ABSTRACT
Objectives: development of cytomegalovirus (CMV)-specific CD8+ T cell response is crucial in preventing symptomatic CMV infection specially, in stem cell transplant (SCT) patients. The aim of this study was to evaluate CMV-specific CD8+ T cell reconstitution in allogeneic SCT recipients and to study the possible association between CMV-specific CD8+ T cell recovery with protection from CMV reactivation and persistency.
Methods: Human leuKocyte antigen (HLA)-tetramers were used for CMV-specific CD8+ cell quantitation by Flow cytometry in twenty post-allogeneic SCT patients.
Results: Nine patients (45%) developed rapid recovery of CMV-specific CD8+ cells, among them; 7 patients (78%) had no CMV reactivation in the first 95 days post-transplant.
Five patients had developed persistent CMV viremia; all of them had not developed CMV-specific CD8+ recovery till day 95 post-transplant.
Patients with persistent CMV viremia had a statistically significant lower means of CMV-specific CD8+ percent and absolute count compared to those without persistent viremia (p = .001, .015), respectively.
Discussion: The incidence of CMV reactivation and persistency was higher among patients with delayed CMV-specific CD8+ reconstitution in the first 95 days post-transplant.
Conclusion: CMV-specific CD8+ cells can help in categorizing patients into risk groups: (early recovery/low risk) and (delayed recovery/increased risk), this tool may guide clinicians in the selection of patients who may profit from prophylactic antiviral therapy and frequent viral monitoring.
Introduction
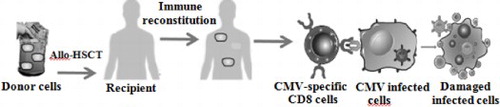
Hematopoietic stem cell transplant (SCT) is a major approach in the treatment of hematological and non-hematological diseases. The demand for both autologous and allogeneic transplants has been progressively expanding [Citation1].
Cytomegalovirus (CMV) infects around 60–90% of individuals all-over the world. Primary CMV infection is usually asymptomatic and remains dormant in the immunocompetent host, while in immunocompromised allogeneic SCT patients, CMV reactivation represents a major risk for transplant-related morbidity/mortality [Citation2].
In immunocompetents, CMV-specific CD8+ T lymphocytes play crucial role in limiting CMV infection symptoms and reactivation [Citation2].
CMV monitoring and therapy require considerable budget aside from the antiviral therapy associated morbidity. Obviously, upgrading CMV management is mandatory in hematopoietic stem cell transplant (HSCT) recipients.
Fluorescent HLA-peptide tetramers offer significant potential in the study of antigen-specific immune reconstitution after SCT. Major histocompatibility complex (MHC) tetramers are complexes between HLA class I and specific antigenic peptides, these complexes bind to a distinctive set of T-cell receptors on a subset of CD8-T cells [Citation3].
The iTAg Tetramers are constructed from mutated HLA molecules to minimize their binding to majority of CD8 cells, but retain peptide-specific binding, thus enabling precise discrimination/quantitation of specific T cell response to a certain virus.
This study evaluated CMV-specific CD8+ T cell reconstitution, in allogeneic HSCT recipients, and their potential protective role in CMV reactivation and persistency; allowing clinicians to further refine prophylactic/therapeutic policies in high-risk populations.
Subjects and methods
This prospectively designed study included 20 fully engrafted recipients who received a non-T-cell depleted peripheral blood hematopoietic stem cell transplantation (PBHSCT) from a fully matched sibling. Patients and donors were CMV-seropositive. Eleven out of the 20 (55%) patients received a graft from a sex-matched sibling. Patients’ age ranged from 3 to 41 with a mean of 21.5 ± 13.7 years. The majority of the enrolled patients 19/20 (95%) received a transplant from his/her brother/sister with a nearby age; only one patient received a graft from his mother with an outstanding age difference. Patients’ characteristics are detailed in (). HLA-A2/HLA-B35 patients were selected as the iTAg Tetramers is allele restricted.
Table 1. Patients characteristics.
All patients received the same myeloablative conditioning regimen before transplantation of a fully matched graft from an HLA-identical sibling, followed by a post-transplant protocol of Cyclosporine for 3–6 months after bone marrow transplant (BMT), Methylprednisolone 1–2 mg kg−1 to be reduced gradually after 15 days, prophylactic antibiotic and prophylactic antifungal while no prophylactic antiviral was given only patients who developed polymerase chain reaction (PCR) detected CMV viremia received Gancyclovair/or Valgancyclovair. The current study didn’t employ anti-thymocyte globulin (ATG) (Campath-1) in the used regimen.
