Organization. Clinical management of COVID-19: living guideline. Geneva: World Health Organization; 2023. Available from: https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2023.2
- Canadian Physiotherapy Association. Rehabilitation for Clients with Post COVID-19 Condition (Long COVID) Canadian Physiotherapy Association; 2021. Available from: chrome-extension://efaidnbmnnnibpcajpcglclefindmkaj/https://physiotherapy.ca/app/uploads/2022/08/long_covid_en-final-rev2.pdf.
- Wasilewski MB, Cimino SR, Kokorelias KM, et al. Providing rehabilitation to patients recovering from COVID-19: A scoping review. Pm R. 2022;14(2):239–258. doi: 10.1002/pmrj.12669.
- Davis HE, McCorkell L, Vogel JM, et al. Long COVID: major findings, mechanisms and recommendations. Nat Rev Microbiol. 2023;21(3):133–146. doi: 10.1038/s41579-022-00846-2.
- DeMars J, Brown DA, Angelidis I, et al. What is safe long COVID rehabilitation? J Occup Rehabil. 2023;33(2):227–230. doi: 10.1007/s10926-022-10075-2.
- Rehabilitation Science Research Network for COVID. Rehabilitation Science Research Network for COVID Toronto: rehabilitation Science Research Network for COVID. 2023; [cited 2023 August 18]. Available from: https://rehabcovidnetwork.med.utoronto.ca/.
- Rehabilitation Science Research Network for COVID. Advisory Committee Members: rehabilitation Science Research Network for COVID University of Toronto: temerty Faculty of Medicine, University of Toronto. 2024; [cited 2024 June 18]. Available from: https://rehabcovidnetwork.med.utoronto.ca/advisory-committee-members.
- O’Brien KK, Ibáñez-Carrasco F, Solomon P, et al. Research priorities for rehabilitation and aging with HIV: a framework from the Canada-International HIV and Rehabilitation Research Collaborative (CIHRRC). AIDS Res Ther. 2020;17(1):21. doi: 10.1186/s12981-020-00280-5.
- O’Brien KK, Ibáñez-Carrasco F, Solomon P, et al. Advancing research and practice in HIV and rehabilitation: a framework of research priorities in HIV, disability and rehabilitation. BMC Infect Dis. 2014;14(1):724. doi: 10.1186/s12879-014-0724-8.
- Charlton P, Kean T, Liu RH, et al. Use of environmental scans in health services delivery research: a scoping review. BMJ Open. 2021;11(11):e050284. doi: 10.1136/bmjopen-2021-050284.
- Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288. doi: 10.1177/1049732305276687.
- Shroff FMC. Flames of transformation: igniting better mental and physical health for racialized and gendered North Americans. Front Glob Womens Health. 2023;4:1126934. doi: 10.3389/fgwh.2023.1126934.
- Office of the Chief Science Advisor of Canada. Post-COVID-19 Condition in Canada: what We Know, What We Don’t Know and a Framework for Action; 2022. Available from: https://science.gc.ca/site/science/sites/default/files/attachments/2023/Post-Covid-Condition_Report-2022.pdf.
- Tyson S, Stanley K, Gronlund TA, et al. Research priorities for myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS): the results of a James Lind alliance priority setting exercise. Fatigue: biomedicine, Health & Behavior. 2022;10(4):200–211. doi: 10.1080/21641846.2022.2124775.
- O’Brien KK, Brown DA, Corbett C, et al. AIDSImpact special issue – broadening the lens: recommendations from rehabilitation in chronic disease to advance healthy ageing with HIV. AIDS Care. 2020;32(Suppl 2):65–73. doi: 10.1080/09540121.2020.1739203.
- World Physiotherapy. World Physiotherapy response to COVID-19. Safe rehabilitation approaches for people living with Long COVID: physical activity and exercise; 2021. Available from: https://world.physio/sites/default/files/2021-07/Briefing-Paper-9-Long-Covid-FINAL-English-202107.pdf.
