Abstract
Introduction: The study investigates health and social conditions among pregnant substance abusers and the children that were born from these pregnancies, and analyses outcomes in relation to type of substance abuse.
Methods: Register data concerning 97 pregnant substance abusers and 104 children, at birth and 5 years on, were analysed with descriptive statistics and chi square tests.
Results: The women presented a multitude of problems, including low education, substance abusing partners, and elevated smoking rates. Compared with the population, more children were born prematurely and average birth weight was almost 350 g lower. About 14% were diagnosed as being affected by maternal substance abuse. During follow-up, 5 women died and 88% showed continued substance-related mental and health problems. All children survived and 85% experienced placement in out-of-home care. Purchase of psychotropic drugs and mental health problems were more common among women with alcohol as one drug of preference.
Conclusions: Parenthood did not represent a turning point for pregnant substance abusers. Comprehensive and persistent support is necessary, but in the short-term, efforts should be made to curb excessive smoking rates. The children faced several disadvantages at birth, but a longer follow-up is required to assess the impact of maternal substance abuse properly.
Introduction
The prevailing notion that the foetus was practically invulnerable in the womb was severely challenged by a German measles epidemic during the early 1960s and the tragic effects of thalidomide prescribed to pregnant women against morning sickness. Since then there has been a substantial increase in clinical, public, and political interest in identifying and protecting the foetus from a whole range of potential harms – not least those associated with tobacco, alcohol and drug use. Apart from an upsurge in research on the effects of substance use in association with pregnancy, we have also witnessed an increased attention and controversy about policy responses to this problem (Lester, Andreozzi, & Appiah, Citation2004). The issue of substance use and pregnancy is, therefore, inherently a clinical, political, legal and ethical concern, and these dimensions are both tightly and loosely connected. As such, this is a perfect case for studying the knowledge-policy nexus (Hoppe, Citation2005).
As a carrier of future human capital, the pregnant woman is a favoured target for interventions aiming at reducing infant mortality and improving health outcomes (Legg, Citation2005; Weir, Citation2006). From a somewhat narrower perspective, it is also possible to define pregnancy and substance use as a part of the increased focus on ‘harms to others’ (Room et al., Citation2010). The typical policy response aimed at the broad population of pregnant women or women in childbearing ages has then been to develop guidelines for alcohol consumption, i.e. ‘safe’ drinking levels (International Center for Alcohol Policies, Citation1999; World Health Organization, Citation2014). These efforts have however exposed a precarious knowledge base and varying interpretations of scientific evidence with recommendations varying across time and between countries (Leppo & Hecksher, Citation2011).
Studies of prevalence and consequences of substance use and abuse among pregnant women are hampered by the same limitations as any such research, with the added challenge of measuring behaviours associated with high social undesirability. Nonetheless, epidemiological and clinical studies on the foetal impact of alcohol, drug, and tobacco use during pregnancy are plentiful. These studies usually focus on outcomes such as birth weight, birth deficiencies, as well as long-term effects on the child’s health, social and psychological development (Bauer et al., Citation2011; Della Grotta et al., Citation2010; Higgins, Clough, & Wallerstedt, Citation1995; Hjerkinn, Rosvold, & Lindbaek, Citation2009; Holmila, Raitasalo, & Kosola, Citation2013; Kissin, Svikis, Morgan, & Haug, Citation2001; Moe, Citation2002; Shankaran et al., Citation2007; Walton-Moss, McIntosh, Conrad, & Kiefer, Citation2009). Smaller clinical samples and register-based population studies have also been used to study substance abuse in connection with pregnancy or among mothers of small children (Holmila et al., Citation2013; Kahila, Gissler, Sarkola, Autti-Ramo, & Halmesmaki, Citation2010; Raitasalo, Holmila, Autti-Ramo, Martikainen, et al., Citation2015; Raitasalo, Holmila, Autti-Ramo, Notkola, & Tapanainen, Citation2015; Sarkola, Gissler, Kahila, Autti-Ramo, & Halmesmaki, Citation2012). In recent years, the increased use of opioid maintenance treatment (OMT) has induced a growing interest in OMT and pregnancy (Finnegan, Winklbaur, Fischer, Olofsson, & Welle-Strand, Citation2009; Lund, Skurtveit, Engeland, et al., Citation2013; Lund et al., Citation2012; Lund, Skurtveit, Sarfi, et al., Citation2013; Wilder, Lewis, & Winhusen, Citation2015).
Policy initiatives regarding women with risky or harmful consumption of alcohol or other drugs have aimed at improving (access to) treatment and care but also imposing legal actions and punishment (Cave, Citation2007; Lester et al., Citation2004; Stogner, Citation2010). Involuntary commitments of pregnant substance abusers1 for the sake of the foetus was, e.g. introduced in Norway in 1996 (Söderström & Skolbekken, Citation2012) and similar measures have in recent years been discussed and proposed in Sweden, Denmark and Finland (Leppo, Citation2012). In 2009, the Swedish government sought to amend the existing compulsory care legislation so that it would allow for involuntary commitments of pregnant substance abusers with the specific aim of protecting the foetus/child. However, the proposal was never presented to parliament and the issue disappeared from the political agenda with the change of government in 2010 (Reitan, Citation2011).
