Abstract
Healthy child development is under the influence of prenatal and perinatal exposure to stress stimuli. The aim of this study is to test the hypotheses that (1) neonates requiring catecholamine blood pressure support are more often born to mothers with stress-related cardiometabolic diseases, (2) maternal stress-related diseases are associated with more frequent requirement of maternal corticosteroid treatment and (3) antenatal steroid exposure of neonates reduces the need of postnatal catecholamine support. A retrospective cohort study was performed on a sample of 427 mature (13%), preterm (64%) and extremely preterm (23%) neonates of both sexes. Mothers at risk of preterm delivery were treated with dexamethasone. The blood pressure support in neonates was performed by intravenous treatment via umbilical or epicutaneous venous catheter with dopamine (5 ug/kg/min) or dobutamine (5 ug/kg/min) or a combination of both. The results showed a lack of association between maternal stress-related diseases and the complicated outcome of their neonates. Maternal treatment with corticosteroid dexamethasone was associated with lower frequency of catecholamine blood pressure support requirement. Catecholamine support was more needed in male infants. Thus, the occurrence of maternal cardiometabolic stress-related diseases does not appear to be related to the need of catecholamine support in the neonate. In agreement with the second hypothesis, a more frequent maternal corticosteroid treatment was associated with the presence of maternal stress-related diseases. Most importantly, the obtained results support the hypothesis on positive influence of maternal glucocorticoid administration on cardiovascular outcome of the neonate, representing an additional beneficial effect of antenatal corticosteroids.
Maternal hypertension, diabetes and obesity, which belong to cardiometabolic stress-related diseases, failed to show a negative influence on neonatal health as was determined by the need of catecholamine blood pressure support in a large sample of 427 immature and mature newborns. Since glucocorticoids are often viewed as negative agents that should be avoided, the important finding of the present study is the beneficial effect of maternal corticosteroid treatment on blood pressure stability of the neonate.
LAY SUMMARY
Introduction
Healthy child development is, among others, under strong influence of prenatal and perinatal exposure to stress stimuli (Kingston et al., Citation2015). Even the child coming to this world is a great stressful event for both the mother and her neonate, in particular in the case of preterm or premature birth. Sympathetic and cardiovascular activation accompanied by catecholamine release from the adrenal medulla belongs to the main components of the stress response. Rapid effects of catecholamines are inevitable for coping with acute “fight or flight” stress situations. In the long-term view, however, catecholamines released under stress conditions are thought to have negative influence on human health and represent risk factors for the development of stress-related adverse factors and diseases (Goldstein & Kopin, Citation2008; Jezova & Herman, Citation2016).
On the other hand, treatment with catecholamines or other drugs with positive inotropic effect is often unequivocal to overcome cardiovascular and general emergency states in neonates with special-care needs (Joynt & Cheung, Citation2018). According to a Canadian database, 10% of neonates of <29 weeks had been treated with inotropes on days 1–3 (Wong et al., Citation2015). The treated neonates were more likely to have a smaller birth weight. The use of inotropes was associated with an increased mortality, after adjusting for gender, gestation, and 5-min Apgar score (Joynt & Cheung, Citation2018).
The second main part of the stress response represents the hypothalamic–pituitary–adrenocortical axis activation with glucocorticoids as the executive component. The glucocorticoids, namely cortisol (hydrocortisone) in humans, are needed for obtaining the necessary energy needed for coping with acute stressors. Glucocorticoids can also induce negative consequences when frequent and intensive stress situations are not under control for prolonged time periods (Jezova et al., Citation1996, Citation2019). Similarly, as in the case of catecholamines, glucocorticoids are being used as medicaments in the intensive care of premature neonates. Even more frequently, the premature neonates are exposed to hydrocortisone or synthetic steroids antenatally. In line with widespread clinical practice, women at risk of preterm delivery before 34 weeks' gestational age should be treated with corticosteroids in order to facilitate fetal lung maturation. It has been suggested that antenatal glucocorticoids may have several positive effects on neonate well-being (Wapner & Jobe, Citation2011).
