Abstract
Previous studies have found that PTSD is associated with hippocampal-related impairment in cognitive flexibility. However, little is known about this impairment following nature adventure interventions. The current ex post facto study aimed to examine the relationship between cognitive flexibility, sailing-based intervention and PTSD symptoms. Thirty-nine individuals with PTSD diagnosis (17 who engaged in sailing and 22 who did not engage in sailing) and 38 healthy control (18 who engaged in sailing and 20 who did not engage in sailing) completed a performance-based reversal learning paradigm to assess cognitive flexibility and were evaluated for PTSD, depressive and anxiety symptoms. The results revealed significantly lower levels of PTSD and trait anxiety symptoms in the PTSD-sailing group, compared to the PTSD-no-sailing group. In addition, both PTSD groups showed selective, though different, impairments in reversal learning. Specifically, PTSD-no-sailing individuals showed a selective impairment in reversing the outcome of a negative stimulus- they struggled to learn that a previously negative stimulus was later associated with a positive outcome. PTSD-sailing individuals, on the other hand, displayed a selective impairment in reversing the outcome of a positive stimulus- they had difficulty learning that a previously positive stimulus was later associated with a negative outcome. The results may suggest that although individuals who participated in a sailing-based intervention had lower clinical symptoms, their hippocampal related cognitive flexibility was mot improved, and the impairment exists in a different domain.
Introduction
Cognitive flexibility is the ability to dynamically adapt and change our reaction in accordance with different contextual demands (Baddeley, Citation2012). Recent research reveal that such ability is associated with hippocampal function and structure (Anacker & Hen, Citation2017; Burghardt, Park, Hen, & Fenton, Citation2012; Levy-Gigi, Szabo, Richter-Levin, & Kéri, Citation2015) and may be vital in determining the way individuals cope with stressful events (Fu & Chow, Citation2017; Haim-Nachum & Levy-Gigi, Citation2019; Ionescu, Citation2012). Indeed, trauma-exposed individuals with better cognitive flexibility show decreased PTSD symptoms, enhanced post-traumatic growth and higher life satisfaction compared to those with poor cognitive flexibility (Hijazi, Keith, & O’Brien, Citation2015; Joseph & Gray, Citation2011; Keith, Velezmoro, & O’Brien, Citation2015; Levy-Gigi et al., Citation2012; Metzl, Citation2009; Palm & Follette, Citation2011; Radell, Beck, Gilbertson, & Myers, Citation2017).
In a set of studies which evaluated the associations between post-traumatic stress disorder (PTSD) and cognitive flexibility we showed that both individuals with and without PTSD are equally able to acquire and retain positive and negative stimulus-outcome associations (Haim-Nachum & Levy-Gigi, Citation2019; Levy-Gigi, Richter-Levin, Okon-Singer, Kéri, & Bonanno, Citation2016; Levy-Gigi et al., Citation2012, Citation2015). However, only individuals with PTSD fail to reverse the acquired rules when the situation changes and learn that previously negative associations become positive. Moreover, this selective impairment negatively correlates with hippocampal volume (Levy-Gigi et al., Citation2015).
Interestingly, while studies revealed alterations in hippocampal volume following clinical interventions in PTSD (Dickie, Brunet, Akerib, & Armony, Citation2011; Levy-Gigi, Szabó, Kelemen, & Kéri, Citation2013; Zhu et al., Citation2018), it is not yet clear, whether such interventions are associated with behavioral implications. The present study is the first step towards this understanding, aiming to test differences in cognitive flexibility as a function of PTSD diagnosis and engagement in nature adventure rehabilitation intervention.
Nature adventure rehabilitation, is an outdoor group therapeutic approach based on physical activity intervention (Russell, Citation2001; Dietrich, Joye, & Garcia, Citation2015). Sailing-related intervention is based on the assumption that exposure to anxiety evoking (but not trauma-related) real-life situations may improve the way PTSD individuals cope with the deleterious effects of traumatic exposure (Caddick & Smith, Citation2014; Dietrich et al., Citation2015; Gelkopf, Hasson-Ohayon, Bikman, & Kravetz, Citation2013; Rosenbaum et al., Citation2015). It was found to be efficient in reducing PTSD and depressive symptoms, as well as improving social and emotional quality of life, daily functioning and sense of hope (Dietrich et al., Citation2015; Gelkopf et al., Citation2013). Here we tested whether PTSD individuals who took part in this intervention are also better in cognitive flexibility, as compared to PTSD individuals who did not get any treatment, healthy controls and individuals who sail as a hobby.
