Abstract
In this review it is discussed if acute stress can be fatal. The review is based on literature searches on PubMed, PsycINFO as well as Web of Science. Literature concerning the conditions excited delirium syndrome (ExDS), malignant catatonia, takotsubo cardiomyopathy (TCM), and capture myopathy (CM) is reviewed and compared. The aim of the article is to identify and discuss a possible fatalness as well as a common pathophysiology behind these conditions. This includes a deregulated autonomic nervous system, neurocardiac reasons for myocardial damage, and rhabdomyolysis. We conclude that these conditions could be different manifestations of the same pathophysiological phenomenon. In addition, we suggest that it is possible to die from acute stress, but that it requires a prior sensitization, as seen in cocaine abusers and certain psychiatric patients, to render individuals disposed to an extreme autonomic nerve reaction.
Lay summary
This article compares different conditions in humans and in other animals, where it appears as if the human or animal dies with no other reason than being submitted to an extreme condition of mental stress. The conditions examined via a literature search are excited delirium syndrome, malignant catatonia and takotsubo cardiomyopathy in humans, and a capture myopathy in different mammals.
The article theoretically suggests that one can die solely from acute stress, but that different forms sensitization probably goes ahead of such a fatal stress reaction. E.g. in cocaine addicts, some psychiatric patients, and in wild animals formerly subjected to stress an extreme sympathetic stress response might be immediately fatal. The article also theorizes that excited delirium syndrome, malignant catatonia, and capture myopathy could be more severe and acute variants of the temporary condition seen in takotsubo patients, also known as patients with broken heart syndrome.
Introduction
The notion that one can get scared to death is widespread in popular culture and has probably been a common understanding for centuries, yet from a scientific point of view this understanding is not widely accepted. In 1942, Walter Cannon tried to comprehend what by anthropologists was described as voodoo death in different indigenous tribes across the globe. In societies where magic was a part of the belief system and people were convinced that a spell could be deadly, people did indeed die after such spells were cast upon them. In some cases this was described as a swift death after a short period of extreme agitation. Cannon theorized that the mental distress caused by the firm belief that death was coming made the sympathetic-adrenal system overreact to such a degree that the blood pressure fell and the victim would consequently die (Cannon, Citation1942).
Today it is understood that an overreaction of the sympathetic-adrenal system is more likely to raise the blood pressure. Furthermore, this voodoo death has never been described under more controlled conditions (Lester, Citation2009). However, Cannon’s theory is worth mentioning as it might help explain other situations where humans and other species seem to die solely from acute mental stress. During his work on this subject, he discusses the fight and flight system. In modern society this system is useful in some situations when faced with actual danger, but it is also the mechanism that prevails in pathological anxiety.
Studies have shown that mammals and more specific primates can die from prolonged exposure to stress, showing gastric ulceration as a central pathology, but neural damage has also been shown postmortem (Uno, Tarara, Else, Suleman, & Sapolsky, Citation1989). There are examples where people have died following an extremely agitated state and no other explanation was found during the autopsy, as in excited delirium syndrome (ExDS) (Vilke, Payne-James, & Karch, Citation2012). In addition, the condition takotsubo cardiomyopathy (TCM) or broken heart syndrome is often initiated by mental stress and can have a fatal course (Yoshikawa, Citation2015).
We review conditions where the death of humans or animals has been closely connected to a state of extreme stress. ExDS, TCM, and malignant catatonia will be presented together with capture myopathy (CM), a similar condition described in animals. Through a comparison of the clinical features and postmortem findings we discuss if acute mental stress can in fact kill and what the underlying pathophysiology might be.
Method
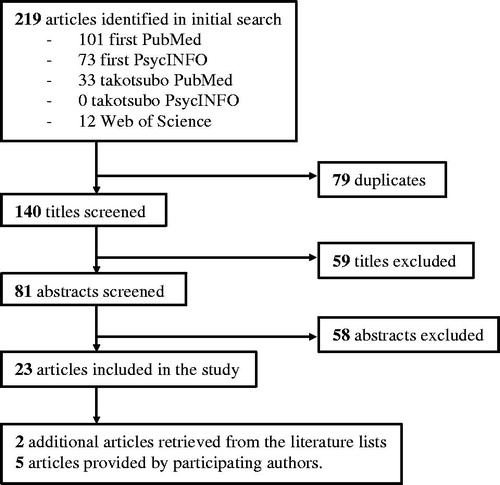
This study is based on two literature searches performed in June 2017, both on PubMed and on PsycINFO. One with the keywords: excited delirium or malignant catatonia or capture myopathy and death. Restrictions on the search were English as language and publication date after 1997. The search included clinical trials as well as reviews. The other search was with the words: takotsubo and death, with the additional restriction of only review articles, as this is a fairly thoroughly examined topic compared to the others. As PubMed and PsycINFO might not cover broadly within zoology and veterinary science, an additional search within these categories was made on Web of Science with the keywords: capture myopathy and death, with the same restrictions as before, see appendix. Hereafter duplicates and titles obviously not relevant to the subject were eliminated. Abstracts were then read through leaving only relevant articles as the basis for this study. Exclusion of abstracts were made when articles didn't address the relevant conditions, only addressed treatment or prevention, or did not address the fatality or pathophysiology of these conditions. Additional articles were found through literature lists, primarily important articles from before the time limit of the literature search, and through the participating authors.