So far, nobody has approached the above mentioned issues from the view of catecholamines and glucocorticoids as stress hormones. These hormones contribute to the development of stress-related disorders (Jezova & Herman, Citation2016) including cardiometabolic diseases. Hypertension, diabetes and obesity were considered to belong to stress-related diseases a long time ago (Liu et al., Citation2017; Marangou et al., Citation1988; Sterling et al., Citation1988; Szczepanska-Sadowska et al., Citation2010).
This study focused on neonatal health as determined by the need for blood pressure support. It is well known that prenatal exposure to stressors/stress hormones leads to pathological consequences later in life (Burgueño et al., Citation2020). Therefore, we put attention to maternal comorbidities belonging to stress-related cardiometabolic diseases and maternal glucocorticoid treatment. The aim of the present study on a relatively large premature and mature neonate sample is to test the hypotheses that (1) mothers of neonates requiring catecholamine blood pressure support shortly after the birth are more often suffering with stress-related diseases than mothers of neonates without such requirement, (2) maternal stress-related diseases are associated with more frequent requirement of corticosteroid treatment due to the risk of preterm delivery and (3) exposure of neonates to antenatal steroids reduces the need of postnatal catecholamine blood pressure support.
Subjects and Methods
Sample
We conducted a single-center retrospective cohort study on a sample of 427 viable infants without lethal anomaly, who were born between 24 and 41 weeks of gestation at a highly specialized intensive care unit for preterm newborns of the Department of Neonatology of the University Hospital Bratislava. We included all infants, who required catecholamine blood pressure support born in the years 2016–2019. The control group consisted of infants not requiring blood pressure support who were matched according to the gestational age. The study period was selected empirically. The study protocol was approved by the Ethics Committee of the University Hospital Bratislava, Slovakia. The study was performed in accordance with the Declaration of Helsinki. All data were de-identified.
Hypertension was defined as systolic blood pressure ≥140 mmHg and/or diastolic blood pressure ≥90 mmHg and the diagnosis of hypertension in pregnancy was performed according to Brown et al. (Citation2018). All cases of hyperglycemia observed during pregnancy comprising gestational diabetes mellitus and pre-gestational diabetes were considered under diagnosis of diabetes (Mirghani Dirar & Doupis, Citation2017). Obesity was defined as body mass index >30 kg/m2 (Purnell, Citation2000–2018).
Measures evaluated
Antepartum (maternal diabetes, obesity, maternal hypertension, maternal corticosteroid treatment), and postpartum (birth weight, gestational age, sex, 1-, 5- and 10-min Apgar scores) variables were extracted from the hospital database. The requirement of catecholamine blood pressure support was considered the main parameter studied. The blood pressure support was performed by intravenous treatment via umbilical or epicutaneous venous catheter with dopamine (5ug/kg/min) or dobutamine (5ug/kg/min) or a combination of both. Mothers at risk of preterm delivery before week 34 of gestational age were treated with corticosteroids in the form of synthetic glucorticoid dexamethasone in a dose of 6 mg repeated 1 − 9 times.
Statistical analysis
Student’s t-test for independent groups was used to compare continuous variables (gestational age, birth weight, Apgar scores) and Pearson's chi-square test was used to compare categorical variables between the groups of neonates with vs. without catecholamine blood pressure support. The odds ratio (OR) and 95% confidence interval (CI) were calculated using the Baptista-Pike method. The significance level was set at p ≤ 0.05 (2-tailed). All significant variables were included into a logistic regression analysis to examine the association of categorical or continuous variables with dependent variable (catecholamine support). Continuous variables are expressed as mean ± SEM.
Results
A total of 427 neonates were evaluated. From those, 210 infants required catecholamine blood pressure support and they were compared to 217 infants which did not require such treatment. The majority of the infants were males (). The gestational age of neonates was 24 − 41 weeks (31.6 ± 3.8) and the birth weight was 490 − 5130 g (1829 ± 874). The majority of the neonates were born in the gestational weeks 29 − 36 (). Student’s t-test did not reveal significant differences in the gestational age () and the birth weight () between the neonates with and without catecholamine blood pressure support.
