Abstract
This study examined how psychedelics reduced symptoms of racial trauma among black, indigenous, and people of color (BIPOC) subsequent to an experience of racism. A cross-sectional internet-based survey included questions about experiences with racism, mental health symptoms, and acute and enduring psychedelic effects. Changes in mental health were assessed by retrospective report of symptoms in the 30 days before and 30 days after an experience with psilocybin, Lysergic acid diethylamide (LSD), or 3,4-Methylenedioxymethamphetamine (MDMA). We recruited 313 diverse BIPOC in the US and Canada. Results revealed a significant (p < .001) and moderate (d = −.45) reduction in traumatic stress symptoms from before-to-after the psychedelic experience. Similarly, participants reported decreases in depression (p < .001; d = −.52), anxiety (p < .001; d = −.53), and stress (p < .001; d = −.32). There was also a significant relationship (Rc = 0.52, p < .001) between the dimension of acute psychedelic effects (mystical-type, insight, and challenging experiences) and decreases in a cluster of subsequent psychopathology (traumatic stress, depression, anxiety, and stress), while controlling for the frequency of prior discrimination and the time since the psychedelic experience. BIPOC have been underrepresented in psychedelic studies. Psychedelics may decrease the negative impact of racial trauma. Future studies should examine the efficacy of psychedelic-assisted therapy for individuals with a history of race-based trauma.
Introduction
The traumatizing impact of racism in people of color
Trauma and stress related disorders are a mental health consequence of experiencing a traumatic event (APA, Citation2013). One form of trauma that has been underrepresented in the empirical literature is racial trauma, also called race-based trauma, which may include symptoms of traumatic stress, anxiety, and depression (Carter, Citation2007; Williams, Metzger, et al., Citation2018). Racial trauma is defined as traumatization due to distressing experiences that can include physical or psychological threats to oneself or witnessing such threats to another based on race or ethnicity (Williams, Metzger, et al., Citation2018). Racial trauma is prevalent among black, indigenous, and people of color (BIPOC). According to the US Department of Justice (DOJ), Black Americans (63%), Latinx Americans (47%), Asian Americans (6%), American Indians or Alaska Natives (5%), and multiracial individuals (4%) have experienced some form of racially charged trauma in their lifetime (Department of Justice, Citation2014). Although the prevalence of racial trauma specifically by racial/ethnic group is not available at the population level for Canadians, national epidemiological survey data indicates that 7% of adult Canadians reported experiencing racial discrimination during their lifetime, of these 79% reported racial discrimination was the main or only type of discrimination they experienced, and Canadians of color (Indigenous, Black, Asian, Southwest Asian, Arab, Latinx, other, and multiracial) were 74% more likely than White Canadians to report racial discrimination (Godley, Citation2018). Further, historical and cultural traumas may contribute to the experience of racial trauma, such as the impact of colonialization on Indigenous Peoples (Gone et al., Citation2019).
Causes of racial trauma
Racial trauma is rarely caused by a discreet single event, but is the culmination of many discriminatory experiences, thus few studies have investigated this type of trauma in the context of prevalence and treatment of post-traumatic stress disorder (PTSD) (Carter, Citation2007; Williams, Printz, Ching, et al., Citation2018). Further, individuals whose PTSD is caused by racial trauma are likely to encounter barriers to effective mental health care due to systematic disparities (Williams et al., Citation2014). Even when treatments are accessed in this population, they may be limited in efficacy and adherence, highlighting the importance of research examining novel therapies for BIPOC (Lester et al., Citation2010; Zoellner et al., Citation1999).
When exploring the causes of racial trauma, both overt and covert racism have been shown to contribute to trauma symptoms (Williams, Printz, & DeLapp, Citation2018). This includes the expression of colorblind ideology, which may be expressed as well-meaning sentiments endorsed in interpersonal interactions that may be patronizing or exclusionary and can have far-reaching deleterious effects on racial and ethnic minorities (Terwilliger et al., Citation2013; Williams, Citation2020a). Colorblind sentiments include statements such as “We’re all one race, the human race,” yet effectively enables White individuals to ignore the realities of White privilege, White supremacy, and racial/ethnic disparities (Mueller, 2017), which further creates pressure on minority individuals to assimilate into the majority culture (Apfelbaum et al., Citation2008; Liu et al., Citation2019). Although colorblind ideology may be a well-intended strategy utilized to counter pervasive pathological stereotypes about BIPOC (Williams et al., Citation2012), both colorblindness and stereotypes contribute to subtle expressions of racism known as microaggressions (Pierce, Citation1970; Williams, Citation2020a). Microaggressions are prejudicial messages expressed via seemingly harmless actions (Sue et al., Citation2007), such as dismissive looks, questions about a minority individual’s place of origin, and compliments based on an individual’s adherence or defiance of stereotypes. Prior research studies have demonstrated that microaggressions are empirically associated with a number of negative physical and psychological health outcomes, including suicidality (Huynh, Citation2012; O’Keefe et al., Citation2015; Williams, Citation2020b). Finally, media dissemination of police violence against BIPOC can also contribute to a sense of racial traumatization and has been shown to result in measurable psychiatric disability in communities of color (Bor et al., Citation2018).
Taken together, racial discrimination experiences have deleterious effects on mental health. For example, in a systematic review of 121 studies, nearly half of these studies found consistent negative effects of racial discrimination on mental health (Desalu et al., Citation2019; Pascoe and Smart Richman, Citation2009; Priest et al., Citation2013). Approximately three-quarters (76%) of examined outcomes were significantly associated with reported experiences of racial discrimination. Similarly, data from large survey studies have found that everyday experiences of racial discrimination were linked to depression, anxiety, and problematic substance use (Clark et al., Citation2015; Soto et al., Citation2011). Yet another study found that both overt and subtle racial discrimination was a significant predictor of trauma symptoms (Williams, Printz, & DeLapp, Citation2018) and ongoing racial discrimination contributed to cumulative effects that may lead to the development of PTSD symptoms or a PTSD diagnosis (Bryant-Davis & Ocampo, Citation2006; Butts, Citation2002; Williams et al., Citation2014).
Treatment of racial trauma
Several treatments have been developed for PTSD. For example, Prolonged Exposure (PE; Foa et al., Citation1991) has been shown to have a large effect on decreasing PTSD symptoms, however, existing studies of this treatment do not address the role of race or ethnicity (Powers et al., Citation2010). Similarly, Cognitive Processing Therapy (CPT) is an effective treatment for PTSD, but race is not accounted for as a moderator in outcome analyses (Asmundson et al., Citation2019). Evidence also shows that dropout rates are high among BIPOC who receive these treatments (Cloitre, Citation2009; Schottenbauer et al., Citation2008). Finally, almost no BIPOC have been included in any studies of Eye Movement Desensitization and Reprocessing (EMDR), thus failing to provide data on its generalizability in helping people with racial traumas (Kusch et al., Citation2017). Although several studies have shown that existing treatments may be effective for reducing PTSD symptoms among BIPOC, the development of treatments for racial trauma are sorely lacking.