Results
The literature search identified 219 articles with 79 duplicates. Fifty nine titles were excluded, 81 abstracts were read, and 23 were judged relevant to this study. Two articles from the literature lists were regarded as relevant and also included. Five additional articles were provided from the participating authors (see ). The articles are presented in and discussed below according to subject.
Table 1. Description of articles found in the literature search.
Capture myopathy
In the 1950–60s fatal stress reaction was defined in captured wild animals as a condition characterized by acidosis, muscular necrosis, and myoglobinuria followed by death within minutes to weeks. It is observed across species and suggested that the human equivalent might be exertional rhabdomyolysis (Spraker, Citation1993). However, not all deaths from CM occur after the animal has been chased. It is widely accepted within zoology, that the stress reaction plays a vital role in CM and that it is not only caused by the physical exertion (Blumstein et al., Citation2015; Paterson, Citation2014; Spraker, Citation1993). In mousedeer, it has been reported that direct human contact causes extreme stress followed by sudden death within 90 seconds (Semrau, Verstappen, Wolters, Szánthó, & Hoyer, Citation2010, p. 77). In the light of this CM has been suggested as a model for stress-induced cardiomyopathy or TCM in humans (Blumstein et al., Citation2015).
Four types of CM are described in the literature, differing mainly in the time from stress exposure until death and the extent of skeletal and cardiac muscle fiber damage (Spraker, Citation1993). The suggested pathophysiology behind them is a combination of fear, activation of the sympathetic nervous system, and the endocrine adrenal system together with muscular activity. A crucial role of acute stress as a fatal mechanism is primarily likely in the two types of CM that have a short timespan from stress exposure to death: capture shock syndrome (CSS) and delayed per acute syndrome (DPS). In CSS the animal dies while restrained or up to 6 hours later and the condition is characterized by the animals fervent attempt to escape and then suddenly lying motionless with rapid and shallow breathing, tachycardia, a weak pulse, and hyperthermia (Spraker, Citation1993). DPS occurs after an initial stress exposure and in response to a new stress exposure, in which the animal briefly attempts to escape, but then suddenly stops resisting, stands, or lies still, has dilated pupils, and within few minutes dies in ventricular fibrillation (Montane, Marco, Manteca, Lopez, & Lavin, Citation2002; Spraker, Citation1993). In both conditions, aspartate aminotransferase, lactate dehydrogenase, and creatinine kinase (CK) blood levels are elevated. In CSS there are small areas of necrosis and occasionally small thrombi in the capillaries in the skeletal muscle as well as in the viscera, and in cardiac muscle (Spraker, Citation1993). However, in DPS there are no or only a few lesions corresponding to mild rhabdomyolysis and only in the skeletal muscle fibers (Montane et al., Citation2002; Spraker, Citation1993).
A considerable variation in sensitivity toward CM is found among species; indeed not all captured wild animals die. Generally a prey is more likely to die from CM than a predator (Blumstein et al., Citation2015; Paterson, Citation2014). Blumstein et al. (Citation2015) found in ungulates evolutionary traits of CM that might be beneficial when an animal has to flee from a predator, but also made the animal likely to die from CM. These were: larger brains, rapid acceleration, living in larger groups, and longer lifespan. From this it is suggested that animals that can react and run fast have an explosive but potentially fatal autonomic nervous response to acute stress (Blumstein et al., Citation2015). Vulnerability to CM has been evolutionary labile. Presumably, this reflects that the traits have been advantageous in some environments and a disadvantage in others (Blumstein et al., Citation2015). A highly reactive autonomic nervous system is advantageous in an environment where it is likely to be hunted by predators. In such environments an ungulate has a greater chance of surviving an explosive stress reaction and fleeing than surviving an interaction with a predator. However, in an environments without predators it might be more likely that the ungulate dies from the explosive stress reaction than from the dangers the animal meets and reacts to.