Figure 1. Differences between the group of neonates requiring catecholamine support (CA+) and those that did not require such support (CA-) in (A) gestational age; (B) birth weight; (C) 1-minute Apgar score; (D) 5 minute Apgar score; (E) 10 minute Apgar score.
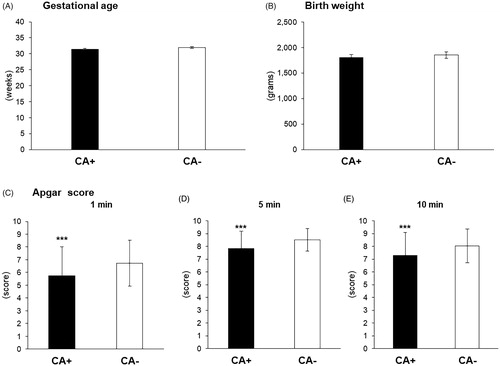
Table 1. Sample characteristics.
From the whole sample of infants (), 29.3% were born to mothers suffering with stress-related cardiometabolic diseases. Out of these neonates, 47.2% required catecholamine blood pressure support. The results showed that 75% of the whole sample were neonates born to mothers treated with corticosteroids.
Unpaired t-test and Pearson's chi-square revealed three variables (Apgar score, sex and maternal corticosteroids) that were significantly associated with the requirement of catecholamine blood pressure support in the whole sample of neonates. As expected, the mean Apgar score in the 1st (t425 = −4.99, p < 0.001, ), the 5th (t425 = −4.96, p < 0.001, ) and the 10th (t425 = −5.48, p < 0.001, ) minute was significantly lower in neonates requiring catecholamine support compared to those without such requirement. Pearson's chi-square test showed a significant relationship (OR: 1.51; CI: 1.02–2.24, p < 0.05) between the sex and the requirement of catecholamine blood pressure support (). Statistical analysis also revealed a significant association (OR: 1.76; CI: 1.33–2.72, p < 0.05) between the exposure to antenatal corticosteroids and the requirement of catecholamine support ().
Table 2. Association between catecholamine support and selected sample characteristics.
Statistical analysis by Pearson's chi-square test did not show any significant association between the requirement of catecholamine support in neonates and the presence of maternal stress-related cardiometabolic diseases when considered all diseases altogether, namely hypertension, diabetes and obesity. If the chi-square test was performed on data only from mothers suffering from hypertension before and during pregnancy versus healthy mothers, there was a significant relationship between the requirement of catecholamine support in neonates and the presence of maternal hypertension (OR: 0.36; CI: 0.15–0.92, p < 0.05). The majority of mothers suffering from hypertension were treated with methyldopa (80%). The rest of the mothers were without antihypertensive drug treatment (16%) or were treated with amlodipine (4%). No significant associations were found between the requirement of catecholamine support and the presence of maternal preeclampsia or diabetes.
Significant variables were incorporated into a multiple logit regression model. We found that only the presence of maternal corticosteroid treatment was associated with the requirement of catecholamine blood support by the infant, explaining 29% of the variance.
Pearson chi-square test also indicated a significant relationship between the maternal stress-related diseases and maternal corticosteroid treatment (OR: 0.52; CI: 0.31–0.89, p < 0.05).
Discussion
The present study on a large sample of immature and mature neonates and their mothers clearly demonstrates a lack of association between maternal stress-related cardiometabolic diseases and the complicated outcome of their neonates, namely the need of catecholamine blood pressure support. Maternal treatment with corticosteroid dexamethasone was associated with lower frequency of blood pressure support requirement in their neonates. A weak association was observed between the need of catecholamine support and sex, with higher frequency in males. Of interest is the positive relationship between the presence of maternal stress-related diseases and maternal corticosteroid treatment.