There is, nonetheless, nothing that prevents a pregnant woman from being committed to care as long as she meets the requisites stated in the Swedish Care for Substance Abusers (Special Provisions) Act. The act was first introduced in 1982 and according to the revised act from 1988 a person may be committed to compulsory care if (a) he/she has an ongoing abuse of alcohol, drugs or volatile solvents, (b) is in need of care in order to come clear of this abuse and (c) voluntary measures have proved to be insufficient. Moreover, it must be proved that he/she is at great risk of severely harming his or her health, or destroying his/her life, or that it can be feared the he/she will inflict serious harm to him-/herself or to a next of kin.2 The municipal social welfare board is obliged to apply to an administrative court for compulsory care if there is reason to believe a person fulfils these legal requisites. Around 1000 persons are annually committed to involuntary care for a maximum of six months. Approximately one third of the clients are women, of which some 10–15 are pregnant at some point during their placement. The government agency National Board of Institutional Care, NBIC, is responsible for providing compulsory care in one of their 11 closed facilities or in out- and inpatient services run by municipalities and other caregivers (Reitan Citation2016).
Political initiatives and public debate are commonly prompted by rapid increases in observed or perceived harms (e.g. the birth of ‘crack babies’ during the so-called crack epidemic of the 1980s (Hartman & Golub, Citation1999) or by lobby organisations’ efforts to draw attention to certain problems (Gibbs & Sherwood, Citation2017). Therefore, substance use and pregnancy is continuously present on the political agenda, albeit not always manifestly so. Why this issue materialised into political initiatives in Finland, Sweden and Denmark at the same time is not clear, but the EU alcohol strategy from 2006 (European Commission, Citation2006) is one likely driving force. The strategy’s first priority was to ‘protect young people, children and the unborn child’ from alcohol-related harms – a seemingly uncontroversial aim which nonetheless may have put pressure on the Nordic ministers to take some action in this direction (Stenius, Citation2009).
Although the strategy had a public health approach, a large part of the political debate came to revolve around severe substance abuse during pregnancy and various forms of compulsory measures. It is, then, fair to say that the potential political ‘power’ of the issue is far bigger than the actual number of pregnant substance abusers. They are perhaps small in numbers, but pregnant substance abusers are likely to consume a proportionally large amount of welfare services and the complexity and severity of their problems often poses a great challenge to the health care and social service systems. More importantly though, clinical practice is not devoid of the social, ethical, legal – and ultimately political – aspects of substance use and pregnancy (Anderson, Elk, & Andres, Citation1997). Hence, clinicians are in the midst of policy-making every day when deciding on how to approach these women, what measures to recommend, what knowledge to base their judgments on, etc. Parenthood may be a possible turning point in the recovery from substance abuse (Myra, Ravndal, Wie, & Wiig, Citation2016; Teruya & Hser, Citation2010), but the likelihood of a number of negative outcomes for both mother and child must be addressed as well.
It is then, important to increase our knowledge of the health and life conditions of women who seriously misuse substances – in order to identify hazards and harms, but also to uncover characteristics and outcomes that are relatively normal or positive.
Aims
This study aims to (1) investigate the health and social conditions in a clinical sample of pregnant substance abusers and the children that were born from these pregnancies in a 5-year perspective, and (2) analyse differences in outcomes during the follow-up period in relation to type of substance abuse. Findings will also be contrasted with comparable studies or the national population wherever possible.
Methods
Participants, data sources and procedures
The study encompasses all women who were pregnant in connection with placement in compulsory care for substance abuse in Sweden between 2000 and 2009, who ended up giving birth, and the children that were born from these pregnancies. Due to lack of complete data from any single documentation system, a number of sources within the NBIC were used to identify the relevant population. This procedure has been described in further detail elsewhere (Reitan & Weding, Citation2012). The gross sample came to consist of 106 cases where there was documentation that the woman had given birth to the child or where there was reason to believe so. Moreover, information about type of substance abuse, partners’ substance abuse, previous and later admissions was retrieved from these case records.
The study population was finally defined by matching personal identification numbers within the relevant timeframe for these 106 cases with entries in the Medical Birth Register (MBR). The MBR covers practically all births in Sweden (National Board of Health and Welfare, Citation2003). A total of 103 births and 104 live born children were identified in the register. Six women were pregnant and placed in compulsory care on two separate occasions, so the study’s net population came to include 97 women and 104 children.
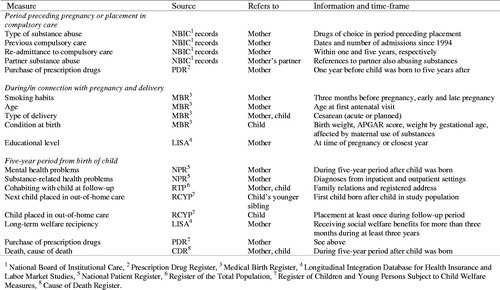
Through the MBR, the mothers’ personal identification numbers were matched with those of the children, and data on mothers and children was obtained from the MBR and six other national registers – the Register of Children and Young Persons Subject to Child Welfare Measures (RCYP), the National Patient Register (NPR), the Cause of Death Register (CDR), the Prescribed Drug Register (PDR), the Register of the Total Population (RTP), and the Longitudinal Integration Database for Health Insurance and Labour Market Studies (LISA). The first five are administered by the National Board of Health and Welfare and the last two by Statistics Sweden. Matching of information from these registers was performed by these two authorities, and personal identification numbers were replaced with anonymous serial numbers before data was made accessible to the project. An overview of measures and their sources, as well as which persons and the points of observation the data refer to, is provided in .
