Abstract
Purpose
Previous studies exhibited differences in sensory processing, motor coordination, metacognitive executive functions (EF-MI), and sleep quality among adults with neurodevelopmental disorders (NDD). This study aims to find relationships between those abilities and organization-in-time, focusing on emotional responses after decreased organization abilities.
Materials and methods
This is a secondary data analysis of a larger sample from three previous studies conducted in one laboratory. Data were collected from 290 adults; 149 with NDD and 141 sex- and age- (20–50 years) matched controls completed the Adolescent/Adult Sensory Profile, Adult Developmental Coordination Disorder, Adults Behavioral Rating Inventory of Executive Functions, Mini Sleep, and Time Organization and Participation questionnaires. Structural equation model (SEM) analysed relationships and variable prediction.
Results
Significant between-group differences were found for all variables; SEM indicated similar paths in both groups. Sensory processing affected EF-MI and sleep quality and significantly correlated with motor coordination, affecting EF-MI; EF-MI affected organization-in-time. Sleep quality significantly affected organization-in-time, affecting emotional responses.
Conclusions
Sensory, motor, EF, and sleep differences were associated with decreased organization-in-time abilities of adults with NDD, adversely affecting their emotional well-being. Early detection of such differences and targeted interventions may improve daily functioning and life quality and prevent negative emotional implications.
IMPLICATIONS FOR REHABILITATION
Neurodevelopmental disorders (NDD) emerging early in development affect lifelong well-being, and personal, social, academic, and occupational function.
Adults with NDD may experience reduced quality of life due to ineffective time organization and life management.
Ineffective time organization and consequence negative emotional responses are tied with deficient sensory processing, motor coordination, metacognitive executive function abilities, and sleep quality.
Early diagnosis of such deficiencies following by targeted intervention may enhance daily functioning, reduce emotional challenges, and improve overall life outcomes.
Introduction
Neurodevelopmental disorders (NDD) are lifelong health conditions originating during early development. They are characterized by differences in personal, social, academic, or occupational functioning and encompass a broad range of neurological health conditions. Attention-deficit/hyperactivity disorder (ADHD) and specific learning disorders (SLD) are highly common NDD [Citation1]. The reported prevalence of ADHD symptoms in adulthood ranges from 2.5% to 5.0% [Citation2]. The rate of adulthood SLD is unknown but estimated at around 4% [Citation1].
These health conditions and their characteristics may lead to daily functional limitations related to long-term emotional, social, and occupational outcomes [Citation3–7]. It is assumed that adults with ADHD may experience decreased quality of life due to less effective organization of their time [Citation7,Citation8].
This study is based on the World Health Organization’s [Citation9] International Classification of Functioning Disability and Health (ICF) framework, which views NDD as health conditions. This internationally recognized, comprehensive health-related perspective enables the understanding of people’s daily organization-in-time abilities through various factors, including body functions [Citation10,Citation11]. These functions encompass sensory processing, motor coordination, executive functions (EF), and sleep functions [Citation9].
Organization-in-time
Organization-in-time ability reflects a person’s ability to organize their time relative to actual, concrete daily performance. Wennberg [Citation12] defined daily time management as the ability to perform and complete everyday activities in the correct sequence and within specific time frames and identified two related ICF activity and participation codes: managing one’s life (d2305) and adapting to time demands (d2306). The estimation of time to perform daily activities, which poses challenges for adults with SLD [Citation13], is a component of this ability [Citation14]. This article uses the closely related term, organization-in-time ability, which is also classified under activity and participation and pertains to the ICF code for managing one’s life (d2308).
Organization-in-time has crucial effects on a person’s self-directed feelings, autonomy, and life motivation [Citation14]. Effectively organizing time is essential for participation in everyday life at home, work, and academic environments and during play and leisure activities [Citation15]. Poor organization-in-time abilities, as found in adults with SLD or ADHD, can lead to disrupted work–life balance and decreased well-being and quality of life [Citation7,Citation8,Citation13,Citation16].
Emotional consequences following unsuccessful organization-in-time
One component of organization-in-time ability reflects the experience of frequent emotional responses following unsuccessful organization-in-time [Citation14]. It highlights the emotional consequences that arise from differences in daily organization-in-time and its functional implications. As a result of daily confrontations in diverse life domains, adults with SLD/ADHD may experience frustration and even reduced global and mental health if their sensory, motor, cognitive, or sleep differences are not understood or acknowledged [Citation17].
Sensory processing
As an ICF body function [Citation9], sensory processing pertains to how people receive, incorporate, and structure incoming sensory information [Citation18]. Dunn’s [Citation19] theoretical model of sensory processing explores connections between the neurological threshold and behavioural-response-regulation spectrums. It delineates four sensory-processing patterns stemming from those relationships: low registration, sensation-seeking, sensitivity to stimuli, and sensation-avoiding. Although most people with neurotypical development do not struggle with sensory-processing differences, some exhibit extreme sensory-processing patterns [Citation20].
Previous studies indicated that adults with SLD or ADHD had more sensory-processing differences in multiple life domains than adults without NDD [Citation4,Citation21]. They exhibit decreased performance, activity avoidance, and affective mental health problems, such as anxiety and depression [Citation4,Citation22–24].
Motor coordination
Coordinating voluntary movements, another ICF body function [Citation9], can manifest as motor coordination. Developmental coordination disorder (DCD) is diagnosed when acquiring and executing coordinated motor skills is significantly decreased, even considering the person’s age and opportunity for skill learning and use. Decreased motor coordination might manifest in dropping and bumping into objects or difficulty catching objects, using scissors, handwriting, riding a bike, or participating in sports [Citation1]. These symptoms affect daily functioning with changes in social behaviours, such as avoiding clubbing, dancing [Citation25], and other leisure activities. Compared to controls, adults with DCD symptoms take longer and may require more effort to complete daily tasks involving fine and gross motor skills and spatial orientation (e.g., driving), resulting in less efficient and lower quality performance. They also report negative emotional effects of these limitations [Citation26,Citation27].
Although 67% of adults with SLD were classified as having DCD symptoms based on their self-reports [Citation28], studies of motor coordination among adults with SLD/ADHD have been rare [Citation25,Citation29]. However, studies have shown that some children with SLD and ADHD demonstrate DCD symptoms [e.g., Citation30,Citation31] and estimated that such symptoms exist in 50% of children with ADHD [e.g., Citation30,Citation32].
Executive functions
Beside modulating sensory responses and efficient motor coordination, organizing time effectively requires adequate EF, such as planning, decision-making, and attention [Citation14,Citation33]. Executive functions are higher-level cognitive functions required to perform and participate effectively in complex, self-directed activities [Citation34,Citation35]. These abilities allow people to achieve short- and long-term goals, modify their thinking and actions [Citation36], and engage in successful problem-solving and planning [Citation37]. They comprise two close but separate executive abilities: metacognitive and motivational–emotional [e.g., Citation38]. Differences in EF have been reported in people with SLD [Citation7], ADHD [Citation39], and DCD [Citation40] and suggested as a common mechanism in NDD [e.g., Citation41].
