ABSTRACT
This report describes the case of a 15-year-old female Arabian camel with omaso-abomasal adenocarcinoma showing prolonged anorexia with colic bouts leading to cachexia during the last 6 months. Hematological and biochemical findings were indicative of a moderate to severe haemorrhagic anaemia. Ultrasonographic examination revealed hyperechoic severely thickened (68 mm) and corrugated omaso-abomasal walls with heterogonous contents. Exploratory laparotomy revealed a large barrel-shaped mass with dense contents including parts of the compound stomach adhered to the parietal peritoneum. A definitive diagnosis was based on histopathological examination confirming the mass as an omaso-abomasal adenocarcinoma. Omaso-abomasal adenocarcinoma should be included in the differential diagnosis of abdominal tumours in camel.
Introduction
Abdominal tumours are rare in camels and account for less than 0.05% of all reported neoplasms (Kühn et al. Citation2003; Sartin et al. Citation2004). To the authors’ knowledge, omaso-abomasal adenocarcinoma has not been described in dromedary camels. Gastric adenocarcinomas are rare in domestic animals other than dogs and cats. Evidence for the aetiology of camel gastric tumour has not been defined until now (Ritchey et al. Citation1996). While, in humans and dogs, adenocarcinoma is the most common gastric malignancy, and it is frequently reported in correlation with several risk factors (Swann and Holt Citation2002). The present report describes the clinical, hematological, biochemical, ultrasonographic and pathologic findings of an omaso-abomasal adenocarcinoma in a female Arabian camel without evidence of metastasis.
Case report
A 15-year-old female dromedary camel was admitted to the Veterinary Teaching Hospital, Qassim University, Saudi Arabia, because of a 6 months’ history of chronic inappetence and decreased body weight with colic bouts which were not resolved after treatment at the local private clinics. On presentation, the camel underwent a thorough clinical examination which revealed poor general condition and demeanour with a body condition score of 2 out of 5. Physical examination of the animal was performed according to Higgins and Kock (Citation1984). The study protocol was approved by the committee of animal welfare and ethics, Faculty of Agriculture and Veterinary Medicine, Qassim University, Saudi Arabia.
Basic haematological results in the investigated she-camel are summarized in . A moderate to severe anaemia, leukopenia, neutrophilia and lymphocytopenia were noted. Biochemical panel showed low total protein and albumin concentrations. In contrast, the calcium, magnesium, globulin and blood urea nitrogen (BUN) concentrations were slightly elevated. In addition, increased creatine kinase (CK), aspartate aminotransferase (AST) and γ-glutamyl transferase (γ-GTP) were revealed in blood biochemical analysis. Faecal samples were evaluated for parasites eggs and cysts by the commercial analysis system (faecal flotation technique). Fresh faeces were collected directly from the rectum of the affected she-camel and mixed thoroughly in the fecalyzer with a denser solution (NaCl/ sugar). The fecalyzer filled with more solution until meniscus forms, then a coverslip was placed on the formed meniscus. After 10–15 min, the coverslip was removed and examined under the light microscope. While polymerase chain reaction (PCR) method was used for diagnosis of Johne’s disease in the affected animal. DNA template was extracted from faeces, rectal samples and lymph nodes. Positive samples were considered when show amplification of 229-bp PCR product which is the specific product of Mycobacterium avium subsp. paratuberculosis-IS900. No abnormal findings were reported in the faecal examination and Johne’s disease serology was negative. Reference hematological and serum chemistry values were in accordance to Tharwat (Citation2015).
Table 1. Results of hematological and biochemical examinations.
Abdominal ultrasonography was carried out in sternal recumbency position using 3.5 MHz sector and 7.5 MHz linear transducers (SSD-500, Aloka, Tokyo, Japan). The abdomen was examined through the right and left flanks without a definitive localization of the lesion. While intraoperative ultrasonography revealed hyperechoic severely thickened (68 mm) and corrugated omaso-abomasal walls with heterogonous contents (). Almost all the gastric wall was infiltrated by the mass without transition to the other abdominal organs.
Figure 1. Intraoperative ultrasonographic view of the gastric mass showing the abomasal wall appeared thickened, vascularized, hyperechoic (black arrow, A) and the contents appeared heterogeneous (gray arrow, B).