The first hypothesis of the present study that mothers of neonates requiring catecholamine blood pressure support shortly after the birth are more often suffering with stress-related diseases than mothers of neonates without such requirement was not confirmed. About one third of 427 mothers included in this study suffered with cardiometabolic diseases, namely hypertension, obesity and diabetes. It is well known that children exposed prenatally to maternal hypertension or preeclampsia are at greater risk of developing elevated blood pressure in childhood, and cardiovascular disease in adulthood (Kajantie et al., Citation2009; Reveret et al., Citation2015; Tenhola et al., Citation2006). Previous reports were mainly focused on the association of early life hypotension and preeclampsia with both confirmative (e.g., Teng et al., Citation2006) and negative (e.g., Cordero et al., Citation2003) results. In the present study, we failed to observe any association between maternal preeclampsia (59 cases) and the need of catecholamine support in their neonates. However, the univariate analysis revealed a significant relationship of hypertension before and during pregnancy and neonatal catecholamine blood pressure support in spite of low number of cases (25 cases). Neonates of mothers suffering with hypertension required the catecholamine support less frequently, which represents a novel observation. One possible explanation of this phenomenon are adaptive changes developed during prenatal exposure to maternal hypertension. We cannot judge whether the specific type of antenatal antihypertensive treatment plays a role because the vast majority of mothers were treated with methyldopa.
An important finding of this study is a clear evidence on the beneficial effect of maternal dexamethasone treatment on the need of early postnatal blood pressure support revealed by a multiple logit regression model. Exposure to antenatal corticosteroids has been considered among the factors contributing to higher mean blood pressure and less hypotension soon after birth but the evidence is still not convincing (Dempsey, Citation2017). Antenatal exposure to maternal glucocorticoid administration in extremely preterm or very low birth weight infants was related to less blood pressure support (Moise et al., Citation1995; Wong et al., Citation2015) or higher mean blood pressures (Demarini et al., Citation1999), but these findings were not confirmed by another group of authors (LeFlore et al., Citation2000). An interesting study on early neonatal hypotension in premature infants born to preeclamptic mothers (Teng et al., Citation2006) failed to demonstrate that arterial blood pressure in newborns was influenced by antenatal glucocorticoid exposure. We suggest that the association between antenatal glucocorticoid exposure and the requirement of blood pressure support in the present study was observed thanks to a broad spectrum of gestational age starting from week 24 and ending with week 42.
The finding of higher proportion of male infants requiring catecholamine blood pressure support than those without such need is consistent with the general view (O'Driscoll et al., Citation2018). The male sex was associated with neurological, pulmonary, cardiovascular an infectious morbidities as well as overall mortality when compared to female infants of similar preterm gestation (Kent et al., Citation2012). One possible mechanism involved in these differences is the action of maternal glucocorticoids, which are important in fetal growth and organ maturation. The actions of maternal glucocorticoid are manifested especially under adverse environmental situations during gestation accompanied by increased stress hormone release. It was shown that the placentae in female fetuses inactivate maternal glucocorticoids more efficiently compared to males (Alur, Citation2019). It is due to the activity of the enzyme 11-beta-hydroxysteroid dehydrogenase type 2 known to metabolize cortisol to its inactive derivative (Tseilikman et al., Citation2020). Resulting higher prenatal exposure to cortisol in males, particularly during maternal adverse stress situations, may explain why male fetuses are more prone to maternal stress-related complications (Alur, Citation2019). However, no significant relationship between sex and maternal glucocorticoid treatment was observed in the present study.
Interestingly, the presence of maternal stress-related diseases was found to be associated with more frequent corticosteroid treatment. It might mean that mothers with stress-related diseases were at higher risk of preterm delivery compared to mothers without hypertension or diabetes. Further studies are needed to elaborate and broaden this interesting observation.
In conclusion, the present study brings new knowledge on the stress hormones and their importance in the perinatal care (). We have approached the importance of glucocorticoids as maternal treatment and catecholamines as blood pressure support in neonates. We failed to find support for the hypothesis on higher requirement of catecholamine blood pressure support in mothers with stress-related disease. The occurrence of maternal somatic stress-related diseases does not appear to be related to the need of catecholamine support in the neonate. Interestingly, neonates of mothers suffering with hypertension required the catecholamine support less frequently. In agreement with the second hypothesis, a more frequent maternal corticosteroid treatment was associated with the presence of maternal stress-related diseases. Most importantly, the obtained results support the hypothesis on positive influence of maternal glucocorticoid administration on cardiovascular outcome of the neonate, representing an additional beneficial effect of antenatal corticosteroids.