To that end we recruited participants from four groups differed as a function of PTSD diagnosis and Sailing intervention. We postulated that the PTSD-sailing group would exhibit less PTSD, depressive, and anxiety symptoms as compared to the PTSD no-sailing group. In addition, we predicted that in line with previous studies, all groups would equally be able to learn and retain positive and negative stimulus–outcome associations. However, the PTSD-sailing group would exhibit a better reversal learning from negative to positive outcome, and therefore greater cognitive flexibility as compared to the PTSD-no-sailing group.
Methods
Participants
Seventy-seven participants volunteered to take part in the study. Thirty-nine individuals diagnosed with chronic PTSD acknowledged by the Israeli department of defense; 17 of them took part in a sailing intervention (PTSD-sailing group) while the remained 22 matched for time of PTSD onset, had not participated in such activity (PTSD-no sailing group), 38 healthy controls; 18 individuals who participate in the same sailing activity but do it as a hobby (Control-Sailing group), and 20 individuals without such a hobby (Control-no-sailing group). The sailing intervention lasted one year and included one 4-hour session a week. The Control-Sailing group was active at the same club and spent in average the same amount of time. PTSD groups (sailing and no-sailing) had previous therapeutic experience including participation in supportive therapy and different types of CBT. However, no significant differences between the groups as a function of past therapeutic experiences (t(37) = .31, p = .76).
Demographic data of the sample is presented in . As can be seen, participants in all four groups were matched for gender and education. The mean age of the PTSD-sailing group was significantly higher compared to the mean age of the participants in the other groups. However, we controlled for these differences in our analyses. Exclusion criteria included any history of psychiatric or neurological disorders and current alcohol abuse or dependence. Investigation was carried out in accordance with the Declaration of Helsinki. The study design was reviewed by the appropriate ethical committee. All participants provided a written informed consent at the beginning of the experiment after the nature of the procedure was fully explained.
Table 1. Demographic characteristics of the sample.
Measures
The cue and context reversal paradigm
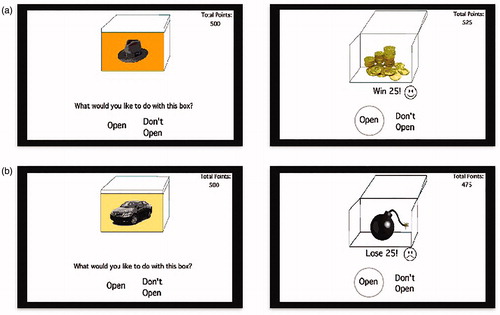
In this paradigm (Levy-Gigi et al., Citation2015) participants viewed a series of boxes on a computer screen (). On each box, a picture of a various objects, (cues, e.g. a hat) was presented against various color (context; e.g. orange). Each combination of cue and context (i.e. a box with a hat on an orange background or a box with a car on a yellow background) was associated with either a positive (points earned, marked as gold coins) or a negative (points lost, marked as a bomb) outcomes (). Participants aim was to open the boxes associated with positive outcomes only, and refrain from opening the boxes associated with negative outcomes.
Figure 1. Illustration of the different experimental conditions. This Figure is being reproduced with the permission of the copyright holder Neuropsychology. Reference of the original source Levy-Gigi et al. (Citation2015). Reduced hippocampal volume is associated with overgeneralization of negative context in individuals with PTSD. Neuropsychology 29(1), 151–161.