Aside from clinically based treatments, BIPOC may also use substances to cope with the sequalae of racial trauma (Gerrard et al., Citation2012; Hurd et al., Citation2014), especially if they do not have access to empirically-supported treatments or when those treatments are not effective. Although many substances can exacerbate existing mental health problems, the use of psychedelics has been associated with less psychological distress (Johansen & Krebs, Citation2015), and in fact many people report lasting benefits. Research has shown that the administration of psychedelics in naturalistic settings is associated with reductions in mental health conditions. For example, in a 5-methoxy-N,N-dimethyltryptamine (5-MeO-DMT) study, 80% of those with depression and 79% of those with anxiety reported improvement in symptoms. Compared to those who did not see improvements, those who experienced improvements reported a greater intensity of mystical-type experiences and greater spiritual significance and personal meaning of the experience (Davis, et al., Citation2019). Similar findings were found for PTSD symptom reduction, with 79% of those with PTSD experiencing improvements, and those who experienced improvements reporting greater spiritual significance and personal meaning of their experience (Cox et al., Citation2018).
There are no studies to date documenting the results of using psychedelics for racial trauma. However, Argento et al. (Citation2018) studied the moderating effect of psychedelics on illicit drug use and suicide risk among marginalized women (sex workers in Canada, where 35% reported indigenous ancestry), and found that naturalistic use of psychedelics served as a protective factor on the association between illicit drug use and risk of suicide.
Psychedelic-assisted therapy for mental health
One area of emerging research has been testing the efficacy of novel pharmacologically assisted therapies for the treatment of trauma, depression, and anxiety in clinical settings. For example, two clinical trials of psilocybin administered as an adjunct to therapy showed that this treatment decreased depression and anxiety symptoms among chronically ill cancer patients and that positive outcomes lasted for up to six months following a single dose (Griffiths et al., Citation2016; Johnson & Griffiths, Citation2017; Ross et al., Citation2016). Similarly, two studies with a population of individuals with depression and treatment-resistant depression showed decreased depression and anxiety after two doses of psilocybin in the context of supportive psychotherapy (Carhart-Harris et al., Citation2016; Davis et al., Citation2020). Specific to PTSD treatment, 3,4-Methylenedioxy-methamphetamine (MDMA) has been examined as an adjunct to therapy among people with treatment-resistant PTSD (Mithoefer et al., Citation2018; Ot’alora et al., Citation2018), demonstrating that this treatment led to a reduction in PTSD symptoms, as well as decreases in depression and other related symptoms. Furthermore, a meta-analytic comparison of MDMA-assisted psychotherapy compared to PE found MDMA to be significantly more effective based on both clinician reports and self-reports of PTSD symptoms, with lower attrition rates for MDMA (13%) than PE (27%; Amoroso & Workman, Citation2016). Finally, a study showed the effectiveness of ayahuasca resulting in significant decreases in depression scores among a sample of individuals with recurrent depression (Sanches et al., Citation2016).
Although these recent trials have found positive effects of psychedelic-assisted therapy on mental health outcomes, these trials are small and have lacked inclusion of BIPOC. For example, a literature review found that out of 18 studies on psychedelic-assisted therapy worldwide, the large majority of participants were non-Hispanic White (82%) with low percentages of BIPOC, (3% Black; 2% Latinx, 2% Asian, 5% Indigenous; 5% mixed race; 2% “other,” and 8% unknown; Michaels et al., Citation2018). Although the lack of representativeness in these studies could be related to a variety of factors (e.g. the lack of cultural inclusivity fostered by the research community, mental illness stigma, access to treatment, recruitment methods, differing attitudes towards psychedelic use based on country and cultural norms), the lack of BIPOC in these studies substantially limits the generalizability of the findings.
Purpose of this study
Given the paucity of research focusing on healing for BIPOC who have experienced racial trauma, the lack of representation of BIPOC in psychedelic research, and the lack of BIPOC in the broader literature on psychedelic use in general, the present study aims to address these gaps by exploring how non-clinical samples use and experience psychedelics in the natural ecology, particularly after experiencing racial trauma. Our research questions are (1) is psychedelic use in the natural environment associated with a reduction in mental health symptoms among BIPOC who have experienced racial trauma, and (2) what factors contribute to reductions in mental health symptoms among those who experience benefit from naturalistic psychedelic use? This is the first study to examine symptoms of traumatic stress, depression, and anxiety among those who have experienced racial trauma and whether the intensity of such symptoms can change after using psychedelics. Furthermore, this study will explore possible mechanisms by which psychedelics may be associated with changes in symptomology.
Methods
Procedures and participants
This study is a cross-sectional, observational study of BIPOC who have experienced racial trauma and used psychedelics in non-clinical settings. Participants were recruited through Qualtrics survey research panels, and all data were provided anonymously. Potential participants were screened for inclusion. Criteria for the study inclusion were: 1) at least 18 years old, 2) able to read, write, and speak English fluently, 3) had taken a dose of a classic psychedelic (e.g. psilocybin mushrooms, LSD, ayahuasca, mescaline, DMT, 5-MeO-DMT, etc.) that produced moderate to strong psychoactive effects, 4) after taking the substance they had an experience they believed contributed to “relief from the challenging effects of ethnic discrimination,” and 5) they currently reside in the United States or Canada). Our inclusion criteria also included only BIPOC as racial trauma is a necessary precursor to ethnic discrimination, therefore participants were required to identify as Black, Asian, Latinx, or Native/Indigenous heritage for inclusion. Following screening, potential participants were presented with the informed consent document and then continued on in the secure online survey and completed the questionnaires. Once enrolled in the study, participants were asked to report on past experiences with racial trauma, psychedelic use, and mental health symptoms. Furthermore, participants were asked to recall a memorable psychedelic experience and provided details about this psychedelic experience, including the acute and enduring effects.
Qualtrics provides an incentive to their research participant panels for their time completing the survey. Specifically, the participants were compensated as per pre-agreed rates determined within their role on the Qualtrics panel. Qualtrics participants receive an incentive based on the length of the survey, their specific panelist profile and target acquisition difficulty. The specific type of rewards varied and may have included cash, airline miles, gift cards, redeemable points, sweepstakes entrance or vouchers. This research study was approved by the Ohio State University Institutional Review Board, and all participants agreed to an approved informed consent page before proceeding with the survey (available upon request).
Recruitment for this study occurred during September 2019. A total of 26,710 advertisements were sent from Qualtrics to members of their research panels. These advertisements resulted in 5,534 clicks to the survey screening and informed consent document. Of those who clicked the secure weblink, 3,253 did not meet eligibility for the study. Of the remaining 2,281 who were eligible and consented to participate, a total of 824 went on to complete study questionnaires. Among the 824 who completed the survey, 274 were identified by Qualtrics as being a “poor responder” which included participants who completed the survey too quickly and those that passed screening but later revealed responses to items that should have excluded them from participation (e.g. revealed in demographics form that they were “White” despite this being an exclusion criterion). Qualtrics then provided a sample of 550 participants to the investigator for further evaluation of data quality. Further examination of participant responses revealed that additional 22 participants should be excluded (i.e. not passing “bot” detection = 12, potentially duplicate identifiers = 3, did not provide country of residence = 2, did not provide an answer to which psychedelic drug consumed = 4, no response to primary outcome measures = 1). An additional 121 participants were removed because of a review of their responses revealed indications of poor or inconsistent responding that contributed to data with questionable validity. Lastly, we removed 94 participants who reported use of mescaline/peyote, dimethyltryptamine/ayahuasca, and iboga/ibogaine to more precisely attribute outcomes in the study to the effects of more commonly used psychedelics (e.g. psilocybin, LSD, and MDMA). Thus, the final sample comprised 313 participants.