Pursuing the question whether one can die from an acute stress reaction it is relevant to consider to which degree humans have these traits. Animals other than humans rarely hunt humans in modern society, but possibly an explosive autonomic nervous system in certain vulnerable humans could be at work when they perceive extreme danger or other stressors.
Excited delirium syndrome
In the 1980s, Wetli and Fishbain (Citation1985) described a condition where humans died after an extreme and acute state of stress. They described how an increased incidence rate of this condition correlated with the introduction of cocaine in the USA (Mash, Citation2016; Schiavone et al., Citation2016; Vilke, Payne-James et al., Citation2012). Often recreational cocaine addicts that die from ExDS have cocaine in their blood, but in doses ten times lower than in deaths due to overdose (Wetli & Fishbain, Citation1985). After the introduction of the ExDS term it has also been used to describe a similar condition in non-cocaine using psychiatric patients, mainly with a diagnosis within the schizophrenic spectrum and with insufficient or incorrect medical treatment (Mash et al., Citation2009; Vilke et al., Citation2012).
While not recognized as a psychiatric diagnosis, ExDS is an official cause of death in forensic medicine (Takeuchi, Ahern, & Henderson, Citation2011; Vilke, Payne-James et al., Citation2012). Here ExDS is determined as the cause of death when no physiological cause is found during the autopsy, but a particular behavioral pattern is recognized leading up to the time of death. The deceased is usually a young man who uses cocaine regularly or has a psychiatric diagnosis (Mash et al., Citation2009; Samuel, Williams, & Ferrell, Citation2009). The behavioral pattern consists of bizarre, uncontrollable, and aggressive behavior with shouting, panic, fear, extreme physical activity, seemingly superhuman strength, and immunity to pain. In addition, a victim of ExDS has hyperthermia and diaphoresis (Gill, Citation2014; Lipsedge, Citation2016; Mash, Citation2016; Vilke et al., Citation2012). The victim has usually been in confrontation with the police or psychiatric staff and often been restrained for a period. Sometimes the victim dies in the agitated state, but more often they first become still with a shallow breathing (Mash et al., Citation2009; Vilke et al., Citation2012). This condition prevails for a while before cardiac arrest occurs and the person dies, usually in bradyasystolia (Vilke et al., Citation2012). Another study with 90 ExDS suspicious casualties found, that death occurred on average less than 1 hour after the first encounter with the police (Mash et al., Citation2009). The same study suggested two brain biomarkers to identify ExDS as the cause of death. One is a dopamine transporter site, which is less present in deceased persons with ExDS behavior prior to death than in deceased cocaine drug addicts without ExDS behavior before death and non-addict controls. The same group had increased levels of heat shock protein 70 (Hsp70) compared to the two other groups. This protein is present in the brain when body temperature reaches 39 °C, underscoring that ExDS is associated with hyperthermia (Mash et al., Citation2009). Finally, Schiavone et al. (Citation2016) suggested that oxidative stress from cocaine usage also plays a role in ExDS.
Malignant catatonia
Some of the earliest descriptions of catatonia noted that this condition sometimes came after a state of extreme excitement (Castillo, Rubin, & Holsboer-Trachsler, Citation1989). A patient suffering from malignant catatonia tends to shift between a state of extreme agitation often with non-directed aggressive behavior and a state of catatonic stupor, where the patient is motionless (Ghaziuddin, Hendriks, Patel, Wachtel, & Dhossche, Citation2017; Lipsedge, Citation2016; Moskowitz, Citation2004). During malignant catatonia most patients are autonomically unstable with abnormal alternating blood pressure, pulse, respiration rate, perspiration, and hyperthermia (Dhossche, Citation2014; Ghaziuddin et al., Citation2017). This is also observed in 40% of patients in the immobile catatonic state (Dhossche, Citation2014). Ghaziuddin et al. (Citation2017) estimate that 10–20% of patients with malignant catatonia die and usually during a phase of stupor (Moskowitz, Citation2004). In the literature malignant catatonia is synonymous with Bell’s mania, lethal catatonia, and manic delirium (Ghaziuddin et al., Citation2017). As early as 1927 Stauder defined lethal catatonia based on 27 patients that had an acute onset of agitation, excitement, clouded consciousness, and violent or self-destructive behavior. Later, these patients went into a more quiescent state in a cramped and rigid posture occasionally still trying to hurt themselves until they died apparently after being physically exhausted. This sequence of symptoms lasted between 4 and 14 days (Stauder in Castillo et al., Citation1989).