Points of observation
The study’s point of departure is an event combining three factors; placement in compulsory care for substance abuse, pregnancy and the following birth of a child from this pregnancy. The data relate to circumstances (a) before this event, (b) in connection with or during this event or (c) during the follow-up period. More specifically, information on previous commitments to care cover the time-period from 1994, when the NBIC was established. Data concerning type of substance abuse refer to circumstances leading up to this particular placement in compulsory care. Purchase of prescription drugs refers to the period starting one year before the child was born (in order to enable later analyses of impact of prescription drugs during pregnancy) till the end of the 5-year follow-up period. Data regarding smoking habits refer to both the period directly preceding the pregnancy and during the pregnancy. Cohabitation with the father of the child refers to the situation at the woman’s first antenatal visit, and her level of education refers to the closest time for which data was available – usually the same year.
The follow-up period was set to 5 years from the child’s birth. In three cases, comprehensive information was only available for 4 years due to data lag in several registries.
Measures
Drugs of preference is based on information from various client records at the NBIC. Up to five (classes of) drugs was recorded for each client: alcohol, opiates, methadone, cocaine, amphetamine, benzodiazepines, cannabis or other. Thereafter the women were categorised according to type of substance abuse. Because very few women had alcohol as their only preferred drug (6%) it was not feasible to distinguish between alcohol abuse, mixed alcohol and drug abuse, and drug abuse (Holmila et al., Citation2013). Therefore, women who had alcohol as one of their drugs of choice (32%) were placed in one group (AD), and those whose drugs of choice did not include alcohol (68%) in another (DD). Previous admission to compulsory care for substance abuse as well as readmissions within 1 and 5 years after the child was born, were all defined dichotomously (yes/no) based on administrative data from the NBIC. Records date back to 1994 when the NBIC was established. Partner substance abuse was based on references to the mother’s partner also abusing substances in client records at the NBIC. Level of education was based on self-reports from LISA and defined dichotomously in terms of having completed at least upper secondary school or not. Family status, i.e. whether the woman was living with the child’s father at the time of the first antenatal visit, and parity (the child’s birth order), were retrieved from MBR.
Data concerning the mother’s age and smoking habits during pregnancy, type of delivery, the child’s gestational age, birth weight, APGAR score, and whether the child was born prematurely, light for its gestational age, or affected by maternal use of alcohol or maternal use of drugs of addiction (ICD-10 codes P04.3, P04.4 and P96.1) were also obtained from MBR (WHO, Citation2010).
Long-term welfare dependency was defined as receiving social welfare benefits of at least SEK 9000 (corresponding to the maximum benefit of SEK 3000 per month for a single-person household in year 2000) during at least 3 years in the follow-up period (see Holmila et al., Citation2013). This information was collected from the LISA register. Information about placement in out-of-home care (at least once in the follow-up period) was obtained from the RCYP.
In accordance with Holmila et al. (Citation2013), mental health problems was measured dichotomously, taking into account whether the mother had received a psychiatric diagnosis from either in- or outpatient care in the follow-up period and having purchased prescription drugs for psychoactive medicines affecting the central nervous system from the year before giving birth to the end of the follow-up period. Psychiatric diagnoses were retrieved from NPR and included primary or secondary ICD-10 diagnoses related to schizophrenia, schizotypal and delusional disorders (F20–29), mood (affective) disorders (F30–39), neurotic, stress-related and somatoform disorders (F40–48) and disorders of adult personality and behaviour (F60–69). Purchase of prescription drugs included information from PDR about purchases of the following drugs, based on their ACT-codes (WHOCC, Citation2013); antipsychotics (N05A), tranquilisers and sedatives (N05B), sleeping medication (N05C) and antidepressants (N06A).
Alcohol or drug-related mental and behavioural problems and Alcohol and drug related health problems was defined dichotomously as the presence of at least one alcohol or drug-related ICD-10 diagnosis in the NPR; F10–F16 and F18–F19 (mental and behavioural disorders due to psychoactive substance use), B16, B17.0–1, B18.0–2 (acute/chronic viral hepatitis B, C and acute infection of hepatitis B carrier), B20–24 and Z21 (human immunodeficiency virus), K70–71 (alcoholic/toxic liver disease), T40–43 (poisoning by narcotics, other psychotropic drugs), T50–T51 (toxic effects of alcohol/organic solvents) and Z72.1–2 (lifestyle problems related to alcohol or drugs). Mortality included all deaths registered in the CDR. Child and mother cohabitation measured whether both were registered at the same address in the RTP.
Statistical analysis
Descriptive statistics were used to portray social and health characteristics of the mothers and children both at the outset and during/after the follow-up period and compared with population figures whenever possible. Differences in social situation and outcomes according to type of substance abuse were compared by Chi-square tests. Data analyses were performed with SPSS version 25 (SPSS, Chicago, IL).
Results
Social and medical status of women during pregnancy and at delivery
As shown in , the average age among the mothers in this study was just short of 29 years, varying between 19 and 46. For primaparas (52% of the pregnancies), the average age was 25.9 years. Almost a third of the women (29%) had completed upper secondary education and 38% were living with the father of the child at the first antenatal visit. There were indications that the partner was also abusing substances in 72% of the cases.