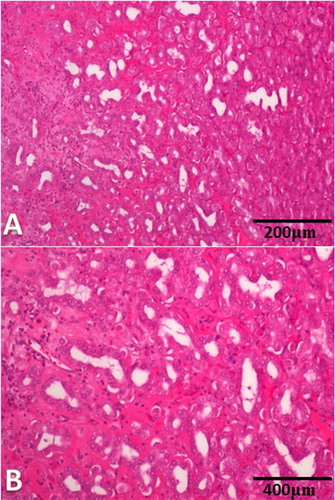
The animal showed no signs of pain and it was decided to assign for routine exploratory laparotomy of the mass. Surgical exploration revealed barrel-shaped mass with dense contents at palpation including parts of the compound stomach adhered to the parietal peritoneum. There were no any gross abnormalities in other abdominal organs and peripheral lymph nodes. These findings indicated that the animal had a grave prognosis and it was decided to euthanize it at this stage. Postmortem examination of the abdomen revealed a large barrel-shaped mass weighting about 10.5 kg involving the omasum and abomasum. The cut surface of the mass showed a thick dense omasal and abomasal wall with malodorous bloody contents (). The omasal and abomasal laminae were thickened, congested and ulcerated given the perceived extent of the neoplasia into the wall of omasum and abomasum (). Also, adhesion between the mass and the thickened parietal peritoneum was seen. Specimens from the abomasal wall, omasal wall, heart, liver and spleen were fixed in 10% neutral buffered formalin and processed routinely for staining with haematoxylin and eosin (HE). Histopathological findings of the abomasal and omasal walls revealed well-differentiated invasive adenocarcinoma. The tumour consisted of variably sized acini lined by malignant epithelial cells with moderate atypia separated by desmoplastic stroma with dense mixed inflammatory cell infiltrate. Extensive areas of necrosis with suppuration were also seen (). No evidence of metastasis was found in the heart, liver and spleen, despite an extensive postmortem examination. The definitive diagnosis was a non-metastatic omaso-abomasal adenocarcinoma associated with chronic proliferative gastritis.
Figure 2. Abdominal enlarged hard mass weighting 10.5 kg (A). The cut section of the mass showing the abomasal (B) and omasal (C) folds were thickened, congested and ulcerated.
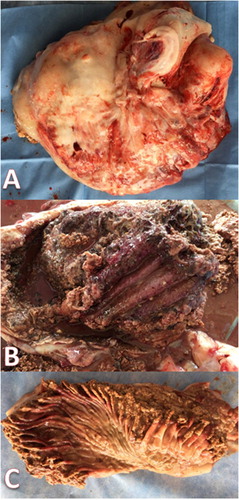
Figure 3. (A,B). Omaso-abomasal adenocarcinoma. (A) The tumor consisted of variably sized acini lined by malignant epithelial cells with moderate atypia separated by desmoplastic stroma with dense mixed inflammatory cell infiltrate (HE, ×200). (B) Extensive areas of necrosis with suppuration (HE, ×400).
Discussion
Gastric adenocarcinoma is a global health problem in humans and pets ranking as the fifth most common cancer and third leading cause of cancer-related mortality worldwide (Swann and Holt Citation2002), while in large ruminant practice, these tumours are not frequently diagnosed. It has been reported in the abomasum of cattle (Ritchey et al., Citation1996) and only a case in a Bactrian camel (Kühn et al. Citation2003). To our knowledge, omaso-abomasal adenocarcinoma has not been reported in Arabian camels. The rare occurrence of gastric neoplasia in Arabian camels could be attributed to the fact that, in many Arabic countries, dead camels are usually buried without postmortem examination. Even if necropsy is carried out, it is done by non-specialized persons without experience in postmortem examination. Therefore, many subtle lesions may go unnoticed, hence unreported (Sartin et al. Citation2004).
Gastric tumours may arise in any part of the stomach, assume a wide range of forms and can metastasize (Kühn et al. Citation2003). However, the gastric adenocarcinoma in the present report was restricted to the omasum and abomasum without apparent metastasis suggesting that, although the tumour is locally aggressive, it does not easily spread to other parts of the camel body. These tumours in humans and small animals are commonly treated surgically in combination with chemotherapy and/or radiotherapy (Makris and Poultsides Citation2017). In camel practice, these techniques are usually impractical due to the location of the tumour, the hazardous consequences regarding food safety and economic feasibility. Generally, the prognosis of gastric adenocarcinoma is poor even after surgical intervention, and in most affected cases, life expectancy was few months of diagnosis (Makris and Poultsides Citation2017).
The main clinical findings, in this case, were chronic inappetence and decreased body weight with colic bouts. No obvious reason for this digestive upset was detected and it has been hypothesized that dietary, inflammatory, functional or mechanical factors are incriminated (Zaghloul et al. Citation2009). Gastric neoplasia was a part of the differential diagnosis because the abnormal hematological and biochemical profiles and the advanced age of our patient favoured a diagnosis of neoplasia.