Disclosure statement
The authors report no conflict of interest.
Additional information
Funding
Notes on contributors
Alexandra Garafova
Alexandra Garafova, MD, PhD is a physician of the Department of Neonatology, University Hospital, Bratislava. She is acting as a special assistent of the Institute of Pediatrics, Slovak Medical University, Bratislava. She has finished her PhD in normal and pathological physiology at the Faculty of Medicine of Comenius University. Her research is focused on stress and neuroendocrine relations mainly in clinical studies in humans.
Eva Kornanova
Eva Kornanova, MD is a trainee of the 1st Department of Obstetrics and Gynaecology, Faculty of Medicine, Comenius University in Bratislava. She is also a PhD student in gyneacology and obstetrics at the Faculty of Medicine of the Comenius University, Bratislava, Slovakia.
Darina Chovancova
Assoc. Prof. Darina Chovancova, MD, PhD is a superintendent of the Department of Neonatology, University Hospital, Bratislava and she is a specialist responsible for education in neonatology at the Slovak Medical University, Bratislava. She is the President of the Neonatology Panel of the Slovak Pediatric Association. Up to now, her research has been focused on diagnostics and treatment in neonatology.
Miroslav Borovsky
Prof. Miroslav Borovsky, MD, PhD is a superintendent of the 1st Department of Obstetrics and Gynaecology, Faculty of Medicine, Comenius University in Bratislava. He is the main expert of the Ministry of Health of the Slovak Republic for gynecology and obstetrics. In addition to these positions, he also holds many other presidential positions in the Section of Gynecological Endocrinology, Slovak Society for Endocrinology, Menopause and Andropause. His main subspecialization is gynecological endocrinology.
Peter Karailiev
Peter Karailiev, Dr rer. nat., is a PhD student at the Laboratory of Pharmacological Neuroendocrinology which is part of the Department of Endocrine Regulations and Psychopharmacology of the IEE BMC SAS under the supervision of Prof. Jezova. He has a master degree in molecular biology at the Faculty of Natural Sciences of Comenius University. His research is focused on molecular mechanisms and atypical markers of the stress response.
Natasa Hlavacova
Natasa Hlavacova, PhD. is a Head of the Department of Endocrine Regulations and Psychopharmacology at the Institute of Experimental Endocrinology of the Biomedical Research Center, SAS, Slovakia. She is a member of the Scientific Committee of the Biomedical Research Center, SAS. She is serving as an Editor of the General Physiology and Biophysics. She is expert in the field of Behavioral Neuroscience.
Daniela Jezova
Prof. Daniela Jezova, PharmD is a full professor of Pharmacology at the Faculty of Medicine of Comenius University and the Head of the Laboratory of Pharmacological Neuroendocrinology being a part of the Department of Endocrine Regulations and Psychopharmacology of the IEE BMC SAS, Slovakia. She has been a vice-president of the Slovak Academy of Sciences and vice-president of All European Academies. She is serving as an international expert in European research networks including the panel of European Research Council (ERC) on Endocrinology, Pathophysiology and Physiology. Her research team focused on stress research and psychopharmacology in both humans and animals belongs to the evaluated top research teams in Slovakia.
References
- Alur, P. (2019). Sex differences in nutrition, growth, and metabolism in preterm infants. Frontiers in Pediatrics, 7, 22–22. https://doi.org/10.3389/fped.2019.00022
- Brown, M. A., Magee, L. A., Kenny, L. C., Karumanchi, S. A., McCarthy, F. P., Saito, S., Hall, D. R., Warren, C. E., Adoyi, G., & Ishaku, S, International Society for the Study of Hypertension in P (2018). Hypertensive disorders of pregnancy: ISSHP Classification, Diagnosis, and Management Recommendations for International Practice. Hypertension (Dallas, Texas: 1979)), 72(1), 24–43. https://doi.org/10.1161/HYPERTENSIONAHA.117.10803
- Burgueño, A. L., Juárez, Y. R., Genaro, A. M., & Tellechea, M. L. (2020). Prenatal stress and later metabolic consequences: systematic review and meta-analysis in rodents. Psychoneuroendocrinology, 113, 104560. https://doi.org/10.1016/j.psyneuen.2019.104560
- Cordero, L., Giannone, P. J., & Rich, J. T. (2003). Mean arterial pressure in very low birth weight (801 to 1500 g) concordant and discordant twins during the first day of life. Journal of Perinatology, 23(7), 545–551. https://doi.org/10.1038/sj.jp.7210982
- Demarini, S., Dollberg, S., Hoath, S. B., Ho, M., & Donovan, E. F. (1999). Effects of antenatal corticosteroids on blood pressure in very low birth weight infants during the first 24 hours of life. Journal of Perinatology, 19(6), 419–425. https://doi.org/10.1038/sj.jp.7200245
- Dempsey, E. M. (2017). What should we do about low blood pressure in preterm infants. Neonatology, 111(4), 402–407. https://doi.org/10.1159/000460603
- Goldstein, D. S., & Kopin, I. J. (2008). Adrenomedullary, adrenocortical, and sympathoneural responses to stressors: a meta-analysis. Endocrine Regulations, 42(4), 111–119.
- Jezova, D., Balagova, L., Chmelova, M., & Hlavacova, N. (2019). Classical steroids in a new fashion: Focus on testosterone and aldosterone. Current Protein and Peptide Science, 20(11), 1112–1118. https://doi.org/10.2174/1389203720666190704151254
- Jezova, D., & Herman, J. P. (2016). Lessons from regular gathering of experts in stress research: focus on pathophysiological consequences of stress exposure. Stress (Amsterdam, Netherlands)), 19(4), 339–340. https://doi.org/10.1080/10253890.2016.1213515
- Jezova, D., Jurankova, E., Mosnarova, A., Kriska, M., & Skultetyova, I. (1996). Neuroendocrine response during stress with relation to gender differences. Acta Neurobiologiae Experimentalis, 56(3), 779–785.
- Joynt, C., & Cheung, P. Y. (2018). Treating hypotension in preterm neonates with vasoactive medications. Frontiers in Pediatrics, 6, 86. https://doi.org/10.3389/fped.2018.00086
- Kajantie, E., Eriksson, J. G., Osmond, C., Thornburg, K., & Barker, D. J. (2009). Pre-eclampsia is associated with increased risk of stroke in the adult offspring: the Helsinki birth cohort study. Stroke, 40(4), 1176–1180. https://doi.org/10.1161/STROKEAHA.108.538025
- Kent, A. L., Wright, I. M., Abdel-Latif, M. E., New South, W., & Australian Capital Territory Neonatal Intensive Care Units Audit, G., New South Wales and Australian Capital Territory Neonatal Intensive Care Units Audit Group (2012). Mortality and adverse neurologic outcomes are greater in preterm male infants. Pediatrics, 129(1), 124–131. https://doi.org/10.1542/peds.2011-1578
- Kingston, D., McDonald, S., Austin, M. P., & Tough, S. (2015). Association between prenatal and postnatal psychological distress and toddler cognitive development: A systematic review. PLoS One, 10(5), e0126929. https://doi.org/10.1371/journal.pone.0126929
- LeFlore, J. L., Engle, W. D., & Rosenfeld, C. R. (2000). Determinants of blood pressure in very low birth weight neonates: lack of effect of antenatal steroids. Early Human Development, 59(1), 37–50. https://doi.org/10.1016/S0378-3782(00)00083-9
- Liu, Y. Z., Wang, Y. X., & Jiang, C. L. (2017). Inflammation: The common pathway of stress-related diseases. Frontiers in Human Neuroscience, 11, 316. https://doi.org/10.3389/fnhum.2017.00316
- Marangou, A. G., Alford, F. P., Ward, G., Liskaser, F., Aitken, P. M., Weber, K. M., Boston, R. C., & Best, J. D. (1988). Hormonal effects of norepinephrine on acute glucose disposal in humans: a minimal model analysis. Metabolism Clinical and Experimental, 37(9), 885–891. https://doi.org/10.1016/0026-0495(88)90124-2
- Mirghani Dirar, A., & Doupis, J. (2017). Gestational diabetes from A to Z. World Journal of Diabetes, 8(12), 489–511. https://doi.org/10.4239/wjd.v8.i12.489
- Moise, A. A., Wearden, M. E., Kozinetz, C. A., Gest, A. L., Welty, S. E., & Hansen, T. N. (1995). Antenatal steroids are associated with less need for blood pressure support in extremely premature infants. Pediatrics, 95(6), 845–850.