Table 1. Characteristics of clinical sample and corresponding population averages. Percent if not otherwise stated.
Commitment to compulsory care took place at different stages of the pregnancies (22% during the first trimester, 37% during the second and 41% in the last trimester). Almost half of the women had been committed to compulsory care before and 16% had experienced compulsory care for young persons.
The main drugs of preference were amphetamine, opiates and benzodiazepines/sedatives (23%, respectively), while cannabis and alcohol constituted the second most preferred substances (15 and 12, respectively). During the 3 months before pregnancy, more than 80% of the women were smoking, and almost half (48%) were still smoking in late pregnancy. At delivery (of which 24% were Caesareans), 8% of the women were diagnosed with mental and behavioural disorders due to psychoactive substance use, while 50% had viral hepatitis complicating pregnancy or childbirth. Moreover, 39% received maternal care for suspected damage to foetus from alcohol or drugs.
Status of children at birth
All children were live born and, as shown in , the average birth weight was 3176 g. Around 15% of the children weighed under 2500 g. Almost 14% were born prematurely and 6.7% were small for their gestational age. The proportion of children with a low Apgar score was 2.9%. At birth, 14% of the children were diagnosed as being affected by maternal use of substances.
Table 2. Characteristics of the children born to pregnant substance abusers (n = 104Table Footnotea). Percent if not otherwise stated.
Health and social situation of mothers and children at follow-up
As shown in , five of the 97 women in the study died in the follow-up period. All deaths were related to alcohol or drug-use, and most deaths were categorised as accidental (not shown in table). Some 80% of the women showed indications of mental health problems, of which 72% had received psychiatric treatment. Moreover, almost 9 out of 10 women had indications of continued alcohol- or drug-related health problems (77% with such principal diagnoses).
Table 3. Health and social situation of mothers during follow-up period (N = 103).
In terms of social problems, almost three out four mothers received long-standing income support during the follow-up period and 85% experienced their child being placed in out-of-home care at least once. After 5 years, 30% of the mothers were cohabiting with their child. One fourth of the women were readmitted to compulsory care at least once during the follow-up period. Nearly half of the women had some employment or studied at some point in the follow-up period. However, in the final follow-up year, only 16% of the women had some employment (not shown in table).
Outcome at follow-up in relation to type of substance abuse
Health and social outcomes by type of maternal substance abuse are presented in . In terms of previous or repeated compulsory care, the drug and alcohol group (DD), consisting of 68% of the mothers, was more likely to have been committed to compulsory care previously than the AD group. AD mothers were more likely to be readmitted to compulsory care within 1 year (although number of cases was very small), but there were no notable differences concerning readmission within 5 years. Moreover, the DD group was more likely to have a partner who also was abusing substances and to have had some form of employment in the follow-up period. AD mothers were more likely to have purchased prescription drugs or to have received a psychiatric diagnosis. There were no significant differences between the groups in terms of having their child placed in out of home care, cohabiting with the child after 5 years or receiving long-term income support.
Table 4. Commitments to compulsory care, social situation, social and health outcomes among mothers and children, by type of substance abuse (n = 97/103). Percent and Chi-square test results.
Discussion
This study concerns a small population and a marginal phenomenon, but the data are rich in several ways. First, data refer to the women and their partners, the children that were born, younger siblings, as well as the pregnancies as such. Second, the data include several points of observation (before and during pregnancy, at birth, and a 5-year follow-up period). Third, the type and source of data are diverse, including variables pertaining to health, social situation and substance abuse from client records and several national registers. From the variety of descriptions and findings, it is particularly worth mentioning the following:
The cohort of women in this study show a high level of social and health problems, both at the outset and during the follow-up period. In comparison to the national population of women who gave birth in 2005,3 these women were somewhat younger (for primaparas the difference was almost 3 years), and were marked by manifest social and health problems in several life areas. Almost all pregnant women in the population are cohabiting with the father in early pregnancy, but the corresponding rate in this group was around four in 10. Moreover, less than a third of these women had completed upper secondary education, compared to 84% in the population. Although relatively few women were living with the child’s father, most of them did have partners, who were commonly also substance abusers. In addition, it is worth noting the dramatic difference between the group and the population in smoking rates. The great majority of the women in the cohort smoked before and in early pregnancy (82 and 74%, respectively). Among pregnant women in the population at large, one in five smoked 3 months before pregnancy but only 8% at the first antenatal visit.
The severe abuse of substances, which defines the group, is as such a major health (and social) problem. Despite their relatively young age, almost half of the women had been committed to compulsory care for substance abuse previously and 16% had been subject to compulsory youth care. All in all these are indicators of a precarious social situation and socio-economic marginalisation.
With the sample being small to begin with is was not possible to make any elaborate analyses of inter-group differences. However, there were some interesting findings relating to type of substance abuse. In general, clients in compulsory care fall into two main categories; younger clients with narcotics as drugs of preference (commonly also injecting drugs) and older clients where alcohol and benzodiazepines/sedatives are the drugs of preference. The difference between the AD and DD groups in terms of purchase of prescription drugs may very well reflect this general difference, which may again be associated with the difference in rates of psychiatric diagnoses in the follow-up period (higher in the AD group). High rates of comorbidity in clinical populations are well known but it is possible that type of substance abuse reflects varying degrees of mental health problems – not only among pregnant substance abusers but among substance abusers in general. also reveals that previous commitments to compulsory care were more common in the DD group, which probably reflects a lower threshold for intervening if a person uses (illicit) drugs compared with a person who mainly uses alcohol and/or prescription drugs.
