Abstract
Women with cerebral palsy have the same sexual and reproductive healthcare (SRH) needs and rights as non-disabled women across the life course. Multi-level barriers prevent their SRH needs from being met in a timely way. Grouped according to Bronfenbrenner’s socio-ecological model, these include physical and psychosocial determinants. The aim of this scoping review was to collate global literature of access to, and utilisation of, SRH for women with cerebral palsy across the life course. We screened five databases for international empirical studies published in English between 2000–2019. Twelve studies met the inclusion criteria. The review highlights that women with cerebral palsy face challenges to receiving good quality healthcare, including limited practitioner knowledge and training on the effects of cerebral palsy in adulthood and how it interacts with women’s SRH needs. Much more research is needed to inform the provision of appropriate SRH treatment for women with cerebral palsy across the life course.
This article blends together the findings of 12 international studies on healthcare of girls and adult women with cerebral palsy, particularly focusing on sexual and reproductive health and healthcare.
The review indicates a significant gap in evidence about the experiences of healthcare transitions for women with cerebral palsy as they move from childhood to adulthood and children’s to adult healthcare
The review highlights large gaps in the global literature, in relation to sexual and reproductive healthcare across the lifecourse of disabled women in general, but women with cerebral palsy in particular.
The studies found that General Practitioners (GPs) (family doctors) did not consider how prescribed contraceptives relate to impairment effects for girls and women with cerebral palsy.
Barriers to good quality sexual and reproductive healthcare for women with cerebral palsy include: inaccessible physical environment and procedures (cervical smear and breast scans), and limited practitioner knowledge about the effects of cerebral palsy in adulthood for women and its interaction with sexual and reproductive health needs.
Points of interest
Introduction
Access to and utilisation of sexual and reproductive healthcare (SRH) is a key principle of the UK National Health Service (NHS) (Wenzl, McCuskee, and Mossialos Citation2015) and a global human right for disabled women including women with cerebral palsy (United Nations Citation2015). Article 25 of the UNCRPD states that appropriate measures should be taken to ensure health services provide disabled people with all types of health care, including SRH, in a gender sensitive way and of the same standard and affordability as provided to non-disabled people. Neglecting the SRH needs of disabled women is a violation of their human rights (United Nations Citation2015) and will increase risk of chronic disease and mortality (Ramjan et al. Citation2016).
Women with cerebral palsy require the same level of routine primary and preventative healthcare as non-disabled women, but previous studies have shown that they are under-represented in areas of preventative services and regular health checks such as cervical smears and mammograms (Llewellyn et al. Citation2011, Horner-Johnson, Dobbertin, and Iezzoni Citation2015). This is due to multiple-level barriers including lack of physical access to the service, negative responses from healthcare workers, lack of adaptable equipment, and presumptions of women’s sexual activity, sexual desires and multiple comorbidities (United Nations Citation2015; Becker, Stuifbergen, and Tinkle Citation1997; Jo’s Cervical Cancer Trust Citation2019). Long-standing prejudices and myths which construct disabled women as asexual; unable to become parents; and low risk victims of sexual violence can influence incorrect assumptions among health care practitioners (HCPs) that access to, and utilisation of, regular and good quality SRH is not a priority for disabled women (Hayward et al. Citation2017; Hameed et al. Citation2020). This can be exacerbated for women who have speech impairments and/or have difficulties being understood by HCPs, and can cause delays in diagnosis or preventative treatment, subsequently placing them at a higher risk of developing debilitating or life-threatening conditions (Boehme et al. Citation2015).
This paper reports a scoping review of empirical literature about access to, and utilisation of, sexual and reproductive healthcare for girls and women with cerebral palsy across the female life course, from youth to older life. This is timely as women with cerebral palsy are a growing group with the same rights to sexual and reproductive healthcare as all women, but research and service provision has mostly focused on children with cerebral palsy, with few systematic follow up studies for adults: research into the life cycle of women with cerebral palsy is particularly lacking.
In this article we provide a short background on the cerebral palsy impairment, particularly what it means for adult women; describe the scoping review method; and summarise our findings. For the purposes of this paper, the concept ‘life course’ indicates our focus on progression through biological and generational stages and socially negotiated life phases and norms: this includes consideration of how the body physically changes as females with cerebral palsy grow older, but also the roles and relationships women encounter as they move from one generational stage to the next, and the role social institutions and policies play to regulate this.
Background
Cerebral palsy is a non-genetic lifelong impairment, traditionally referred to as a childhood impairment, resulting from a non-progressive injury in the foetal or infant brain before, after or during birth (Moll and Cott Citation2013). It affects people’s limbs and motor system differently, depending on the part of the brain which is damaged, and varies in terms of severity. It is characterised by impairment in muscle, tone, movement and posture (Turk et al. Citation2001). International reporting on the prevalence of cerebral palsy ranges from 1.5 to more than 4 per 1000 live births (Arneson et al. Citation2009; Maenner et al. Citation2016). In the UK, NICE estimates 2–3.5 per 1000 live births result in cerebral palsy (Shaunak and Kelly Citation2018). The survival rates of infants with cerebral palsy has increased over time due to developments in neonatal and paediatric healthcare. Well-functioning adults with cerebral palsy are expected to live for around the same time as their non-disabled peers (Gannotti and Frumberg Citation2020; Morgan and McGinley Citation2014). This, together with the global age specific prevalence of disability being higher for women than men, suggests that women with cerebral palsy are a growing population (WHO, 2011).