Patients were admitted in BMT unit of Naser institute where 5 sequential samples, starting on day 35 post-transplant and every 15 days to day 95, were taken and sent to the Clinical Pathology Department, Kasr Al Aini Hospital, for flowcytometry quantitation of CMV-specific CD8 using iTAg MHC Tetramers and CMV detection by qualitative-PCR in addition to complete blood picture. This study was conducted from May 2014 to April 2016 after being approved by the ethics committee of both Cairo University and Naser institute, informed consent was obtained from each participant or his/her guardians.
HLA-A2 and/or HLA-B35 Patients were selected as the iTAg Tetramers are allele restricted. Quantitation of CMV-specific CD8+ T-lymphocytes by the iTAg MHC Tetramers was done by Flow cytometry.
Each specimen was immunostained for CD8-FITC/CMV-iTAg-PE/CD3-PC5 and CD8-FITC/CD4-PE/CD3-PC5 to obtain percentage of CMV-specific CD8+T cells, CD3, CD4 and CD8 and hence absolute numbers per micro liter were calculated as product of: (Absolute lymphocyte count) (% CD8+ cells in the lymphocyte gate) (% tetramer-stained cells in the CD8+ T-cells) [Citation4].
Monocles were supplied by Beckman Coulter, Inc. Fullerton, CA, USA. Anti-CD8-FITC, PN 6603861, Anti-CD3-PC5, PN IM2635U, Anti-CD4-PE, PN IM0449U2, iTAg TM MHC Class I Human Tetramer-SA-PE Streptavidin-Phycoerythrin Beckman Coulter, Inc. 92835 USA. Negative controls used were PBMNCs from CMV-seronegatives and A2- and B35-negative individuals. Analysis was done on tricolor FCIP ‘EPICS-XL coulter flowcytometer’.
For qualitative real-time PCR, PB-DNA isolation was done on QIAcube (Qiagen, Germany) using QIAamp DNA-blood mini-kit (Qiagen, Germany, Cat. 51304). Real-time PCR assay protocol was applied as described previously [Citation5] on the LC 2.0 (Roche), using FastStart DNA Master HybProbe (Roche Diagnostics).
Statistical analysis was performed on Statistical Package for Social Sciences (SPSS) version 21. Numerical data were summarized using means and standard deviations or medians and ranges. Categorical data were summarized as percentages. Data were explored for normality using Kolmogrov-Smirnov test and Shapiro–Wilk test. Correlations among different variables were determined by using Pearson’s test and spearman rho. Detecting difference in laboratory measurements overtime was tested by repeated measure ANOVA followed by paired t-test for pairwise comparisons. Comparisons between two groups were done by Chi-square test or fisher exact for categorical variables and independent t-test or Mann–Whitney test as appropriate. p-value of ≤.05 was considered statistically significant.
Results
During the first 95 days post-transplant, 5 patients (25%) developed fever, 8 patients (40%) had early CMV viremia (first 100 days following SCT), in 5 of them viremia was persistent (≥4 weeks positive PCR) according to Gratama et al. [Citation3]. Within 2 years post-transplant 6 patients (30%) passed away (data concerning morbidity and mortality were not available).
A mean CMV-specific CD8% and absolute count (AC) was calculated for the 5 sequential samples of each patient before calculating the entire group mean values. Mean CMV-specific CD8% ranged from 0 to 4.9% with a mean of 0.8 ± 1.1%, while it’s mean AC ranged from 0.0 to 74 with a mean of 9.5 ± 17.2 µL−1.
In one patient, CMV-specific CD8 reconstitution was marked as 10.6 and 8.3% of all CD8 lymphocytes on day 65 and day 80, respectively, representing an AC of 178.9 and 141.5 µL−1, respectively, this patient didn’t develop CMV reactivation throughout the study.