Measures
Participant demographics were collected for age, gender, race, ethnicity, nationality, income, level of education, and marital status. We also collected information about prior psychedelic experiences using an eight-item multiple choice questionnaire that was designed for this study to assess the type of psychedelic substance used (11 options), memory of the experience, and subjective dose (low, moderate, moderately high, high).
General ethnic discrimination scale
(GEDS; Landrine et al., Citation2006). This measure was designed to evaluate the frequency and severity of discrimination in education, employment, legal, healthcare, or community settings due to one’s race/ethnicity. It includes 17 multi-part questions wherein participants are asked to rate the frequency of a specific discrimination experience on a 6-point scale ranging from 1 (Never) to 6 (Almost all the time), and then rate the severity of their stress due to each experience on a 5-point scale ranging from 0 (Not at all stressful) to 4 (Extremely stressful). The sections are scored separately to provide a frequency and a stress score. We modified the instructions to prompt participants to report how often each experience of ethnic discrimination happened prior to the psychedelic experience. For this study, a frequency score was used. Internal consistency of the frequency scale was excellent (α= .95).
Psychological insight questionnaire
(PIQ; Davis et al., Citation2020; Davis et al., Citationin press). The 23-item PIQ was included in the study to assess participants’ insights had during the psychedelic experience related to emotions, beliefs, memories, and relationships. Participants were asked to report their insights regarding their psychedelic experience (e.g. “Realized how current feelings or perceptions are related to events from my past”) on a 6-point scale ranging from 0 (No; not at all) to 5 (Extremely/More than ever before in my life). A total scale mean score was used for the primary analyses in this study. Internal consistency reliability of the total scale mean score was excellent (α= .95).
Mystical experience questionnaire
(MEQ; (Barrett et al., Citation2015; MacLean et al, Citation2011). The 30-item MEQ was included in this study to assess participants’ mystical-type experiences that they might have after taking a psychedelic substance. Participants were asked to report their mystical-type experience through questions such as “Loss of your usual sense of time” or “Experience of amazement” on a 6-point scale ranging from 0 (None; not at all) to 5 (Extremely/More than ever before in my life). This scale has been used extensively in prior research and demonstrated excellent internal consistency reliability and predictive validity (Griffiths et al., Citation2011, Citation2016). A total scale mean score was used for the primary analyses in this study. Internal consistency reliability of the total scale mean score was excellent (α= .96).
Challenging experience questionnaire
(CEQ; Barrett et al., Citation2016). This 26-item measure was included to assess challenging experiences related to the psychedelic experience, including feelings of grief, fear, insanity, death, isolation, physical distress, or paranoia. Participants were asked to report challenges they have suffered from their psychedelic experience (e.g. “I felt like crying” or “I felt shaky inside”) on a 6-point scale ranging from 0 (No; not at all) to 5 (Extremely/More than ever before in my life). Prior research demonstrated that the scale has very good internal consistency and external reliability (Barrett et al., Citation2016). A total scale mean score was used for the primary analyses in this study. Internal consistency reliability of the total scale mean score was excellent (α = .97).
Depression anxiety and stress scale
(DASS21; Lovibond & Lovibond, Citation1995). The 21-item scale was included to assess symptoms related to depression, anxiety, and stress in the 30 days before and 30 days after the psychedelic experience. This measure has three subscales that assess depression (DASS21-D, 7 Items; e.g. “I felt downhearted and blue”), anxiety (DASS21-A, 7 Items; e.g. “I felt that I was using a lot of nervous energy”), and stress (DASS21-S, 7 items; e.g. “I found myself getting agitated”) symptoms. Participants were asked to report the frequency at which these symptoms appear in their life on a 4-point scale ranging from 1 (Never) to 4 (Always). Prior studies have demonstrated high internal consistency reliability and similar reliability and validity across racial groups (Norton, Citation2007). A subscale total mean score was used for the primary analyses in this study. We also calculated the average change in symptoms for each subscale by subtracting the total mean score of each “after” measure from the total mean score for the “before” measures. This produced a mean change in depression, anxiety, and stress scores. Internal consistency reliability was: 1) DASS21-D-before subscale (α= .89), 2) DASS21-A-before (α = .82), 3) DASS21-S-before subscale (α = .86), 4) DASS21-D-after subscale (α = .86), 5) DASS21-A-after subscale (α = .83), and 6) DASS21-S-after subscale (α = .87).
Trauma symptoms of discrimination scale
(TSDS; Williams, Printz, & DeLapp, Citation2018). The 21-item scale was included in this study to evaluate participants’ discriminatory distress related to symptoms of trauma. Symptoms were assessed for the 30 days before and 30 days after the psychedelic experience. The measure assessed uncontrollable arousal, feelings of alienation, worries about future negative events, and perceiving others as dangerous. Participants were asked to report the frequency of their experience of discriminatory distress regarding trauma (e.g. “Due to the past experience of discrimination, I often worry too much about different things”) on a 4-point scale ranging from 0 (Never) to 3 (Often). This scale has excellent internal consistency and test-retest reliability and revealed good concurrent validity as it was significantly positively correlated with distress from general ethnic discrimination (Williams, Printz, & DeLapp, Citation2018). A total scale score was used for the primary analyses in this study. We also calculated the average change in trauma symptoms by subtracting the total score of each “after” measure from each total score of the “before” measures. This produced a total mean change in trauma symptoms score. Internal consistency reliability for the total scale score was 1) “before” measure (α = .96) and 2) “after” measure (α = .95).
Data analysis
Descriptive analyses of demographic and background characteristics for all study variables were calculated. Next, a preliminary analysis was conducted using a series of chi-square and one-way ANOVAs to examine whether there were differences in study variables (e.g. demographics, psychedelic experiences, acute psychedelic effects, ethnic discrimination experiences, and changes in discrimination-related trauma, depression, anxiety, and stress symptoms) as a function of the type of psychedelic drug (e.g. psilocybin, LSD, MDMA) participants consumed. Experiences of discrimination were assessed by examining the frequency of various experiences as reported on the GEDS-Frequency scale.
Next, the primary study aim was evaluated by conducting a canonical correlation analysis (CCA; Tabachnick & Fidell, Citation2007). CCA was chosen because it is a form of multivariate analysis that allows one to include multiple related independent and dependent variables in the same analysis. CCA also allows for interpretation of dimensional relations that exist both within a set of independent variables and within a set of dependent variables while controlling for the intercorrelations among all variables entered in the model (Tabachnick & Fidell, Citation2007). If a significant canonical correlation is found, then the model produces two canonical variates, an independent variate (comprised of variables from the independent set) and a dependent variate (comprised of variables from the dependent set). Each variable has a standardized canonical function coefficient (interpreted as the relative weight each variable contributes to that canonical variate set). Furthermore, variables with a coefficient of >0.40 are interpreted as meaningful variables in the set (for more details see Sherry & Henson, Citation2005). Finally, a redundancy coefficient is calculated for each canonical variate. This value represents the proportion of variance in one set of variables that is explained by the variant in the other set of variables (similar to R2 in multiple regression; Dattalo, Citation2014). We used one CCA to evaluate the potential dimensional relations between the following independent variables related to the acute psychedelic effects (1) acute insight experiences (PIQ), acute mystical-type experiences (MEQ), acute challenging experiences (CEQ). We used the following dependent variables related to mental health outcomes of the psychedelic experience (2) trauma symptoms change score (TSDSdiff), depression symptoms change score (DASS-21-Ddiff), anxiety symptoms change score (DASS-21-Adiff), and stress symptoms change score (DASS-21-Stressdiff). The GEDS-Frequency scale, and time since the psychedelic experience occurred, were included as control variables. Analyses were conducted in SPSS version 27 (IBM Corp, Citation2020).