People with cerebral palsy experience deterioration across multiple bodily functions as they age – including musculoskeletal, functional, psychological and communication systems – earlier than adults with no lifelong impairment (Mudge et al. Citation2016). There is limited evidence about the specific experiences of women and girls, but some early studies have reported that women with congenital impairments like cerebral palsy experience early hormonal changes, in terms of menarche and menopause (Becker, Stuifbergen, and Tinkle Citation1997; Siddiqi et al. Citation1999; Turk et al. Citation2001) influenced by the overall process of accelerated ageing (i.e. experiencing early symptoms of reaching old age). Previous empirical studies on disability and menopause have suggested that disabled women may experience earlier and more severe menopausal symptoms then their non-disabled contemporaries (De Almeida and Greguol Citation2015, Dormire, Becker, and Lin Citation2006). Losing the protective effect of oestrogen at an earlier age can lead to diminished skin integrity and tissue resiliency, which is particularly detrimental among wheelchair users (Dormire, Becker, and Lin Citation2006). Further, although physical activity is promoted to maintain the health and well-being of women during menopause (De Azevedo Guimarães and Baptista Citation2011, Moilanen et al. Citation2012), disabled women are less likely to participate in regular physical exercise and are thus at increased risk of cardiovascular, muscle and bone diseases, as well as hormonal changes (Dormire, Becker, and Lin Citation2006). Although low levels of activity in adulthood could be a result of reduction in mobility and functionality, and increase in pain, it is also a consequence of barriers to appropriate physical activity and a dearth in care and rehabilitation for adults with lifelong impairments, such as cerebral palsy (Hurvitz et al. Citation2021).
Women with cerebral palsy are likely to experience adversity through their engagement with disabling structures and relationships across the life course, the accumulation of which can negatively impact their psychosocial, physical and biological health and wellbeing (Ferraro and Shippee Citation2009). From childhood, women with cerebral palsy encounter disruptions across the perceived normative life course as a consequence of disabling social, political and environmental relationships and structures (Priestley Citation2003). These hamper their opportunities to meet generational milestones, establish relationships, and access support and resources, thus placing them at a disadvantage in relation to their nondisabled contemporaries (Shah and Priestley Citation2011; Moll and Cott Citation2013).
Keeping women and girls with cerebral palsy healthy and ensuring their health needs are met across the life course is challenging due to several factors. These include the problematic transition from child-centred to adult-centred healthcare, and the lack of specialist multidisciplinary teams and expertise specific to adults with cerebral palsy in general, and women with cerebral palsy in particular; absence of or truncated sexual health education (formal and informal); limited access to preventative healthcare and health promotion activities such as gyms and counselling services (Turk et al. Citation2001; Field, Scheinberg, and Cruickshank Citation2010).
Cervical smear tests and mammography (breast screening) are widely recognised procedures offered routinely to all women in the UK above the ages of 25 and 50 respectively, for the early detection of cancer in different stages of life (Citation2002). This has enabled the drastic reduction of cancer related death in women over the past few years (Wilacy and Tiley Citation2021). However routine screening of disabled women may be deferred by HCPs, as the invasive nature of equipment such as breast scanners and cervical smear tests may be uncomfortable or problematic for women with cerebral palsy to use, triggering pain and spasms (Poulos at al., 2006). Although alternative procedures such as smear tests under anaesthesia or mammograms using ultrasound can be used to overcome these problems, the perceived inconvenience of this, both to women and practitioners, is likely to lead to screening being deferred or cancelled (Ramjan et al. Citation2016). Such decisions are justified by the belief that disabled women are unlikely to be sexually active, and arethus at low risk of sexually transmitted diseases or the development of cervical cancer (Llewellyn et al. Citation2011; Poulos et al. Citation2006; Franco, Duarte-Franco, and Ferenczy Citation2001).
Table 1. Thematic chart.
Purpose
To provide a comprehensive overview of the factors associated with access and utilisation of healthcare, particularly in relation to sexual and reproductive health, for women and girls with cerebral palsy and how this is experienced across the life course.
Research process
We followed the processes and structure of a scoping review to identify relevant studies of women and adolescent girls with cerebral palsy in relation to the access to, and utilisation of, SRH. These included qualitative, quantitative, mixed method studies and systemic reviews between and including the years 2000 to 2019. We used a widely used framework for scoping reviews, developed by Arksey and O’Malley (Citation2005) which follows an iterative process across five core stages as described below:
Identification of research questions.
Identification of relevant studies.
Study selection.
Charting the data.
Collating, summarising and reporting results.
Identification of research questions
For women and girls with cerebral palsy:
What are the factors that influence access to sexual and reproductive healthcare and its utilisation?
How is sexual and reproductive healthcare accessed and utilised across the female life course?
What are the barriers and enablers to access and utilisation of health services?
Identification of relevant studies
We searched for literature published between 2000 and 2019 using relevant search terms and Boolean operators (e.g. or/and/*).
We searched five key databases across health and social care, chosen for their likelihood to contain articles about access to healthcare for women and teenage girls with cerebral palsy relevant to our review.
Study selection
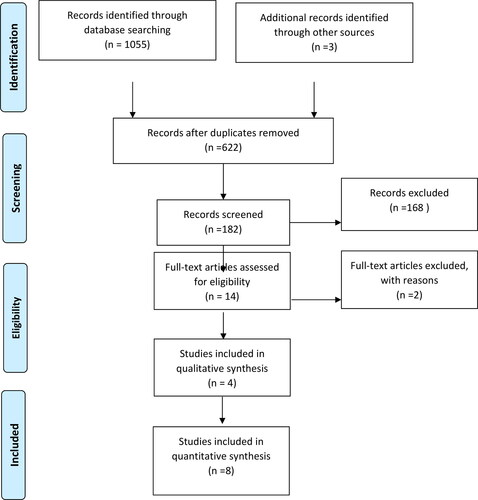
The flow of the articles through the review process are shown in the Preferred Reporting Items for Systematic Reviews and Meta Analyses (PRISMA) Flow Diagram (Page et al. Citation2021) (). This is an important representation of how the included studies made it into the review, that supports the description of the process in the following section.