Ultrasonographic examination of the omaso-abomasal adenocarcinoma revealed a 68 mm hyperechoic severely thickened and corrugated omaso-abomasal wall with heterogonous contents. In this case study, ultrasonography provided a precise non-invasive diagnostic tool for interpreting the size, location and morphology of gastric tumour and for obtaining biopsy samples, which could not be evaluated with the physical investigation. Similar recommendations were reported by Abouelnasr et al. (Citation2016) and El-Shafaey and Hamed (Citation2017).
Histopathological investigation represents an important tool to detect and confirm gastric adenocarcinoma. The investigated tumour in this report showed a well-differentiated invasive omaso-abomasal adenocarcinoma. These findings are in accordance with Ritchey et al. (Citation1996) and Swann and Holt (Citation2002). In contrast to Kühn et al. (Citation2003) and Braun et al. (Citation2011), there was no apparent metastasis of the gastric adenocarcinoma to any other part of the body.
The collaboration between hematological, biochemical, ultrasonographic and histopathological examinations initiate a constant approach for a precise diagnosis of gastric adenocarcinoma in a dromedary camel. To our knowledge, this report is the first description of omaso-abomasal adenocarcinoma, such as occurred in this dromedary camel which broadens the diagnostic spectrum of abdominal disorders in a dromedary camel. Gastric adenocarcinoma should be included in the differential diagnosis of abdominal tumours in camel.
Conflict of interest
This study is supported by the King Abdulaziz City for Science and Technology (KACST) (project: AC-34-292).
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Abouelnasr K, El-Shafaey E, Mosbah E, El-Khodery S. 2016. Utility of ultrasonography for diagnosis of superficial swellings in buffalo (Bubalus bubalis). J Vet Med Sci. 78:1303–1309. doi: 10.1292/jvms.15-0629
- Braun U, Schnetzler C, Dettwiler M, Sydler T, Meyer S, Gerspach C. 2011. Ultrasonographic findings in a cow with abomasal lymphosarcoma: case report. BMC Vet Res. 7:20. doi: 10.1186/1746-6148-7-20
- El-Shafaey E, Hamed M. 2017. Ultrasonographic and histopathological findings of mammary fibroadenoma in a buffalo heifer (Bubalus bubalis) with special reference to surgical treatment: a case report. J Vet Med Allied Sci. 1:35–37.
- Higgins AJ, Kock RA. 1984. I. A guide to the clinical examination, chemical restraint and medication of the camel. Br Vet J. 140:485–504. doi: 10.1016/0007-1935(84)90045-9
- Kühn N, Gröne A, Pagan O, Bacciarini LN. 2003. Metastatic gastric adenocarcinoma and diffuse hyperplastic gastritis resembling human Menétrier’s disease in a camel (Camelus ferus bactrianus). J Vet Med A Physiol Pathol Clin Med. 50:359–362. doi: 10.1046/j.1439-0442.2003.00553.x
- Makris EA, Poultsides GA. 2017. Surgical considerations in the management of gastric adenocarcinoma. Surg Clin North Am. 97:295–316. doi: 10.1016/j.suc.2016.11.006
- Ritchey JW, Marshall C, David C, Brown TT. 1996. Mucinous adenocarcinoma in the abomasum of a cow. Vet Pathol. 33:454–456. doi: 10.1177/030098589603300418
- Sartin EA, Crowe DR, Whitley EM, Treat RE, Purdy SR, Belknap EB. 2004. Malignant neoplasia in four alpacas. J Vet Diag Invest. 16:226–229. doi: 10.1177/104063870401600309
- Swann HM, Holt DE. 2002. Canine gastric adenocarcinoma and leiomyosarcoma: a retrospective study of 21 cases (1986–1999) and literature review. J Am Anim Hosp Assoc. 38:157–164. doi: 10.5326/0380157
- Tharwat M. 2015. Hematology, biochemistry and blood gas analysis in healthy female dromedary camels, their calves and umbilical cord blood at spontaneous parturition. J Camel Pract Res. 22:239–245. doi: 10.5958/2277-8934.2015.00039.9
- Zaghloul A, Karrouf G, Fouda T, El-Shafaey E. 2009. Diagnosis and management of abomasal disorders in cattle. 6th Int. Sci. Conf. Fac. Vet. Med. Mans. Univ. 87:114.
