Abstract
Patients on sick leave due to work-related stress often present with cognitive impairments as well as sleep disturbances. The aim of this longitudinal study was to examine the role of perceived stress and sleep disturbances in the longitudinal development in cognitive impairments in a group of patients with prolonged work-related stress (N = 60) during a period of 12 months following initial professional care-seeking. Objective cognitive impairments (neuropsychological tests) were measured on two occasions – at initial professional care-seeking and at 12-month follow-up. Questionnaires on perceived stress, sleep disturbances, and cognitive complaints were completed seven times during the 12 months which facilitated multilevel analysis with segregation of within-person (change) and between-person (baseline level) components of the time-varying predictors (perceived stress and sleep disturbances). Change in perceived stress was associated with concurrent and subsequent change in self-reported cognitive complaints over the period of 12 months and to a lesser extent the change in performance on neuropsychological tests of processing speed from baseline to 12-month follow-up. Change in sleep disturbances was also associated with concurrent and subsequent change in self-reported cognitive complaints over the 12 months but not with change on neuropsychological test performance. Although the mechanism behind the improvement in cognitive impairments in patients with work-related stress should be further explored in future studies, the results could suggest that improvement in cognitive impairments is partly mediated by decreasing levels of perceived stress and, to a lesser extent, decreasing levels of sleep disturbances.
Lay summary
This study examines the role of perceived stress and sleep disturbances in respect to the development of cognitive impairments (e.g. memory and concentration) in a group of patients with work-related stress. We found that change in cognitive impairments seems to be partly explained by change in perceived stress and, to a lesser extent, sleep disturbances over time. This could suggest that cognitive impairments can be reduced by stress management interventions which aim to reduce perceived stress and sleep disturbances but future studies are needed to confirm this interpretation.
Introduction
Prolonged work-related stress is a major concern in Denmark as well as in other EU countries (Broughton, Citation2010). Work-related stress can be defined as a process, in which an individual perceives demands associated with work as being more than the individual can handle and thereby negatively affecting the psychological and/or physiological state of the individual. The various symptoms of prolonged work-related stress can be fatigue, tension, complaints of physical pain, anxiety, and feelings of sadness (Eskildsen, Andersen, Pedersen, Vandborg, & Andersen, Citation2015). Sleep disturbances (e.g. difficulties falling asleep or staying asleep) are also often present in this patient group (Dalgaard et al., Citation2014; Willert, Thulstrup, Hertz, & Bonde, Citation2010). In general, stress and sleep disturbances seem closely related since research studies have shown that perceived stress are associated with disturbed sleep – both in clinical and healthy populations (Åkerstedt, Lekander, Petersen, Kecklund, & Axelsson, Citation2014; Kashani, Eliasson, & Vernalis, Citation2012; Theadom & Cropley, Citation2008). Furthermore, other studies have shown that different kinds of stressors at work can increase the risk of disturbed sleep in employees (Linton et al., Citation2015).
Patients with prolonged work-related stress do also often complain about cognitive impairments (Dalgaard et al., Citation2014; Öhman, Nordin, Bergdahl, Birgander, & Neely, Citation2007; Van der Linden, Keijsers, Eling, & Van Schaijk, Citation2005; Willert et al., Citation2010). They report having difficulties sustaining attention, learning new things, and remembering plans and appointments. Furthermore, an increasing number of studies suggest that the self-reported cognitive complaints are accompanied by objectively measurable impairments in cognitive performance on neuropsychological tests. These impairments are most apparent on complex tests of sustained attention in particular when mental control such as inhibition of prepotent (predominant or spontaneous) responses are required and when time pressure is inherent in the task (Eskildsen, Andersen, et al., Citation2015; Jonsdottir et al., Citation2013; Jovanovic, Perski, Berglund, & Savic, Citation2011; Sandström, Rhodin, Lundberg, Olsson, & Nyberg, Citation2005; Sandström et al., Citation2011; van Dam, Keijsers, Eling, Paul, & Becker, Citation2011).
Sleep disturbances and cognitive impairments are also closely connected and it is well-documented in experimental studies that sleep deprivation can impair multiple aspects of cognitive function in healthy individuals (Lim & Dinges, Citation2010; Reynolds & Banks, Citation2010; Van Dongen, Maislin, Mullington, & Dinges, Citation2003). A previous observational study has also found an association between sleep and cognitive performance in students. They found that both pre-exam stress and sleep quality were associated with exam performance and that the association between stress and performance decreased after adjusting for sleep quality (Ahrberg, Dresler, Niedermaier, Steiger, & Genzel, Citation2012). In addition, a randomized controlled trial has indicated that cognitive complaints, but not performance on a working memory test, can be reduced by cognitive behavioral therapy incorporating sleep interventions (Willert et al., Citation2010). However, it is still not known to what extent sleep disturbances explain the incidence of cognitive impairments in patients with prolonged work-related stress or whether decreasing levels of perceived stress and/or sleep disturbances can explain improvement in cognitive function in the same patient group.