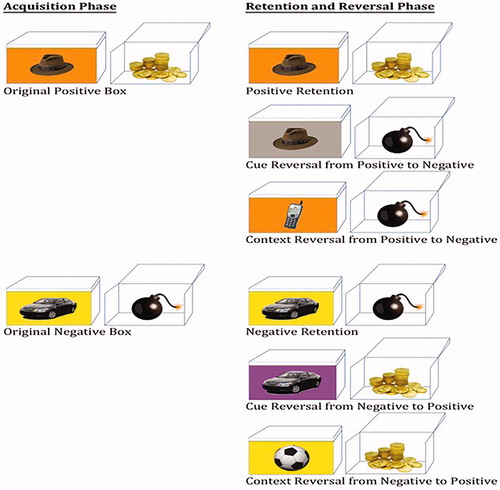
Figure 2. Examples of experimental trials in which participants chose to (a) open a positive outcome box and (b) open a negative-outcome box. This Figure is being reproduced with the permission of the copyright holder Neuropsychology. Reference of the original source Levy-Gigi et al. (Citation2015). Reduced hippocampal volume is associated with overgeneralization of negative context in individuals with PTSD. Neuropsychology 29(1), 151-161.
The paradigm had two phases (). In the first, acquisition, phase, participants learned by trial and error to predict the outcome of four different cue-context combinations (i.e. open the two “positive” boxes and skip the two “negative” boxes). In order to complete the acquisition phase and move on to the second, retention and reversal phase, participants needed to learn the four cue-context-outcome associations to a criterion of six consecutive error-free responses within a minimum of 40 trials. Correct responses refer to conditions in which participants opened positive cue-context combinations and left negative cue-context combinations untouched. Similarly, incorrect responses refer to conditions in which participants opened negative cue-context combinations (boxes) or left positive boxes untouched.
A subsequent retention and reversal phase started immediately following the acquisition phase without any transition or warning. In this phase, participants saw both retention (old) and newly formed cue-context-outcome combination. The retention trials included already-learned trials in which the original cue-context-outcome combinations were presented. The new trials included two different types of trials: old cue with new background (e.g. a hat on a gray background) or new cue and old background (e.g. a phone on an orange background) (). Crucially, the newly formed cue-context combinations were associated with the opposite outcome relative to the combinations including the original cue or context (i.e. if the original cue-background was associated with reward, then the new-cue-old-background was associated with punishment). Therefore, in order to successfully learn these new combinations, participants need to reverse the association rules of either the original cue or the original context.
Boxes in this phase were presented in 10 blocks of 12 boxes each (two boxes from each of the following conditions: positive/negative retention, positive/negative cue reversal, positive/negative context reversal). Thus, a total of 120 trials with 20 trials per condition were presented. At the end of the task participants, saw the total sum of earned points.
Self-report questionnaires and cognitive assessment
PTSD symptoms were assessed using the PTSD Check List (PCL-5, Blevins, Weathers, Davis, Witte, & Domino, Citation2015). In addition, all participants completed the following self-report questionnaires in order to control for possible confounds and possible effects of levels of cumulative trauma exposure: the revised version of the Beck Depression Inventory (BDI–II; Beck, Steer, & Brown, Citation1996) was used to assess depressive symptoms over the previous 2 weeks. The STAI (State–Trait Anxiety Inventory; Spielberger, Gorsuch, Lushene, Vagg, & Jacobs, Citation1983) was used to assess current and general anxiety.
Data analysis
All data were checked for normality of distribution using Kolmogorov–Smirnov tests. Because participants were instructed to open all new boxes when they first saw them, we did not include the first response to each new box in the acquisition and reversal phases in our analyses (note that retention trials include only old boxes, and therefore all trials are analyzed).
Results
Acquisition and retention of stimulus–outcome associations
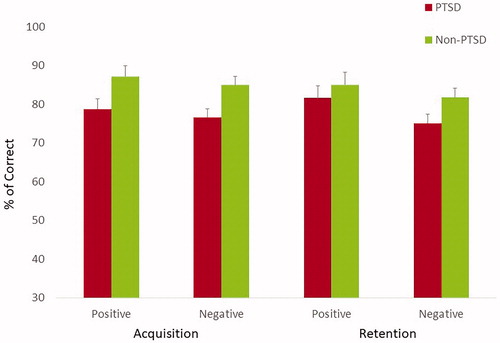
We conducted a Phase (acquisition vs. retention) by Valence (positive vs. negative outcome) by PTSD (yes vs. no) by Sailing (yes vs. no) mixed model ANOVA on the percentage of correct responses, in order to examine whether the groups were equally able to learn and retain positive and negative stimulus–outcome associations. In this model PTSD and Sailing were the between-subjects factor, whereas Phase and Valence were the within-subject factors. Age and gender were added as control variables. We found a significant main effect of PTSD (F (1,71) = 5, p < .05, η2 = .07) indicating that overall the performance of individuals with PTSD was significantly lower compared to the performance of control participants. However, as predicted, there was no significant main effect of sailing (F (1,71) = .19, p = .66) nor significant interaction of PTSD by phase (F (1,71) = 2.58, p = .11) or PTSD by valence (F (1,71) = .28, p = .60). The results are depicted in .