- Twomey R, DeMars J, Franklin K, et al. Chronic fatigue and postexertional malaise in people living with long COVID: an observational study. Phys Ther. 2022;102(4):pzac005. doi: 10.1093/ptj/pzac005.
- Davenport TE, Stevens SR, Stevens J, et al. Lessons from myalgic encephalomyelitis/chronic fatigue syndrome for Long COVID: postexertional symptom exacerbation is an abnormal response to exercise/activity. J Orthop Sports Phys Ther. 2022. doi: 10.2519/jospt.blog.20220202
- Ghali A, Lacombe V, Ravaiau C, et al. The relevance of pacing strategies in managing symptoms of post-COVID-19 syndrome. J Transl Med. 2023;21(1):375. doi: 10.1186/s12967-023-04229-w.
- World Health Organization. Support for rehabilitation: self-management after COVID-19-related illness. World Health Organization. Copenhagen, Denmark: Regional Office for Europe; 2021.
- Brehon K, Niemeläinen R, Hall M, et al. Return-to-work following occupational rehabilitation for long COVID: descriptive cohort study. JMIR Rehabil Assist Technol. 2022;9(3):e39883. doi: 10.2196/39883.
- Bigdelou B, Sepand MR, Najafikhoshnoo S, et al. COVID-19 and preexisting comorbidities: risks, synergies, and clinical outcomes. Front Immunol. 2022;13:890517. doi: 10.3389/fimmu.2022.890517.
- Jacobs ET, Catalfamo CJ, Colombo PM, et al. Pre-existing conditions associated with post-acute sequelae of COVID-19. J Autoimmun. 2023;135:102991. doi: 10.1016/j.jaut.2022.102991.
- Brown DA, O’Brien KK, Josh J, et al. Six lessons for COVID-19 rehabilitation from HIV rehabilitation. Phys Ther. 2020;100(11):1906–1909. doi: 10.1093/ptj/pzaa142.
- Realize Canada. Episodic Disabilities: realize Canada. 2023. Available from: https://www.realizecanada.org/our-work/episodic-disabilities/.
- Komaroff AL, Lipkin WI. ME/CFS and Long COVID share similar symptoms and biological abnormalities: road map to the literature. Front Med (Lausanne). 2023;10:1187163. doi: 10.3389/fmed.2023.1187163.
- Council of Medical Specialty Societies, Patient-Led Research Collaborative. Patient-Led Research Scorecards; 2023. Available from: https://patientresearchcovid19.com/storage/2023/02/Patient-Led-Research-Scorecards.pdf.
- Monnat SM. Rural-Urban variation in COVID-19 experiences and impacts among US working-age adults. Ann Am Acad Pol Soc Sci. 2021;698(1):111–136. doi: 10.1177/00027162211069717.
- Sanford S, Roche B. The healthcare experiences of people with Long COVID in the GTA. Toronto (OA): Wellesley Institute; 2023.
- Hale N, Meit M, Pettyjohn S, et al. The implications of long COVID for rural communities. J Rural Health. 2022;38(4):945–947. doi: 10.1111/jrh.12655.
- United Nations Department of Economic and Social Affairs. COVID-19 and indigenous peoples: united Nations, 2023. Available from: https://www.un.org/development/desa/indigenouspeoples/covid-19.html.
- Jacobs MM, Evans E, Ellis C. Racial, ethnic, and sex disparities in the incidence and cognitive symptomology of long COVID-19. J Natl Med Assoc. 2023;115(2):233–243. doi: 10.1016/j.jnma.2023.01.016.
- Ledford H. Long COVID is a double curse in low-income nations – here’s why. Nature. 2024;625(7993):20–22. doi: 10.1038/d41586-023-04088-x.
- Jassat W, Reyes LF, Munblit D, et al. Long COVID in low-income and middle-income countries: the hidden public health crisis. Lancet. 2023;402(10408):1115–1117. doi: 10.1016/S0140-6736(23)01685-9.