Results
Participant characteristics
We had an intentionally diverse sample, with about one-half of the participants currently living in the United States, and the other half in Canada. The average age in the sample was 33.1 (SD = 11.2), and additional participant demographics are detailed in . The average age participants reported having their psychedelic experience was 22.9 (SD = 7.2). Most participants reported consuming psilocybin (37%) or LSD (36%) with slightly fewer reporting use of MDMA (27%), and approximately 93% reported that the dose they consumed was moderate, moderately high, or high. Additionally, 73% of participants reported that their psychedelic experience occurred at least one year before the survey. Participant psychedelic use is detailed in .
Table 1. Demographic characteristics of the total sample (N = 313).
Table 2. Psychedelic experiences of participants (N = 313).
Experiences of discrimination
Frequency of discrimination was assessed by the GEDS-Frequency scale (M = 41.95, SD 17.23), which indicated that participants experienced notable levels of discrimination across several domains. As shown in , items for which participants responded with 5 (Almost all the time), 4 (Most of the time), or 3 (A lot), were combined into a single category termed “Occurs Frequently” to indicate the percentage of respondents who experience the form of discrimination on a frequent basis. The most commonly reported experiences included feeling angry and wanting to “tell someone off for being racist” but instead doing nothing, which was a frequent experience in over 40% of respondents. Over one-third reported frequent experiences of being treated unfairly by others, such as by strangers and those employed in service jobs. Some items which were expected to be low-frequency were endorsed with alarming frequency, such as being called a racist name (34.5%). And approximately one-half of participants said “Never” (46.2%) to the question: “How often had you been forced to take drastic steps (such as filing a grievance, filing a lawsuit, quitting your job, moving away, and other actions) to deal with some racist thing that was done to you?”
Table 3. Frequency of experiences of discrimination from the M-GEDS (N = 313).
Comparison of mental health variables before and after the psychedelic experience
Overall, participants reported they experienced a mean decrease in traumatic stress (M = −8.6, SD = 16.2), depression (M = −2.9, SD = 5.5), anxiety (M = −1.5, SD = 4.5), and stress (M = −2.4, SD = 5.4) symptoms from before to after the psychedelic experience. The greatest reductions were seen in traumatic stress symptoms of the discrimination (TSDS) and depression (DASS21-D) and anxiety (DASS21-A). See for effect sizes and other details.
Table 4. Changes in symptoms before and after psychedelic experience (N = 313).
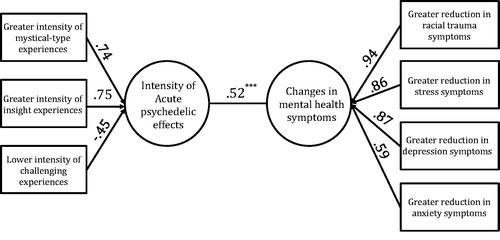
Canonical correlation analysis examining the relationship between acute psychedelic effects and mental health outcomes
reveals that there was one significant canonical correlation (Rc=0.52; p < .001). For the independent set, the canonical variate was represented primarily by greater intensity of acute mystical-type effects, greater intensity of acute insight effects, and lower intensity of acute challenging effects of the psychedelic experience, while controlling for the frequency of ethnic discrimination events (GEDS-Frequency) participants reported having prior to the psychedelic experience and the time since the psychedelic experience occurred. The canonical variate for the dependent set was represented primarily by greater reduction in racial trauma symptoms, greater reductions in stress symptoms, greater reduction in depression symptoms, and greater reduction in anxiety symptoms. The total amount of variance in the independent set explained by dependent set was 0.29, and the total amount of variance in the dependent set explained by the independent set was 0.68. This analysis revealed that the dimensional features of the acute psychedelic experience were significantly related to the dimensional reductions in mental health symptoms associated with ethnic discrimination among BIPOC.
Figure 1. Canonical Correlation Analysis (N = 313), F20,1009 = 5.571, p < .001; correlation =.52. Variance explained: Set 1 (acute effects): .29; Set 2 (MH variables): .68. Control variables: Time since psychedelic experience occurred and frequency of ethnic discrimination prior to psychedelic experience. ***p<.001.
Discussion
There is very little research focused on helping people who are suffering as a result of racial trauma, and likewise scant representation of BIPOC in psychedelic research. As a result, there has been little to no empirical work on the potential of psychedelics to address racial trauma. This study is the first to explore how mental health symptoms among BIPOC who have experienced racial trauma can change after using psychedelics. This study elucidated the psychological mechanisms by which psychedelics may lead to improvements in symptomology, with the intensity of the psychedelic experience significantly correlated with positive changes.
Characteristics of the sample
One of the strengths of the study is the large, diverse sample that spanned two major countries in North America, where both countries share a common legacy of colonization of Indigenous Peoples and racialization of BIPOC. We were successful in recruiting Native American, Indigenous Canadian, and Asian people – groups that are often underrepresented in substance use research (e.g. Michaels et al., Citation2018). The participants in our sample reported using LSD, psilocybin, or MDMA, and the dose was often reported as moderate to moderately high. Our sample was fairly young and well-educated. These findings are similar to those from a study that examined people recruited from 52 countries, including the U.S. and Canada, who use natural psychoactive drugs, including psychedelics, and found participants were likely to be between the age of 21–50 years and were well-educated, and the most common substance used was psilocybin (Aixalá et al., Citation2020). Data from the third iteration of the National Epidemiological Survey on Alcohol and Related Conditions indicates lifetime hallucinogen (e.g. LSD, psilocybin, mescaline) use is highest among adults 30–64 years old, whereas hallucinogen use in the past 12 months is highest among those 18–29 years old (Shalit et al., Citation2019). Further, the rate of lifetime use is highest among Native American (14.8%) and White people (11.6%) followed by Latinx (5.6%), Asian (3.5%), and Black people (3.4%).
Also consistent with our findings, epidemiological data on novel (i.e. newer psychedelics with a shorter history of human use) versus classic (e.g. LSD, psilocybin, peyote) psychedelic use found that people who used novel psychedelics tended to be younger (18–34 years), never married, have lower income, and had higher rates of all other illicit drug use except for sedatives and Phencyclidine (PCP), whereas people who use classic psychedelics tended to be older (35–64), married, divorced, or separated, and have higher income (Sexton et al., 2019). Notably, White and multiracial people are more likely to use novel psychedelics and Black, Asian and Latinx people were less likely to use novel psychedelics. Further, Black, Native American/Alaska Native, and Asian people are more likely to use classic than novel psychedelics. Taken together these similarities provide some evidence in favor of the generalizability of our sample.