There are several theories of what causes catatonia. But relevant in this context is the theory that catatonia is an extreme fear response (Dhossche, Citation2014; Moskowitz, Citation2004). That benzodiazepines can successfully treat catatonia and that many patients describe their experiencing of malignant catatonia as states of intense anxiety supports this theory (Moskowitz, Citation2004). In “‘Scared stiff’: Catatonia as an evolutionary-based fear response” Moskowitz (Citation2004) argues that malignant catatonia is a deadly form of anxiety, and in that view, one can be scared to death. Moskowitz argues that the immobile state of catatonia is an unadjusted primitive reaction, which in a modern context becomes pathological and is a reaction to fearful situations where the immobility makes no sense (Moskowitz, Citation2004).
Takotsubo cardiomyopathy
TCM is a recognized, sub-acute, and often transitional syndrome where mental stress causes a heart condition with an in-hospital mortality rate around 4.5% (Singh et al., Citation2014). It was first defined by Japanese researchers in 1990 and has clinical manifestations resembling acute coronary syndrome (ACS), but with normal coronary arteries.
Transient left ventricular wall motion abnormalities characterize the pathology. In about 80% of the cases there is akinesia or dyskinesia with ballooning of the apical half of the left ventricle. In the remaining cases, the abnormal wall motion is in the mid-ventricular or basal region. In most cases the left ventricular function is normalized within four to eight weeks. (Templin et al., Citation2015). Some form of stress usually precedes the condition, but in about one-third of the cases it is not possible to identify any specific stressor (Roshanzamir & Showkathali, Citation2013; Silva et al., Citation2009; Templin et al., Citation2015; Yoshikawa, Citation2015). TCM has been associated with perioperative stress, sepsis, drug abuse, thyrotoxicosis, the death of an immediate family member, surprise parties, and lightning strikes (Yoshikawa, Citation2015). Compelling for this review there have been cases of cocaine-induced TCM (Otahbachi, Cevik, Bagdure, & Nugent, Citation2010). According to Templin et al. (Citation2015) 36% of the triggers are physical and 27% are emotional. In a few cases, TCM has been related to strong positive emotions (Ghadri et al., Citation2016). TCM is associated with relatively low early mortality as compared to the fatal progress described in the cases of CM and ExDS. In the acute phase the TCM patients can suffer from ventricular arrhythmias and in rare cases even cardiac rupture (Otahbachi et al., Citation2010; Roshanzamir & Showkathali, Citation2013; Templin et al., Citation2015; Yoshikawa, Citation2015). A few patients die from progressive heart failure within the first 30 days. However, TCM is associated with substantial long-term mortality exceeding that of a population with acute ST-elevation myocardial infarction (Stiermaier et al., Citation2016). About 90% of TCM cases are post-menopausal women, which suggests that hormonal factors may play a role in this condition (Roshanzamir & Showkathali, Citation2013; Silva et al., Citation2009).
Discussion – possible pathophysiological similarities
In the following section the possible pathophysiology behind the different potentially fatal conditions mentioned in this article and their similarities are discussed. The physiological and behavioral symptoms characteristic of the different conditions are compared in .
Table 2. Summarizing selected characteristics from the four conditions: timespan from debut of symptoms till death – or recovery in most TCM cases –, physiological symptoms, selected post-mortal findings, and behavioral characteristics.
One shared pathophysiological mechanism is an extreme autonomic stress reaction. Whether and how the resulting catecholamine release has a role in the fatality of these conditions is debated in the literature. An overloaded physiological stress reaction, sympathetic and adrenal, appears to trigger the four conditions CM, ExDS, malignant catatonia, and TCM. In CM elevated catecholamine levels play a central role but how death occurs is different depending on the type of CM. In CSS the extended sympathetic stimuli end in a shock condition with low blood pressure, decreased venous return, and decreased cardiac output. This results in a vicious circle that eventually leads to an insufficient supply of oxygen and nutrients to the myocardium (Spraker, Citation1993).
In DPS it is suggested that during the first stressor the animal is subjected to a mild form of rhabdomyolysis without clinical signs, but enough to cause hyperkalemia. This results in an abnormal polarization of the cardiac muscles. When the animal again is subjected to stress and the catecholamines hit the heart the result is ventricular fibrillation and cardiac arrest (Spraker, Citation1993). A mild form of rhabdomyolysis may also play a role in the fatality of ExDS, as survivors of the acute stress condition are seen to develop acidosis and rhabdomyolysis (Takeuchi et al., Citation2011). Elevated levels of CK is also observed in TCM (Roshanzamir & Showkathali, Citation2013) and in malignant catatonia (Daniels, Citation2009).