As far as the deliveries and newborn children are concerned, there were also several notable differences compared with the corresponding national population: The rate of Cesarean deliveries was higher, average birth weight almost 350 g lower and 15.4% weighed under 2500 g compared with 4.3% in the population. Furthermore, the rates of prematurely born children and children small for their gestational age were higher. Not surprisingly, the share of children born with affects from maternal substance abuse was very much higher than that in the general population. From one perspective, it is worth pointing out the average birth weight was – after all – over 3 kilograms, that most of the children were not born prematurely or diagnosed as affected by maternal substance abuse. On the other hand, relative to the population of newborns, it is evident that these children did face a more difficult start in life according to traditional obstetrical measures.
In their qualitative study of pregnant women in compulsory care in Norway, Myra et al. (Citation2016) reveal how the ultrasound check represented a turning point in terms of change of perspective and mental preparation for parenthood. This may also have been the case for the women in this study, but based on the available quantitative indicators it is fair to say that becoming mothers (again) did not generally represent a turning point in life conditions. Above all, five women died within these 5 years. This mortality rate is far higher than in comparable segments of the population. Indicators of continued substance abuse and mental health problems did not point in the direction of ‘turning point’ – overall, a vast majority of women showed signs of continued mental health problems as well as alcohol- or drug-related mental and behavioural problems. These findings, both at the outset and during follow-up, confirm the strong comorbidity between substance abuse and mental health problems recognised in many clinical studies (Brunette, Mueser, & Drake, Citation2004; Watkins et al., Citation2004).
None of the children died during the follow-up period. However, as in a similar Finnish study (Holmila et al., Citation2013), the rate of placements of children in out-of-home care was high – 85% and almost half among eventual younger siblings. This could easily be defined as a negative outcome, but may also be seen as a reflection of societal readiness to intervene given that growing up with one or more substance abusing parents exposes children to a number of social and health risks, including injuries and accidents (Raitasalo & Holmila, Citation2017). The relatively short follow-up period is a limitation, although, particularly when it comes to the children as cognitive, emotional, and social problems for example tend to become more evident when children get to school age. Another limitation is the choice of outcome measures, which was restricted by availability of indicators that do not necessarily reflect broader well-being and life conditions. Furthermore, we have no knowledge about the role of the fathers apart from the fact that many fathers/partners were also abusing substances at the time the mother was committed to care.
The question of harmful use of alcohol and other drugs in connection with pregnancy potentially concerns all women of childbearing age. Within this large population group a smaller, but often non-negligible, proportion may be defined as at risk consumers of substances – mainly alcohol (Göransson, Magnusson, Bergman, Rydberg, & Heilig, Citation2003; Nayak & Kaskutas, Citation2004). This study concerns an even more select sub-group, consisting of women with a manifest and severe abuse of any or all types of psychoactive substances. This group is bound to be comparatively small in most societies and in a small country like Sweden also limited in absolute numbers. The entire population in this study did not consist of more than some 100 mother–child dyads. On the other hand, the study includes the entirety of a well-defined population and is based on comprehensive register data which other follow-up studies often lack. As with any clinical population, it is possible to argue that the findings only apply to that particular context. The overall conclusions from this study are, however, likely to be relevant for a larger population of pregnant women who severely misuse psychoactive substances. For example, the results confirm that pregnant substance abusers commonly present a complexity of social and health problems (Anderson et al., Citation1997; Crome et al., Citation2005), including a multifaceted consumption of substances (Crome et al., Citation2005; Delano, Gareri, & Koren, Citation2013; Kelly et al., Citation2017).
Implications
The results of this study have implications along several dimensions. At the health and social policy level, the findings challenge the prospects of designing evidence based policies or interventions, at least from a narrow understanding of ‘evidence’. The political and popular debate on substance abuse and pregnancy commonly focuses on the effects of alcohol and on identifying general harmful levels of consumption for alcohol. From a public health perspective, with alcohol being the most widespread drug, this is understandable. However, in a clinical sample such as this one, alcohol as the primary or only preferred drug is rare. Therefore, policy makers – and researchers – are probably wise to avoid putting too much effort into attempts at identifying harmful – and thereby harmless – levels of consumption. This is simply not possible in a group characterised by so many problematic circumstances (low income, single parenthood, low education level, unstable family relations) – in addition to harmful consumption of a multitude of drugs.
Having said that, there is good reason to address the excessive smoking rates in clinical contexts. Many studies have shown elevated smoking rates in high-risk groups (Crome et al., Citation2005) and, the need for efforts to reduce smoking should therefore not be underestimated (Havens, Simmons, Shannon, & Hansen, Citation2009). Smoking rates in the study group were extremely high, compared with other expecting mothers – but information about smoking was at the time not even recorded systematically in client records at the NBIC.
From a service system perspective, the need for coordinated, comprehensive and longstanding support for women who are not only high risk but have a manifest severe substance abuse is clear. This also means that the definition of ‘substance abuse treatment’ or services must be broad. As substance abusers and as mothers, these women are often recipients or subject to a number of societal interventions – and are in contact with many agencies (somatic and mental health care, employment office, social services, child protection services, housing office, etc.). The need for coordination of services is obvious. Clinicians need to consider the entire life situation of the woman (and child) and plan for long-term support and care. The likely presence of substance abusing partners is another complicating factor that needs to be taken into consideration, not least which role the partner is expected or expects to have in relation to the child. Clinicians must also balance encouragement and empowerment of the woman as a mother (to be) with sound realism – becoming a parent is not a recommendable ‘treatment’. Future research and service interventions would, then, be helped by prospective, longitudinal qualitative and quantitative studies of the entire families and all service providers’ contributions at different stages.