Graham [Citation42] suggested that a better understanding of EF among people with NDD could lead to a better understanding of their aetiology. Despite evidence that motor and sensory-processing patterns among adults with neurotypical development [Citation20] and sensory functions among adults with SLD [Citation43] can predict EF, there is no complete picture of their relationship in adults with ADHD and SLD. Considering previous research [Citation43,Citation44], this study focuses on five domains that tap the executive regulation of cognitive problem-solving, deemed “metacognition”: initiate, working memory, plan/organize, organization of materials, and monitor [Citation45].
Sleep quality
Sleep functions also play a vital role in daily function. The ICF categorizes sleep—including its amount, onset, maintenance, and quality—as a specific mental body function [Citation9]. Poor sleep refers mainly to insomnia, the dissatisfaction with sleep quantity, or quality causing clinically significant distress or difficulty [Citation34]. Decreased sleep quality has been found among adults with SLD [Citation21] and ADHD [Citation4,Citation46]. The literature emphasizes that sleep is essential to performing daily activities and occupations [Citation32,Citation47]. A relationship between sleep quality and cognitive, emotional, and functional abilities has been reported among adults with ADHD [Citation48]. However, studies on the effects of decreased sleep on the daily functioning of adults with NDD are scarce.
Study Rationale and Aims
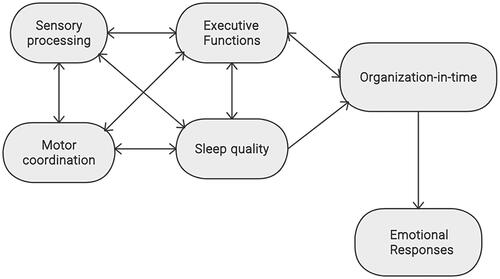
Despite the possible implications of these differences on the mental health, self-esteem, and well-being of adults with NDD, research on their daily functional characteristics has been scarce [Citation49,Citation50]. Nevertheless, it is essential to identify the relationships among these body functions, organization-in-time abilities, and subsequent emotional responses following decreased organization-in-time. This analysis will enhance the understanding of the broader implications for adults with NDD. visually represents a theoretical model of these relationships.
Figure 1. Theoretical model for the relationships between sensory processing, motor coordination, executive functions, sleep quality, and organization-in-time abilities and emotional responses.
This study is a secondary data analysis of a larger sample from three previous studies conducted in one laboratory. It aims to identify relationships among these body functions and predict the emotional consequences of disorganization-in-time among adults with SLD and ADHD due to their high incidence and frequent co-occurrence in adults with NDD [Citation49,Citation51,Citation52]. Considering the results of previous studies, we hypothesize that: (a) significant differences between a sample of adults with NDD and controls in their sensory, motor, EF, and sleep body functions, as reflected in their daily functions, will be observed; (b) a significantly higher percentage of the group with NDD will show a decrease in these body functions; and (c) sensory, motor, EF and sleep quality will predict organization-in-time abilities and the emotional consequences of disorganization.
Materials and methods
Participants
The sample comprised 290 participants: 149 in the group with NDD and 141 in the control group, matched for age and sex (self-defined gender). This sample size surpasses the theoretically required number of 256 participants, calculated using statistical parameters at a 95% probability level, 80% statistical power, 16 observed variables, 6 latent variables, and an effect size of 0.3 [Citation53].
Inclusion criteria for the entire sample were ages 20–50 years, ability to write Hebrew at a native-language level, intact or corrected vision and hearing, no physical or neurological medical observations, and generally healthy without chronic disease or significant injuries that might affect daily function. Subjects were divided into the research group (participants with NDD) and the control group (participants without NDD) based on their self-reports in the studies and on their previous professional diagnoses.
Specifically, participants in the control group self-declared that they were without ADHD or SLD diagnoses. Participants in the research group were people with SLD (with or without ADHD symptoms) or ADHD diagnoses, based on their self-reports or professional diagnoses (i.e., psychologists specializing in SLD). Participants with SLD were also diagnosed with ADHD symptoms based on the Adult ADHD Self-Report Scale (ASRS-V1.1) [Citation54]. For those diagnosed with ADHD, a formal medical diagnosis by an expert neurologist, psychiatrist, or family doctor based on the Diagnostic and Statistical Manual of Mental Disorders (5th edition) criteria [Citation34] was required. Symptoms consistent with ADHD [Citation55] were also confirmed by the ASRS v1.1 final score or medium-to-high probability of ADHD according to the Brown Attention-Deficit Disorder Scales [Citation56,Citation57]. In addition, participants with an ADHD diagnosis were asked whether they had previously been diagnosed with SLD.
Procedure
We used convenience sampling to recruit participants through social media in the three previous related studies. Researchers asked potential participants initial questions based on the inclusion criteria to confirm their eligibility for the research group or control group. Participants with NDD were asked to provide documentation to confirm their diagnoses.
The Ethics Committee for Human Subject Research at the University of Haifa approved the three related studies (confirmations No. 170/10, No. 032/17, and No. 457/18). During individual meetings with the researcher, which took place in a quiet area to ensure no interruptions, participants signed written informed consent forms and completed the sociodemographic questionnaire and other evaluations.
Measures
Time Organization and Participation Scale
The Time Organization and Participation Scale (TOPS) [Citation14] examines time organization ability while performing daily tasks. The questionnaire includes three parts comprising 35 items scored on a five-point scale; a lower score indicates a greater lack of organization-in-time. Two additional questions are for clinical use only. Part A (20 items) evaluates the performance of each daily activity at an appropriate pace, as expected by the environment. It uses a scale of 5 (always), 4 (usually), 3 (sometimes), 2 (rarely), and 1 (never). Part B (five items) examines the way of organizing the performance over the day or within a certain time on a scale of 5 (excellent) to 1 (very bad). Part C (eight items) includes a report of emotional responses following unsuccessful organization of time on a scale of 5 (never), 4 (rarely), 3 (sometimes), 2 (usually), and 1 (always).
The emotional response share a lack of motivation to perform, sadness, frustration, anger, crying, outbursts toward family members or friends, and stress [Citation14]. Thus, lower TOPS scores (cutoff scores: Part A = 3.18, Part B = 3.11, Part C = 3.16) indicate a higher probability for more limitations in time organization and participation in daily tasks. High internal consistency was reported for Parts A, B, and C (0.87 < α < 0.92), and discriminant validity was reported for differences in age groups [Citation14] and between adults with and without SLD [Citation13].