Cue and context reversal
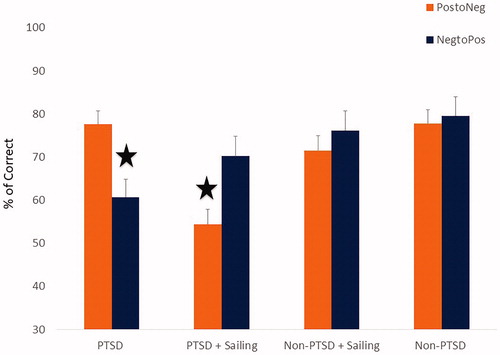
We conducted a Reversal Type (Cue vs. Context) by Reversal-Valence (Positive to Negative vs. Negative to Positive) by Sailing (Yes vs. No) by PTSD (Yes vs. No) mixed model ANOVA on the percentage of correct responses in order to examine whether the PTSD-sailing group exhibited better reversal learning from negative to positive outcome. In this model Sailing and PTSD were the between-subjects factor whereas Reversal-Type and Reversal-Valence were the within-subject factors. Age and gender were added as control variables. There was a significant main-effects of PTSD (F (1,71) = 9.42, p < .01, η2 = .12). In addition, there was a significant interaction of Reversal-Valence by Sailing (F (1,71) = 10.97, p < .01, η2 = .13), and most importantly there was a significant three-way interaction of Reversal-Valence by Sailing by PTSD (F (1,71) = 9.42, p < .01, η2 = .12). graphically depicts these findings. To understand the nature of this interaction we conducted simple effects analyses with Bonferroni’s correction for multiple comparisons. The results revealed that individuals in the PTSD-no-sailing group showed impaired ability to reverse negative to positive outcome compared to all other groups (F (3,71) = 5.05, p < .01, η2 = .18), which did not differ in their performance (All F < 1). As predicted, PTSD-sailing group exhibited better reversal learning from negative to positive outcome, as compared to the PTSD-no-sailing group. However, individuals in the PTSD-sailing group showed impaired ability to reverse positive to negative outcome compared to all other groups (F (3,71) = 4.74, p < .01, η2 = .17), which did not differ in their performance (All F < 1).
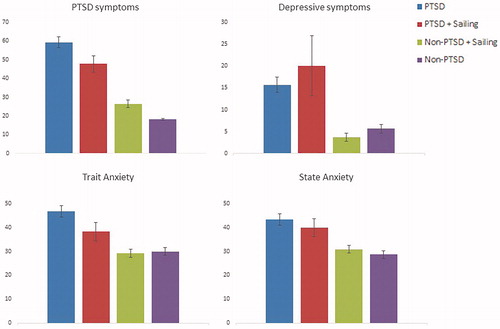
Symptoms severity measures
We conducted a multivariate analysis of covariance (MANCOVA) with PTSD (yes, no) and sailing (yes, no) in order to examine differences in PTSD, depressive and anxiety symptoms. Age and gender were added as control variables. Significant main effect was demonstrated for group (Wilks’s lambda = 0.29, F (12,180) = 9.23, p < .001, η2 = .34). No other main effects or interactions were found (all ps > 0.27) The results are depicted in . There were significant differences between the groups (F (3,71) = 45.7, p < .001, η2 = .36; F (3,71) = 10.59, p < .001, η2 = .31; F (3,71) = 8.38, p < .001, η2 = .26; F (3,71) = 10.95, p < .001, η2 = .32 for PTSD, depressive, state and trait anxiety symptoms respectively). Sidak post-hoc tests revealed the following significant relationships between the groups: PTSD symptoms: PTSD-no-sailing > PTSD-Sailing > Control-Sailing = Control-No-Sailing; Depressive symptoms: PTSD = PTSD-Sailing > Control-Sailing = Control-No-Sailing; State anxiety: PTSD = PTSD-Sailing > Control-Sailing = Control-No-Sailing; Trait anxiety: PTSD > PTSD-Sailing > Control-Sailing = Control-No-Sailing. Results suggest that our hypothesis was partially supported- the PTSD-sailing group exhibited less PTSD and trait anxiety symptoms but not less depressive symptoms nor state anxiety as compared to the PTSD no-sailing group.