Symptom response to psychedelics
Overall, participants in this study reported reductions from before to after the memorable psychedelic experience in all symptoms assessed. Further, it is noteworthy that 58% of participants reported that their relevant psychedelic experience was 3 or more years ago, indicating potentially long-lasting benefits. The decrease in traumatic stress was pronounced, as were decreases in symptoms of depression and anxiety. The symptoms captured in the TSDS are primarily anxiety-based, so the fact that reduction in depressive symptoms is similar to the reduction in general anxiety is notable. It may indicate that anxiety caused by racial trauma is as responsive to psychedelics as the more somatic symptoms of anxiety assessed by the DASS21-A. It could also indicate that depressive symptoms are quite responsive to psychedelics in those with racial trauma. Generally, BIPOC, regardless of racial and ethnic group, are less likely to meet the criteria for depression as compared to White people, although symptoms tend to be more persistent in BIPOC (Budhwani et al., Citation2015; Wu et al., Citation2003). Budhwani and colleagues (2015) found that more frequent discrimination (being treated as dishonest, less smart, disrespected, threatened, or called names) was associated with increases in depression in BIPOC. In our sample, the most highly endorsed discrimination experiences were being “really angry about something racist that was done” and wanting “to tell someone off for being racists towards you but [you] didn’t say anything.” There is a well-known connection between anger and depression and given the powerlessness many BIPOC feel in the face of racist experiences, it is not surprising that the anger and helplessness could manifest as depression (e.g. Atkins, Citation2015; Gerrard et al., 2018; Simons et al., Citation2006).
Psychological mechanisms
How psychedelics reduce distress due to racial trauma seems to depend on the intensity of the reported acute psychedelic effects, which were in turn correlated to reductions in mental health symptoms. Of the three facets of the psychedelic experience we examined, the intensity of the mystical-type experience was the most strongly related to the intensity of the psychedelic experience overall. The connection between mystical-type experience and mental health has been previously documented, with mystical-type experiences positively affecting a person’s mental health, regardless of whether they are naturally occurring or a result of psychedelic substances, and such experiences are correlated with subsequent positive changes in life satisfaction, purpose, and meaning (Griffiths et al., Citation2019). Also well-documented in the literature is the connection between insight and healing, which is a common goal of the psychotherapeutic process. Lane and colleagues (2015) argue that for traumatization, the essential ingredients of therapeutic change include reactivating old memories and then engaging in new emotional experiences that are incorporated into these reactivated memories via the process of reconsolidation. Insight would then represent the natural product of this process which psychedelics appear to facilitate (Davis et al., Citation2020; Davis et al., in press).
Notably, challenging experiences seemed to attenuate the positive effects of the psychedelic experience. These included fears of death or insanity, sadness, and isolation. Although challenging psychedelic experiences can ultimately be a positive avenue for change (e.g. catharsis leading to emotional breakthrough; Roseman et al., Citation2018), the challenging factors assessed in this study did not seem to be helpful for our respondents. In terms of clinical implications, psychedelic therapists and guides can help clients in these areas of potential difficulty to reduce the likelihood of unhelpful challenging experiences. This may include good preparation before the experience in terms of discussing the range of feelings that might emerge (positive and negative), use of connecting techniques during the experience (such as therapeutic touch) to reduce feelings of loneliness and isolation, and responsive caring (such as assertions of support in the moment) to address acute feelings of grief or paranoia. Because racism creates barriers between people, positive connecting experiences during the window of increased neuroplasticity (Barrett et al., Citation2020) may potentiate benefits by pairing a positive interpersonal experience with emergent racial trauma material (e.g. Lane et al., Citation2015). Likewise, it would also be important for therapists and guides to have training in culturally-informed approaches and/or be ethnically matched with clients, which would necessitate the training of more diverse psychedelic-assisted therapists (Williams et al., Citation2019).
Limitations and future directions
Although this study provided some important information about psychedelic use among BIPOC, outcomes were based on participant recall, which may be limiting for obtaining the most accurate data, especially for those whose memorable psychedelic experience was several years ago. Further, only people who reported benefits related to their psychedelic experience were included, so it cannot be assumed that psychedelics will be helpful for every BIPOC with racial trauma, and those who opted to participate in the study may have a positive bias in terms of their beliefs about the benefits of psychedelics. Moreover, self-report measures were utilized for this study, which poses both limitations and benefits. Notably, data collected in person via a clinical interview designed to capture symptoms of racial trauma might be more accurate (e.g. Williams, Metzger, et al., Citation2018). However, due to the highly stigmatized nature of substance use, along with the greater legal and social persecution faced by BIPOC who use illicit substances (Moore & Elkavich, Citation2008), an anonymous survey may be better suited for eliciting the type sensitive information required for this investigation (e.g. Williams & Bonner, Citation2006).
This study also utilized crowdsourced recruitment methods, which come with their own limitations such as inattentiveness and non-naivety (Chandler et al., Citation2014; Peer et al., Citation2017). We did not assess the influence of these factors; however, the internal consistency of all measures used in the study were highly reliable, thus providing confidence in the survey responses. Lastly, this study included a diverse group, but a more in-depth study of psychedelics and racial trauma in specific ethnic groups is also needed. Given the different psychedelics used among BIPOC, future research should examine whether the types of psychedelics used result in varied experiences and differentially impact racial trauma and other psychological symptoms among BIPOC by ethnic group. We also included BIPOC who reported use of three different substances (psilocybin, LSD, and MDMA), and there are differences between these drugs in terms of their acute effects. Although we did not find any differences in subjective measures as a function of drug type in this study, further studies should explore the potential differences these substances and their acute and enduring effects among BIPOC. Future studies should also document the presence or absence of another person, and what that person did to assist, to determine how much change is attributable to a supportive facilitator.
Conclusion
Humans have ingested psychedelics since the beginning of recorded history to defuse from harmful mental patterns, potentiate psychological growth, and heal from trauma. Although psychedelics are moving into the mainstream, including efforts to decriminalize psychedelic use and medicalize use of certain psychedelics (MDMA and psilocybin), many communities of color remain wary of psychedelics, resulting in low participation in research studies and raising concerns that once these substances are freely available, BIPOC may choose not to make use of them (Michaels et al., Citation2018). Our study shows that psychedelics can ameliorate symptoms of racial trauma, and several psychedelics seem equally effective for this task. As long as discrimination exists, there will be a need for effective treatments to help people suffering from racial trauma. The next important step in this work is to conduct clinical trials to determine if the results of this investigation would be replicated in a controlled setting. Due to the pervasive nature of racism, developing effective approaches to addressing racial trauma should become a priority, and psychedelics are a promising avenue.
Disclosure statement
Drs. Williams and Davis are board members of Source Research Foundation. This organization was not involved in the design/execution of this study or the interpretation or communication of findings.
Additional information
Funding
References
- Aixalá, M., Ona, G., Parés, Ò., & Bouso, J. C. (2020). Patterns of use, desired effects, and mental health status of a sample of natural psychoactive drug users. Drugs: Education, Prevention and Policy, 27(3), 191–198. https://doi.org/10.1080/09687637.2019.1611739
- Amoroso, T., & Workman, M. (2016). Treating posttraumatic stress disorder with MDMA-assisted psychotherapy: A preliminary meta-analysis and comparison to prolonged exposure therapy. Journal of Psychopharmacology (Oxford, England), 30(7), 595–600. https://doi.org/10.1177/0269881116642542
- APA. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Publishing.