Adolescent/Adult Sensory Profile
The Adolescent/Adult Sensory Profile (AASP) is a 60-item self-reported sensory-processing questionnaire based on Dunn’s model of sensory processing. Using a five-point Likert scale from 1 (almost never) to 5 (almost always) for each item, the participant indicates how often they respond to a sensory event in the manner described. For scoring, the items are sorted into four subscales reflecting sensory-processing patterns: low registration (inability to perceive sensations and exhibiting inattentive behaviours), sensation-seeking (searching for intense sensations, e.g., strong tastes, loud sounds, and arousing visual stimuli), sensory sensitivity (inattention to sensory input, e.g., hearing or smelling), and sensation-avoiding (keeping distractions to a minimum) [Citation58]. A validation process conducted for the Hebrew version indicated good internal consistency. Psychometric properties and norms were published for adults aged 18–64 years for each subscale [Citation59].
Adult Developmental Coordination Disorder Checklist
The Adult Developmental Coordination Disorder Checklist (ADC) [Citation25] screening tool identifies youth and adults at risk for DCD. It is a 40-item, Hebrew, self-report questionnaire that examines respondents’ motor coordination abilities. The questionnaire includes three subscales that evaluate (a) difficulties the respondent experienced as a child (10 items), (b) current symptoms (10 items), and (c) current symptoms manifested by others (20 items). Each item is scored from 1 (never) to 4 (always), with higher scores indicating a higher risk for DCD. Summary scores of 80 and above indicate being at risk for DCD (probable); scores of 90 and above indicate DCD. Internal reliability levels for the whole scale (α = 0.953) and three subscales (0.873 < α < 0.914) have been established [Citation25].
Behavioral Rating Inventory of Executive functions-Adolescent/Adult version
The Behavioral Rating Inventory of Executive Functions-Adolescent/Adult version (BRIEF-A) [Citation60] is a self-report ecological validity questionnaire reflecting EF abilities through daily function. It is designated for adults aged 18–90 years [Citation61] and is appropriate for people with developmental, neurological, and psychiatric disorders [Citation43,Citation62]. Its 75 items include nine subscales divided into two index scores: a behavioural regulation index and a metacognition index. A global executive composite score is also achieved [Citation60].
In this study, we focused on the BRIEF-A metacognitive index, comprising five of the nine scales: initiate, working memory, plan/organize, task monitor, and organization of materials [Citation63]. For each metacognitive index item, participants indicate how often they behave as described on a three-point scale; higher ratings indicate more EF deficiency.
These subscales are standardized to produce t-scores according to age and sex norms. The expected normative score for the whole scale is t = 50; above 65 signifies clinical difficulty. The BRIEF-A has moderate to high internal consistency (α = 0.58–0.92), high test–retest stability (α = 0.82–0.94), and high test–retest reliability (r = 0.91–0.94) [Citation63,Citation64].
Mini Sleep Questionnaire
The Mini Sleep Questionnaire (MSQ) [Citation65] is a self-report measure examining respondents’ sleep quality and insomnia risk. Using a seven-point Likert scale, respondents indicate how often they face different sleep difficulties; a higher score indicates more severe sleep difficulties. Natale et al. [Citation66] found the questionnaire to have good internal consistency and that two factors explained about 50% of the total variance, with loading values higher than 0.50 (excluding Item 6, snoring). Fabbri et al. [Citation67] labelled the sleep (Items 1, 2, 3, 7, and 10) and wake (Items 4, 5, 8, and 9) dimensions. Sleep–wake quality is measured by the total score, with higher scores indicating more sleeping problems (10–24 points for good sleep–wake quality; 25–27 points for mild sleep–wake difficulties; 28–30 points for moderate sleep–wake difficulties; and >30 points for severe sleep–wake difficulties) [Citation65].
Data analyses
This study is a secondary data analysis of a larger sample from three previous studies that used the same inclusion and exclusion criteria and variables analysed in this study [Citation4,Citation13,Citation29,Citation43,Citation68]. Descriptive statistics were conducted using frequencies for categorical variables (e.g., sex) and means with standard deviations for continuous variables (e.g., age). We compared the groups using Chi-squared and independent t-tests and analysed the internal reliability of each test’s domain with Cronbach’s alpha. A multivariate analysis of variance (MANOVA) was conducted to examine between-group differences in the tests’ domain scores and ability percentiles. We used IBM SPSS (ver. 27) for descriptive statistics and correlations and MANOVA and AMOS software (ver. 27) to implement the structural equation model (SEM).
The SEM was implemented to strengthen the theoretical understanding of functional behaviour and provide insight into individual abilities. It divided behaviour into components and analysed them sequentially. The model was evaluated for the whole sample and then for each group. We calculated missing data values (<5%) before the SEM analysis to ensure a complete dataset. The following indices were used to evaluate the model: Chi-squared, which is acceptable when the value is not significant; the goodness of fit index (GFI); the comparative fit index (CFI); the non-normed fit index, with adequate values above 0.90 and excellent fit above 0.95; and the root mean square error of approximation (RMSEA), with adequate values less than 0.08 and excellent fit less than 0.06 [Citation69].
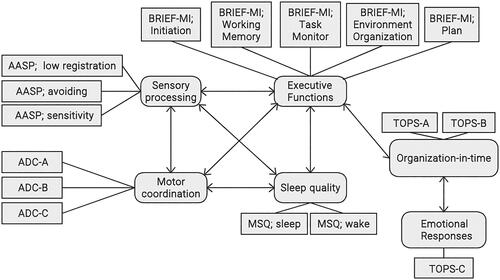
illustrates the latent variables (circles) and observed variables (squares). Due to its low degree of effect, the AASP sensation-seeking domain was excluded from the model. In addition, given the importance of the emotional responses following daily functional experiences of disorganization, we separated the TOPS Part C in the model (this part represents emotional responses tied to decreased functional behaviour). A path analysis using SEM was conducted to assess the meditation relationships between the study variables.
Figure 2. Theoretical model representing latent and observed variable.
We used the bootstrapping method to examine the models’ indirect effects. The key principle underlying the bootstrapping procedure is that it enables the researcher to simulate repeated subsamples from an original database. Thus, it allows the assessment of parameter estimate stability and reporting the values with greater accuracy [Citation70]. The significance level (p value) was 0.05.
Results
The research group included 30 (20%) adults diagnosed with only SLD, 57 (38%) adults with SLD accompanied with ADHD symptoms, and 62 (42%) adults with only ADHD. shows the demographic characteristics of the research group (n = 149) and the control group (n = 141).
Table 1. Descriptive statistics by group.
No significant group differences were found for age, sex, or number of participants working or university students. Significant group differences were found for education: more control group participants than research group participants were academics. In addition, more control group participants indicated a stable relationship with a spouse. No significant correlation was found between those demographic variables and organization-in-time, sensory, motor, EF, and sleep variables.