Discussion
The aim of the present study was to compare cognitive flexibility and clinical symptoms among four groups of participants who differed as a function of PTSD diagnosis (yes/no) and participation in sailing nature adventure intervention (yes/no). The results revealed decreased level of clinical symptoms in PTSD individuals who participated in the sailing intervention compared to patients in the no-sailing group. Specifically, similar to previous findings (Gelkopf et al., Citation2013), they displayed lower levels of PTSD symptoms. In addition, PTSD individuals who participated in the sailing intervention showed lower levels of trait, but not state, anxiety symptoms. These results may suggest that while both groups may experience an intense degree of state anxiety to specific situations, among those who participated in sailing intervention this experience is narrowed to limited conditions and hence describes a temporary feeling rather than a personality characteristic (Julian, Citation2011).
Importantly for the focus of the present study, as expected and in line with previous findings, all groups were equally able to acquire and retain positive and negative stimulus-outcome associations. However, there were significant differences in cognitive flexibility as a function of PTSD diagnosis (Levy-Gigi, Richter-Levin, & Kéri, Citation2014; Levy-Gigi et al., Citation2015; Levy-Gigi & Richter-Levin, Citation2014). Specifically, while non-PTSD individuals were able to flexibly modify their reaction in accordance with situational demands individuals with PTSD showed impaired cognitive flexibility. However, distinct patterns of such impairment were noted in the different groups. Specifically, PTSD individuals who did not participate in the sailing intervention showed impaired ability to learn that a previously negative stimulus becomes positive when presented later in a new combination. These results replicate our previous findings in PTSD individuals, suggesting that PTSD symptomatology relates to impaired ability to learn that a stimulus that was once negative might become positive in a different context (Levy-Gigi et al., Citation2012, Citation2016; Levy-Gigi & Richter-Levin, Citation2014). Therefore, it may explain why individuals with PTSD more likely to react in a similar way when hearing a loud noise either in a battle field (e.g. missile attack) or in a safe environment (e.g. fireworks). Surprisingly, PTSD individuals who took part in the sailing intervention displayed an opposite impairment. While they were able to learn that a negative stimulus becomes positive, they struggled to learn that positive stimulus becomes negative.
Taken together, the results indicate that while individuals after sailing intervention displayed lower PTSD and trait- anxiety symptoms they still suffered cognitive flexibility impairment. Therefore, while sailing intervention might be associated with enhanced self-regulation and improved capacity to face fears (Gelkopf et al., Citation2013), it is also associated with a rigid behavior. Specifically, it is possible that the need to deal with stressful unknown situations may lead individuals to follow a clear set of rules, which does not allow any exception, and therefore, may not encourage nor improve flexibility.
These results question previous studies which showed that poor cognitive flexibility is associated with a more severe PTSD and depressive symptoms (Keith et al., Citation2015; Palm & Follette, Citation2011), whereas adequate cognitive flexibility predicts reduction in PTSD symptoms following a yoga intervention (Avery, Blasey, Rosen, & Bayley, Citation2018). A possible explanation for such a discrepancy may relate to the fact that despite the lower PTSD symptoms in the PTSD-sailing group, those participants did not reach full remission and still exhibited higher levels of symptoms compared to healthy controls.