- Apfelbaum, E. P., Sommers, S. R., & Norton, M. I. (2008). Seeing race and seeming racist? Evaluating strategic colorblindness in social interaction. Journal of Personality and Social Psychology, 95(4), 918–932. https://doi.org/10.1037/a0011990
- Argento, E., Braschel, M., Walsh, Z., Socias, M. E., & Shannon, K. (2018). The moderating effect of psychedelics on the prospective relationship between prescription opioid use and suicide risk among marginalized women. Journal of Psychopharmacology (Oxford, England), 32(12), 1385–1391. https://doi.org/10.1177/0269881118798610
- Asmundson, G. J. G., Thorisdottir, A. S., Roden-Foreman, J. W., Baird, S. O., Witcraft, S. M., Stein, A. T., Smits, J. A. J., & Powers, M. B. (2019). A meta-analytic review of cognitive processing therapy for adults with posttraumatic stress disorder. Cognitive Behaviour Therapy, 48(1), 1–14. https://doi.org/10.1080/16506073.2018.1522371
- Atkins, R. (2015). Depression in black single mothers: A test of a theoretical model. Western Journal of Nursing Research, 37(6), 812–830. https://doi.org/10.1177/0193945914528289
- Barrett, F. S., Bradstreet, M. P., Leoutsakos, J.-M S., Johnson, M. W., & Griffiths, R. R. (2016). The challenging experience questionnaire: Characterization of challenging experiences with psilocybin mushrooms. Journal of Psychopharmacology (Oxford, England), 30(12), 1279–1295. https://doi.org/10.1177/0269881116678781
- Barrett, F. S., Doss, M. K., Sepeda, N. D., Pekar, J. J., & Griffiths, R. R. (2020). Emotions and brain function are altered up to one month after a single high dose of psilocybin. Scientific Reports, 10(1), 2214. https://doi.org/10.1038/s41598-020-59282-y
- Barrett, F. S., Johnson, M. W., & Griffiths, R. R. (2015). Validation of the revised Mystical Experience Questionnaire in experimental sessions with psilocybin. Journal of Psychopharmacology, 29(11), 1182–1190. https://doi.org/10.1177/0269881115609019
- Bor, J., Venkataramani, A. S., Williams, D. R., & Tsai, A. C. (2018). Police killings and their spillover effects on the mental health of black Americans: A population-based, quasi-experimental study. The Lancet, 392(10144), 302–310. (18)31130-9. https://doi.org/10.1016/S0140-6736(18)31130-9
- Bryant-Davis, T., & Ocampo, C. (2006). A therapeutic approach to the treatment of racist-incident-based trauma. Journal of Emotional Abuse, 6(4), 1–22. https://doi.org/10.1300/J135v06n04_01
- Budhwani, H., Hearld, K. R., & Chavez-Yenter, D. (2015). Depression in racial and ethnic minorities: The impact of nativity and discrimination. Journal of Racial and Ethnic Health Disparities, 2(1), 34–42. https://doi.org/10.1007/s40615-014-0045-z
- Butts, H. F. (2002). The black mask of humanity: Racial/ethnic discrimination and post-traumatic stress disorder. The Journal of the American Academy of Psychiatry and the Law, 30(3), 336–339.
- Carhart-Harris, R. L., Bolstridge, M., Rucker, J., Day, C. M. J., Erritzoe, D., Kaelen, M., Bloomfield, M., Rickard, J. A., Forbes, B., Feilding, A., Taylor, D., Pilling, S., Curran, V. H., & Nutt, D. J. (2016). Psilocybin with psychological support for treatment-resistant depression: An open-label feasibility study. The Lancet Psychiatry, 3(7), 619–627. https://doi.org/10.1016/S2215-0366(16)30065-7
- Carter, R. T. (2007). Racism and psychological and emotional injury: Recognizing and assessing race-based traumatic stress. The Counseling Psychologist, 35(1), 13–105. https://doi.org/10.1177/0011000006292033
- Chandler, J., Mueller, P., & Paolacci, G. (2014). Nonnaïveté among Amazon Mechanical Turk workers: Consequences and solutions for behavioral researchers. Behavior Research Methods, 46(1), 112–130. https://doi.org/10.3758/s13428-013-0365-7
- Clark, T. T., Salas-Wright, C. P., Vaughn, M. G., & Whitfield, K. E. (2015). Everyday discrimination and mood and substance use disorders: A latent profile analysis with African Americans and Caribbean Blacks. Addictive Behaviors, 40, 119–125. https://doi.org/10.1016/j.addbeh.2014.08.006
- Cloitre, M. (2009). Effective psychotherapies for posttraumatic stress disorder: A review and critique. CNS Spectrums, 14(1 Suppl 1), 32–43.
- Cox, K., Lancelotta, R. L., Barsuglia, J., & Davis, A. K. (2018). November). 5-MeO-DMT and subjective improvements in post-traumatic stress disorder [Poster presentation]. Annual Convention of the Maryland Psychological Association.
- Dattalo, P. V. (2014). A demonstration of canonical correlation analysis with orthogonal rotation to facilitate interpretation [Unpublished manuscript]. School of Social Work, Virginia Commonwealth University, Richmond, Virginia.
- Davis, A. K., Barrett, F. S., So, S., Gukasyan, N., Swift, T. C., & Griffiths, R. R. (In press). Development of the Psychological Insight Questionnaire among a sample of people who have consumed psilocybin or LSD. Journal of Psychopharmacology.
- Davis, A. K., Barrett, F. S., & Griffiths, R. R. (2020). Psychological flexibility mediates the relations between acute psychedelic effects and subjective decreases in depression and anxiety. Journal of Contextual Behavioral Science, 15, 39–45. https://doi.org/10.1016/j.jcbs.2019.11.004
- Davis AK, Barrett FS, May DG, et al. Effects of Psilocybin-Assisted Therapy on Major Depressive Disorder: A Randomized Clinical Trial. JAMA Psychiatry. Published online November 04, 2020. doi:10.1001/jamapsychiatry.2020.3285
- Davis, A. K., So, S., Lancelotta, R., Barsuglia, J. P., & Griffiths, R. R. (2019). 5-methoxy-N,N-dimethyltryptamine (5-MeO-DMT) used in a naturalistic group setting is associated with unintended improvements in depression and anxiety. The American Journal of Drug and Alcohol Abuse, 45(2), 161–169. https://doi.org/10.1080/00952990.2018.1545024
- Department of Justice. (2014). Hate crime statistics. Department of Justice. Retrieved June 2, 2020, from https://ucr.fbi.gov/hate-crime/2014
- Desalu, J. M., Goodhines, P. A., & Park, A. (2019). Racial discrimination and alcohol use and negative drinking consequences among Black Americans: A meta-analytical review. Addiction (Abingdon, England), 114(6), 957–967. https://doi.org/10.1111/add.14578
- Foa, E. B., Rothbaum, B. O., Riggs, D. S., & Murdock, T. B. (1991). Treatment of posttraumatic stress disorder in rape victims: A comparison between cognitive-behavioral procedures and counseling. Journal of Consulting and Clinical Psychology, 59(5), 715–723. https://doi.org/10.1037//0022-006X.59.5.715
- Gerrard, M., Gibbons, F. X., Fleischli, M. E., Cutrona, C. E., & Stock, M. L. (2018). Moderation of the effects of discrimination-induced affective responses on health outcomes. Psychology & Health, 33(2), 193–212. https://doi.org/10.1080/08870446.2017.1314479
- Gerrard, M., Stock, M. L., Roberts, M. E., Gibbons, F. X., O'Hara, R. E., Weng, C., & Wills, T. A. (2012). Coping with racial discrimination: The role of substance use. Psychology of Addictive Behaviors: Journal of the Society of Psychologists in Addictive Behaviors, 26(3), 550–560. https://doi.org/10.1037/a0027711