With a study population such as this one it is obviously easiest, and most relevant, to focus on the many problems and challenges in these women’s and children’s lives. Still, it is also important to emphasise the potential resources and capacities of both women, children and welfare services. These women were, despite their life circumstance, actually able to become pregnant in the first place and to give birth to live born children whose average birth weight was indeed lower than the national average but still over 3 kg.
Conclusions
Pregnant substance abusers show severe social and health problems in many life areas, including polydrug abuse and elevated smoking rates. Overall, becoming parents did not represent a turning point in the lives of the mothers. Most women showed indications of continued mental and health problems related to substance abuse, as well as high mortality rates. Most children were placed in out-of-home care at least once and relatively few were living together at follow-up. All children survived but they faced several social and health disadvantages at birth. However, a longer follow-up period is necessary to assess the long-term outcomes for the children properly.
Acknowledgements
The study was approved by the Regional Ethical Review Board in Stockholm. The study was greatly facilitated by Mikaela Persson, MA, who prepared the complex dataset for analysis. Two anonymous reviewers provided extremely helpful comments.
Disclosure statement
No potential conflict of interest was reported by the author.
Notes
Additional information
Funding
Notes
1 In line with recent changes in DSM-V, the preferred term is now people with substance use disorder. This study is, however, based on data from a period where substance abuse was the “going term”. More importantly – the women in this study are placed in compulsory care according to social welfare legislation, which does not imply the presence of any formal diagnosis. It would therefore be misleading to refer to the clients as persons with substance use disorders, implying that they actually have been diagnosed as such.
2 This does not, however, include an unborn child.
3 This year was chosen for comparison as it is the in the middle of the period from which the study group was chosen (2000–2009).
References
- Anderson, M., Elk, R., & Andres, R.L. (1997). Social, ethical and practical aspects of perinatal substance use. Journal of Substance Abuse Treatment, 14, 481–486. doi: 10.1016/S0740-5472(96)00152-3
- Bauer, C.R., Lambert, B.L., Bann, C.M., Lester, B.M., Shankaran, S., Bada, H.S., … Higgins, R.D. (2011). Long-term impact of maternal substance use during pregnancy and extrauterine environmental adversity: Stress hormone levels of preadolescent children. Pediatric Research, 70, 213–219. doi: 10.1038/pr.2011.438
- Brunette, M.F., Mueser, K.T., & Drake, R.E. (2004). A review of research on residential programs for people with severe mental illness and co-occurring substance use disorders. Drug and Alcohol Review, 23, 471–481. doi: 10.1080/09595230412331324590
- Cave, E. (2007). Drink and drugs in pregnancy: Can the law prevent avoidable harm to the future child? Medical Law International, 8, 165–187. doi: 10.1177/096853320700800203
- Crome, I., Ismail, K.M.K., Ghetau, E., McAuley, R., Bloor, R., Jones, P., & O'Brien, P.M.S. (2005). Opiate misuse in pregnancy: Findings of a retrospective case note series. Drugs: Education, Prevention and Policy, 12, 431–436. doi: 10.1080/09687630500241695
- Delano, K., Gareri, J., & Koren, G. (2013). Rates of fetal polydrug exposures in methadone-maintained pregnancies from a high-risk population. PLoS One, 8, 1. doi: 10.1371/journal.pone.0082647
- Della Grotta, S., LaGasse, L.L., Arria, A.M., Derauf, C., Grant, P., Smith, L.M., … Lester, B.M. (2010). Patterns of methamphetamine use during pregnancy: Results from the Infant Development, Environment, and Lifestyle (IDEAL) Study. Maternal and Child Health Journal, 14, 519–527. doi: 10.1007/s10995-009-0491-0
- European Commission. (2006). An EU strategy to support Member States in reducing alcohol related harm. Brussels: Communication from the Commission to the Council, the European Parliament, the European Economic and Social Committee and the Committee of the regions.
- Finnegan, L., Winklbaur, B., Fischer, G., Olofsson, M., & Welle-Strand, G. (2009). New approaches in the treatment of opioid dependency during the pregnancy. Heroin Addiction and Related Clinical Problems, 11, 47–57.
- Gibbs, A., & Sherwood, K. (2017). Putting fetal alcohol spectrum disorder (FASD) on the map in New Zealand: A review of health, social, political, justice and cultural developments. Psychiatry, Psychology and Law, 24, 825–842. doi: 10.1080/13218719.2017.1315784
- Göransson, M., Magnusson, Å., Bergman, H., Rydberg, U., & Heilig, M. (2003). Fetus at risk: Prevalence of alcohol consumption during pregnancy estimated with a simple screening method in Swedish antenatal clinics. Addiction, 98, 1513–1520. doi: 10.1046/j.1360-0443.2003.00498.x
- Hartman, D.M., & Golub, A. (1999). The social construction of the crack epidemic in the print media. Journal of Psychoactive Drugs, 31, 423–433. doi: 10.1080/02791072.1999.10471772
- Havens, J.R., Simmons, L.A., Shannon, L.M., & Hansen, W.F. (2009). Factors associated with substance use during pregnancy: Results from a national sample. Drug and Alcohol Dependence, 99, 89–95. doi: https://doi.org/10.1016/j.drugalcdep.2008.07.01010.1016/j.drugalcdep.2008.07.010
- Higgins, P.G., Clough, D.H., & Wallerstedt, C. (1995). Drug-taking behaviours of pregnant substance abusers in treatment. Journal of Advanced Nursing, 22, 425–432. doi: 10.1046/j.1365-2648.1995.22030425
- Hjerkinn, B., Rosvold, E.O., & Lindbaek, M. (2009). Neonatal findings among children of substance-abusing women attending a special child welfare clinic in Norway. Scandinavian Journal of Public Health, 37, 751–757. doi: 10.1177/1403494809342310
- Holmila, M., Raitasalo, K., & Kosola, M. (2013). Mothers who abuse alcohol and drugs: Health and social harms among substance-abusing mothers of small children in three child cohorts. Nordic Studies on Alcohol and Drugs, 30, 361–373. doi: 10.2478/nsad-2013-0030
- Hoppe, R. (2005). Rethinking the science-policy nexus: From knowledge utilization and science technology studies to types of boundary arrangements. Poiesis and Praxis, 3, 199–215. doi: 10.1007/s10202-005-0074-0
- International Center for Alcohol Policies. (1999). Government policies on alcohol and pregnancy. ICAP Report 6. Journal of Substance Use, 4, 216–219. doi: 10.3109/14659899909053031
- Kahila, H., Gissler, M., Sarkola, T., Autti-Ramo, I., & Halmesmaki, E. (2010). Maternal welfare, morbidity and mortality 6–15 years after a pregnancy complicated by alcohol and substance abuse A register-based case–control follow-up study of 524 women. Drug and Alcohol Dependence, 111, 215–221. doi: 10.1016/j.drugalcdep.2010.04.014
- Kelly, P.J., Robinson, L.D., Baker, A.L., Deane, F.P., McKetin, R., Hudson, S., & Keane, C. (2017). Polysubstance use in treatment seekers who inject amphetamine: Drug use profiles, injecting practices and quality of life. Addictive Behaviors, 71, 25–30. doi: http://dx.doi.org/10.1016/j.addbeh.2017.02.006
- Kissin, W.B., Svikis, D.S., Morgan, G.D., & Haug, N.A. (2001). Characterizing pregnant drug-dependent women in treatment and their children. Journal of Substance Abuse Treatment, 21, 27–34. doi: 10.1016/S0740-5472(01)00176-3
- Legg, S. (2005). Foucault's population geographies: classifications, biopolitics and governmental spaces. Population, Space and Place, 11, 137–156. doi: 10.1002/psp.357
- Leppo, A. (2012). The emergence of the foetus: Discourses on foetal alcohol syndrome prevention and compulsory treatment in Finland. Critical Public Health, 22, 179–191. doi: 10.1080/09581596.2011.619518
- Leppo, A., & Hecksher, D. (2011). The rise of the total abstinence model. Recommendations regarding alcohol use during pregnancy in Finland and Denmark. Nordic Studies on Alcohol and Drugs, 28, 7–27. doi: 10.2478/v10199-011-0002-7
- Lester, B.M., Andreozzi, L., & Appiah, L. (2004). Substance use during pregnancy: Time for policy to catch up with research. Harm Reduction Journal, 1, 5. doi: 10.1186/1477-7517-1-5
- Lund, I.O., Skurtveit, S., Engeland, A., Furu, K., Ravndal, E., & Handal, M. (2013). Prescription drug use among pregnant women in opioid maintenance treatment. Addiction, 108, 367–376. doi: 10.1111/j.1360-0443.2012.04049
- Lund, I.O., Skurtveit, S., Sarfi, M., Bakstad, B., Welle-Strand, G., & Ravndal, E. (2012). Substance use during and after pregnancy among a national cohort of pregnant women in opioid maintenance treatment and their partners. Journal of Substance Use, 17, 277–286. doi: 10.3109/14659891.2011.580415
- Lund, I.O., Skurtveit, S., Sarfi, M., Bakstad, B., Welle-Strand, G., & Ravndal, E. (2013). A 2-year prospective study of psychological distress among a national cohort of pregnant women in opioid maintenance treatment and their partners. Journal of Substance Use, 18, 148–160. doi: 10.3109/14659891.2011.642928
- Moe, V. (2002). Foster-placed and adopted children exposed in utero to opiates and other substances: Prediction and outcome at four and a half years. Journal of Developmental and Behavioral Pediatrics, 23, 330–339. doi: 10.1097/00004703-200210000-00006
- Myra, S.M., Ravndal, E., Wie, V.T., & Wiig, E.M. (2016). Pregnant substance-abusing women in involuntary treatment: Attachment experiences with the unborn child. Nordic Studies on Alcohol and Drugs, 33, 299–313. doi: 10.1515/nsad-2016-0023