The first author (initials, initials) undertook all the reviewing, after which the second and third authors (initials, initials) verified all stages. A total of 1,055 records were retrieved and appraised for their suitability for inclusion. After removal of duplicates, 619 records, identified through the database searches, were retained and supplemented with a further three, identified through manual searching (n = 622) – the method of identifying relevant articles through scrutiny of the references lists of the included articles and viewing their citations for further potentially relevant articles, rather than searching databases using keywords. At this stage, screening took place at the level of title only, according to a set of predetermined inclusion and exclusion criteria. Studies were included if they were:
Peer reviewed empirical studies
Focused on females with cerebral palsy (from puberty to menopause, or teenagers to older age (14 to over 55)
Focused on access and utilisation of healthcare, particularly sexual and reproductive healthcare
Published in English language
Following further exclusions, 182 records were then reviewed according to available abstracts, which resulted in 168 being excluded. Twelve articles met the inclusion criteria and were included in the review.
Charting the data
Key demographic information of each of the twelve included studies was extracted using Ritchie and Spencer’s (Citation2002) framework analysis approach. This included the demographic data of each article (i.e. title, author, method, aims). Framework analysis provides a clear, systematic process of organising, analysing and synthesizing data. Therefore it has become a popular approach in scoping reviews (Levac, Colquhoun, and O’Brien Citation2010). This analysis approach was used for the identification of key themes from the data, as well as details about each study’s principal findings and some recommendations for future research. We systematically built up the analytical frame through a process of charting one article, followed by another, and so on. This was an iterative, rather than linear process, with frequent revisiting of each included study to ensure completeness of the charting process.
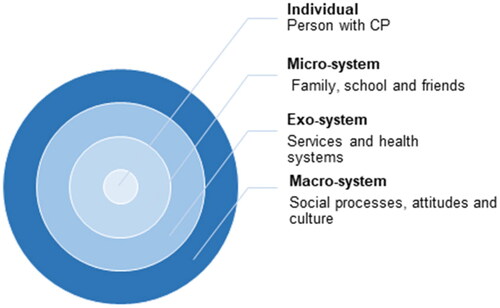
From the data extraction process and charting of data, we could conceptualise prominent themes within the dimensions of Bronfenbrenner’s (Citation1974) socio-ecological model, a theoretical framework adopted that inspired the thematic analysis of the data. shows this diagrammatically.
The socio-ecological model provides an interesting approach to examine the multiple layers of factors at play that determine the extent to which women and girls with cerebral palsy can access good quality healthcare to meet their SRH needs across the life course, from menarche to menopause. It considers the interaction between the micro-level individual factors and macro-level social structures (for instance, personal agency and healthcare institutions), and how these influence the women’s choices and trajectories across the female life cycle. In the centre of this model is the individual’s personal attributes which can impact their health and access to healthcare. These include age, gender, medical diagnosis (type of cerebral palsy), and the physical and psychosocial effects of impairment which change as individuals age, thus influencing the women’s access to and utilisation of healthcare. However, their choices and experiences are also influenced by family, school and peer relationships and other networks in their immediate environment, and regulated by organisational and societal level policies, culture, barriers and relationships.
We used the socio-ecological model and its different layers to construct a rudimentary thematic chart, capturing both the physical and psychosocial components associated with each ().
Collating, summarising, and reporting results
In this section we show how the thematic analysis can be summarised into a framework that captures the overall patterning of the findings ().
Table 2. Patterning chart.
Findings
Overview of included studies
We found 12 articles focusing on the health and healthcare of women and girls with cerebral palsy, from USA (n = 6), Australia (n = 3), Sweden (n = 2) and New Zealand (n = 1). They included biomedical studies focusing on specific health concerns, and papers that reported surveys exploring the reproductive healthcare of women with cerebral palsy. Most of the studies were concerned with the physical aspects of cerebral palsy, with limited mention of the psychosocial impacts associated with cerebral palsy. All papers were published in health-related journals and there was no engagement with disability theory. No papers considered the lifelong sexual and reproductive health needs of women with cerebral palsy (i.e. from puberty to post-menopause). We connect with these issues in the discussion.
The methods were predominantly quantitative (n = 8), with four articles reporting on qualitative studies. We were interested in a life-course approach and the generation of the participants included in the studies were as follows: Focus on adult women (n = 8), adolescents (n = 3) and both adult women and adolescent girls (n = 1). Disabled women’s life choices and experiences, including access and utilisation of SRH services, are influenced be a complex interplay of systems and structures which are connected and have bi-directional impact on each other. The ecological model, based on nested systems, provides a clear lens with which to identify the intersecting personal and social factors that determine the choices available to different women with cerebral palsy, and the extent to which their SRH needs are met.
Individual system
In our analysis, the first theme relates to the physical and psychosocial impacts of the cerebral palsy impairment on the individual across the life course, including secondary effects related to premature ageing and associated musculoskeletal abnormalities and decline. Fowler et al. (Citation2015) quantitative cross-sectional study, sampling premenopausal women and men under age 50, reported that adults with cerebral palsy had an average Bone Mineral Density (BMD) of 1 or 2 standard deviations below the general population when matched for age, gender and race. BMD scores were particularly low for adults who were non-ambulatory. The evidence is important to inform HCPs about appropriate treatment for this population. Zacharin, Savasi, and Grover (Citation2010) questionnaire-based study focused on the interplay of cerebral palsy impairment, menstruation effects and menstruation management practices for girls with cerebral palsy ages 12–18. The study reports how, although the prevalence and intensity of menarche for girls with cerebral palsy and girls with no impairment was not significantly different, there is a correlation between severity of impairment and the level of impact menstruation had on their participation in activities. Further, over half of families of the population surveyed sought medical advice in relation to menstruation management planning for their teenage daughter prior to or just after the start of menarche. Hayward et al. (Citation2017) survey-based study reported a high percentage of women with cerebral palsy (75%), especially those who were ambulatory, experienced loss or impeded mobility after pregnancy, but the impact of cerebral palsy on pregnancy was not discussed with the women’s primary care providers. The studies highlight the lack of knowledge and information base available for parents, carers, and HCPs about gynaecological needs of females with lifelong impairments like cerebral palsy, documenting this as a barrier to the provision of appropriate care and interventions for adolescent girls with cerebral palsy.
Morgan, Pogrebnoy, and McDonald (Citation2014), Mudge et al. (Citation2016), and Turk et al. (Citation2001) ethnographic studies report on secondary impairments in adults with cerebral palsy, associated to premature ageing. All were qualitative studies based in Australia, NZ, and USA respectively. All reported that ageing is accelerated in adults with cerebral palsy, causing pain, deterioration in mobility and functionality, and osteoporosis and osteopenia which is unlikely to be detected and treated as a consequence of limited knowledge of cerebral palsy in adult healthcare. Mudge et al. (Citation2016) interviewed 28 adults with cerebral palsy, including 14 women. As well as physical effects of ageing, they revealed the impact of ageing on their personal and social identity, feeling ‘more disabled’ as a consequence of age-related changes than their younger selves when they were more likely to identify as ‘normal’. These authors highlight the mental health issues experienced by adults with cerebral palsy, relating to changes in health and subsequent loss of ability to participate in different activities. Morgan, Pogrebnoy, and McDonald (Citation2014) interviewed six adults with cerebral palsy (five women) who had experienced mobility decline and falls in adulthood. Participants noted that physical changes also triggered changes in identity. The authors highlighted a frustration among the participants who perceived treatment they received in adulthood as inadequate, unlike their experiences of paediatric care. Participants described their frustration with service type and availability, facility access, staff knowledge and skills, staff turnover, and lack of engagement with their needs. One participant in the study pointed out:
I think there should be some sort of specialist that specialises in adult CP, because there isn’t. And if there is then they are hiding in the corner and people can’t afford them or people don’t know they are out there or something because I have a number of friends like me who say “I wish there was someone who can help us in our older age, work out what’s happening to our body or what’s going to happen or whatever,” because we all know we are going to age faster than the average bear and all that stuff and probably die earlier and have different issues earlier but if you know about it and you have no one to help you other than a GP who is just a basic GP without any disrespect, you’re not going to be able to help yourself very well. That’s my belief anyway. (Morgan, Pogrebnoy, and McDonald Citation2014, 286)
Micro system – family, school, and friends
Three papers focused on the people, institutions and relationships that influence how girls and women with cerebral palsy plan, manage and make decisions about different aspects of their SRH as they move through the life course. These include family members, friends, education, and healthcare practitioners. Hayward et al. (Citation2017) survey-based study reported that 20% of the women who responded to their survey experienced pregnancy, but less than a third had ever been asked by an HCP if they wanted to have children. This percentage was lower for respondents who were black (13.9%), did not attend college (27.3%) or were unable to work (20.3%). The study also indicated that many of the women reported decreased mobility during pregnancy (71%), but very few were offered appropriate rehabilitation or therapy, either physical or occupational or mental health.
The lack of communication about pregnancy with girls and women with cerebral palsy, by primary care providers, has been identified as a barrier to accessing good quality specialist healthcare for women with cerebral palsy on their reproductive journey. A similar finding was reported by Flavin et al. (Citation2019) and Zacharin, Savasi, and Grover (Citation2010) with regards to contraception for teenage girls. Both found that primary care workers did not consider the special healthcare needs of women with cerebral palsy when prescribing hormonal contraceptives: this was perhaps due to their limited recognition that teenage girls with cerebral palsy have the same level of sexual interest as those without impairments. Through surveying 344 women with cerebral palsy between ages of 18-66, Gray et al. (Citation2017) found that, compared to the general population, fewer women with cerebral palsy reported they had talked before the age of 18 years with a parent about how to say no to sex (41% vs. 63%, p<.001), methods of birth control (39% vs. 51%, p<.001), sexually transmitted infections (32% vs. 55%, p<.001), how to prevent HIV (30% vs. 41%, p<.001) and how to use a condom (19% vs. 29%, p<.001) The study indicated that topics of birth control were more likely to be discussed with a HCP than a parent.
Exo-system – services
The most common investigative theme of the reviewed literature was the service or organisational level factors that could potentially impact the quality of healthcare received by women with cerebral palsy across the life course. Altogether seven papers focused on this theme, divided into the physical and psychosocial aspects. Three of these (Morgan, Pogrebnoy, and McDonald Citation2014; Mudge et al. Citation2016; Nandam et al. Citation2018) considered the physical inaccessibility of services as a barrier to women with cerebral palsy accessing regular and good quality preventative healthcare on par to their non-disabled contemporaries. Based in Australia, Morgan, Pogrebnoy, and McDonald (Citation2014) ethnographic study reported participants’ perceptions of adult health services as being inadequate. They described their frustration with service type and availability, facility access, staff knowledge and skills, staff turnover, and lack of engagement with their needs. Similarly, Mudge et al. (Citation2016) highlighted how prior knowledge of impairment, together with a willingness to listen to the patient, resulted in positive patient-practitioner interaction. They showed, through patient experiences, how limited knowledge contributed to diagnostic overshadowing and thus the delay of appropriate treatment. Nandam et al. (Citation2018) study was the first to focus on breast screening of women with cerebral palsy. Through survey data from 118 women, age 40-64, they reported that most clinics were seen to be accessible, both in terms of environmental accommodations (e.g. ramps and lifts) and also staff attitudes. However, the study evidence indicated that the healthcare facilities surveyed were least likely to employ reasonable adjustments to accommodate such issues as difficulty standing or positioning the arm or using a wheelchair during the mammogram procedure. It was suggested that this may be due to a lack of training among mammography providers regarding the unique access needs of women with cerebral palsy. The authors identified this as a barrier to breast cancer screening compliance for women with cerebral palsy, which they reported as lower than that for general population. The authors suggested screening compliance rates would improve by addressing structural barriers and procedural accommodations, which would help decrease morbidity and mortality of this population.