- Godley, J. (2018). Everyday discrimination in Canada: Prevalence and patterns. Canadian Journal of Sociology, 43(2), 111–142. https://doi.org/10.29173/cjs29346
- Gone, J. P., Hartmann, W. E., Pomerville, A., Wendt, D. C., Klem, S. H., & Burrage, R. L. (2019). The impact of historical trauma on health outcomes for indigenous populations in the USA and Canada: A systematic review. The American Psychologist, 74(1), 20–35. https://doi.org/10.1037/amp0000338
- Griffiths, R. R., Hurwitz, E. S., Davis, A. K., Johnson, M. W., & Jess, R. (2019). Survey of subjective "God encounter experiences": Comparisons among naturally occurring experiences and those occasioned by the classic psychedelics psilocybin, LSD, ayahuasca, or DMT. PloS One, 14(4), e0214377. https://doi.org/10.1371/journal.pone.0214377
- Griffiths, R. R., Johnson, M. W., Carducci, M. A., Umbricht, A., Richards, W. A., Richards, B. D., Cosimano, M. P., & Klinedinst, M. A. (2016). Psilocybin produces substantial and sustained decreases in depression and anxiety in patients with life-threatening cancer: A randomized double-blind trial. Journal of Psychopharmacology, 30(12), 1181–1197. https://doi.org/10.1177/0269881116675513
- Griffiths, R. R., Johnson, M. W., Richards, W. A., Richards, B. D., McCann, U., & Jesse, R. (2011). Psilocybin occasioned mystical-type experiences: Immediate and persisting dose-related effects. Psychopharmacology, 218(4), 649–665. https://doi.org/10.1007/s00213-011-2358-5
- Hurd, N. M., Varner, F. A., Caldwell, C. H., & Zimmerman, M. A. (2014). Does perceived racial discrimination predict changes in psychological distress and substance use over time? An examination among Black emerging adults. Developmental Psychology, 50(7), 1910–1918. https://doi.org/10.1037/a0036438
- Huynh, V. W. (2012). Ethnic microaggressions and the depressive and somatic symptoms of Latino and Asian American adolescents. Journal of Youth and Adolescence, 41(7), 831–846. https://doi.org/10.1007/s10964-012-9756-9
- IBM Corp. (2020). IBM SPSS Statistics for Windows (Version 27.0) [Computer software]. IBM Corp.
- Johansen, P.-Ø., & Krebs, T. S. (2015). Psychedelics not linked to mental health problems or suicidal behavior: A population study. Journal of Psychopharmacology (Oxford, England), 29(3), 270–279. https://doi.org/10.1177/0269881114568039
- Johnson, M. W., & Griffiths, R. R. (2017). Potential Therapeutic Effects of Psilocybin. Neurotherapeutics: The Journal of the American Society for Experimental Neurotherapeutics, 14(3), 734–740. https://doi.org/10.1007/s13311-017-0542-y
- Kusch, M., Grau, P., Warner, R. C., Loyo, K. T., Zhang, X., Fritz, N., & Wetterneck, C. T. (2017). Inclusion of ethnic and racial minorities with PTSD in evidence-based clinical trials: A report card [Poster presentation]. International Society for Traumatic Stress Studies.
- Landrine, H., Klonoff, E. A., Corral, I., Fernandez, S., & Roesch, S. (2006). Conceptualizing and measuring ethnic discrimination in health research. Journal of Behavioral Medicine, 29(1), 79–94. https://doi.org/10.1007/s10865-005-9029-0
- Lane, R. D., Ryan, L., Nadel, L., & Greenberg, L. (2015). Memory reconsolidation, emotional arousal, and the process of change in psychotherapy: New insights from brain science. The Behavioral and Brain Sciences, 38, e1. https://doi.org/10.1017/S0140525X14000041
- Lester, K., Resick, P. A., Young-Xu, Y., & Artz, C. (2010). Impact of race on early treatment termination and outcomes in posttraumatic stress disorder treatment. Journal of Consulting and Clinical Psychology, 78(4), 480–489. https://doi.org/10.1037/a0019551
- Liu, W. M., Liu, R. Z., Garrison, Y. L., Kim, J. Y. C., Chan, L., Ho, Y., & Yeung, C. W. (2019). Racial trauma, microaggressions, and becoming racially innocuous: The role of acculturation and White supremacist ideology. The American Psychologist, 74(1), 143–155. https://doi.org/10.1037/amp0000368
- Lovibond, S. H., & Lovibond, P. F. (1995). Manual for the depression anxiety & stress scales (2nd Ed.). Psychology Foundation.
- MacLean, K. A., Johnson, M. W., & Griffiths, R. R. (2011). Mystical experiences occasioned by the hallucinogen psilocybin lead to increases in the personality domain of openness. Journal of Psychopharmacology, 25(11), 1453–1461. https://doi.org/10.1177/0269881111420188
- Michaels, T. I., Purdon, J., Collins, A., & Williams, M. T. (2018). Inclusion of people of color in psychedelic-assisted psychotherapy: A review of the literature. BMC Psychiatry, 18(1), 245. https://doi.org/10.1186/s12888-018-1824-6
- Mithoefer, M. C., Mithoefer, A. T., Feduccia, A. A., Jerome, A., Wagner, M., Wymer, J., Holland, J., Hamilton, S., Yazar-Klosinski, B., Emerson, A., & Doblin, R. (2018). 3,4-methylenedioxymethamphetamine (MDMA)-assisted psychotherapy for post-traumatic stress disorder in military veterans, firefighters, and police officers: A randomised, double-blind, dose-response, phase 2 clinical trial. The Lancet Psychiatry, 5(6), 486–497. https://doi.org/10.1016/S2215-0366(18)30135-4
- Moore, L. D., & Elkavich, A. (2008). Who's using and who's doing time: Incarceration, the war on drugs, and public health. American Journal of Public Health, 98(9 Suppl), S176–S180. https://doi.org/10.2105/ajph.98.supplement_1.s176
- Norton, P. J. (2007). Depression Anxiety and Stress Scales (DASS-21): Psychometric analysis across four racial groups. Anxiety, Stress, and Coping, 20(3), 253–265. https://doi.org/10.1080/10615800701309279
- O’Keefe, V. M., Wingate, L. R., Cole, A. B., Hollingsworth, D. W., & Tucker, R. P. (2015). Seemingly harmless racial communications are not so harmless: Racial microaggressions lead to suicidal ideation by way of depression symptoms. Suicide & Life-Threatening Behavior, 45(5), 567–576. https://doi.org/10.1111/sltb.12150
- Ot’alora, G. M., Grigsby, J., Poulter, B., Van Derveer, J. W., Giron, S. G., Jerome, L., Feduccia, A. A., Hamilton, S., Yazar-Klosinski, B., Emerson, A., Mithoefer, M. C., & Doblin, R. (2018). 3,4-Methylenedioxymethamphetamine-assisted psychotherapy for treatment of chronic posttraumatic stress disorder: A randomized phase 2 controlled trial. Journal of Psychopharmacology, 32(12), 1295–1307. https://doi.org/10.1177/0269881118806297
- Pascoe, E. A., & Smart Richman, L. (2009). Perceived discrimination and health: A meta-analytic review. Psychological Bulletin, 135(4), 531–554. https://doi.org/10.1037/a0016059
- Peer, E., Brandimarte, L., Samat, S., & Acquisti, A. (2017). Beyond the Turk: Alternative platforms for crowdsourcing behavioral research. Journal of Experimental Social Psychology, 70, 153–163. https://doi.org/10.1016/j.jesp.2017.01.006
- Pierce, C. (1970). Offensive mechanisms. In F. Barbour (Ed.), The Black seventies (pp. 265–282). Porter Sargent.