From the findings of a loss of dopamine transporter sites by Mash et al. (Citation2009) it is concluded that people subjected to ExDS, cocaine addicts as well as non-users, have an impaired ability to regulate dopamine stimulation (Mash et al., Citation2009; Takeuchi et al., Citation2011). Therefore, they are susceptible to large and unregulated dopamine stimulations, which could initiate the hyperactive behavior (Mash, Citation2016; Mash et al., Citation2009; Schiavone et al., Citation2016; Takeuchi et al., Citation2011; Vilke, Payne-James et al., Citation2012). This dopamine theory also offers an explanation as to why psychiatric patients, specifically patients with a schizophrenia diagnosis can get ExDS. Since these patients, according to the hyper dopamine hypothesis, have problems with central dopamine regulation (Mash, Citation2016; Vilke et al., Citation2012; Vilke, Payne-James et al., Citation2012). A similar theory could be applied to patients suffering from malignant catatonia, as these often have a known psychiatric disorder. Similar to victims of ExDS, there is a higher prevalence of psychiatric disorders, but also neurologic disorders, among TCM patients compared to patients with ACS (Templin et al., Citation2015).
However, a dysfunctional dopamine system does not in itself explain the fatality of the conditions. In ExDS it has been suggested that the deadly pathophysiology could be a dysfunctional autonomic nervous system caused by the deregulated dopamine system. As with CM the theory is that overstimulation of the sympathetic nervous system results in cardiac arrest (Mash, Citation2016; Mash et al., Citation2009), though in CM signs of dopaminergic dysfunction preceding such overstimulation has not been reported. An underlying mechanism could be that catecholamines released during such an overreaction have a damaging effect directly on the cardiomyocytes, on the coronary microvasculature, or on both (Lipsedge, Citation2016; Nugent, Orellana-Barrios, & Buscemi, Citation2017).
A dominating theory regarding the pathophysiology of TCM is that the precedent stressor induces an extreme sympathetic nervous response which gives the heart a “neurogenic stunning” (Yoshikawa, Citation2015, p. 300). The plasma concentration of catecholamines is elevated, even compared to the levels found associated with myocardial infarction (Silva et al., Citation2009; Yoshikawa, Citation2015). It is thought that this elevation causes transient myocardial stunning which explains the abnormal left ventricular wall motion in TCM (Roshanzamir & Showkathali, Citation2013; Silva et al., Citation2009; Singh et al., Citation2014; Templin et al., Citation2015). Furthermore, local cardiac concentrations of catecholamines at the coronary sinus have been measured to be higher than at the aortic root, suggesting damaging high levels of catecholamines to originate from the cardiac sympathetic nervous endings (Otahbachi et al., Citation2010; Yoshikawa, Citation2015).
In cardiac biopsies from autopsies of patients dying after TCM, necrosis of contraction bands has been found. These are early and minimal myocardial damages that probably are temporary like the ventricular wall motion abnormalities in surviving TCM patients (Fineschi et al., Citation2010; Otahbachi et al., Citation2010; Yoshikawa, Citation2015). In experiments subjecting animals to stress, e.g. repeated restraining, it has been shown that stress alone can cause minimal myocardial damage with contract band necrosis suggesting a hyper contracted state of the myocardium. These damages are more concentrated near the autonomic nerve endings and more widespread in the left ventricle where nerve endings are abundant (Samuel et al., Citation2009). Contraction band necrosis is also observed 5–10 min after experimental infusion of catecholamines in myocardial tissue (Fineschi et al., Citation2010; Samuel et al., Citation2009). That a sympathetic response with catecholamine release can cause contraction band necrosis in cardiac muscle tissue has also been shown in different patients undergoing extreme physiological stress before death (Nugent et al., Citation2017; Otahbachi et al., Citation2010). Cocaine addicts are prone to have similar damages in their myocardium and this might make their hearts more vulnerable to ExDS and high concentrations of catecholamines (Lipsedge, Citation2016; Takeuchi et al., Citation2011). Such a neurologic-cardiac connection could offer part of an explanation to cardiac death in ExDS victims if they suffer from a lost ability to autoregulate their autonomic nervous system (Mash et al., Citation2009; Takeuchi et al., Citation2011; Vilke, Payne-James et al., Citation2012). In CM, damage to the cardiac muscle tissue has been found in CSS but not in DPS (Spraker, Citation1993). As mentioned the minimal myocardial damage described above is not severe enough to be the sole cause of death. However, the combination of these damages and a severe autonomic nervous overreaction could result in fatal cardiac arrhythmias (Nugent et al., Citation2017; Samuel et al., Citation2009). This offers a possible pathophysiological background for the rare, deadly cases of TCM, for CM, and possibly also for ExDS as well as malignant catatonia although the presence of minimal myocardial damage has not been systematically examined in these cases.