Decreased organization-in-time, sensory processing, motor coordination, EF, and sleep quality: between-group comparison
shows the MANOVA results for each questionnaire regarding participants’ organization-in-time abilities and body function characteristics. Except for the AASP’s sensation-seeking domain and sleep–wake quality, all variables had medium to strong effect sizes (ηp2 = 0.03–0.53).
Table 2. MANOVA for questionnaire domains.
Significant group differences were found for all organization-in-time, sensory, motor coordination, EF, and sleep quality domains except sensation-seeking. In these domains, participants with NDD demonstrated decreased performance compared to the controls. Considering those results, we examined each construct’s degree and proportion of participants with two or more sensory, motor, or EF differences. illustrates the results of each construct’s degree of differences.
Table 3. Frequencies of deficient function in organization-in-time domains, sensory processing, motor coordination, Executive functions, and sleep quality per cutoff points, norms, or mean final scores by group.
As presented in , 19% of the participants in the research group reported difficulty organizing their daily activities at an expected pace. More than 50% reported difficulty organizing their entire day, and 40% reported a high frequency of negative emotional responses. Only 2–9% of the participants in the control group reported deficient organization-in-time features in those domains (pace, whole day, and emotional responses). Except for the sensation-seeking domain, at least 45% of the research group dealt with abnormal sensory patterns (low registration, sensitivity, or avoidance) compared to around 32% of the control group. Further, 45% of the research group were at risk of DCD or probable DCD compared to 6% of the control group. More than 61% of the participants in the research group reported more EF deficiencies on the BRIEF-A metacognitive index and global executive composite compared to less than 5% of the participants in the control group, and 67% of them dealt with moderate to severe sleep deficits compared to 20% of the controls.
Table 4. Observed variable loadings with latent variables by group.
In each BRIEF-A metacognitive index domain, 2–10% of the control group had a deficiency (score > 65) in one or more domains compared to 21–76% of the research group. The higher percentage (76%) indicated decreased working memory. Related to sleep quality, whereas 20% of the control group reported moderate to severe sleep difficulties; 67% of the research group reported the same.
Further analysis of results from the research group indicated that seven (4.7%) participants dealt with both sensory processing and motor coordination decreases, 11 (7.4%) had decreased motor coordination and EF abilities, 31 (20.8%) had decreased sensory processing and EF abilities, and four (2.7%) had decreased sensory processing, motor coordination, and EF abilities. In sum, 35.6% of the participants in the group with NDD were confronted with two or more decreased sensory/motor/EF abilities.
Structural equation model
The SEM model for the sample achieved adequate fit indices, χ2(84) = 231.08, p < 0.001, CFI = 0.958, NFI = 0.936, GFI = 0.910, RMSEA = 0.078, SRMR = 0.053. Although p is significant, the value divided by the degrees of freedom (df) is smaller than 3 and, thus, adequate (χ2/df = 2.74). In addition, acceptable fit indices were found for the research group, χ2(81) = 152.50, p < 0.001, CFI = 0.943, NFI = 0.890, GFI = 0.90, RMSEA = 0.077, SRMR = 0.051, and the control group, χ2(81) = 109.9, p = 0.018, CFI = 0.970, NFI = 0.900, GFI = 0.917, RMSEA = 0.050, SRMR = 0.053, indicating that the model may be applied to either/both groups.
presents the relationships between the variables in each group. Correlation and regression coefficients levels for the group with NDD are bold above the lines; bold below the lines indicates levels for the group of controls. Double-headed (bidirectional) arrows represent correlations between variables, and single-headed (unidirectional) arrows represent regression coefficients. Correlations that were not significant are represented by a broken line. presents the observed variable loadings with latent variables, described separately for each group.
Figure 3. Structural equation model: relationships and regression coefficients between organization-in-time and emotional responses and between these variables and executive functions, sensory processing, motor coordination, and sleep quality.
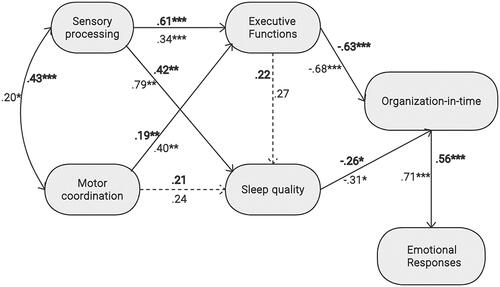
As presented in , a significant correlation was found in both groups between sensory processing and motor coordination (research group: r = 0.43, p < 0.001; control group: r = 0.20, p = 0.046). A significant difference was found between the groups in these correlations (p = 0.015), indicating stronger relations among the group with NDD.
A significant effect was found in both groups between sensory processing and EF-MI (NDD: β = 0.61, p < 0.001; control: β = 0.31, p = 0.001) and between motor coordination and EF-MI (research group: β = 0.19, p < 0.05; control group: β = 0.40, p < 0.001). Significant differences were found between the groups in both paths (sensory processing and EF-MI: p = 0.001; motor coordination and EF-MI: p = 0.026).
A nonsignificant effect was found between EF-MI and sleep quality (research group: β = 0.22, p = 0.07; control group: β = 0.27, p = 0.154), whereas significant negative effect was found between EF-MI and organization-in-time in both groups (research group: β = −0.63, p < 0.001; control group: β = −0.68, p < 0.001). This effect was similar between groups (EF-MI and sleep: p = 0.327; EF-MI and organization-in-time: p = 0.230).
Sleep quality also significantly negatively affected organization-in-time (research group: β = −0.26, p = 0.012; control group: β = −0.31, p = 0.05), with similarly between the groups (p = 0.323). Note that the negative effects were because higher scores on the MSQ indicated poor sleep quality, whereas higher scores on the TOPS indicated better abilities. Significant negative effects were also found between organization-in-time abilities and emotional responses in both groups (research group: β = 0.56, p < 0.001; control group: β = 0.71, p < 0.001), with a stronger effect among participants in the control group (p = 0.016).
Discussion
This study describes the results of a secondary analysis based on data from three previous studies conducted in one laboratory. In all three studies, a research group of adults with NDD and a match control group without NDD were compared. The comparison included organization-in-time abilities of daily activities and their emotional consequences following decreased organization-in-time, as well as sensory, motor, EF, and sleep functions. The results highlight associations among these body functions and organization-in-time abilities with emotional consequences of daily disorganization-in-time.
This discussion relates first to the sample demographics and then to the study hypotheses, as defined in the Study Rationale and Aims section. As with previous results [Citation21], the sample’s demographic characteristics show that significantly fewer adults with NDD than controls achieved academic education or reported a stable relationship with a spouse.
Additionally, as with previous results, we found significant between-group differences in organization-in-time abilities, sensory, motor, metacognitive EF (EF-MI), and sleep quality [Citation4,Citation7,Citation21,Citation28,Citation29,Citation43]. Significantly more participants in the research group than in the control group were defined as dealing with untypical sensory-processing patterns, decreased motor coordination and EF abilities, or low sleep quality. These results strengthen our previous results, this time with a larger sample, and broaden the existing literature by identifying characteristics of adults with NDD.