While the present study serves as an important first step toward understanding the relationship between cognitive flexibility, sailing intervention and clinical symptoms, several limitations need to be noted. First, similar to other ex post facto studies in which the participants were not randomly assigned to the different groups, the interpretation of the results is limited. Specifically, our experimental design does not allow reaching conclusions regarding causality and all the observed effects reflect between-groups differences rather than individual progress. However, the participants in the different PTSD groups were matched for education and time since onset, whereas possible effects of age and gender were controlled in all analyses (see also Anantharaman & Swee Han, Citation2001; Besser, Neria, & Haynes, Citation2009; Engelhard, van den Hout, Weerts, Hox, & van Doornen, Citation2009 for similar experimental design). Importantly, the current results serve as a proof of concept which paves the way for a future longitudinal study with randomized controlled design and symptoms assessment at multiple time points.
Another limitation relates to the cognitive flexibility assessment. Specifically, the current study used a well validated performance based paradigm to assess cognitive flexibility (Levy-Gigi et al., Citation2016, Citation2015; Levy-Gigi & Kéri, Citation2015; Levy-Gigi & Richter-Levin, Citation2014). In opposed to self-report questionnaires which may suffer from different biases and provide a biased view of the individuals’ abilities (Holtgraves, Citation2004; Van De Mortel, Citation2008), performance-based paradigms may reflect the individual condition more accurately. However, this paradigm focuses on a single aspect of cognitive flexibility – the ability of individuals to update their reaction in accordance with changes in the situation. Other aspects of flexibility may have generated a different result pattern. Future studies may aim to test multiple aspects of cognitive, as well as emotional, flexibility in order to provide a wider picture of this phenomenon.
Finally, while the current study suggests no associations between lower symptoms-severity and cognitive flexibility, future neuroimaging studies may further test this relationship as well as its correlations with hippocampal structure and function, treatment related symptoms reduction and cognitive flexibility. Specifically, it is possible that in opposed to CBT, sailing intervention does not result in hippocampal volume modification (Levy-Gigi et al., Citation2013). Alternatively, it might be found that post- treatment hippocampal volume growth is not associated with improved cognitive flexibility.
To summarize, the present study serves as a crucial first step towards understanding the relationship between cognitive flexibility, sailing intervention and clinical symptoms. The results add to previous findings, which highlight the central role of cognitive flexibility. It shows that while individuals who took part in sailing intervention display lower level of PTSD and trait anxiety symptoms, they still exhibit impaired cognitive flexibility, though it shifted from one domain to another. Therefore, it suggests that not only cognitive flexibility deficit may appear in various forms, it may also exist after intensive therapeutic intervention. In conclusion, while individuals with PTSD who took part in therapeutic interventions may show reduced level of clinical symptoms, they may still suffer difficulties to adaptively behave in new circumstances. Hence, there is a need to develop focused interventions to improve cognitive flexibility as a key factor towards a more comprehensive rehabilitation process.
Notes on contributors
E.L.G. developed the study concept. All authors contributed to the study design. Testing and data collection were performed by E.L.G. and O.D.. E.L.G. and R.Z. performed the data analysis and interpretation and drafted the paper. G.R.L. and E.G.S. provided critical revisions. All authors approved the final version of the paper for submission.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
Data availability statement
The data that support the findings of this study are available from the corresponding author upon request.
Additional information
Funding
References
- Anantharaman, V., & Swee Han, L. (2001). Hospital and emergency ambulance link: using IT to enhance emergency pre-hospital care. International Journal of Medical Informatics, 61, 147–161. doi:10.1016/S1386-5056(01)00137-X
- Anacker, C., & Hen, R. (2017). Adult hippocampal neurogenesis and cognitive flexibility – linking memory and mood. Nature Reviews Neuroscience, 18, 335–346. doi:10.1038/nrn.2017.45
- Avery, T., Blasey, C., Rosen, C., & Bayley, P. (2018). Psychological Flexibility and Set-Shifting Among Veterans Participating in a Yoga Program: A Pilot Study. Military Medicine, 183, e359–e363. doi:10.1093/milmed/usy045
- Baddeley, A. (2012). Working memory: theories, models, and controversies. Annual Review of Psychology, 63, 1–29. doi:10.1146/annurev-psych-120710-100422
- Beck, A.T., Steer, R.A., & Brown, G.K. (1996). Manual for the Beck depression inventory-II. San Antonio, TX: Psychological Corporation.