- National Board of Health and Welfare. (2003). The Swedish Medical Birth Register. A Summary of Content and Quality. Retrieved from www.socialstyrelsen.se/Lists/Artikelkatalog/Attachments/10655/2003-112-3_20031123.pdf
- Nayak, M.B., & Kaskutas, L.A. (2004). Risky drinking and alcohol use patterns in a national sample of women of childbearing age. Addiction, 99, 1393–1402. doi: 10.1111/j.1360-0443.2004.00840.x
- Raitasalo, K., & Holmila, M. (2017). Parental substance abuse and risks to children’s safety, health and psychological development. Drugs: Education, Prevention and Policy, 24, 17–22. doi: 10.1080/09687637.2016.1232371
- Raitasalo, K., Holmila, M., Autti-Ramo, I., Martikainen, J.E., Sorvala, V.M., & Makela, P. (2015). Benzodiazepine use among mothers of small children: A register-based cohort study. Addiction, 110, 636–643. doi: 10.1111/add.12808
- Raitasalo, K., Holmila, M., Autti-Ramo, I., Notkola, I.L., & Tapanainen, H. (2015). Hospitalisations and out-of-home placements of children of substance-abusing mothers: A register-based cohort study. Drug and Alcohol Review, 34, 38–45. doi: 10.1111/dar.12121
- Reitan, T. (2011). Pregnant drug users in Swedish compulsory treatment. Nordic Studies on Alcohol and Drugs, 28, 211–233. doi: 10.2478/v10199-011-0021-4
- Reitan, T. (2016). Commitment without confinement. Outpatient compulsory care for substance abuse, and severe mental disorder in Sweden. International Journal of Law and Psychiatry, 45, 60–69. doi: 10.1016/j.ijlp.2016.02.011
- Reitan, T., & Weding, L. (2012). Gravida missbrukare inom LVM-vården [Pregnant substance abusers in compulsory care]. Report no 9. Stockholm: National Board of Institutional Care. Retrieved from https://www.stat-inst.se/contentassets/c3223a55a2704649a7ec335d72bcd736/gravida-missbrukare-inom-lvm-varden.pdf
- Room, R., Ferris, J., Laslett, A.M., Livingston, M., Mugavin, J., & Wilkinson, C. (2010). The drinker's effect on the social environment: A conceptual framework for studying alcohol's harm to others. International Journal of Environmental Research and Public Health, 7, 1855–1871. doi: 10.3390/ijerph7041855
- Sarkola, T., Gissler, M., Kahila, H., Autti-Ramo, I., & Halmesmaki, E. (2012). Alcohol and substance abuse identified during pregnancy: Maternal morbidity, child morbidity and welfare interventions. Acta Paediatrica, 101, 784–790. doi: 10.1111/j.1651-2227.2012.02670
- Shankaran, S., Lester, B.M., Das, A., Bauer, C.R., Bada, H.S., Lagasse, L., & Higgins, R. (2007). Impact of maternal substance use during pregnancy on childhood outcome. Seminars in Fetal & Neonatal Medicine, 12, 143–150. doi: 10.1016/j.siny.2007.01.002
- Stenius, K. (2009). Ogenomtänkta förslag om tvångsvård av gravida missbrukare. (Ill-considered proposals of compulsory care for pregnant substance abusers). Editorial. Nordic Studies on Alcohol and Drugs, 26, 241–242. doi: 10.1177/145507250902600301
- Stogner, J. (2010). The war on whisky in the womb: Assessing the merit of challenges to statutes restricting the alcohol intake of pregnant women. Rutgers Journal of Law & Public Policy, 7, 259–288.
- Söderström, K., & Skolbekken, J.-A. (2012). Pregnancy and substance use – the Norwegian § 10-3 solution. Ethical and clinical reflections related to incarceration of pregnant women to protect the foetus from harmful substances. Nordic Studies on Alcohol and Drugs, 29, 155–171. doi: 10.2478/v10199-012-0011-1
- Teruya, C., & Hser, Y.-I. (2010). Turning points in the life course: Current findings and future directions in drug use research. Current Drug Abuse Reviews, 3, 189–195. doi: 10.2174/1874473711003030189
- Walton-Moss, B.J., McIntosh, L.C., Conrad, J., & Kiefer, E. (2009). Health status and birth outcomes among pregnant women in substance abuse treatment. Womens Health Issues, 19, 167–175. doi: 10.1016/j.whi.2009.02.003
- Watkins, K.E., Hunter, S.B., Wenzel, S.L., Tu, W., Paddock, S.M., Griffin, A., & Ebener, P. (2004). Prevalence and characteristics of clients with co-occurring disorders in outpatient substance abuse treatment. American Journal of Drug and Alcohol Abuse, 30, 749–764. doi: 10.1081/ADA-200037538
- Weir, L. (2006). Pregnancy, risk and biopolitics: On the threshold of the living subject. New York: Taylor & Francis.
- Wilder, C., Lewis, D., & Winhusen, T. (2015). Medication assisted treatment discontinuation in pregnant and postpartum women with opioid use disorder. Drug and Alcohol Dependence, 149, 225–231. doi: 10.1016/j.drugalcdep.2015.02.012
- World Health Organization (WHO). (2010). International statistical classification of diseases and related health problems. 10th Rev ed. Geneva: World Health Organization.
- World Health Organization (WHO). (2014). Guidelines for identification and management of substance use and substance use disorders in pregnancy. Geneva: World Health Organization.
- WHOCC. (2013). Guidelines for ACT classification and DDD assignment. 16th ed. Oslo: WHO Collaborating Centre for Drug Statistics Methodology, Norwegian Institute of Public Health.