Limitations in HCP knowledge and understanding about the interplay of cerebral palsy impairment effects and SRH for women and girls with cerebral palsy, across the life course, was also indicated in four other studies (Hayward et al. Citation2017; Sundelin et al. Citation2020; Zacharin, Savasi, and GroverCitation2010; Flavin et al. Citation2019). Both Flavin et al. (Citation2019) and Zacharin, Savasi, and Grover (Citation2010) focused on adolescent girls with cerebral palsy and contraceptive treatment. The studies highlight that when General Practitioners (GPs) prescribed contraceptives, no special considerations were taken regarding the girls’ impairment effects in combination with different forms of contraceptives. For example, Depot Medoxyprogesterone (DPMA) can lead to weight gain and, in women with cerebral palsy, could negatively impact walking and transfers. It could also cause decreased bone density, and thus increase risk of fractures after falls which are prevalent in adults with cerebral palsy who are ambulant (Stockburger and Omar Citation2015). In terms of reproductive healthcare of adult women, Hayward et al. (Citation2017) and Sundelin et al. (Citation2020) found more women with cerebral palsy become pregnant then expected, but the reproductive journey does have negative effects on mobility and has adverse risks on pregnancy outcomes. These studies found no evidence of specialist accommodations in place for these women.
Macro-system
The macro-system focuses on structural and cultural processes and practices in society that govern the perceptions, behaviour, and actions of its members. Three of the papers briefly discussed the societal level factors that could trigger healthcare inequalities for girls and women with cerebral palsy (Hayward et al. Citation2017; Gray et al. Citation2017; Nandam et al. Citation2018). In relation to preventative healthcare for older women, Nandam et al. (Citation2018) survey indicated that structural barriers did have an impact on the screening and mammography rates among women with cerebral palsy. They observed how environmental and procedural accommodations were cited as problematic within healthcare facilities. The authors noted that overall patient needs during the mammogram procedure were least likely to be assisted with or met – difficulties positioning arms (57.1%), difficulty with standing (59.3%), and need for a wheelchair-accessible machine (59.1%). They intimated this to be a consequence of the culture of medical training which focuses on the non-disabled female body. Nandam et al. (Citation2018) study also evidenced a correlation between severity of cerebral palsy and level of screening, indicating that women with multiple impairment effects were less likely to undergo regular screening with serious implications for their health and wellbeing.
Both Hayward et al. (Citation2017) and Gray et al. (Citation2017) discuss, albeit briefly, the impact of pervasive societal attitudes that disabled women and girls are asexual beings on their opportunities for sex and relationship education, and access to sexual and reproductive healthcare across the life course.
Discussion
The aim of this scoping review was to identify studies focusing on the access to and utilisation of healthcare, especially SRH, for girls and women with the diagnosis of cerebral palsy. Inspired by Bronfenbrenner’s (Citation1974) socio-ecological model, our analysis indicated that while none of the studies examined the issue solely in terms of the social context of the problem, a few did capture the organisational and societal factors that influenced the quality and timely delivery of SRH for the population in question. Each of the studies focused on experiences of health and health care of individuals in single generational cohorts (i.e. adolescence, adulthood and older life), rather than across the life course. This indicates a significant gap in evidence about the experiences of healthcare transitions for women with cerebral palsy as they move from childhood to adulthood and paediatric to adult healthcare.
Although limited studies exist which specifically focus on women with cerebral palsy, there are several recent international studies on the healthcare experiences of disabled women in general (Hameed et al. Citation2020; Matin et al. Citation2021). These evidence that disabled women encounter multiple challenges when negotiating access to healthcare, as well as their position and rights as females and sexual beings, across the life course. Structural and cultural barriers, including assumptions of sexual activity and limitations in medical knowledge and expertise, have generated disparities in the quality of sexual health education and care received by disabled and non-disabled women across the female life course (Matin et al. Citation2021; Llewellyn et al. Citation2011). Lacking a full knowledge and understanding of their sexual and reproductive health needs, and what healthcare trajectories should be followed by all women across the life course, makes disabled women vulnerable to sexual abuse or bad choices, and increases their risks of poor health, wellbeing, and quality of life. Ensuring they are socialised as sexual citizens and can access sexual and relationship education on par to their non-disabled contemporaries is important to reduce healthcare disparities for women with cerebral palsy in particular and disabled women in general, as emphasised by Article 25 of the Convention on the Rights of Persons with Disabilities (2006).
Our review suggests that practitioners and service providers need training about the lifelong effects of cerebral palsy for women and girls, and how the impairment effects interact with the female reproductive life cycle and hormones, in order to plan and provide the most appropriate treatment, management and mode of intervention to their patient. Girls and women with cerebral palsy, and those with other impairments, may have limited options or choices in terms of contraceptives. Decisions about which is the most suitable should be part of an honest dialogue between doctor and patient. Studies suggest that although oral contraceptives are the most frequently used, they have an increased embolic risk for people with reduced mobility or who use a wheelchair (Flavin et al. Citation2019) or can negatively impact tone and spasticity (Becker, Stuifbergen, and TinkleCitation1997). DPMA, given as an injection of 150 mg every 12 weeks, can be an effective contraceptive which is associated with lower rates of postmenstrual tension syndrome, and is easier to take for women who experience difficulties swallowing tablets, or have impaired manual dexterity which prevents the use of barrier methods (e.g. diaphragm or cap):but it does cause weight gain, and decreased bone density, which are particularly concerning for women with limited mobility (Stockburger and Omar Citation2015).
A handful of early studies, sampling women with different lifelong impairments (including cerebral palsy), have reported how this group experience menopause at an earlier age than non-disabled women (Turk et al. Citation2001; Siddiqi et al. Citation1999; Becker, Stuifbergen, and Tinkle Citation1997). During the perimenopause, a drop in oestrogen occurs, which can negatively affect women’s overall health and increase risks of osteoporosis and heart disease (Becker, Stuifbergen, and Tinkle Citation1997). As our review indicates, women with cerebral palsy will experience premature ageing, so are also likely to be at risk of secondary health conditions earlier than would be expected of the general population, including those associated with early menopausal symptoms. However more targeted research is needed to find out exactly how many years earlier menopause occurs for women with cerebral palsy, compared to women in the general population.
More research is necessary to generate new knowledge to inform the development of strategies and tailor-made interventions to meet the special SRH needs of women with cerebral palsy across the life course in a timely fashion. This includes regular screening with the assistance of well-trained staff in accessible environments, and other preventative health treatments that do not interfere with functionality, mobility and overall health and wellbeing of patients. Limitations in staff knowledge about cerebral palsy also can hinder women’s participation in breast screening and can lead to inappropriate and sometimes dangerous treatment (Barr et al. Citation2008). Furthermore, the feeling of not being understood or respected by HCPs can influence women’s decision to opt out of screening, thus contributing to low participation rates among disabled women and their increased risk of unmet need and preventable mortality (Barr et al. Citation2008; Mele, Archer, and Pusch Citation2005). It can also lead to complications for women with cerebral palsy during and/or after childbirth as GPs, gynaecologists and maternity health staff will not be aware that pregnancy can cause reduction in balance and mobility for this population of women, thus not be prepared with the necessary postnatal support and resources.
Strengths and limitations
Our review was limited to English language papers which may have missed other important work in this field. Whilst we have provided a broad picture of the links between cerebral palsy and SRH across the life course, it was surprising to find so little relevant research in the UK. The review highlights stark gaps in the global literature, in relation to SRH of females with cerebral palsy across the life course. There is a lack of evidence of how girls and adult women with cerebral palsy experience healthcare transitions, from paediatric to adult healthcare, with a particular focus on SRH. This suggests work is still required to meet Sustainable Development Goals (SDG) 3.7 – ensure universal access to sexual and reproductive healthcare services (United Nations Citation2015). Future work on cerebral palsy and other lifelong impairments should adopt a life course approach to health to prevent exposure to health risks, starting in early life and continuing (with specialist teams and interventions) through adulthood to older life. This approach would be useful to research the psychosocial impacts of cerebral palsy, particularly in relation to ageing and the female reproductive cycle. Such evidence is crucial to develop appropriate practices and policies that will appropriately support the physical and mental health and wellbeing of women with cerebral palsy as they grow older alongside their non-disabled peers.
Conclusions
This scoping review has highlighted stark gaps in research in relation to the access to and utilisation of SRH services for girls and women with cerebral palsy. The evidence from the twelve included studies identified that not much is known about the gynaecological health needs of women with cerebral palsy, the effects of cerebral palsy in adulthood, and indeed how both interact with and affect each other. As a result, girls and women with cerebral palsy are less likely than their non-disabled contemporaries to have their SRH needs met adequately and in a timely way. Further there is limited evidence of the social, environmental and economic factors that influence access to SRH for women with cerebral palsy, and indeed how education and social class play a part. More research is required in this area, especially in the UK and in low-income countries, to promote SRH services, education and interventions across the life course for girls and women with cerebral palsy and identify how to improve transitions between child and adult healthcare.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Arksey, H, and L. O’Malley. 2005. “Scoping Studies: Towards a Methodological Framework.” International Journal of Social Research Methodology 8 (1): 19–32. doi:10.1080/1364557032000119616.
- Arneson, C., M. Durkin, R. Benedict, R. Kirby, M. Yeargin-Allsopp, K. Van Naarden Braun, and N. Doernberg. 2009. “Prevalence of Cerebral Palsy: Autism and Developmental Disabilities Monitoring Network, Three Sites, United States, 2004.” Disability and Health Journal 2 (1): 45–48. doi:10.1016/j.dhjo.2008.08.001.
- Balandin, S., B. Hemsley, J. Sigafoos, and V. Green. 2007. “Communicating with Nurses: The Experiences of 10 Adults with Cerebral Palsy and Complex Communication Needs.” Applied Nursing Research: ANR 20 (2): 56–62. doi:10.1016/j.apnr.2006.03.001.
- Barr, J., T. Giannotti, T. Hoof, J. Mongoven, and M. Curry. 2008. “Understanding Barriers to Participation in Mammography by Women with Disabilities.” American Journal of Health Promotion: AJHP 22 (6): 381–385. doi:10.4278/ajhp.22.6.381.
- Becker, H., A. Stuifbergen, and M. Tinkle. 1997. “Reproductive Health Care Experiences of Women with Physical Disabilities: A Qualitative Study.” Archives of Physical Medicine and Rehabilitation 78 (12): S26–S33. doi:10.1016/S0003-9993(97)90218-5.
- Boehme, J., J. Yoshimachi, H. Matsumoto, M. Sullivan, T. Pickar, J. Dutkowsky, H. Kim, and D. Roye. 2015. “Healthcare Gaps Perceived by Women with Cerebral Palsy: J9.” Developmental Medicine & Child Neurology: 57 (S5).
- Bronfenbrenner, U. 1974. “Developmental Research, Public Policy, and the Ecology of Childhood.” Child Development 45 (1): 1. doi:10.2307/1127743.
- De Almeida, E. Werle, and M. Greguol. 2015. “Healthcare for Women with Disabilities in the Climacteric and Menopause.” Sexuality and Disability 33 (2): 279–298. doi:10.1007/s11195-014-9390-4.
- De Azevedo Guimarães, A, and F. Baptista. 2011. “Relationship between Physical Activity and Menopausal Symptoms.” Revista Brasileira de Atividade Física & Saúde 16 (2): 144–149.
- Dormire, S., H. Becker, and C. Lin. 2006. “Menopause Healthcare for Women with Physical Disabilities.” The Nurse Practitioner 31 (6): 42–50.
- Duffy, S., L. Tabár, and R. Smith. 2002. “The Mammographic Screening Trials: Commentary on the Recent Work by Olsen and Gøtzsche.” CA: a Cancer Journal for Clinicians 52 (2): 68–71.
- Ferraro, K, and T. Shippee. 2009. “Aging and Cumulative Inequality: How Does Inequality Get under the Skin?” The Gerontologist 49 (3): 333–343. doi:10.1093/geront/gnp034.
- Field, B., A. Scheinberg, and A. Cruickshank. 2010. “Health Care Services for Adults with Cerebral Palsy.” Australian Family Physician 39 (3): 165–167.
- Flavin, M., B. Shore, P. Miller, and S. Gray. 2019. “Hormonal Contraceptive Prescription in Young Women with Cerebral Palsy.” The Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine 65 (3): 405–409. doi:10.1016/j.jadohealth.2019.03.010.
- Fowler, E., S. Rao, A. Nattiv, K. Heberer, and W. Oppenheim. 2015. “Bone Density in Premenopausal Women and Men under 50 Years of Age with Cerebral Palsy.” Archives of Physical Medicine and Rehabilitation 96 (7): 1304–1309. doi:10.1016/j.apmr.2015.03.012.
- Franco, E., E. Duarte-Franco, and A. Ferenczy. 2001. “Cervical Cancer: Epidemiology, Prevention and the Role of Human Papillomavirus Infection.” CMAJ 164 (7): 1017–1025.
- Gannotti, M, and D. Frumberg. 2020. “Clinical Therapy Services for Adults with Cerebral Palsy.” Cerebral Palsy: 2519–2541.
- Gray, S., M. Wylie, Z. Bloom, R. Byrne, and L. Glader. 2017. “Reproductive Health Education Received by Young Women with Cerebral Palsy.” Journal of Pediatric and Adolescent Gynecology 30 (2): 286–287. doi:10.1016/j.jpag.2017.03.042.
- Hameed, S., A. Maddams, H. Lowe, L. Davies, R. Khosla, and T. Shakespeare. 2020. “From Words to Actions: Systematic Review of Interventions to Promote Sexual and Reproductive Health of Persons with Disabilities in Low- and Middle-Income Countries.” BMJ Global Health 5 (10): e002903. doi:10.1136/bmjgh-2020-002903.
- Hammar, G., A. Ozolins, E. Idvall, and C. Rudebeck. 2009. “Body Image in Adolescents with Cerebral Palsy.” Journal of Child Health Care: For Professionals Working with Children in the Hospital and Community 13 (1): 19–29. doi:10.1177/1367493508098378.
- Hayward, K., A. Chen, E. Forbes, R. Byrne, M. Greenberg, and E. Fowler. 2017. “Reproductive Healthcare Experiences of Women with Cerebral Palsy.” Disability and Health Journal 10 (3): 413–418. doi:10.1016/j.dhjo.2017.03.015.
- Horner-Johnson, W., K. Dobbertin, and L. Iezzoni. 2015. “Disparities in Receipt of Breast and Cervical Cancer Screening for Rural Women Age 18 to 64 with Disabilities.” Women’s Health Issues: Official Publication of the Jacobs Institute of Women’s Health 25 (3): 246–253. doi:10.1016/j.whi.2015.02.004.
- Hurvitz, E., D. Whitney, B. Waldron-Perrine, D. Ryan, H. Haapala, M. Schmidt, C. Gray, and M. Peterson. 2021. “Navigating the Pathway to Care in Adults with Cerebral Palsy.” Frontiers in Neurology 12: 1606. doi:10.3389/fneur.2021.734139.
- Jo’s Cervical Cancer Trust. 2019. “We’re made to feel invisible” Barriers to accessing cervical screening for women with physical disabilities. Available at: <https://www.jostrust.org.uk/our-research-and-policy-work/our-research/barriers-cervical-screening-physical-disabilities> [Accessed 5 April 2021].
- Levac, D., H. Colquhoun, and K. O’Brien. 2010. “Scoping Studies: Advancing the Methodology.” Implementation Science 5 (1), 1-9. doi:10.1186/1748-5908-5-69.
- Llewellyn, G., S. Balandin, A. Poulos, and L. McCarthy. 2011. “Disability and Mammography Screening: Intangible Barriers to Participation.” Disability and Rehabilitation 33 (19–20): 1755–1767. doi:10.3109/09638288.2010.546935.
- Maenner, M., S. Blumberg, M. Kogan, D. Christensen, M. Yeargin-Allsopp, and L. Schieve. 2016. “Prevalence of Cerebral Palsy and Intellectual Disability among Children Identified in Two U.S. National Surveys, 2011-2013.” Annals of Epidemiology 26 (3): 222–226. doi:10.1016/j.annepidem.2016.01.001.
- Matin, B., H. Williamson, A. Karyani, S. Rezaei, M. Soofi, and S. Soltani. 2021. “Barriers in Access to Healthcare for Women with Disabilities: A Systematic Review in Qualitative Studies.” BMC Women’s Health 21 (1), 1-23. doi:10.1186/s12905-021-01189-5.