- O'Driscoll, D. N., McGovern, M., Greene, C. M., & Molloy, E. J. (2018). Gender disparities in preterm neonatal outcomes. Acta Paediatrica, 107(9), 1494–1499. https://doi.org/10.1111/apa.14390
- Purnell, J. Q. (2000-2018). Definitions, classification, and epidemiology of obesity. [www.endotext.org]. South Dartmouth (MA). In K. R. Feingold, B. Anawalt, A. Boyce, G. Chrousos, K. Dungan, A. Grossman, J. M. Hershman, G. Kaltsas, C. Koch, P. Kopp, M. Korbonits, R. McLachlan, J. E. Morley, M. New, L. Perreault, J. Purnell, R. Rebar, F. Singer, D. L. Trence, A. Vinik & D. P. Wilson editors.
- Reveret, M., Boivin, A., Guigonnis, V., Audibert, F., & Nuyt, A. M. (2015). Preeclampsia: effect on newborn blood pressure in the 3 days following preterm birth: a cohort study. Journal of Human Hypertension, 29(2), 115–121. https://doi.org/10.1038/jhh.2014.50
- Sterling, P., Eyer, J., Fisher, S., & Reason, J. (1988). Handbook of life stress, cognition and health. Allostasis; A new paradigm to explain arousal pathology. Wiley. 629–649.
- Szczepanska-Sadowska, E., Cudnoch-Jedrzejewska, A., Ufnal, M., & Zera, T. (2010). Brain and cardiovascular diseases: common neurogenic background of cardiovascular, metabolic and inflammatory diseases. Journal of Physiology and Pharmacology: An Official Journal of the Polish Physiological Society, 61(5), 509–521.
- Teng, R. J., Wu, T. J., Sharma, R., Garrison, R. D., & Hudak, M. L. (2006). Early neonatal hypotension in premature infants born to preeclamptic mothers. Journal of Perinatology: Official Journal of the California Perinatal Association, 26(8), 471–475. https://doi.org/10.1038/sj.jp.7211558
- Tenhola, S., Rahiala, E., Halonen, P., Vanninen, E., & Voutilainen, R. (2006). Maternal preeclampsia predicts elevated blood pressure in 12-year-old children: evaluation by ambulatory blood pressure monitoring. Pediatric Research, 59(2), 320–324. https://doi.org/10.1203/01.pdr.0000196734.54473.e3
- Tseilikman, V., Dremencov, E., Tseilikman, O., Pavlovicova, M., Lacinova, L., & Jezova, D. (2020). Role of glucocorticoid- and monoamine-metabolizing enzymes in stress-related psychopathological processes. Stress (Amsterdam, Netherlands)), 23(1), 1–12. https://doi.org/10.1080/10253890.2019.1641080
- Wapner, R., & Jobe, A. H. (2011). Controversy: antenatal steroids. Clinics in Perinatology, 38(3), 529–545. https://doi.org/10.1016/j.clp.2011.06.013
- Wong, J., Shah, P. S., Yoon, E. W., Yee, W., Lee, S., & Dow, K. (2015). Inotrope use among extremely preterm infants in Canadian neonatal intensive care units: variation and outcomes. American Journal of Perinatology, 32, 9–14. https://doi.org/10.1055/s-0034-1371703