- Powers, M. B., Halpern, J. M., Ferenschak, M. P., Gillihan, S. J., & Foa, E. B. (2010). A meta-analytic review of prolonged exposure for posttraumatic stress disorder. Clinical Psychology Review, 30(6), 635–641. https://doi.org/10.1016/j.cpr.2010.04.007
- Priest, N., Paradies, Y., Trenerry, B., Truong, M., Karlsen, S., & Kelly, Y. (2013). A systematic review of studies examining the relationship between reported racism and health and wellbeing for children and young people. Social Science & Medicine (1982), 95, 115–127. https://doi.org/10.1016/j.socscimed.2012.11.031
- Roseman, L., Nutt, D. J., & Carhart-Harris, R. L. (2018). Quality of acute psychedelic experience predicts therapeutic efficacy of psilocybin for treatment-resistant depression. Frontiers in Pharmacology, 8, 974. https://doi.org/10.3389/fphar.2017.00974
- Ross, S., Bossis, A., Guss, J., Agin-Liebes, G., Malone, T., Cohen, B., Mennenga, S. E., Belser, A., Kalliontzi, K., Babb, J., Su, Z., Corby, P., & Schmidt, B. L. (2016). Rapid and sustained symptom reduction following psilocybin treatment for anxiety and depression in patients with life-threatening cancer: A randomized controlled trial. Journal of Psychopharmacology (Oxford, England), 30(12), 1165–1180. https://doi.org/10.1177/0269881116675512
- Sanches, R. F., de Lima Osório, F., Dos Santos, R. G., Macedo, L. R. H., Maia-de-Oliveira, J. P., Wichert-Ana, L., de Araujo, D. B., Riba, J., Crippa, J. A. S., & Hallak, J. E. C. (2016). Antidepressant effects of a single dose of ayahuasca in patients with recurrent depression: A SPECT study. Journal of Clinical Psychopharmacology, 36(1), 77–81. https://doi.org/10.1097/JCP.0000000000000436
- Schottenbauer, M. A., Glass, C. R., Arnkoff, D. B., Tendick, V., & Gray, S. H. (2008). Nonresponse and dropout rates in outcome studies on PTSD: Review and methodological considerations. Psychiatry, 71(2), 134–168. https://doi.org/10.1521/psyc.2008.71.2.134
- Shalit, N., Rehm, J., & Lev-Ran, S. (2019). Epidemiology of hallucinogen use in the U.S. results from the national epidemiologic survey on alcohol and related conditions III. Addictive Behaviors, 89, 35–43. https://doi.org/10.1016/j.addbeh.2018.09.020
- Sherry, A., & Henson, R. K. (2005). Conducting and interpreting canonical correlation analysis in personality research: A user-friendly primer. Journal of Personality Assessment, 84(1), 37–48. https://doi.org/10.1207/s15327752jpa8401_09
- Simons, R. L., Simons, L. G., Burt, C. H., Drummund, H., Stewart, E., Brody, G. H., Gibbons, F. X., & Cutrona, C. (2006). Supportive parenting moderates the effect of discrimination upon anger, hostile view of relationships, and violence among African American boys. Journal of Health and Social Behavior, 47(4), 373–389. https://doi.org/10.1177/002214650604700405
- Soto, J. A., Dawson-Andoh, N. A., & BeLue, R. (2011). The relationship between perceived discrimination and Generalized Anxiety Disorder among African Americans, Afro Caribbeans, and non-Hispanic Whites. Journal of Anxiety Disorders, 25(2), 258–265. https://doi.org/10.1016/j.janxdis.2010.09.011
- Sue, D. W., Capodilupo, C. M., Torino, G. C., Bucceri, J. M., Holder, A. M. B., Nadal, K. L., & Esquilin, M. (2007). Racial microaggressions in everyday life: Implications for clinical practice. The American Psychologist, 62(4), 271–286. https://doi.org/10.1037/0003-066X.62.4.271
- Tabachnick, B. G., & Fidell, L. S. (2007). Using multivariate statistics (5th Ed.). Allyn & Bacon/Pearson Education.
- Terwilliger, B. G., Bach, N., Bryan, C., & Williams, W. T. (2013). Multicultural versus colorblind ideology: Implications for mental health and counseling. Nova Science Publishers.
- Williams, M. T. (2020a). Microaggressions: Clarification, evidence, and impact. Perspectives on Psychological Science: A Journal of the Association for Psychological Science, 15(1), 3–26. https://doi.org/10.1177/1745691619827499
- Williams, M. T. (2020b). Psychology cannot afford to ignore the many harms caused by microaggressions. Perspectives on Psychological Science: A Journal of the Association for Psychological Science, 15(1), 38–43. https://doi.org/10.1177/1745691619893362
- Williams, M. T., & Bonner, L. (2006). Sex education attitudes and outcomes among North American women. Adolescence, 41(161), 1–14.
- Williams, M. T., Malcoun, E., Sawyer, B. A., Davis, D. M., Nouri, L. B., & Bruce, S. L. (2014). Cultural adaptations of prolonged exposure therapy for treatment and prevention of posttraumatic stress disorder in African Americans. Behavioral Sciences (Basel, Switzerland), 4(2), 102–124. https://doi.org/10.3390/bs4020102
- Williams, M. T., Metzger, I. W., Leins, C., & DeLapp, C. (2018). Assessing racial trauma within a DSM–5 framework: The UConn racial/ethnic stress & trauma survey. Practice Innovations, 3(4), 242–260. https://doi.org/10.1037/pri0000076
- Williams, M. T., Printz, D., Ching, T., & Wetterneck, C. T. (2018). Assessing PTSD in ethnic and racial minorities: Trauma and racial trauma. Directions in Psychiatry, 38(3), 179–196.
- Williams, M. T., Printz, D. M. B., & DeLapp, R. C. T. (2018). Assessing racial trauma with the Trauma Symptoms of Discrimination Scale. Psychology of Violence, 8(6), 735–747. https://doi.org/10.1037/vio0000212
- Williams, M. T., Reed, S., & Aggarwal, R. (2019). Culturally-informed research design issues in a study for MDMA-assisted psychotherapy for posttraumatic stress disorder. Journal of Psychedelic Studies, 4(1), 40–50. https://doi.org/10.1556/2054.2019.016
- Williams, M., Gooden, A. M. C., & Davis, D. (2012). African Americans, European Americans and pathological stereotypes: An African-centered perspective. In G. R., Hayes, & M. H. Bryant (Eds.), Psychology of culture (pp. 25–46. Nova Science Publishers.
- Wu, Z., Noh, S., Kaspar, V., & Schimmele, C. M. (2003). Race, ethnicity, and depression in Canadian society. Journal of Health and Social Behavior, 44(3), 426–441. https://doi.org/10.2307/1519788
- Zoellner, L. A., Feeny, N. C., Fitzgibbons, L. A., & Foa, E. B. (1999). Response of African American and Caucasian women to cognitive behavioral therapy for PTSD. Behavior Therapy, 30(4), 581–595. https://doi.org/10.1016/S0005-7894(99)80026-4