In a sample of out-patients with prolonged work-related stress, we have previously found mild to moderate cognitive impairments as measured with a neuropsychological test battery at initial professional care-seeking. The magnitude of these impairments was largest regarding prospective memory, processing speed, and manipulation in working memory. In addition, the patients reported higher perceived stress and more self-reported cognitive complaints (Eskildsen, Andersen, et al., Citation2015). Twelve months after initial professional care-seeking, patients had improved in respect to perceived stress, self-reported cognitive complaints, and performance on two of the neuropsychological tests (processing speed and prospective memory) (Eskildsen, Andersen, Pedersen, & Andersen, Citation2016). The underlying processes of change, which could explain this improvement, have not previously been examined. This was the aim of the present study. We wanted to examine the role of perceived stress and sleep quality in predicting change in (1) objective performance on the two neuropsychological tests on which the patients improved (Eskildsen et al., Citation2016) and (2) self-reported cognitive complaints in the 12 months following initial professional care-seeking. Concerning the relationship between perceived stress, sleep quality, and objective performance, we had only two measurements (baseline and 12-months follow-up). We had seven measurements on the data with self-reported cognitive complaints as the outcome. Therefore, we could benefit from multilevel analysis with proper methods of segregating the within-person (change) and between-person (level) components of the time-varying predictors (perceived stress and sleep quality) (Curran & Bauer, Citation2011; Hoffman & Stawski, Citation2009). We hypothesized the following:
Hypothesis 1: Change in perceived stress and sleep quality (baseline to 12 month follow-up) is positively associated with change in objective performance on the tests of processing speed and prospective memory.
Hypothesis 2: Change in both perceived stress and sleep quality during the 12 months (the within-person effect) is positively associated with concurrent and subsequent change in self-reported cognitive complaints.
Methods
Participants
This paper describes the analyses of additional data from an observational longitudinal study examining the long-term consequences of work-related stress (Eskildsen, Andersen, et al., Citation2015; Eskildsen et al., Citation2016). The participants (N = 60) were outpatients referred to Department of Occupational Medicine, the Regional Hospital West Jutland by their general practitioner. Patients with work-related stress were referred if the patient needed help in returning to work and/or if the condition was eligible for being reported to the National Board of Industrial Injuries.
At intake, the patients were interviewed by an occupational psychologist regarding work-related stressors, other kinds of stressors, previous mental history, symptom development and duration, etc. In case of depressive symptoms, the 6-item Hamilton Depression Scale was used to rate the severity of depressive symptoms (Bech et al., Citation1975; Hamilton, Citation1960). Following this, the patients were treated according to standard practice at the Department of Occupational Medicine. This included guidance regarding return to work and/or Cognitive Behavioral Therapy (approximately four sessions on average) (Eskildsen et al., Citation2016).
Inclusion criteria were (a) duration of stress symptoms for at least 1 month, which was established in the interview, (b) both the patient and the occupational psychologist should consider it likely that the patient’s mental health symptoms were a reaction to work-related stressors, and (c) patient symptom severity should correspond to a T-score of at least 63 of one or more of the Symptom Checklist (SCL-90-R) subscales: Somatization (SCL-SOM), Anxiety (SCL-ANX), and Depression (SCL-DEP) (Derogatis, Citation1977). A T-score of 63 was recommended to identify a “case” in the Danish manual of the SCL-90-R (Olsen, Mortensen, & Bech, Citation2007). The exclusion criteria were (a) current or previous psychiatric disorder (within the last two years) with the exception of mild depressive symptoms defined as a score <9 on the 6-item Hamilton Depression Scale, (b) physical illness causing cognitive impairment, (c) alcohol or substance abuse, (d) native language other than Danish, (e) learning disabilities, and (f) psychoactive drug use other than current antidepressants.
Materials
Self-reports
After inclusion, a questionnaire was sent to the e-mail of all participants. All questionnaires referred to the last month and were repeated after 1, 2, 3, 6, 9, and 12 months.
The 10-item Perceived Stress Scale (PSS-10) (Cohen, Kamarck, & Mermelstein, Citation1983) is a global stress measure developed to assess the extent to which individuals find their lives to be unpredictable, uncontrollable, and overloaded (e.g. In the last month, how often have you been upset because of something that happened unexpectedly?). Each item is scored on a five-point scale ranging from 0 (Never) to 4 (Very often). The total score (range 0–40) is calculated as the sum of item scores after converting the positively formulated items (4, 5, 7, and 8). The development and validation of the Danish version are published elsewhere (Eskildsen, Dalgaard, et al., Citation2015).