- Mele, N., J. Archer, and B. Pusch. 2005. “Access to Breast Cancer Screening Services for Women with Disabilities.” Journal of Obstetric, Gynecologic, and Neonatal Nursing: JOGNN 34 (4): 453–464. doi:10.1177/0884217505276158.
- Moilanen, J., A. Aalto, J. Raitanen, E. Hemminki, A. Aro, and R. Luoto. 2012. “Physical Activity and Change in Quality of Life during Menopause-an 8-Year Follow-up Study.” Health and Quality of Life Outcomes 10 (1): 1–7. doi:10.1186/1477-7525-10-8.
- Moll, L, and C. Cott. 2013. “The Paradox of Normalization through Rehabilitation: Growing up and Growing Older with Cerebral Palsy.” Disability and Rehabilitation 35 (15): 1276–1283. doi:10.3109/09638288.2012.726689.
- Morgan, P, and J. McGinley. 2014. “Gait Function and Decline in Adults with Cerebral Palsy: A Systematic Review.” Disability and Rehabilitation 36 (1): 1–9.
- Morgan, P., D. Pogrebnoy, and R. McDonald. 2014. “Health Service Experiences to Address Mobility Decline in Ambulant Adults Ageing with Cerebral Palsy.” Journal of Intellectual & Developmental Disability 39 (3): 282–289. doi:10.3109/13668250.2014.927841.
- Mudge, S., J. Rosie, S. Stott, D. Taylor, N. Signal, and K. McPherson. 2016. “Ageing with Cerebral Palsy; What Are the Health Experiences of Adults with Cerebral Palsy? A Qualitative Study.” " BMJ Open 6 (10): e012551. doi:10.1136/bmjopen-2016-012551.
- Nandam, N., D. Gaebler-Spira, R. Byrne, J. Wolfman, J. Reis, C. Hung, A. Todd, J. Durkin, and C. Marciniak. 2018. “Breast Cancer Screening in Women with Cerebral Palsy: Could Care Delivery Be Improved?” Disability and Health Journal 11 (3): 435–441. doi:10.1016/j.dhjo.2018.02.002.
- Page, Matthew J., Joanne E. McKenzie, Patrick M. Bossuyt, Isabelle. Boutron, Tammy C. Hoffmann, Cynthia D. Mulrow, Larissa. Shamseer, et al. 2021. “The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews.” BMJ (Clinical Research ed.) 372: n71. doi:10.1136/bmj.n71.
- Poulos, A., S. Balandin, G. Llewellyn, and A. Dew. 2006. “Women with Cerebral Palsy and Breast Cancer Screening by Mammography.” Archives of Physical Medicine and Rehabilitation 87 (2): 304–307. doi:10.1016/j.apmr.2005.09.020.
- Priestley, M. 2003. Disability: A Life Course Approach. Polity, Cambridge, UK.
- Ramjan, L., A. Cotton, M. Algoso, and K. Peters. 2016. “Barriers to Breast and Cervical Cancer Screening for Women with Physical Disability: A Review.” Women & Health 56 (2): 141–156. doi:10.1080/03630242.2015.1086463.
- Ritchie, J, and L. Spencer. 2002. “Qualitative Data Analysis for Applied Policy Research.” In The Qualitative Research Companion, edited by A. Huberman and M. Miles, 305–329. Thousand Oaks: Sage.
- Shah, S, and M. Priestley. 2011. Disability and Social Change: Private Lives and Public Policies. Bristol: Policy Press.
- Shaunak, M, and V. Kelly. 2018. “Cerebral Palsy in Under 25 s: Assessment and Management (NICE Guideline NG62).” Archives of Disease in Childhood. Education and Practice Edition 103 (4): 189–193. doi:10.1136/archdischild-2017-312970.
- Siddiqi, S., D. Van Dyke, P. Donohoue, and D. McBrien. 1999. “Premature Sexual Development in Individuals with Neurodevelopmental Disabilities.” Developmental Medicine and Child Neurology 41 (6): 392–395. doi:10.1017/s0012162299000857.
- Stockburger, S, and H. Omar. 2015. “Women with Disabilities: Reproductive Care and Women’s Health.” International Journal of Child Health and Human Development 8 (4): 429–447.
- Sundelin, H., O. Stephansson, S. Johansson, and J. Ludvigsson. 2020. “Pregnancy Outcome in Women with Cerebral Palsy: A Nationwide population-based cohort study.” Acta Obstetricia et Gynecologica Scandinavica 99 (4): 518–524. doi:10.1111/aogs.13773.
- Turk, Margaret A., Joanne. Scandale, Paula P. Rosenbaum, and Robert J. Weber. 2001. “The Health of Women with Cerebral Palsy.” Physical Medicine and Rehabilitation Clinics of North America 12 (1): 153–168. doi:10.1016/S1047-9651(18)30088-3.
- United Nations. 2015. Sustainable Development Goals. New York: Sustainable Development Knowledge Platform.
- Wenzl, M., S. McCuskee, and E. Mossialos. 2015. “Commissioning for Equity in the NHS: Rhetoric and Practice.” British Medical Bulletin 115 (1): 5–17. doi:10.1093/bmb/ldv031.
- Wilacy, H, and C. Tiley. 2021. Screening Tests in the UK. Available at: https://patient.info/treatment-medication/screening-tests-in-the-uk. [Accessed 1 April 2021]. World Health Organization. 2011. World report on disability. Available at: <https://www.who.int/disabilities/world_report/2011/report.pdf>. [Accessed 5 April 2021].
- Zacharin, Margaret, Ingrid. Savasi, and Sonia. Grover. 2010. “The Impact of Menstruation in Adolescents with Disabilities Related to Cerebral Palsy.” Archives of Disease in Childhood 95 (7): 526–530. doi:10.1136/adc.2009.174680.