Finally, Otahbachi et al. (Citation2010) speculate that a common pathophysiology underlies ExDS and TCM since echocardiography of hyperthermia patients have shown heart wall abnormalities similar to the ones observed in TCM. As mentioned ExDS patients suffer from hyperthermia.
In general, the literature includes few patients or animals and the reportings are limited by the emergent characteristics of the conditions. In addition there have never been any empirical comparisons between any of these conditions. Therefore, the hypotheses presented in this article are difficult to support with physiological evidence. The pathophysiological similarities of the conditions are mostly clinical observations and behavioral characteristics of the victims. An overview is available in .
Conclusion
In conclusion ExDS, malignant catatonia, and TCM could be different manifestations of a human form of CM. The behavioral and physiological patterns of ExDS and malignant catatonia share similarities with CM. More research, mainly on the cardiac manifestations of the conditions, is needed to confirm whether the different conditions described in this paper originate from the same pathophysiology. Such research should include genetic studies to examine predisposition to cardiac arrhythmias.
In this review we suggest that it is possible to die solely from acute stress but a multifactorial sensitization probably precedes such a fatal stress reaction. This sensitization could be a mild degree of rhabdomyolysis or catecholamine evoked cardiac damages like contract band necrosis. In cocaine addicts, psychiatric patients with impaired dopamine regulation, and in wild animals formerly subjected to stress an extreme sympathetic stress response might be immediately fatal. Malignant catatonia usually has a longer timespan than ExDS and the acute versions of CM. Perhaps this period of alternating states of mental stress serves as a sensitization, which gradually makes the patient vulnerable to suffer the same fate as victims of ExDS and acute CM.
After reviewing the literature we theorize that all three conditions could be more severe and acute variants of the transient cardiomyopathy seen in TCM patients. In light of this it would be intriguing to examine whether the abnormal wall motion of the left ventricle seen in TCM patients is also present in patients with malignant catatonia or ExDS.
Disclosure statement
The authors report no conflicts of interest.
Additional information
Notes on contributors
Solveig Baltzer Nielsen
Solveig Baltzer Nielsen is an MD in her internship and an MSc in Music, Mind and Brain.
Sharleny Stanislaus
Sharleny Stanislaus is an MD and psychiatric resident and Phd student.
Kari Saunamäki
Kari Saunamäki is MD and invasive cardiologist.
Carsten Grøndahl
Carsten Grøndahl is chief veterinarian at the Copenhagen Zoo.
Jytte Banner
Jytte Banner is an MD and professor of forensic pathology at the university of Copenhagen.
Martin Balslev Jørgensen
Martin Balslev Jørgensen is an MD and professor of clinical psychiatry at the University of Copenhagen.