Early recovery is defined as ≥7 of CMV-specific CD8 cells µL−1 in any of the 65 days post-transplant samples, while delayed recovery is defined as <7 cells µL−1 in all these samples [Citation3], accordingly 9 patients (45%) developed early recovery [7/9 were males (77.8%) and 6/9 (66.7%) were adults, 7/9 (77.8%) had A2 allele and 2/9 (22.2%) had B35 allele], while 11 patients (55%) developed delayed recovery [6/11 were males (54.5%), 4/11 (36.4%) were adults, 4/11 (36.4%) had A2 allele and 7/11 patients (63.6%) had B35 allele]. With no significant difference in age/gender between the two groups, as for HLA-alleles patients’ numbers were too small for analysis.
In early recovery group; only 2/9 patients (22%) developed early CMV viremia, while in delayed recovery group; 6/11 patients (55%) developed early CMV viremia, however, this wasn’t statistically significant (p = .197).
Five patients developed persistent CMV viremia; none of them recovered CMV-specific CD8 cells till the end of the study.
Patients with persistent CMV viremia had a significantly lower mean of CMV-specific CD8% and AC compared to non-persistent viremia ( and ).
Table 2. Comparison of transplant patients with persistent CMV viremia versus those without persistent viremia as regards CMV-specific CD8+ percent, absolute number of: CMV-specific CD8+, CD3, CD4 and CD8 in the 5 sequential samples.
Table 3. Comparison of transplant patients with early CMV reactivation versus those with no CMV reactivation as well as those with persistent CMV viremia versus those without persistent viremia as regards medians of CMV-specific CD8+ percent and absolute number in the 5 sequential samples.
Patients with delayed recovery have 16 folds greater risk of developing persistent CMV viremia (Odds Ratio) compared to early recovery group ().
Table 4. Calculation of Odds ratio (OR) for the risk of developing persistent CMV viremia in association with delayed CMV-specific CD8+ recovery in post-allogenic BMT patients.
In a trial to validate the protective cut off value that has been used in our study which was adopted by Gratama et al. [Citation3], we performed a ROC curve analysis, which revealed a cutoff value of 2 CMV-specific CD8 µL−1 at day 80 as the best discriminator for patients who underwent CMV reactivation with a specificity of 83.3% a sensitivity of 75%, as all of the patients who showed viral reactivation afterwards 5/20 (25%) were below this cut off.
On Day 35, adult patients had; a significantly higher CMV-specific CD8 AC (median, 1.825, range 0.00–32.3 µL−1) compared to children (median, 0.450, range 0.046–3.4 µL−1), (p = .07); a significantly higher CD3 and CD8 AC (median CD3, 1240.9, range 345.1–2100.8 µL−1, and median CD8, 686.4, range 204.5–1425.3 µL−1) compared to children (median CD3, 460.1, range 96.1–1319.7 µL−1, and median CD8, 220.7, range 128.9–1068.4 µL−1) (p = .034 for both), while for CD4 AC comparison between the two groups revealed a p value of .059. No significant difference was encountered in any other sample.
No gender-based difference was encountered in the present work by comparing CMV-specific CD8 AC or percent/CD3, CD4 or CD8 AC in any of the samples.
On day 35 post-transplant, HLA-A2 patients had a significantly higher CMV-specific CD8% and AC compared to HLA-B35 group (p = .03, .012), respectively. On day 50 and day 80, A2 allele group showed a statistically higher median CD8 AC compared to the B35 allele group (p = .03, .025), respectively, this difference was not encountered in the remaining samples.
Discussion
The lack of CMV-specific T-cells has been associated with CMV disease which remains problematic for successful HSCT [Citation6].
In our study, mean CMV-specific CD8 was 0.8 ± 1.1%, (range, 0–4.9%), while it’s AC was 9.5 ± 17.2 µL−1 (range 0.0–74 µL−1). CMV-specific CD8 AC and percent were positively correlated in all samples. (p = .0 in the 1st 4 samples, .01 in the 5th sample).
In agreement Gratama et al. [Citation3] reported that CMV-specific CD8+ cells % and ACs were positively correlated.
One of our patients had a marked CMV-specific CD8 reconstitution (10.6% and 8.3% of CD8 lymphocytes on day 65, day 80, respectively), representing an AC of 178.9 and 141.5 µL−1, respectively. This patient didn’t develop CMV reactivation all through the study.
In accordance, an extremely marked CMV-specific CD8 reconstitution of >10% of CD8 lymphocytes on day 43 (AC of 409 × 105 L−1) and 21% of CD8T cells on day 21 (AC of 139 × 105 L−1) were reported emphasizing the potency of CMV in stimulating virus-specific CD8 cells [Citation7].