The Cognitive Failures Questionnaire (CFQ) (Broadbent, Cooper, FitzGerald, & Parker, Citation1982) contains 25 items and is designed to measure the frequency of lapses in perception, memory, and action (e.g. How often do you read something and find you haven’t been thinking about it and must read it again?). Each item is scored on a five-point scale ranging from 0 (Never) to 4 (Very often). The total score (0–100) is calculated as the sum of all item scores.
The Pittsburgh Sleep Quality Index (PSQI) (Buysse, Reynolds, Monk, & Berman, Citation1989) is a measure of subjective sleep quality and contains 18 items concerning, for instance, time spent in bed, sleeping medication and subjective sleep quality (e.g. During the past month, how would you rate your sleep quality overall?). Seven component scores (0–3) and one global score (0–21) can be calculated. Larger scores indicate more severe sleep problems. A PSQI global score >5 was originally recommended as an indicator of relevant sleep disturbances (Buysse et al., Citation1989), but a later study has suggested a cutoff of 6 instead to maximize the specificity (Backhaus, Junghanns, Broocks, Riemann, & Hohagen, Citation2002). Therefore, we use the cutoff point of 6 to calculate the proportion of the sample who report having relevant sleep disturbances.
Neuropsychological test battery
All participants were tested with a comprehensive neuropsychological test battery after inclusion and again after 12 months. The tests used in the present study were those on which the performance of the patients improved from baseline to 12-month follow-up after adjusting for the change in performance in a group of healthy controls who were tested at the same two occasions. The two tests were (1) processing speed (Wechsler Adult Intelligence Scale III) (Wechsler, Citation1997) and (2) a self-made test of prospective memory – the ability to remember to perform an intended action at a particular point in the future (Eskildsen et al., Citation2016). The prospective memory test proceeded throughout the entire test session (approx. 1½ hour) and implied that the respondent was instructed to try to remember to give the test examiner a piece of candy after each of the tasks in the test battery. The tests are described in detail elsewhere (Eskildsen, Andersen, et al., Citation2015).
Statistical analyses
Hypothesis 1: prediction of change in performance on processing speed and prospective memory
To examine if change in perceived stress (PSS-10) and sleep quality (PSQI) could predict change in performance on processing speed and prospective memory, we conducted several linear regression analyses. Change in PSS-10 and PSQI from baseline to 12-month follow-up was the independent variables (alone and combined) and results from the neuropsychological tests were the dependent variables. The models were checked by diagnostic plots of the residuals.
Hypothesis 2: prediction of change in self-reported cognitive complaints
The between-person component of a time-varying predictor corresponds to the effect of the overall level of the predictor across individuals (e.g. patients with a high level of the predictor variable would also be expected to have a high level of the outcome variable) while the within-person component corresponds to the effect of change in the predictor on change in the outcome over time (a high degree of change in the predictor variable within a given individual is associated with a high degree of change in the outcome variable within the same individual) (Curran & Bauer, Citation2011). Curran and Bauer (Citation2011) have suggested estimating the between- and within-person components of one or more time-varying predictors on a time-varying outcome by a two-step regression approach, where one would first fit a random coefficient model to the predictors, estimate the individual intercepts, and then secondly use these intercepts as regressors in a regression model for the outcome. There are, however, two disadvantages to this approach, which are discussed in the supplementary information. In this study, we apply a multivariate random coefficient model to model the interdependence of the scores directly (Demidenko, Citation2013). In this approach, the individual development in CFQ, PSS-10, and PSQI is assumed to follow a linear curve with an individual intercept and slope. A subject’s intercept and slope are interpreted as the individual level (the between-person component) and change (the within-person component), respectively.
We used the multivariate random coefficient model to examine whether within-person change in PSS-10 and PSQI (alone and combined) was predictive of concurrent change in CFQ after adjusting for the between-person components of the predictors. An additional moderation analysis was carried out to test if there was an interaction of PSQI level and change in PSS-10 on change in CFQ.
To explore the timeline in the association between PSS-10, PSQI, and CFQ, we performed similar analyses with lagged time (i.e. where the outcome was change in CFQ the following month). We estimated the effect of time and entered the lagged covariate (i.e. PSS-10 and/or PSQI at the previous time point). Initially, as the size of the lags was uneven (one or three months) and to account for any heterogeneous effect during the progression of time, we included time as an effect modificator.
To explore if the relation between the predictors and CFQ was bidirectional, we also performed the reversed analyses with change in CFQ as the predictor and subsequent change in PSS-10 and PSQI as the outcome.
The data analyses and model validation are described in detail in the supplementary information.
Ethics
All participants gave their written consent and the study was approved by the Danish Data Protection Agency. All procedures were carried out in accordance with the Helsinki Declaration.
Results
Demographic and clinical characteristics of the sample
The demographic and clinical characteristics of the 60 patients recruited can be seen in . One patient failed to complete the PSQI at baseline. The mean score for the PSQI total score was calculated using single mean imputation for one patients who left one item unanswered at all time points (item 5j: During the past month, how often have you had trouble sleeping because you… Other reasons). A total of one, four, and three patients failed to complete the three questionnaires at 2-, 9-, and 12-month follow-up, respectively, and four patients failed to show up to the re-test session at 12-month follow-up. The patients who dropped out of the study before the re-test tended to score lower than completers on the prospective memory test at baseline (difference = 22.02 [95% CI: −0.95: 45.00], p = .06) but, otherwise, there were no differences between dropouts and completers in regard to the variables used in this study (Eskildsen et al., Citation2016).
Table 1. Demographic and clinical characteristics of the sample.
At baseline, 76% of the patients scored higher than 6 on the PSQI, which indicates clinically relevant sleep disturbances (Backhaus et al., Citation2002). The same was true for 40% at follow-up.
Hypothesis 1: prediction of change in performance on processing speed and prospective memory
lists the results of the linear regression analyses between change in PSS-10 and PSQI and change in neuropsychological test performance. All regression coefficients were positive but the only statistically significant finding was that change in PSS-10 (alone and when adjusting for change in PSQI) was associated with change in processing speed (p < .05).
Table 2. Linear regression analyses with change in perceived stress (PSS) and sleep quality (PSQI) as predictors of change in processing speed and prospective memory.
Hypothesis 2: prediction of change in self-reported cognitive complaints
By fitting a multivariate random coefficient model to the longitudinal responses, we obtained estimates of the population intercepts and slopes of the three measures (CFQ, PSS-10, and PSQI) separately and observed that all the three curves were significantly declining (p < .001). The estimates are given in the supplementary information.
contains the estimates of the within-person effects of PSS-10 and PSQI (alone and combined) on concurrent change in CFQ. The estimates are adjusted for the between-person effects.
Table 3. Within-person effects of PSS-10 and PSQI – alone and combined – on concurrent change in CFQ.
The effect of a one point increase in change in PSS-10 in a given individual is associated with a concurrent increase in change in CFQ of 1.79 (95% CI: 1.68, 1.91) after adjustment for the effect of baseline level of PSS-10. Adjusting for the effect of change in PSQI reduces the estimate to 1.36 (95% CI: 0.82, 1.91). Regarding the PSQI, the within-person effect is statistically significant only when entering the regression model without PSS-10. The adjusted R2 and the MSE suggest that the variation explained by the PSS-10 and PSQI is overlapping.
contains the results of the lagged analyses where we estimated the within-person effect of PSS-10 and PSQI on subsequent change in CFQ (1 month later).
Table 4. Within-person effects of perceived stress (PSS) and sleep quality (PSQI) – alone and combined – on subsequent (lagged) change in cognitive complaints (CFQ).
The effect of within-person change in the predictors is statistically significantly associated with subsequent change in CFQ. But again, PSQI is only a statistically significant predictor of change in CFQ when entering the regression without the PSS-10. A one-point change in PSS-10 is associated with a 0.35 point change in CFQ the following month.
When performing the reversed analysis, we observed that within-person change in CFQ was also predictive of subsequent change in PSS-10 (b = 0.11 [95% CI: 0.06, 0.17], p < .001) and PSQI (b = 0.05 [95% CI: 0.02, 0.08], p < .001) indicating a bidirectional association between PSS-10, PSQI, and CFQ.
Testing for interaction between level of PSQI and change in PSS on change in CFQ did not give cause to reject the hypothesis that there was no effect modification (p = .06). Details and effect estimates can be found in the supplementary information.
Discussion
This study followed a group of patients with prolonged work-related stress from their initial contact to an occupational health clinic and the subsequent 12 months and examined the role of perceived stress and sleep quality in predicting cognitive impairments during the follow-up period.
Concerning our first hypothesis that change in perceived stress and sleep quality from baseline to 12-month follow-up would be associated with change in performance on the tests of processing speed and prospective memory; we only partly confirmed this hypothesis. Even though all regression coefficients were positive as hypothesized, the associations were weak and only the association between change in perceived stress and change in processing speed was statistically significant. Nevertheless, the size of the associations was comparable to the findings from the study by Ahrberg et al. (Citation2012), who examined the association between pre-exam stress level, sleep quality, and exam performance. In a previous paper on cross-sectional data from the same sample (Eskildsen, Andersen, et al., Citation2015), we have examined if the level in PSS-10 was associated with performance on a broad neuropsychological test battery. We failed to find a statistically significant association. In this study where we examined the association between change on the PSS-10 and change on the two tests from the test battery, on which the patients improved, we found a statistically significant association. This fact indicates that the within-person association between PSS-10 and performance on the test of processing speed is stronger than the between-person association in this sample.
Regarding our second hypothesis, within-person change in PSS-10 and PSQI predicted concurrent change in CFQ after adjusting for the baseline level of PSS-10 and PSQI, respectively. When PSS-10 and PSQI are entered together in the model, PSS-10 seems to be the most important predictor of change in performance on the tests and self-reported cognitive complaints. The R2 and MSE seem to suggest that PSQI does not contribute very much in predicting change in CFQ when PSS-10 is already in the model. The fact that PSS-10 seems to be a stronger predictor of cognitive impairments is in line with the above-mentioned study (Ahrberg et al., Citation2012).
The estimated monthly change on PSS-10 and PSQI (see the supplementary information) and the estimates of the within-person effect of PSS-10 and PSQI on concurrent change in CFQ () specify that CFQ is expected to decrease 1.36 × 0.64 + 1.32 × 0.26 = 1.21 points per month. This estimate corresponds to a predicted change in CFQ of 14.52 points during the 12 months period. Since the observed mean change in CFQ was 14.8, the combined effect of within-person change in PSS-10 and PSQI on CFQ seems to be clinically relevant.
Regarding the effect of within-person change in PSS-10 and PSQI on subsequent change in CFQ (the following month or quarter), the estimates were a lot smaller compared to the estimates concerning prediction of concurrent change in CFQ, but both change in PSS-10 (alone and combined) and PSQI (alone) were statistically significant.
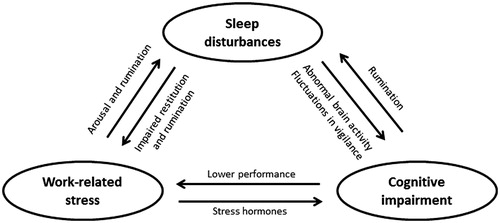
To test whether the relationship between the two predictors and the outcome was unidirectional or bidirectional, we also estimated whether CFQ could predict subsequent change in PSS-10 and PSQI. We found a small but statistically significant association, which suggests that the relationship between CFQ, PSS-10, and PSQI is bidirectional. This is perhaps not surprising since it seems likely that cognitive impairments can maintain work-related stress and hinder recovery by decreasing the ability of the individual to manage work assignments and through ruminations about cognitive impairments at bedtime, which in turn can impair sleep. This bidirectionality is illustrated in . The figure suggests that prolonged work-related stress can have direct effects on cognitive functions by the effect of stress hormones such as cortisol (Lupien, Gunnar, McEwen, & Heim, Citation2009). In addition, prolonged work-related stress can impair sleep through physiological arousal and increased ruminations. Impaired sleep, though, is not only a symptom of prolonged stress, but seems to maintain stress by hindering the restitution and probably also by increasing ruminations about lack of sleep (Grossi et al., Citation2015). The results from this study are not convincing evidence for the right arrow in (from sleep disturbances to cognitive impairments), however, and this relationship should be further studied.
Figure 1. The hypothesized relationship between work-related stress, sleep disturbances, and cognitive impairments.
Summing up, our results suggest that change in PSS-10 over a period of 12 months predicts change in CFQ and, to a lesser extent, change in performance on neuropsychological tests of processing speed. Change in PSQI is also predictive of change in CFQ but not of change in performance on tests of processing speed or prospective memory.
A possible explanation for the weaker association between performance on neuropsychological tests and perceived stress and PSQI, respectively, could be that the mean improvement in performance on the tests, after adjusting for learning effects, is relatively small in this sample (Eskildsen et al., Citation2016). It is also possible that the cognitive impairments in this patient group are not caused or maintained by stress or sleep problems and that the close association between the self-reported measures is caused by common method variance bias and/or that the CFQ is measuring worries about own cognitive abilities rather than measuring cognitive abilities per se (Wilhelm, Witthöft, & Schipolowski, Citation2010). The last-mentioned explanation would suggest that a decreasing level of PSS-10 or PSQI would mean a decreasing level of worries about own cognitive abilities instead of an improvement in actual abilities. Another explanation could be that the test results are a poor indicator of change in cognitive function. Test performance on a given day and time is to some extent influenced by contextual factors and by motivation and fatigue at that specific time point. It is also possible that several of the patients with cognitive problems in everyday life can maintain their normal level of functioning for a short time as when being tested but not in the long run during the whole day. Furthermore, in the test session, the respondent benefits from the fact that the test examiner plans, leads and structures the tasks on behalf of the respondent and there are no or few distractions during a test session. In daily life, however, the individual is dependent upon own initiative and ability to plan and organize the day.
The strengths of this study were the longitudinal design with the separation of the between-person and within-person effect of the predictors which makes a more exact investigation of the change processes during recovery from prolonged work-related stress possible. Furthermore, we explored the timing of the change processes and whether or not change in perceived stress and sleep predicted subsequent change in cognitive impairments. In addition, we used both self-reported and objective measures of cognitive impairments which reduced the risk of common method variance bias. Unfortunately, we did not have more than two test sessions, and therefore, we were not able to include objective cognitive impairments in the multivariate random coefficient analyses, and consequently, common method variance can still bias these results by enlarging the association between perceived stress, sleep, and cognitive complaints as mentioned above. In this respect, the validity of the self-reported sleep quality also merits a discussion. Previous data from a sleep lab have demonstrated that, although self-reported sleep estimates in the morning are correlated with recordings from the lab, fewer than one in five patients with complaints of very short sleep length or very long sleep latency will have the complaint confirmed in a laboratory sleep recording (Carskadon et al., Citation1976). One of the reasons for the relatively low correlation between self-reported and objective sleep measures could be that periods with light sleep or repeated arousals are misinterpreted as waking states (Carskadon et al., Citation1976; Harvey & Tang, Citation2012). In addition, the risk of memory distortion is also present because of the retrospective nature of the scale. Nevertheless, the PSQI is considered to be a useful first-line, easy-to-handle, and time-efficient questionnaire to evaluate sleep disturbances and is one of the two most commonly used and recommended sleep questionnaires (Backhaus et al., Citation2002; Buysse, Ancoli-Lsrael, Edinger, Lichstein, & Morin, Citation2006; Cox & Olatunji, Citation2016).
Another important limitation is the relatively small sample and resulting low power in the analyses concerning hypothesis 1, which meant that the confidence intervals around the estimates were large and might have led to a type II error.
Regarding the time-lagged analyses, the small estimates of the within-person effects could possibly be explained by the long time duration between the measurements (1 month in the first quarter and thereafter 3 months between the completions of the questionnaires). Since change in stress and sleep might affect cognitive function immediately (within days or weeks), there is a risk that we were not able to detect this in our data. We would probably have exhausted the patients, though, if we had asked them to complete the scales every week for several months which may have left us with a lot of missing data.
In conclusion, the extent of improvement in perceived stress and sleep quality predicted concurrent and subsequent improvement in self-reported cognitive complaints but not, convincingly, the improvement in performance on the neuropsychological tests.
The results could suggest that improvement in perceived stress mediate the improvement in cognitive impairments. A part of this association could be further mediated by improvement in sleep quality. This cannot be clarified in just one study, though, but has to draw on a series of studies often from different disciplines and study designs (Kazdin, Citation2007). For instance, the role of sleep disturbances could be further examined, by randomizing patients with work-related stress and cognitive impairments to treatment as usual or treatment incorporating sleep interventions to examine if cognitive impairments are reduced more in the group who receives the sleep intervention.
Whether the self-reported cognitive complaints or performance on the cognitive test is the most valid measure of true cognitive impairment in this patient group remains unclear and therefore, cognitive function should preferably be measured with both objective and self-reported measures.
Anita_Eskildsen_et_al_supplemental_content.zip
Download Zip (177.4 KB)Acknowledgements
The study was funded by The Danish Working Environment Research Fund (project number: 36-2011-09) and The Health Research Fund of Central Denmark Region. We thank the patients and controls participating in the study.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Ahrberg, K., Dresler, M., Niedermaier, S., Steiger, A., & Genzel, L. (2012). The interaction between sleep quality and academic performance. Journal of Psychiatric Research, 46, 1618–1622. doi:10.1016/j.jpsychires.2012.09.008
- Åkerstedt, T., Lekander, M., Petersen, H., Kecklund, G., & Axelsson, J. (2014). Sleep polysomnography and reported stress across 6 weeks. Industrial Health, 52, 36–42. doi:10.2486/indhealth.2013-0169
- Backhaus, J., Junghanns, K., Broocks, A., Riemann, D., & Hohagen, F. (2002). Test–retest reliability and validity of the Pittsburgh Sleep Quality Index in primary insomnia. Journal of Psychosomatic Research, 53, 737–740. doi:10.1016/S0022-3999(02)00330-6
- Bech, P., Gram, L.F., Dein, E., Jacobsen, O., Vitger, J., & Bolwig, T.G. (1975). Quantitative rating of depressive states. Acta Psychiatrica Scandinavica, 51, 161–170. doi:10.1111/j.1600-0447.1975.tb00002.x
- Broadbent, D., Cooper, P., FitzGerald, P., & Parker, K. (1982). The Cognitive Failure Questionnaire and its correlates. British Journal of Clinical Psychology, 21, 1–16. doi:10.1111/j.2044-8260.1982.tb01421.x
- Broughton, A. (2010). Work-related stress. Dublin, Ireland: European Foundation for the Improvement of Living and Working Conditions.
- Buysse, D.J., Ancoli-Lsrael, S., Edinger, J.D., Lichstein, K.L., & Morin, C.M. (2006). “Recommendations for a standard research assessment of insomnia”: Erratum. Sleep: Journal of Sleep and Sleep Disorders Research, 29, 1380. doi:10.1093/sleep/29.9.1155
- Buysse, D.J., Reynolds, C.F., Monk, T.H., & Berman, S.R. (1989). The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Research, 28, 193–213. doi:10.1016/0165-1781(89)90047-4
- Carskadon, M.A., Dement, W.C., Mitler, M.M., Guilleminault, C., Zarcone, V.P., & Spiegel, R. (1976). Self-reports versus sleep laboratory findings in 122 drug-free subjects with complaints of chronic insomnia. The American Journal of Psychiatry, 133, 1382–1388. doi:10.1176/ajp.133.12.1382
- Cohen, S., Kamarck, T., & Mermelstein, R. (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24, 385–396. doi:10.2307/2136404.
- Cox, R.C., & Olatunji, B.O. (2016). A systematic review of sleep disturbance in anxiety and related disorders. Journal of Anxiety Disorders, 37, 104–129. doi:10.1016/j.janxdis.2015.12.001
- Curran, P.J., & Bauer, D.J. (2011). The disaggregation of within-person and between-person effects in longitudinal models of change. Annual Review of Psychology, 62, 583–619. doi:10.1146/annurev.psych.093008.100356
- Dalgaard, L., Eskildsen, A., Carstensen, O., Willert, M.V., Andersen, J.H., & Glasscock, D.J. (2014). Changes in self-reported sleep and cognitive failures: A randomized controlled trial of a stress management intervention. Scandinavian Journal of Work, Environment & Health, 40, 569–581. doi:10.5271/sjweh.3460
- Demidenko, E. (2013). 1948-Mixed models: Theory and applications with R (2nd ed.). Hoboken, NJ: Wiley.
- Derogatis, L.R. (1977). SCL-90-R: Symptom Checklist-90-R. Administration, scoring and procedures manual (1st ed.). Minneapolis, MN: National Computer Systems.
- Eskildsen, A., Andersen, L.P., Pedersen, A.D., & Andersen, J.H. (2016). Cognitive impairments in former patients with work-related stress complaints – One year later. Stress (Amsterdam, Netherlands), 19, 559–566. doi:10.1080/10253890.2016.1222370
- Eskildsen, A., Andersen, L.P., Pedersen, A.D., Vandborg, S.K., & Andersen, J.H. (2015). Work-related stress is associated with impaired neuropsychological test performance: A clinical cross-sectional study. Stress (Amsterdam, Netherlands), 18, 198–207. doi:10.3109/10253890.2015.1004629
- Eskildsen, A., Dalgaard, V.L., Nielsen, K.J., Andersen, J.H., Zachariae, R., Olsen, L.R., … Christiansen, D.H. (2015). Cross-cultural adaptation and validation of the Danish consensus version of the 10-item Perceived Stress Scale. Scandinavian Journal of Work, Environment & Health, 41, 486–490. doi:10.5271/sjweh.3510
- Grossi, G., Jeding, K., Söderström, M., Osika, W., Levander, M., & Perski, A. (2015). Self-reported sleep lengths ≥ 9 hours among Swedish patients with stress-related exhaustion: Associations with depression, quality of sleep and levels of fatigue. Nordic Journal of Psychiatry, 69, 292–299. doi:10.3109/08039488.2014.973442
- Hamilton, M. (1960). A rating scale for depression. Journal of Neurology, Neurosurgery, and Psychiatry, 23, 56–62. doi:http://dx.doi.org/10.1136/jnnp.23.1.56.
- Harvey, A.G., & Tang, N.K.Y. (2012). (Mis)perception of sleep in insomnia: A puzzle and a resolution. Psychological Bulletin, 138, 77–101. doi:10.1037/a0025730
- Hoffman, L., & Stawski, R.S. (2009). Persons as contexts: Evaluating between-person and within-person effects in longitudinal analysis. Research in Human Development, 6, 97–120. doi:10.1080/15427600902911189
- Jonsdottir, I.H., Nordlund, A., Ellbin, S., Ljung, T., Glise, K., Währborg, P., & Wallin, A. (2013). Cognitive impairment in patients with stress-related exhaustion. Stress (Amsterdam, Netherlands), 16, 181–190. doi:10.3109/10253890.2012.708950
- Jovanovic, H., Perski, A., Berglund, H., & Savic, I. (2011). Chronic stress is linked to 5-HT(1A) receptor changes and functional disintegration of the limbic networks. Neuroimage, 55, 1178–1188. doi:10.1016/j.neuroimage.2010.12.060
- Kashani, M., Eliasson, A., & Vernalis, M. (2012). Perceived stress correlates with disturbed sleep: A link connecting stress and cardiovascular disease. Stress: The International Journal on the Biology of Stress, 15, 45–51. doi:10.3109/10253890.2011.578266
- Kazdin, A.E. (2007). Mediators and mechanisms of change in psychotherapy research. Annual Review of Clinical Psychology, 3, 1–27. doi:10.1146/annurev.clinpsy.3.022806.091432
- Lim, J., & Dinges, D.F. (2010). A meta-analysis of the impact of short-term sleep deprivation on cognitive variables. Psychological Bulletin, 136, 375–389. doi:10.1037/a0018883
- Linton, S.J., Kecklund, G., Franklin, K.A., Leissner, L.C., Sivertsen, B., Lindberg, E., … Hall, C. (2015). The effect of the work environment on future sleep disturbances: A systematic review. Sleep Medicine Reviews, 23, 10–19. doi:10.1016/j.smrv.2014.10.010
- Lupien, S.J., Gunnar, M.R., McEwen, B.S., & Heim, C. (2009). Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nature Reviews. Neuroscience, 10, 434–445. doi:10.1038/nrn2639
- Öhman, B.A., Nordin, S., Bergdahl, J., Birgander, L.S., & Neely, A.S. (2007). Cognitive functions in outpatients with perceived chronic stress. Scandinavian Journal of Work, Environment & Health, 33, 223–232. doi:10.5271/sjweh.1131
- Olsen, L.R., Mortensen, E.L., & Bech, P. (2007). Dokumentation for den danske udgave af SCL-90-R. In P. Hartmann (Ed.), SCL-90-R Vejledning til administration og scoring. Dansk Psykologisk Forlag.
- Reynolds, A.C., & Banks, S. (2010). Total sleep deprivation, chronic sleep restriction and sleep disruption. Progress in Brain Research, 185, 91–103. doi:10.1016/B978-0-444-53702-7.00006-3
- Sandström, A., Peterson, J., Sandström, E., Lundberg, M., Nyström, I., Nyberg, L., & Olsson, T. (2011). Cognitive deficits in relation to personality type and hypothalamic-pituitary-adrenal (HPA) axis dysfunction in women with stress-related exhaustion. Scandinavian Journal of Psychology, 52, 71–82. doi:10.1111/j.1467-9450.2010.00844.x
- Sandström, A., Rhodin, I.N., Lundberg, M., Olsson, T., & Nyberg, L. (2005). Impaired cognitive performance in patients with chronic burnout syndrome. Biological Psychology, 69, 271–279. doi:10.1016/j.biopsycho.2004.08.003
- Theadom, A., & Cropley, M. (2008). Dysfunctional beliefs, stress and sleep disturbance in fibromyalgia. Sleep Medicine, 9, 376–381. doi:10.1016/j.sleep.2007.06.005
- van Dam, A., Keijsers, G.P.J., Eling, Paul, A.T.M., & Becker, E.S. (2011). Testing whether reduced cognitive performance in burnout can be reversed by a motivational intervention. Work & Stress, 25, 257–271. doi:10.1080/02678373.2011.613648
- Van der Linden, D., Keijsers, G., Eling, P., & Van Schaijk, R. (2005). Work stress and attentional difficulties: An initial study on burnout and cognitive failures. Work & Stress, 19, 23–36. doi:10.1080/02678370500065275
- Van Dongen, H.P.A., Maislin, G., Mullington, J.M., & Dinges, D.F. (2003). The cumulative cost of additional wakefulness: Dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation. Sleep, 26, 117. doi:10.1093/sleep/26.2.117
- Wechsler, D. (1997). Wechsler adult intelligence scale (3rd ed.). San Antonio: The Psychological Corporation.
- Wilhelm, O., Witthöft, M., & Schipolowski, S. (2010). Self-reported cognitive failures: Competing measurement models and self-report correlates. Journal of Individual Differences, 31, 1–14. doi:10.1027/1614-0001/a000001
- Willert, M.V., Thulstrup, A.M., Hertz, J., & Bonde, J.P. (2010). Sleep and cognitive failures improved by a three-month stress management intervention. International Journal of Stress Management, 17, 193–213. doi:10.1037/a0019612