The literature describes some implications of these body functions related to daily activities and participation. Therefore, our results that more than a third of the participants in the group with NDD dealt with two or more decreased sensory/motor/EF/sleep functions emphasize the implications of comorbidity and the vast burden of NDD on people’s daily lives. Considering the possible implications for daily function, a more holistic picture of these functions must be gathered when planning evaluation and intervention methods for people with NDD.
Regarding the study hypotheses, overall, the results show that the predicted conceptual model describes interactions between sensory/motor/EF/sleep functions, organization-in-time, and emotional responses following disorganization-in-time. The model may be applied to both groups or each group separately. The model fits well using sensory processing and motor coordination to predict EF-MI and sleep quality, in turn predicting organization-in-time abilities and emotional responses following disorganization ().
However, certain effects were unexpectedly stronger among the control group, including those between sensory processing and sleep quality, motor coordination and EF, sleep quality and organization-in-time, EF and organization-in-time, and organization-in-time and emotional responses. These unanticipated findings may be attributed to the self-reported nature of the questionnaires used in this study. Consistent with previous research [Citation13], people with NDD may have difficulty accurately estimating their abilities compared to their actual performance. This discrepancy might explain the observed results. It is worth continuing to examine these findings and explanation in additional studies.
Organization-in-time and emotional consequences
In this secondary analysis, organization-in-time abilities predicted the participants’ emotional responses. Previous studies tied decreased organization-in-time abilities to negative emotional responses among adults with SLD [Citation13] and ADHD [Citation71]. Ferdous et al. [Citation72] indicated that life balance is achieved not according to how many roles people have but how they organize their time within their tasks. For instance, students’ organization-in-time levels predicted their life participation, motivation, and enjoyment [Citation73]. Unsuccessful organization-in-time could cause dysfunctional behaviours like being late to lessons or work, result in distress, and affect the person’s ability to regulate emotional responses [Citation13].
Sensory processing
In both groups, sensory processing significantly correlated with EF-MI, motor coordination, and sleep quality. The relationship between sensory and motor functions is unsurprising. Sensory processing and motor abilities are interconnected aspects of human functioning since early development [Citation74]. Recent studies reported that visual feedback increased the information available to the brain when generating complex, adaptive motor output among physically healthy adults [Citation75] and described sensory functions and EF-MI as related [Citation43,Citation76]. Explaining those associations, Drigas and Mitsea [Citation77] tied sensory awareness to inner and external stimuli and cognitive attentional processes. They suggested that capturing too many stimuli reduces attentional resources and slows sensory processing. If the sensory processing is efficient, it enables the mind to receive and process the sensory input according to the task or goals the person wishes to achieve. However, the results show that the sensory processing is more commonly inefficient among adults with NDD.
The finding of the significant relationships between sensory processing and sleep quality among adults with NDD broadens the limited literature about such relationships in this population [Citation4, Citation21, Citation78]. As with the current findings, previous neurophysiologic studies claimed that people with insomnia are more aroused than are good sleepers because sensory hyperarousal decreases their ability to successfully filter external sensory information during sleep [Citation79,Citation80].
The results of the current data analysis identify sensory processing as a central mechanism interacting with body functions (particularly EF-MI and sleep quality) that significantly and directly affect the daily activities of people with NDD, as expressed in their organization-in-time abilities. Given their possibly crucial impact on participation in various life domains and on their emotional status [Citation24], our findings suggest that sensory functions must be considered in evaluations and interventions of people with NDD.
Motor coordination
The results of this data analysis demonstrate a significant relationship between motor coordination and EF-MI among adults with NDD. Although the literature on adolescents and adults with DCD is limited, the few existing studies suggested that this population experiences difficulties performing EF-based daily tasks [e.g., Citation81]. These results indicate that the input adults with NDD receive from their sensory and motor systems contribute to decreased EF-MI and, thus, to decreased performance of daily tasks. Previous literature about the implications of deficient motor coordination on adults’ health-related quality of life [Citation82] led to the need to consider this domain when evaluating adults with SLD and/or ADHD.
Executive functions
In both the research and control groups in this secondary data analysis, EF-MI significantly correlated with organization-in-time abilities. This finding stresses the meaning of efficient EF-MI among adults without NDD versus the inefficient EF-MI of adults with NDD and the effect of this difference on their daily challenges and emotional reactions. This finding emphasizes the need to relate to EF in evaluation and intervention processes among adults with NDD to increase their daily organizational abilities and, consequently, their quality of life [Citation7].
Sleep quality
The SEM model revealed that sleep quality is also tied with organization-in-time abilities at the level of daily activities and participation, with a stronger relationship in the group with NDD. The existing literature on the implications of decreased sleep quality and quantity on adults’ work performance [Citation4] supports the effects found in our study between organization-in-time abilities and sleep quality in both the research and control group. Increased sleep deprivation considerably affected information processing, reducing task performance [Citation83].
Summary
The holistic picture presented in this study ties decreased organization-in-time and varied body functions to consequential emotional responses among adults with NDD (SLD and/or ADHD). Their daily experiences may cause negative emotions, and, presumably, negative environmental feedback may lead to more negative feelings. Such emotional and psychological factors add to the challenges that people with NDD may experience and may further affect their performance [Citation51]. Negative daily experiences can have a high cost in frustration, self-concept, and self-esteem in multiple life domains, including home, work, social, and leisure environments [Citation4,Citation17].
Describing the results of this secondary data analysis in ICF terms [Citation9], it appears that people with health conditions, such as NDD (SLD/ADHD), may experience decreased body functions, including sensory and motor functions, EF-MI, and sleep quality. These related sensory and motor body functions affect EF and sleep quality, disorganizing their body functions. The directly decreased EF-MI and sleep quality affect their activity levels, as reflected in decreased organization-in-time abilities and limited participation in various life domains. Due to a disorganization of time, adults with NDD may express extreme emotional responses. Previous literature suggested that, in the long run, these negative daily experiences may affect their emotional quality of life [Citation7] and lead to additional health conditions, such as depression and anxiety [e.g., Citation4]. Depression and anxiety may result in activity limitations, decreased participation, and different life outcomes in adulthood [e.g., Citation17].
Limitations and future research
This study’s results were based on a secondary data analysis obtained through participants’ subjective self-reports. Future research should use additional objective measures and investigate the possible contributions to this model of additional ICF components, including other body functions and contextual/environmental factors.
Conclusions
The effects among the varied domains reveal intricate relationships between daily functional abilities, such as organization-in-time (classified under activity and participation) and the body functions of sensory, motor, EF-MI, and sleep functions. Our proposed model elucidates an axis of decreased emotional regulation and organization-in-time among adults with NDD, offering a comprehensive view of the interdependencies between these capabilities and overall daily functioning. Crucially, it highlights the emotional consequences of activity limitations, which, if occurring daily, may detrimentally affect emotional health and potentially lead to depression and anxiety [Citation84,Citation85]. Zisman-Ilani [Citation86]. indicated that unrecognized personal differences causing mental deficiencies and the lack of early treatment can exacerbate symptoms, potentially leading to psychiatric conditions. Our study’s distinctiveness lies in its holistic approach, integrating emotional and functional dimensions to provide a clearer "big picture" of NDD.
Implications
This study underscores the need for early and precise evaluation and intervention for people with NDD to prevent secondary negative emotional effects, different life outcomes, and decreased quality of life. In so doing, it aims to inform clinical practices and therapeutic strategies, ensuring that interventions are comprehensive and tailored to address the neurodevelopmental, functional, and emotional aspects of NDD.
Disclosure statement
The authors report no conflicts of interest.
Data availability statement
The data that support the findings of this study are available on request from the corresponding author [SR]. The data are not publicly available because they contain information that could compromise the research participants’ privacy.
Additional information
Funding
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. Text rev., 5th ed. American Psychiatric Publishing; 2022.
- Kooij JJS, Bijlenga D, Salerno L, et al. Updated European Consensus Statement on diagnosis and treatment of adult ADHD. Eur Psychiatry. 2019;56(1):14–34. doi: 10.1016/j.eurpsy.2018.11.001.
- Bonti E, Giannoglou S, Georgitsi M, et al. Clinical profiles and socio-demographic characteristics of adults with specific learning disorder in northern Greece. Brain Sci. 2021;11(5):602. doi: 10.3390/brainsci11050602.
- Grinblat N, Rosenblum S. Work participation, sensory processing and sleep quality in adults with attention-deficit hyperactive disorder. Work. 2022;73(4):1235–1244. doi: 10.3233/WOR-211129.
- Koepp AE, Watts TW, Gershoff ET, et al. Attention and behavior problems in childhood predict adult financial status, health, and criminal activity: a conceptual replication and extension of Moffitt et al.(2011) using cohorts from the United States and the United Kingdom. Dev Psychol. 2023;59(8):1389–1406. doi: 10.1037/dev0001533.
- Matthies S, Sadohara-Bannwarth C, Lehnhart S, et al. The impact of depressive symptoms and traumatic experiences on quality of life in adults with ADHD. J Atten Disord. 2018;22(5):486–496. doi: 10.1177/1087054716654568.
- Sharfi K, Rosenblum S. Executive functions, time organization and quality of life among adults with learning disabilities. PLoS One. 2016;11(12):e0166939. doi: 10.1371/journal.pone.0166939.
- Grinblat N. Development and effectiveness evaluation of a personally tailored work-performance improvement tele-intervention among adults with ADHD [unpublished doctoral dissertation]. Israel: University of Haifa; 2023.
- World Health Organization. International Classification of Functioning, Disability and Health; 2001. Available from: https://www.who.int/standards/classifications/international-classification-of-functioning-disability-and-health
- Mitra S, Shakespeare T. Remodeling the ICF. Disabil Health J. 2019;12(3):337–339. doi:10.1016/j.dhjo.2019.01.008.
- Stucki A, Cieza A, Michel F, et al. Developing ICF core sets for persons with sleep disorders based on the International Classification of Functioning, Disability and Health. Sleep Med. 2008;9(2):191–198. doi: 10.1016/j.sleep.2007.01.019.
- Wennberg B. Keeping track of time daily time management, participation, and time-related interventions for children, adolescents, and young adults with neurodevelopmental disorders [doctoral dissertation, Linköping University]; 2019 (publication no. 1371347). doi: 10.3384/diss.diva-162113.
- Grinblat N, Rosenblum S. Why are they late? Timing abilities and executive control among students with learning disabilities. Res Dev Disabil. 2016;59:105–114. doi: 10.1016/j.ridd.2016.07.012.
- Rosenblum S. Validity and reliability of the Time Organisation and Participation Scale (TOPS). Neuropsychol Rehabil. 2012;22(1):65–84. doi: 10.1080/09602011.2011.640465.
- American Occupational Therapy Association. Occupational therapy practice framework: domain and process. Am J Occup Ther. 2020;56(6):609–639. doi: 10.5014/ajot.56.6.609.
- Mensah A, Kofi Adjei N. Work-life balance and self-reported health among working adults in Europe: a gender and welfare state regime comparative analysis. BMC Public Health. 2020;20(1):1052. doi: 10.1186/s12889-020-09139-w.
- Sharfi K, Rosenblum S. Activity and participation characteristics of adults with learning disabilities: a systematic review. PLoS One. 2014;9(9):e106657. doi: 10.1371/journal.pone.0106657.
- Miller LJ, Coll JR, Schoen SA. A randomized controlled pilot study of the effectiveness of occupational therapy for children with sensory modulation disorder. Am J Occup Ther. 2007;61(2):228–238. doi: 10.5014/ajot.61.2.228.
- Dunn W. The impact of sensory processing abilities on the daily lives of young children and their families: a conceptual model. Infants Young Child. 1997;9(4):23–35. doi: 10.1097/00001163-199704000-00005.
- Engel-Yeger B, Shochat T. The relationship between sensory processing patterns and sleep quality in healthy adults. Can J Occup Ther. 2012;79(3):134–141. doi: 10.2182/cjot.2012.79.3.2.
- Sharfi K, Rosenblum S. Sensory modulation and sleep quality among adults with learning disabilities: a quasi-experimental case-control design study. PLoS One. 2015;10(2):e0115518. doi: 10.1371/journal.pone.0115518.
- Engel-Yeger B, Dunn W. Relationship between pain catastrophizing level and sensory processing patterns in typical adults. Am J Occup Ther. 2011a;65(1):e1–e10. doi: 10.5014/ajot.2011.09004.
- Engel-Yeger B, Dunn W. The relationship between sensory processing difficulties and anxiety level of healthy adults. Br J Occup Ther. 2011b;74(5):210–216. doi: 10.4276/030802211X13046730116407.
- Serafini G, Gonda X, Canepa G, et al. Extreme sensory processing patterns show a complex association with depression, and impulsivity, alexithymia, and hopelessness. J Affect Disord. 2017;210:249–257. doi: 10.1016/j.jad.2016.12.019.
- Kirby A, Edwards L, Sugden D, et al. The development and standardization of the Adult Developmental Coordination Disorders/Dyspraxia Checklist (ADC). Res Dev Disabil. 2010;31(1):131–139. doi: 10.1016/j.ridd.2009.08.010.
- Tal-Saban M, Zarka S, Grotto I, et al. The functional profile of young adults with suspected developmental coordination disorder (DCD). Res Dev Disabil. 2012;33(6):2193–2202. doi: 10.1016/j.ridd.2012.06.005.
- Zaguri-Vittenberg S, Weintraub N, Tal-Saban M. “It feels as though I need to exert more effort than others”: the experience of daily participation of young adults with developmental coordination disorder (DCD); a qualitative study. Disabil Rehabil. 2023;46(15):3332–3341. doi: 10.1080/09638288.2023.2246376.
- Sharfi K. Examining health conditions, body functions, activity and participation, and quality of life among adults with learning disabilities: towards a theoretical model [doctoral dissertation, University of Haifa]. ProQuest Theses and Dissertations Global; 2015 (publication no. 2874627).
- Grinblat N, Rosenblum S. Relationship between comorbid disorders and work features among adults with attention deficit hyperactivity disorder (ADHD). Am J Occup Ther. 2019;73(4_Supplement_1):7311515274p1. doi: 10.5014/ajot.2019.73S1-PO4040.
- Blank R, Barnett AL, Cairney J, et al. International clinical practice recommendations on the definition, diagnosis, assessment, intervention, and psychosocial aspects of developmental coordination disorder. Dev Med Child Neurol. 2019;61(3):242–285. doi: 10.1111/dmcn.14132.
- Poyraz Findik OT, Erdogdu AB, Fadiloglu E. Motor skills in children with specific learning disorder: a controlled study. Dusunen Adam. 2022;35(2):101–110. doi: 10.14744/DAJPNS.2022.00181.
- Green D, Baird G, Sugden DA. A pilot study of psychopathology in developmental coordination disorder. Child Care Health Dev. 2006;32(6):741–750. doi: 10.1111/j.1365-2214.2006.00684.x.
- Katz N, Maeir A. Higher-level cognitive functions enabling participation: awareness and executive functions. In Katz N, editor. Cognition, occupation, and participation across the life span: neuroscience, neurorehabilitation, and models of intervention in occupational therapy. 3rd ed. American Occupational Therapy Association; 2011. p. 13–40.
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington (DC): American Psychiatric Association; 2013. doi: 10.1176/appi.books.9780890425596.
- Josman N, Meyer S. Conceptualisation and use of executive functions in paediatrics: a scoping review of occupational therapy literature. Aust Occup Ther J. 2019;66(1):77–90. doi: 10.1111/1440-1630.12525.
- Crone EA, Dahl RE. Understanding adolescence as a period of social–affective engagement and goal flexibility. Nat Rev Neurosci. 2012;13(9):636–650. doi: 10.1038/nrn3313.
- Ferguson HJ, Brunsdon VE, Bradford EE. The developmental trajectories of executive function from adolescence to old age. Sci Rep. 2021;11(1):1382. doi: 10.1038/s41598-020-80866-1.
- Ardila A. On the evolutionary origins of executive functions. Brain Cogn. 2008;68(1):92–99. doi: 10.1016/j.bandc.2008.03.003.
- Mehta T, Mannem N, Yarasi NK, et al. Biomarkers for ADHD: the present and future directions. Curr Dev Disord Rep. 2020;7(3):85–92. doi: 10.1007/s40474-020-00196-9.
- Wilson P, Ruddock S, Rahimi-Golkhandan S, et al. Cognitive and motor function in developmental coordination disorder. Dev Med Child Neurol. 2020;62(11):1317–1323. doi: 10.1111/dmcn.14646.
- Josman N, Rosenblum S. A metacognitive model for children with neurodevelopmental disorders. In: Katz N, Toglia JP, editors. Cognition, occupation, and participation across the life span: models for intervention in occupational therapy. 4th ed. AOTA Press; 2018. p. 273–293.
- Graham S. Attention-deficit/hyperactivity disorder (ADHD), learning disabilities (LD), and executive functioning: recommendations for future research. Contemp Educ Psychol. 2017;50:97–101. doi: 10.1016/j.cedpsych.2017.01.001.
- Sharfi K, Rosenblum S, Meyer S. Relationships between executive functions and sensory patterns among adults with specific learning disabilities as reflected in their daily functioning. PLoS One. 2022;17(4):e0266385. doi: 10.1371/journal.pone.0266385.
- Smith-Spark JH, Henry LA, Messer DJ, et al. Executive functions in adults with developmental dyslexia. Res Dev Disabil. 2016;53:323–341. doi: 10.1016/j.ridd.2015.10.
- Gioia GA, Kenworthy L, Isquith PK. Executive function in the real world: BRIEF lessons from Mark Ylvisaker. J Head Trauma Rehabil. 2010;25(6):433–439. doi: 10.1097/HTR.0b013e3181fbc272.
- Surman CB, Walsh DM. Managing sleep in adults with ADHD: from science to pragmatic approaches. Brain Sci. 2021;11(10):1361. doi: 10.3390/brainsci11101361.
- Bolge SC, Doan JF, Kannan H, et al. Association of insomnia with quality of life, work productivity, and activity impairment. Qual Life Res. 2009;18(4):415–422. doi: 10.1007/s11136-009-9462-6.
- Wajszilber D, Santiseban JA, Gruber R. Sleep disorders in patients with ADHD: Impact and management challenges. Nat Sci Sleep. 2018;10:453–480. doi: 10.2147/NSS.S163074.
- Grigorenko EL, Compton DL, Fuchs LS, et al. Understanding, educating, and supporting children with specific learning disabilities: 50 years of science and practice. Am Psychol. 2020;75(1):37–51. doi: 10.1037/amp0000452.
- Valentine AZ, Brown BJ, Groom MJ, et al. A systematic review evaluating the implementation of technologies to assess, monitor and treat neurodevelopmental disorders: A map of the current evidence. Clin Psychol Rev. 2020;80:101870. doi: 10.1016/j.cpr.2020.101870.
- DuPaul GJ, Dahlstrom‐Hakki I, Gormley MJ, et al. College students with ADHD and LD: effects of support services on academic performance. Learn Disabil Res Pract. 2017;32(4):246–256. doi: 10.1111/ldrp.12143.
- DuPaul G, Gormley MJ, Laracy SD. Comorbidity of LD and ADHD: implications of DSM-5 for assessment and treatment. J Learn Disabil. 2013;46(1):43–51. doi: 10.1177/0022219412464351.
- Soper DS. Hyperparameter optimization using successive halving with greedy cross validation. Algorithms. 2022;16(1):17. doi: 10.3390/a16010017.
- Kessler RC, Adler L, Ames M, et al. The World Health Organization Adult ADHD Self-Report Scale (ASRS): a short screening scale for use in the general population. Psychol Med. 2005;35(2):245–256. doi: 10.1017/S0033291704002892.
- Pawaskar M, Fridman M, Grebla R, et al. Comparison of quality of life, productivity, functioning and self-esteem in adults diagnosed with ADHD and with symptomatic ADHD. J Atten Disord. 2020;24(1):136–144. doi: 10.1177/1087054719841129.
- Brown TE. Brown attention deficit disorder scales for adolescents and adults. San Antonio (TX): Psychological Corporation; 1996.
- Brown TE. Brown attention-deficit disorder scales. San Antonio (TX): Psychological Corporation; 2012.
- Brown C, Tollefson N, Dunn W, et al. Adult sensory profile. Am J Occup Therapy. 2001;55(1):75–82. doi: 10.5014/ajot.55.1.75.
- Engel-Yeger B. Validating the Adolescent/Adult Sensory Profile and examining its ability to screen sensory processing difficulties among Israeli people. Br J Occup Ther. 2012;75(7):321–329. doi: 10.4276/030802212X13418284515839.
- Roth RM, Gioia GA, Isquith PK. BRIEF-A: Behavior Rating Inventory of Executive Function®-adult version (BRIEF-A) [Database record]. APA PsycTests. 2005. doi: 10.1037/t86244-000.
- Vriezen ER, Pigott SE. The relationship between parental report on the BRIEF and performance-based measures of executive function in children with moderate to severe traumatic brain injury. Child Neuropsychol. 2002;8(4):296–303. doi: 10.1016/j.cpr.2020.101870.
- Regev S, Josman N. Evaluation of executive functions and everyday life for people with severe mental illness: a systematic review. Schizophr Res Cogn. 2020;21:100178. doi: 10.1016/j.scog.2020.100178.
- Roth RM, Lance CE, Isquith PK, et al. Confirmatory factor analysis of the Behavior Rating Inventory of Executive Function-adult version in healthy adults and application to attention-deficit/hyperactivity disorder. Arch Clin Neuropsychol. 2013;28(5):425–434. doi: 10.1093/arclin/act031.
- Rotenberg-Shpigelman S, Rapaport R, Stern A, et al. Content validity and internal consistency reliability of the Behavior Rating Inventory of Executive Function-Adult Version (BRIEF-A) in Israeli adults with attention-deficit/hyperactivity disorder. Isr J Occup Ther. 2008;17(2):77–96.
- Zomer J, Peled R, Rubin AH, et al. Mini Sleep Questionnaire (MSQ) for screening large populations for EDS complaints. In: Koella WP, Ruther E, Schulz H, editors. Sleep ‘84. Stuttgart:. Gustav Fischer; 1985. p. 467–470.
- Natale V, Fabbri M, Tonetti L, et al. Psychometric goodness of the Mini Sleep Questionnaire. Psychiatry Clin Neurosci. 2014;68(7):568–573. doi: 10.1111/pcn.12161.
- Fabbri M, Beracci A, Martoni M, et al. Measuring subjective sleep quality: a review. Int J Environ Res Public Health. 2021;18(3):1082. doi: 10.3390/ijerph18031082.
- Cohen Elimelech O. Functional cognition, time organization ability and driving performance among adults with ADHD [Unpublished master’s thesis]. Haifa (Israel): University of Haifa; 2020.
- Arbuckle JA. IBM SPSS version 22 [Computer Program]; 2014.
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. 2008;40(3):879–891. doi: 10.3758/BRM.40.3.879.
- McGough JJ. Treatment controversies in adult ADHD. Am J Psychiatry. 2016;173(10):960–966. doi: 10.1176/appi.ajp.2016.15091207.
- Ferdous T, Ali M, French E. Use of flexible work practices and employee outcomes: the role of work–life balance and employee age. J Manag Organ. 2021;29(5):833–853. doi: 10.1017/jmo.2020.44.
- Porath M, Rosenblum S. Interaction between time organization and participation dimensions among higher education students. Br J Occup Ther. 2019;82(5):306–315. doi: 10.1177/0308022618816641.
- Kojovic N, Ben Hadid L, Franchini M, et al. Sensory processing issues and their association with social difficulties in children with autism spectrum disorders. J Clin Med. 2019;8(10):1508. doi: 10.3390/jcm8101508.
- Shafer RL, Solomon EM, Newell KM, et al. Visual feedback during motor performance is associated with increased complexity and adaptability of motor and neural output. Behav Brain Res. 2019;376: Article 112214. doi: 10.1016/j.bbr.2019.112214.
- Alperin BR, Tusch ES, Mott KK, et al. Investigating age-related changes in anterior and posterior neural activity throughout the information processing stream. Brain Cogn. 2015;99:118–127. doi: 10.1016/j.bandc.2015.08.001.
- Drigas A, Mitsea E. 8 pillars X 8 layers model of metacognition: educational strategies, exercises & trainings. Int. J Online Biomed Eng. 2021;17(8):115–134. doi: 10.3991/ijoe.v17i08.23563.
- Lufi D, Tzischinsky O. The relationships between sensory modulation and sleep among adolescents with ADHD. J Atten Disord. 2014;18(8):646–653. doi: 10.1177/1087054712457036.
- Devoto A, Violani C, Lucidi F, et al. P300 amplitude in subjects with primary insomnia is modulated by their sleep quality. J Psychosom Res. 2003;54(1):3–10. doi: 10.1016/S0022-3999(02)00579-2.
- Milner CE, Cuthbert BP, Kertesz RS, et al. Sensory gating impairments in poor sleepers during presleep wakefulness. NeuroReport. 2009;20(3):331–336. doi: 10.1097/WNR.0b013e328323284e.
- Fogel Y, Stuart N, Joyce T, et al. Relationships between motor skills and executive functions in developmental coordination disorder (DCD): a systematic review. Scand J Occup Ther. 2023;30(3):344–356. doi: 10.1080/11038128.2021.2019306.
- Engel-Yeger B. The role of poor motor coordination in predicting adults’ health related quality of life. Res Dev Disabil. 2020;103:103686. doi: 10.1016/j.ridd.2020.103686.
- Litwiller B, Snyder LA, Taylor WD, et al. The relationship between sleep and work: a meta-analysis. J Appl Psychol. 2017;102(4):682–699. doi: 10.1037/apl0000169.
- Asadi H, Shoham R, Pollak Y. Intertwined associations among attachment styles, emotional dysregulation, and ADHD: examining unique associations with general risk-taking behavior. J Neural Transm. 2021;128(7):957–968. doi: 10.1007/s00702-021-02320-4.
- Torrente F, López P, Alvarez Prado D, et al. Dysfunctional cognitions and their emotional, behavioral, and functional correlates in adults with attention deficit hyperactivity disorder (ADHD): is the cognitive-behavioral model valid? J Atten Disord. 2014;18(5):412–424. doi: 10.1177/1087054712443153.
- Zisman-Ilani Y. The mental health crisis of individuals with intellectual and developmental disabilities. Psychiatr Serv. 2023;73(3):245–246. doi: 10.1176/appi.ps.202200022.