Ozdemir et al. [Citation8], reported that, 21% of SCT patients had extremely high frequencies of the CMV-specific CD8 cells (>5%), and nearly 88% had measurable response (>0.05%). One (A2+, B7−) subject had 40% CMV-specific CD8 cells.
In allo-HSCT recipients, CMV-specific CD8 of 0–440 cells µL−1 (median 3.33, mean 25.45 ± 55.42 cells µL−1) with a percentage of 0–42% (median 1.53, mean 4.29 ± 6.54%) were reported [Citation3].
Variation in CMV-specific CD8+ cells referred not only to individual responses but also to, tetramer alleles [Citation3], graft (manipulated/unmanipulated) and conditioning regimen (myeloablative/reduced intensity) [Citation6].
This study showed a detectable (>0.1%) percent of CMV-specific CD8 recovery in 18/20 (90%) of the studied patients, one of the 2 patients who had no detectable CMV-specific CD8 cells, developed persistent CMV viremia and passed away within 2 years post-transplant (patient 16). While the other patient developed non-persistent CMV viremia (Patient 9) and he was still alive. When using the AC, 15/20 patients (75%) had detectable CMV-specific CD8 cells (≥1 µL−1). In the other 5 patients; 3 developed persistent CMV viremia and passed away within 2 years post-transplant (Patients 1, 5, 16); one developed non-persistent CMV viremia (Patient 9) and the other patient didn’t develop CMV viremia (Patient 4) and both were still alive.
Detectable level of CMV-specific CD8 cells AC/percentage was not reported to protect against CMV reactivation, persistency or disease; that’s why the need to define accurately the protective recovery threshold and the proper cutoff day of such recovery was crucial.
This study has adapted the cut off recovery threshold that has been proposed by Gratama et al. [Citation3] which is a multicentre prospective longitudinal clinical trial that evaluated CMV-specific CD8 T-cell recovery after allogeneic HSCT in 83 CMV-seropositive recipients. Patients were monitored every 2 weeks from day 28 to day 100, every 2–4 weeks from day 101 to day 270, using a panel of 5 tetramers and were monitored for 1-year post SCT for viral results. In their study they determined the best protective tetramer recovery threshold through evaluating a range of CMV-specific CD8 cells (2–10 cells µL−1). Their results showed that rapid recovery (≥7 cells µL−1 in any blood sample during the first 65 days after transplantation) was associated with protection from recurrent/persistent CMV infection/disease.
Other studies have adapted other cut offs to define the protective tetramer recovery threshold. A study done by Aubert et al. [Citation9] stated that CMV-specific CD8 cells were detected shortly after SCT and proposed that a level of ≥20 × 106 T cells L−1 could control viral replication when maintained. To be noted here that their study was done on 11 HSCT patients, using HLA-A2 tetramer only, around 50% of the patients received a T cell depleted graft whether direct or indirect (CD34-selected graft), also from the start of conditioning until engraftment, patients were receiving high dose intravenous acyclovir, to suppress CMV. Patients were heterogenous as regards the patient/donor CMV seropositivity, besides no fixed time points were used to unify the evaluation of tetramer recovery. These factors may partially explain the different cut off protective tetramer threshold that had been suggested by this study.
Pastore et al. [Citation10] presented a cut off of >5 CMV-specific CD8 cells µL−1 as a protective value after applying a ROC curve analysis for the best point, however, their scheduled time points for monitoring tetramer recovery were quiet distant (1, 2, 3 and 6 months).
Ohnishi et al. [Citation11] proposed a protective tetramer recovery threshold >10 CMV-specific CD8 cells µL−1. It is worth noting here that among the 37 patients enrolled in their study, 11 received Reduced-intensity transplantation (RIST) with ATG, 17 patients received RIST without ATG and the rest received conventional myeloablative protocol. To be mentioned here that ATG is reported to significantly affect the immune recovery secondary to pre-transplant lymphoid depletion. Different conditioning regimen could attribute to this protective threshold variability among different studies.
Using ROC curve analysis, we propose using a protective cut off value of 2 CMV-specific CD8 µL−1 at day 80 as it allowed proper discrimination of our enrolled patients, however, this should be tested first on a larger group of patients with the same enrolment criteria.
According to Gratama et al. defined recovery threshold and cutoff day, 9/20 patients (45%) developed early recovery in our study, and this was in agreement with the defining multicentre study, which reported a 47.2% of early recoveries in their studied patients [Citation3].
Rapid recovery of total CD4 or CD8 lymphocytes is defined by ≥100 cells µL−1 within the first 65 days [Citation3]. Accordingly, 80% of our enrolled patients (16/20) developed rapid CD4 recovery and 90% (18/20) developed rapid CD8 recovery. The 2 patients who showed a delayed CD8 recovery showed also a delayed CD4 and CMV-specific CD8+ recovery, and they developed persistent CMV viremia and passed away within 2 years post-transplant. The other 2 patients with delayed CD4 recovery, one of them showed early total and CMV-specific CD8+ recovery and didn’t develop CMV reactivation. While the other patient showed early total CD8 recovery but, delayed CMV-specific CD8+ recovery and he developed CMV persistency; pointing to the importance of CMV-specific CD8+ rather than total CD8/CD4 in protection against CMV reactivation and persistent viremia.
In agreement, it is stated that 44% of patients with poor outcomes had rapid recovery of total CD4+ cells but delayed recovery of CMV-specific CD8+ T cells; while another 40% of patients with poor outcomes had rapid recovery of total CD8+ cells but delayed recovery of CMV-specific CD8+ T cells [Citation3].
To be mentioned here, that most of our patients had a CD8 AC exceeding their CD4 AC in most of the samples, this is not the normal CD4/8 ratio for their age. Reviewing the literature, it is reported that in the first 100 days after HSCT, CD4T cells reconstitute later than CD8T cells, leading to an inversion of the CD4/CD8 ratio [Citation12]. It is stated also that reversal of the CD4/CD8 ratio may extend up to 5 years post transplantation [Citation13].
On Day 35, we reported that adult patients had a significantly higher CMV-specific CD8+, CD3 and CD8 AC compared to children. Regarding CMV-specific CD8+ % and CD4 AC, no significant difference was encountered. This may indicate that children may show a little bit delayed reconstitution of CD3, CD8 and secondary to that CMV-specific CD8 portion compared to adults as the difference was seen in day 35 sample only. To be mentioned here that a positive correlation was encountered between patients’ ages’ in years and the ACs of lymphocytes, neutrophils and CD8 on day 35 post-transplant (p = .015, .01, .045), respectively.
Reviewing literature, it is reported that the older the patient, the higher the T-cell recovery stems from expansion of memory T cells in the graft, however, the prediction of immune reconstitution in older patients is problematic, as the rate of immune system aging is highly variable. Moreover, the age of the donor is crucial as the graft of an older donor has reduced immune-reconstituting capability in the recipient [Citation12].
In the present study, HLA-A2 patients on Day 35 post-transplant, had a statistically significant higher CMV-specific CD8+ AC and percent compared to HLA-B35 patients group. A statistically significant higher median CD8 AC was encountered in the A2 allele group compared to the B35 allele group on day 50 and day 80 samples.
In agreement Cwynarski et al. [Citation7], reported different allele restricted CMV-specific CD8+ response in individuals assessed with both A2- and B7-restricted tetramers. In most of these subjects, the B7-restricted response was significantly higher than the A2-restricted response.
Comparing between transplant patients with CMV-specific CD8+ recovery versus those with delayed recovery as regards CD3, CD4 and CD8 AC reconstitution in the first 95 days post-transplant, revealed no statistically significant difference in any of the 5 samples.
This study showed no significant difference in the incidence of CMV reactivation between HSCT patients with early CMV-specific CD8 recovery versus those with delayed recovery ().
In consistence, previous results showed that CMV disease did not develop in any patient who showed CMV-specific CD8 lymphocytes recovery; however, CMV reactivation was detected in few patients [Citation7]. Also Ozdemir et al. [Citation8], did not find a relationship between the ability to control CMV reactivation and the recovery of sufficient numbers of CMV-specific T cells.
While Gratama et al. [Citation3], indicated that patients with delayed recovery are at higher risk of viral reactivation.
Among our patients; 6 of the delayed recovery group didn’t develop CMV reactivation; absence of detectable CMV-specific T cells (delayed recovery) may be referred to an impaired immune response or to the unavailability of the relevant tetramers to quantify the CMV-specific CD8 recovery for a specific patient. It is not feasible to judge if another unmeasured allele response is suppressing the CMV reactivation.
Also among the 9 patients who developed early CMV-specific CD8 recovery; 2 patients developed CMV reactivation, questioning the protective value of CMV-specific CD8 recovery. However several studies found that CMV reactivation may be related to impaired function of CMV-specific CD4+ and CD8+ T cells [Citation8,Citation14,Citation15].
The current work enlightens that there is 16 times increased risk of developing persistent CMV viremia in patients with delayed CMV-specific CD8+ recovery.
In agreement, Gratama et al. [Citation3], designated that delayed recovery of CMV-specific CD8T cells predisposes patients to develop recurrent or persistent CMV infection, CMV disease, and lethal complications.
High dose prednisolone was reported to be a risk factor for CMV reactivation being associated with suppression of CMV-specific CD8 cells, on the other hand, neither ganciclovir prophylaxis nor Campath antibody T-cell depletion was found to be associated with CMV-specific CD8+ reconstitution [Citation7].
It is reported also that early reconstitution of CMV-specific CD8 response was not detected if either the donor or recipient was CMV seronegative. Questioning the origin of CMV-specific CD8 cells whether they belong to the donor or to the recipient reconstituted cells? Gandhi et al. [Citation16], reported that all CMV-specific CD8+ cells detected in allo-BMT recipient were of donor origin as confirmed by DNA polymorphism analysis.
Different approaches have been proposed to selectively improve virus-specific T cells reconstitution after allo-BMT, for example, selective isolation of donor CMV-specific T cells to be transferred to the recipient [Citation17,Citation18]. Also activation of CMV-specific T clone by antigen-presenting cells loaded with viral specific proteins followed by in vitro expansion of this clone has been reported [Citation19,Citation20].
Not all alleles are targeted with the tetramer panel used in the current study. Despite this limitation, the panel of tetramers in this study was effective in identifying high- and low-risk patients using tetramers targeting the most common HLA alleles among Egyptians.
In conclusion, CMV-specific CD8 recovery can guide categorizing patients into risk groups: (early recovery/low risk) and (delayed recovery/high risk), enabling clinicians to select patients who may benefit from prophylactic antiviral therapy and frequent viral monitoring. Future studies using functional analysis together with cellular count of CMV-specific CD8 cells with diverse combinations of Tetramer alleles, may improve results further.
The current work proposes that frequent monitoring of CMV-specific CD8 may discriminate patients who might profit from preemptive antiviral therapy from those who might escape treatment considering that CMV-specific CD8 cells reaches the protective threshold of 7 cells µL−1 using day 65 as cutoff day while being frequently monitored for viral reactivation. However a properly designed bed side clinical trial that should be applied on a larger cohort of patients, using the above recommended threshold is mandatory for validation of these conclusions.
Disclosure statement
No potential conflict of interest was reported by the authors.
ORCID
Dalia Gamil Amin Tawadrous http://orcid.org/0000-0003-1672-4647
Said Fathy Hotar http://orcid.org/0000-0001-7722-6508
References
- Gratwohl A, Baldomero H, Passweg J. Hematopoietic stem cell transplantation activity in Europe. Curr Opin Hematol. 2013;20(6):485–493. doi: 10.1097/MOH.0b013e328364f573
- Boeckh M, Nichols WG. The impact of cytomegalovirus serostatus of donor and recipient before hematopoietic stem cell transplantation in the era of antiviral prophylaxis and preemptive therapy. Blood. 2004;103(6):2003–2008. doi: 10.1182/blood-2003-10-3616
- Gratama JW, Boeckh M, Nakamura R, et al. Immune monitoring with iTAg MHC tetramers for prediction of recurrent or persistent cytomegalovirus infection or disease in allogeneic hematopoietic stem cell transplant recipients: a prospective multicenter study. Blood. 2010;116(10):1655–1662. doi: 10.1182/blood-2010-03-273508
- Kraan J, Arroz M, Keeney M, et al. Flow cytometric enumeration of class I HLA-restricted, peptide-specific CD8+ T lymphocytes using tetramer technology and single-platform absolute T-cell counting. J Biol Regul Homeost Agents. 2003;17:268–278.
- Binnicker MJ, Espy ME. Comparison of Six real-time PCR assays for qualitative detection of cytomegalovirus in clinical specimens. J Clin Microbiol. 2013;51(11):3749–3752. doi:10.1128/JCM.02005-13.
- Borchers, S, Luther S, Lips U. Tetramer monitoring to assess risk factors for recurrent cytomegalovirus reactivation and reconstitution of antiviral immunity post allogeneic hematopoietic stem cell transplantation. Transpl Infect Dis. 2011;13(3):222–236. doi: 10.1111/j.1399-3062.2011.00626.x
- Cwynarski K, Ainsworth J, Cobbold M, et al. Direct visualization of cytomegalovirus-specific T-cell reconstitution after allogeneic stem cell transplantation. Blood. 2001;97(5):1232–1240. doi: 10.1182/blood.V97.5.1232
- Ozdemir E, St John LS, Gillespie G, et al. Cytomegalovirus reactivation following allogeneic stem cell transplantation is associated with the presence of dysfunctional antigen-specific CD8+ T cells. Blood. 2002;100(10):3690–3697. doi: 10.1182/blood-2002-05-1387
- Aubert G, Hassan-Walker AF, Madrigal JA, et al. Cytomegalovirus-specific cellular immune responses and viremia in recipients of allogeneic stem cell transplants. J. Infect. Dis. 2001;184:955–963. doi: 10.1086/323354
- Pastore D, Delia M, Mestice A, et al. Recovery of CMV-specific CD8+ T cells and Tregs after allogeneic peripheral blood stem cell transplantation. Biol Blood Marrow Transplant. 2011;17:550–557. doi: 10.1016/j.bbmt.2010.04.011
- Ohnishi M, Sakurai T, Heike Y, et al. Evaluation of cytomegalovirus-specific T-cell reconstitution in patients after various allogeneic haematopoietic stem cell transplantation using interferon-gamma-enzyme-linked immunospot and human leucocyte antigen tetramer assays with an immunodominant T-cell epitope. Br J Haematol. 2005;131:472–479. doi: 10.1111/j.1365-2141.2005.05800.x
- Seggewiss R, Einsele H. Immune reconstitution after allogeneic transplantation and expanding options for immunomodulation. Blood. 2010;115(19):3861–3868. doi: 10.1182/blood-2009-12-234096
- Fujimaki K, Maruta A, Yoshida M. Immune reconstitution assessed during five years after allogeneic bone marrow transplantation. Bone Marrow Transplant. 2001;27:1275–1281. doi: 10.1038/sj.bmt.1703056
- Morita-Hoshi Y, Heike Y, Kawakami M, et al. Functional analysis of cytomegalovirus-specific T lymphocytes compared to tetramer assay in patients undergoing hematopoietic stem cell transplantation. Bone Marrow Transplant. 2008;41(6):515–521. doi: 10.1038/sj.bmt.1705932
- Gratama JW, Brooimans RA, van der Holt B, et al. Monitoring cytomegalovirus IE-1 and pp65-specific CD4+ and CD8+ T-cell responses after allogeneic stem cell transplantation may identify patients at risk for recurrent CMV reactivations. Cytometry B Clin Cytom. 2008;74B(4):211–220. doi: 10.1002/cyto.b.20420
- Gandhi MK, Wills MR, Okecha G, et al. Late diversification in the clonal composition of human cytomegalovirus-specific CD8+ T cells following allogeneic hemopoietic stem cell transplantation. Blood. 2003;102(9):3427–3438. doi: 10.1182/blood-2002-12-3689
- Walter EA, Greenberg PD, Gilbert MJ, et al. Reconstitution of cellular immunity against cytomegalovirus in recipients of allogeneic bone marrow by transfer of T-cell clones from the donor. N Engl J Med. 1995;333:1038–1044. doi: 10.1056/NEJM199510193331603
- Berger C, Turtle CJ, Jensen MC, et al. Adoptive transfer of virus-specific and tumor-specific T cell immunity. Curr Opin Immune. 2009;21(2):224–232. doi: 10.1016/j.coi.2009.02.010
- Kleihauer A, Grigoleit U, Hebart H, et al. Ex vivo generation of human cytomegalovirus-specific cytotoxic T cells by peptide-pulsed dendritic cells. Br J Haematol. 2001;113(1):231–239. doi: 10.1046/j.1365-2141.2001.02681.x
- Einsele H, Kapp M, Grigoleit GU. CMV-specific T cell therapy. Blood Cells Mol Dis. 2008;40(1):71–75. doi: 10.1016/j.bcmd.2007.07.002