References
- Blumstein, D.T., Buckner, J., Shah, S., Patel, S., Alfaro, M.E., & Natterson-Horowitz, B. (2015). The evolution of capture myopathy in hooved mammals: A model for human stress cardiomyopathy? Evolution, Medicine, and Public Health, 2015, 195–203. doi:10.1093/emph/eov015
- Cannon, W.B. (1942). “Voodoo” death. American Anthropologist, 44, 169–181. doi:10.1525/aa.1942.44.2.02a00010
- Castillo, E., Rubin, R.T., & Holsboer-Trachsler, E. (1989). Clinical differentiation between lethal catatonia and neuroleptic malignant syndrome. The American Journal of Psychiatry, 146, 324–328. doi:10.1176/ajp.146.3.324
- Daniels, J. (2009). Catatonia: Clinical aspects and neurobiological correlates. The Journal of Neuropsychiatry and Clinical Neurosciences, 21, 371–380. doi:10.1176/appi.neuropsych.21.4.371 10.1176/jnp.2009.21.4.371
- Dhossche, D.M. (2014). Vagal intimations for catatonia and electroconvulsive therapy. The journal of ECT, 30, 111–115. doi:10.1097/YCT.0000000000000134
- Fineschi, V., Michalodimitrakis, M., D’Errico, S., Neri, M., Pomara, C., Riezzo, I., & Turillazzi, E. (2010). Insight into stress-induced cardiomyopathy and sudden cardiac death due to stress. A forensic cardio-pathologist point of view. Forensic Science International, 194, 1–8. doi:10.1016/j.forsciint.2009.10.025
- Ghadri, J.R., Sarcon, A., Diekmann, J., Bataiosu, D.R., Cammann, V.L., Jurisic, S., … Templin, C. (2016). Happy heart syndrome: Role of positive emotional stress in takotsubo syndrome. European Heart Journal, 37, 2823–2829. doi:10.1093/eurheartj/ehv757
- Ghaziuddin, N., Hendriks, M., Patel, P., Wachtel, L.E., & Dhossche, D.M. (2017). Neuroleptic malignant syndrome/malignant catatonia in child psychiatry: Literature review and a case series. Journal of Child and Adolescent Psychopharmacology, 27, 359–365. doi:10.1089/cap.2016.0180
- Gill, J.R. (2014). The syndrome of excited delirium. Forensic Science, Medicine, and Pathology, 10, 223–228. doi:10.1007/s12024-014-9530-2
- Lester, D. (2009). Voodoo death. Omega – Journal of Death and Dying, 59, 1–18. doi:10.2190/OM.59.1.a
- Lipsedge, M. (2016). Excited delirium: A psychiatric review. Medicine, Science and the Law, 56, 121–127. doi:10.1177/0025802415579617
- Mash, D.C. (2016). Excited delirium and sudden death: A syndromal disorder at the extreme end of the neuropsychiatric continuum. Frontiers in Physiology, 7, 435. doi:10.3389/fphys.2016.00435
- Mash, D.C., Duque, L., Pablo, J., Qin, Y., Adi, N., Hearn, W.L., … Wetli, C.V. (2009). Brain biomarkers for identifying excited delirium as a cause of sudden death. Forensic Science International, 190, e13–e19. doi:10.1016/j.forsciint.2009.05.012
- Montane, J., Marco, I., Manteca, X., Lopez, J., & Lavin, S. (2002). Delayed acute capture myopathy in three roe deer. Journal of Veterinary Medicine Series A, 49, 93–98. doi:10.1046/j.1439-0442.2002.jv409.x
- Moskowitz, A.K. (2004). “Scared stiff”: Catatonia as an evolutionary-based fear response. Psychological Review, 111, 984–1002. doi:10.1037/0033-295X.111.4.984
- Nugent, K., Orellana-Barrios, M.A., & Buscemi, D. (2017). Comprehensive histological and immunochemical forensic studies in deaths occurring in custody. International Scholarly Research Notices, 2017, 9793528. doi:10.1155/2017/9793528
- Otahbachi, M., Cevik, C., Bagdure, S., & Nugent, K. (2010). Excited delirium, restraints, and unexpected death a review of pathogenesis. The American Journal of Forensic Medicine and Pathology, 31, 107–112. doi:10.1097/PAF.0b013e3181d76cdd
- Paterson, J. (2014). Zoo animal and wildlife immobilization and anesthesia. In G. West, D. Heard, N. Caulkett (Eds.), Zoo animal and wildlife immobilization and anesthesia. (2nd ed., pp. 171–179). Ames, IA: Willey.
- Roshanzamir, S., & Showkathali, R. (2013). Takotsubo cardiomyopathy a short review. Current Cardiology Reviews, 9, 191–196. doi:10.2174/1573403X11309030003
- Samuel, E., Williams, R.B., & Ferrell, R.B. (2009). Excited delirium: Consideration of selected medical and psychiatric issues. Neuropsychiatric Disease and Treatment, 5, 61–66. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2695211/.
- Schiavone, S., Neri, M., Mhillaj, E., Pomara, C., Trabace, L., & Turillazzi, E. (2016). The role of the NADPH oxidase derived brain oxidative stress in the cocaine-related death associated with excited delirium: A literature review. Toxicology Letters, 258, 29–35. doi:10.1016/j.toxlet.2016.06.002
- Semrau, A., Verstappen, F., Wolters, M., Szánthó, J., & Hoyer, M. (2010). (Manual). Husbandry manual lesser mousedeer (Tragulus javanicus – group) (2nd ed.). Amsterdam. European Association of Zoos and Aquaria.