- Besser, A., Neria, Y., & Haynes, M. (2009). Adult attachment, perceived stress, and PTSD among civilians exposed to ongoing terrorist attacks in Southern Israel. Personality and Individual Differences, 47, 851–857. doi:10.1016/j.paid.2009.07.003
- Blevins, C.A., Weathers, F.W., Davis, M.T., Witte, T.K., & Domino, J.L. (2015). The posttraumatic stress disorder checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. Journal of Traumatic Stress, 5, 489–498. doi:10.1002/jts.22059
- Burghardt, N.S., Park, E.H., Hen, R., & Fenton, A.A. (2012). Adult-Born hippocampal neurons promote cognitive flexibility in mice. Hippocampus, 22, 1795–1808. doi:10.1002/hipo.22013
- Caddick, N., & Smith, B. (2014). The impact of sport and physical activity on the well-being of combat veterans: A systematic review. Psychology of Sport and Exercise, 15, 9–18. doi:10.1016/j.psychsport.2013.09.011
- Dickie, E.W., Brunet, A., Akerib, V., & Armony, J.L. (2011). Neural correlates of recovery from post-traumatic stress disorder : A longitudinal fMRI investigation of memory encoding. Neuropsychologia Neuropsychologia, 49, 1771–1778. doi:10.1016/j.neuropsychologia.2011.02.055
- Dietrich, Z.C., Joye, S.W., & Garcia, J.A. (2015). Natural medicine: Wilderness experience outcomes for combat veterans. Journal of Experiential Education, 38, 394–406. doi:10.1177/1053825915596431
- Engelhard, I.M., van den Hout, M.A., Weerts, J., Hox, J.J., & van Doornen, L.J. (2009). A prospective study of the relation between posttraumatic stress and physical health symptoms. International Journal of Clinical and Health Psychology, 9, 365–372.
- Fu, F., & Chow, A. (2017). Traumatic exposure and psychological well-being: The moderating role of cognitive flexibility. Journal of Loss and Trauma, 22, 24–35. doi:10.1080/15325024.2016.1161428
- Gelkopf, M., Hasson-Ohayon, I., Bikman, M., & Kravetz, S. (2013). Nature adventure rehabilitation for combat-related posttraumatic chronic stress disorder: A randomized control trial. Psychiatry Research, 209, 485–493. doi:10.1016/j.psychres.2013.01.026
- Haim-Nachum, S., & Levy-Gigi, E. (2019). A chink in the armor: The influence of training on generalization learning impairments after viewing traumatic stimuli. Frontiers in Psychology.
- Hijazi, A.M., Keith, J.A., & O'Brien, C. (2015). Predictors of posttraumatic growth in a multiwar sample of U.S. Combat veterans. Peace and Conflict: Journal of Peace Psychology, 21, 395–408. doi:10.1037/pac0000077
- Holtgraves, T. (2004). Social desirability and self-reports: Testing models of socially desirable responding. Personality and Social Psychology Bulletin, 30, 161–172. doi:10.1177/0146167203259930
- Ionescu, T. (2012). Exploring the nature of cognitive flexibility. New Ideas in Psychology, 30, 190–200. doi:10.1016/j.newideapsych.2011.11.001
- Joseph, J.S., & Gray, M.J. (2011). The utility of measuring explanatory flexibility in PTSD research. Cognitive Therapy and Research, 35, 372–380. doi:10.1007/s10608-010-9301-7
- Julian, L.J. (2011). Measures of anxiety: State-Trait Anxiety Inventory (STAI), Beck Anxiety Inventory (BAI), and Hospital Anxiety and Depression Scale-Anxiety (HADS-A). Arthritis Care and Research, 63, S467–S472. doi:10.1002/acr.20561
- Keith, J., Velezmoro, R., & O’Brien, C. (2015). Correlates of cognitive flexibility in veterans seeking treatment for posttraumatic stress disorder. The Journal of Nervous and Mental Disease, 203, 287–293. doi:10.1097/NMD.0000000000000280
- Levy-Gigi, E., & Kéri, S. (2015). The interactive effect of negative reversal learning and age on depression: Possible cognitive mechanisms underlying the elevated depressive symptoms in older adults. Psychology and Aging, 30, 341–347. doi:10.1037/a0039181
- Levy-Gigi, E., Kéri, S., Myers, C.E., Lencovsky, Z., Sharvit-Benbaji, H., Orr, S.P., … Gluck, M.A. (2012). Individuals with posttraumatic stress disorder show a selective deficit in generalization of associative learning. Neuropsychology, 26, 758–767. doi:10.1037/a0029361
- Levy-Gigi, E., & Richter-Levin, G. (2014). The hidden price of repeated traumatic exposure. Stress, 17, 343–351. doi:10.3109/10253890.2014.923397
- Levy-Gigi, E., Richter-Levin, G., & Kéri, S. (2014). The hidden price of repeated traumatic exposure: different cognitive deficits in different first-responders. Frontiers in Behavioral Neuroscience, 8, 343–351. doi:10.3389/fnbeh.2014.00281
- Levy-Gigi, E., Richter-Levin, G., Okon-Singer, H., Kéri, S., & Bonanno, G.A. (2016). The hidden price and possible benefit of repeated traumatic exposure. Stress, 19, 1–7. doi:10.3109/10253890.2015.1113523
- Levy-Gigi, E., Szabó, C., Kelemen, O., & Kéri, S. (2013). Association among clinical response, hippocampal volume, and FKBP5 gene expression in individuals with posttraumatic stress disorder receiving cognitive behavioral therapy. Biological Psychiatry, 74, 793–800. doi:10.1016/j.biopsych.2013.05.017
- Levy-Gigi, E., Szabo, C., Richter-Levin, G., & Kéri, S. (2015). Reduced hippocampal volume is associated with overgeneralization of negative context in individuals with PTSD. Neuropsychology, 29, 151–161. doi:10.1037/neu0000131
- Metzl, E.S. (2009). The role of creative thinking in resilience after hurricane Katrina. Creativity and the Arts, 3, 112–123. doi:10.1037/a0013479
- Palm, K.M., & Follette, V.M. (2011). The roles of cognitive flexibility and experiential avoidance in explaining psychological distress in survivors of interpersonal victimization. Journal of Psychopathology and Behavioral Assessment, 33, 79–86. doi:10.1007/s10862-010-9201-x
- Radell, M.L., Beck, K.D., Gilbertson, M.W., & Myers, C.E. (2017). Post-traumatic stress disorder symptom burden and gender each affect generalization in a reward- and punishment-learning task. PLoS One, 12, e0172144–21. doi:10.1371/journal.pone.0172144
- Rosenbaum, S., Vancampfort, D., Steel, Z., Newby, J., Ward, P.B., & Stubbs, B. (2015). Physical activity in the treatment of Post-traumatic stress disorder: A systematic review and meta-analysis. Psychiatry Research, 230, 130–136. doi:10.1016/j.psychres.2015.10.017
- Russell, K.C. (2001). What is wilderness therapy? Journal of Experiential Education, 24, 70–79.
- Spielberger, C.D., Gorsuch, R.L., Lushene, R., Vagg, P.R., & Jacobs, G.A. (1983). Manual for the State–Trait Anxiety Inventory, STAI (Form Y): Self-evaluation questionnaire. Palo Alto, CA: Consulting Psychologists Press.
- Van De Mortel, T.F. (2008). Faking it: social desirability response bias in self- report research Faking it: Social desirability response bias in self‑ report research. Australian Journal of Advanced Nursing, 25, 40–48. https://doi.org/http://www.ajan.com.au/ajan_25.4.htm
- Zhu, X., Suarez-Jimenez, B., Lazarov, A., Helpman, L., Papini, S., Lowell, A., … Neria, Y. (2018). Functional connectivity in patients with posttraumatic stress disorder Exposure-based therapy changes amygdala and hippocampus resting-state functional connectivity in patients with posttraumatic stress disorder. Depression and Anxiety, 35, 974. (September). doi:10.1002/da.22816