- Silva, C., Goncalves, A., Almeida, R., Dias, P., Araujo, V., Gavina, C., & Maciel, M.J. (2009). Transient left ventricular ballooning syndrome. European Journal of Internal Medicine, 20, 454–456. doi:10.1016/j.ejim.2008.12.001
- Singh, K., Carson, K., Shah, R., Sawhney, G., Singh, B., Parsaik, A., … Horowitz, J. (2014). Meta-analysis of clinical correlates of acute mortality in takotsubo cardiomyopathy. The American Journal of Cardiology, 113, 1420–1428. doi:10.1016/j.amjcard.2014.01.419
- Spraker, T.R. (1993). Stress and capture myopathy in artiodactylids. In M. E. Fowler (Ed.), Zoo & wild animal medicine: Current therapy 3 (pp. 418–488). Denver, Colorado: W.B. Saunders Co.
- Stiermaier, T., Moeller, C., Oehler, K., Desch, S., Graf, T., Eitel, C., … Eitel, I. (2016). Long-term excess mortality in takotsubo cardiomyopathy: Predictors, causes and clinical consequences. European Journal of Heart Failure, 18, 650–656. doi:10.1002/ejhf.494
- Takeuchi, A., Ahern, T.L., & Henderson, S.O. (2011). Excited delirium. The Western Journal of Emergency Medicine, 12, 77–83. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3088378/.
- Templin, C., Ghadri, J.R., Diekmann, J., Napp, L.C., Bataiosu, D.R., Jaguszewski, M., … Lüscher, T.F. (2015). Clinical features and outcomes of Takotsubo (stress) cardiomyopathy. New England Journal of Medicine, 373, 929–938. doi:10.1056/NEJMoa1406761
- Uno, H., Tarara, R., Else, J.G., Suleman, M.A., & Sapolsky, R.M. (1989). Hippocampal damage associated with prolonged and fatal stress in primates. The Journal of Neuroscience: The Official Journal of the Society for Neuroscience, 9, 1705–1711. doi:10.1523/JNEUROSCI.09-05-01705.1989
- Vilke, G.M., DeBard, M.L., Chan, T.C., Ho, J.D., Dawes, D.M., Hall, C., … Bozeman, W.P. (2012). Excited delirium syndrome (ExDS): Defining based on a review of the literature. Journal of Emergency Medicine, 43, 897–905. doi:10.1016/j.jemermed.2011.02.017
- Vilke, G.M., Payne-James, J., & Karch, S.B. (2012). Excited delirium syndrome (ExDS): Redefining an old diagnosis. Journal of Forensic and Legal Medicine, 19, 7–11. doi:10.1016/j.jflm.2011.10.006
- Wetli, C.V., & Fishbain, D.A. (1985). Cocaine-induced psychosis and sudden death in recreational cocaine users. Journal of Forensic Sciences, 30, 873–880. doi:10.1520/JFS11020J
- Yoshikawa, T. (2015). Takotsubo cardiomyopathy, a new concept of cardiomyopathy: Clinical features and pathophysiology. International Journal of Cardiology, 182, 297–303. doi:10.1016/j.ijcard.2014.12.116
Appendix
First literature search entry on PubMed
(((excited[All Fields] AND (“delirium”[MeSH Terms] OR “delirium”[All Fields])) OR (“catatonia”[MeSH Terms] OR “catatonia”[All Fields] OR (“malignant”[All Fields] AND “catatonia”[All Fields]) OR “malignant catatonia”[All Fields])) OR (capture[All Fields] AND (“muscular diseases”[MeSH Terms] OR (“muscular”[All Fields] AND “diseases”[All Fields]) OR “muscular diseases”[All Fields] OR “myopathy”[All Fields]))) AND (“death”[MeSH Terms] OR “death”[All Fields]) AND ((“1997/01/01”[PDAT]: “3000/12/31”[PDAT]) AND English[lang]).
First literature search entry on PsycINFO
Boolean/phrase: excited delirium syndrome or malignant catatonia or CM and death. Limiters: Published Date: 19970101-20171231. Peer reviewed. English.
Takotsubo literature search entry on PubMed
(takotsubo) AND death AND (Review[ptyp] AND (“1997/01/01”[PDat]: “3000/12/31”[PDat]) AND English[lang]).
Takotsubo literature search entry on PsycINFO
Takotsubo cardiomyopathy AND death. Limiters: Published Date: 19970101-20171231. Peer reviewed. English. Document type: Review – any.
Search on web of science
TOPIC: (“capture myopathy”) AND TOPIC: (death). Refined by: WEB OF SCIENCE CATEGORIES: (VETERINARY SCIENCES OR ZOOLOGY). Timespan: 1997-2017. Indexes: SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI.