Abstract
Background: Despite the immense impact of COVID-19 on mental health, there is a lack of prospective studies examining physiological predictors of current risk factors. Moreover, although physiological processes evidently interact with socio-demographic factors to modulate individuals’ response to a crisis, it remains largely unknown how these complex interactions shape people’s mental responses to COVID-19. To fill these gaps of knowledge, we chose a potent physiological marker of distress – heightened baseline electrodermal activity (EDA) measured before the pandemic began - and hypothesized it would be related to greater COVID-related fears and worries as a function of individuals’ household size.
Method: 185 individuals (71% women), who had participated in our lab studies 2-3 years ago, in which we assessed their baseline EDA, completed several questionnaires online, including assessments of their current fears regarding COVID. Participants also reported the number of people in their household, with whom they had been together during a lockdown which was taking place at the time. We used pre-pandemic EDA measures in combination with their household size to predict participants’ current fears.
Results: Pre-pandemic EDA measures predicted current COVID-related fears and worries. Specifically for the EDA measure “number of skin conductance responses”, we further found that the number of people in the household during the lockdown, moderated the abovementioned relationship, such that it occurred in individuals with average and larger households and not in those with small households.
Conclusions: We provide a highly relevant and unique combination of physiological, socio-demographic, and psychological measures, which augments the potential to optimally target populations vulnerable to COVID-related distress, and subsequently offer them early mental health interventions.
Introduction
The COVID-19 pandemic poses a major challenge to psychological functioning and to mental well-being. Beyond the documented health risks, there are critical unique features to this crisis having to do with the unknown and unfolding nature of the disease, social distancing, lockdowns, isolation, and restriction on mobility (e.g. Brooks et al., Citation2020). COVID-19 has already been linked to a worldwide rise in levels of psychological distress (Berger & Reupert, Citation2020; Dong & Bouey, Citation2020; Roy et al., Citation2020). Despite these well-documented detrimental consequences, most studies to date have focused on environmental and social correlates of distress, such as socio-demographic attributes (Abrams & Szefler, Citation2020; Horesh et al., Citation2020), social isolation (Brooks et al., Citation2020), or quarantine conditions (Orgilés et al., Citation2020). Most notably, prospective studies examining pre-pandemic physiological predictors of current COVID-19-related distress, as well as their interaction with socio-demographic factors, are very scarce.
In the past, one potent physiological marker of heightened mental risk or distress has been elevated electrodermal activity (EDA). EDA denotes physiological arousal predominantly resulting from inputs of the sympathetic branch of the autonomic nervous system (ANS) (Dawson et al., Citation2016). Assessing EDA during baseline stems from literature regarding EDA lability (Crider, Citation2008; Dawson et al., Citation2016), which is defined as spontaneous fluctuations in EDA that take place during resting states in the absence of external stimuli. These labile skin conductance responses are nonspecific as they occur during baseline conditions (Gertler et al., Citation2020; Zimmer, Citation2000). Individual differences in EDA lability are regarded as a “trait” in the literature (Crider, Citation2008) and lability has been shown to be associated with a neural pattern of widespread cortical activation (Gertler et al., Citation2020). Individual differences in lability have been reported already at childhood (Gatzke-Kopp & Ram, Citation2018). Lability in EDA has been associated with increased vigilance, higher allocation of attention, increased emotional reactivity and the efforts made to regulate it (Boucsein, Citation2012; Crider, Citation2008; Dawson et al., Citation2016). Elevations in baseline EDA can thus represent increased reactivity to stress and trauma (Blechert et al., Citation2007; Kelsey, Citation1991). For instance, sustained hyperactivity of the sympathetic branch of the ANS has been described as a signature of the neurophysiology of PTSD, as evidenced in elevated EDA at baseline (Heim & Nemeroff, Citation2009; Kirsch et al., Citation2011; Pole, Citation2007; Stam, Citation2007).
Beyond EDA lability, another major framework that may be useful when connecting social contexts, such as the pandemic, with physiological indices of the ANS, like EDA, is the polyvagal theory (Porges, Citation2011). According to this theory, during times of heightened perceived insecurity or threat, the phylogenetically more ancient sympathetic branch “takes over” and consequently has the major bearing on ANS indices indicating stress and a sense of threat.
In light of the above, we suggest here that pre-pandemic heightened baseline EDA indicates a “backdrop” of SNS lability (Dawson et al., Citation2016) and possibly heightened perceived threat during routine (Benner et al., Citation2014). These pre-pandemic individual differences in physiological arousal, can be considered as physiological risk markers that may positively predict increased fears during the current COVID-19 pandemic. Specifically, we expected labile individuals with higher EDA activity at baseline to report on more COVID-related fears and worries.
The unique characteristics of the COVID-19 pandemic have generated fears and distress in several domains of functioning (Fitzpatrick et al., Citation2020; Schimmenti et al., Citation2020), some can be considered as directly influencing the integrity of the body (Ahorsu et al., Citation2020) and others can be considered as more indirect worries, highly relevant in the current pandemic (Fitzpatrick et al., Citation2020). Bodily fears have to do with getting sick with COVID or dying. Others, which are the focus of the current paper, have to do with fears relevant to the interpersonal, social, and cognitive domains which were outlined in a recent model of fears in this pandemic (Schimmenti et al., Citation2020) - such as fear for significant others and fear of not knowing. We focused here on such fear outcomes to provide a more nuanced and detailed description of worries and distress which may capture the inherent social nature of the COVID-19 pandemic.
There has been extensive work delineating how traumatic events reside within a socio-interpersonal context (Maercker & Hecker, Citation2016). This seems particularly true in the case of COVID-19, which has simultaneously influenced entire communities. We further note that in line with the biopsychosocial perspective to mental health in these times of COVID (Leonardi et al., Citation2020), there is a need to go beyond main effects to assess potential meaningful social moderators of the relationship between EDA and COVID-19 related distress. The unique social context of COVID-19 has been shown to carry various psychological implications (Guo et al., Citation2020; Singh, Citation2020). Throughout the pandemic, individuals in many countries were required to stay home, limit social interactions, and employ careful precautions when meeting other people. In addition, studies have shed light on a wide array of COVID-related worries and fears, many of which are associated with infecting others in one’s close environment (e.g. Norful et al., Citation2021). This unique combination of social limitations, fear for others’ health, and overall high level of worry, calls for studies looking deeper into the social dynamics of the pandemic. Here, we suggest that the number of people in one’s household during lockdown may be a meaningful objective socio-demographic moderator of the hypothesized relationship between pre-pandemic baseline EDA and current COVID-related fears, including fear of other’s infection with the virus. We believe this examination would combine physiological, environmental, and psychological aspects of the pandemic, into a comprehensive model of distress (e.g. Norful et al., Citation2021).
Bearing in mind the extant research regarding the mental health effects of COVID −19 (Horesh et al., Citation2020; Singh, Citation2020), there is a major gap in knowledge we aimed to address in the current study. Most psychological COVID-19 studies to date have not assessed pre-pandemic physiological markers. In a global health crisis intrinsically comprising both mental and physical health risk factors (Guo et al., Citation2020; Horesh & Brown, Citation2020), the absence of psychophysiological prospective research on COVID-19 is a scientific gap that should be critically bridged. Further, although the current health crisis involves unique, perhaps even unprecedented, social circumstances (Suppawittaya et al., Citation2020) (e.g. social distancing, lockdowns, home quarantines on a massive scale), there is very limited knowledge regarding the modulating role of these social circumstances on the relationship between physiological function and mental distress. We thus addressed this gap by assessing the interaction between pre-pandemic EDA and the number of people in the household during lockdown in predicting COVID-related fears.
In light of the above, in the current study we aimed to provide an integrative psychophysiological prospective approach to predicting worries and fears related to COVID. We will present longitudinal data from which we aimed to assess if individuals' pre-pandemic baseline physiological markers - specifically, EDA - collected 2-3 years pre-pandemic in the lab, predict individuals' current fears regarding COVID. We expected pre-pandemic EDA activity to be positively related to current COVID-19 fears and worries. Further, we expected the number of people in the household in which individuals were with during the lockdown to moderate the relationship between EDA activity and COVID fears. Specifically, we hypothesized that people who spent their lockdown with many other family members would present the strongest relationship between EDA activity and salient interpersonal concerns, such as infecting others, having a family member contract the virus or being themselves unknowingly sick. If results follow our predictions, then existing physiological data together with meaningful socio-demographic information, can help us optimally target individuals who are currently at risk to have increased distress in these times of social distancing and quarantines.
Method
Participants and procedure
One hundred and eighty-five (71% women, mean age 23.16 yrs., SD = 3.05) participants filled a COVID-19 survey during two weeks in the first COVID-19 lockdown in Israel (May and June 2020). At that time, only 34% of the participants knew someone who was infected by COVID-19, 6% of them were familiar with a person who died from it. Further, in our sample, no one was tested positive for COVID-19. Nevertheless, 20% of the participants reported a substantial reduction in income, and the financial state of 41% of them decreased, to some degree, because of the pandemic. Our sample consisted of participants who took part in one of two in-lab experiments as undergraduate students in 2017-2018 (109 in study "A" and 76 in study "B"; see details in the supplementary). Out of 185 students, we had sufficient data (physiological and survey response) for 170 participants, which was used for our analyses.
The first wave of lab studies was approved ethically by the Institutional Review Board (IRB) of the Department of Psychology at Bar-Ilan University and carried out accordingly. Informed consent was given by all participants in the lab studies. According to the guidelines of the first IRB, deidentified physiological data was kept separately from identified data. In the second wave of data collection regarding COVID-19, individuals were approached by email and asked to re-consent. The second wave of the study was also approved by the IRB of the Department of Psychology at Bar-Ilan University and all the study’s procedures were performed in accordance with this ethical approval. As mentioned above, all participants provided written informed consent for both the lab study and the COVID phase of the study. The lab studies performed 2-3 years ago (from which we derived physiological predictors) are described in detail in the Supplementary methods. During the first lockdown in Israel (May-June 2020), participants were invited via email to complete an online survey that included a few widely used psychological scales, as well as several backgrounds and COVID-19 related questions.
Measures
Background questionnaires
We asked participants for their age, gender, pre-pandemic occupation, and the number of people living in their house during the lockdown. We also asked them if they were tested for COVID-19 or found positive for the virus. Additionally, we asked if they had any common COVID-19 symptoms, whether they knew someone positive for the virus or died because of it. Lastly, we asked participants if they have suffered from an income decrease due to the pandemic (reduction in the financial state, between 0 [no reduction] to 2 [a large reduction]).
Physiological measures: EDA
We used EDA data from a baseline measurement, which took place 17-36 months prior to the COVID survey. Baseline measurements lasted for 5 minutes in which participants were asked to sit down quietly, relax, and not talk or do anything. We used MindWare Technology's cardiac impedance mobile device (Gahanna, Ohio) to collect skin conductance at 500HZ using two Ag/AgCl MindWare electrodes placed on the non-dominant palm. No additional gel was used on the electrode. Later, we analyzed the data with MindWare Technology's EDA application software, version 3.1.5. The signal was smoothed with a rolling filter of 500 data points per block. Since we tested for EDA at baseline, we did not have non-responders per-se (no stimulus was presented). The data was analyzed as one continuous signal for the full duration of 5 minutes. Visual inspection and manual editing of the data were completed by trained students to ensure proper removal of artifacts related to disconnections. When we found unusual peaks or sudden and unreasonable drops in the data, we used linear spline interpolation to replace the corrupted portions of the signal. We limited this to a maximum of 5% of each individual’s data. For cases in which an unusual peak or a drop of more than 5% of the data was identified, or in the case of a complete loss or flat line of the data, the participant’s EDA signal was excluded from the final analysis. Two main scores were outputted − 1) Mean skin conductance level in microsiemens, representing tonic EDA and 2) Number of skin conductance responses. Both scores were strongly inter-related (Pearson’s r = .532, p = .0001). Higher tonic skin conductance level (tonic SCL in microsiemens) and higher number of nonspecific skin conductance responses (NS-SCR) indicated higher physiological arousal.
COVID-19 related fears
We presented a short questionnaire, which included three items concerning fears and worries related to different aspects of the pandemic – the dependent variable in this study. Specifically, we asked participants the degree to which they were afraid of (Brooks et al., Citation2020) unknowingly carrying Coronavirus, (Roy et al., Citation2020) infecting others with the virus, and (Dong & Bouey, Citation2020) someone in their family contracting the virus. The response scale ranged on a Likert scale of 1-5 (1 = "Not afraid" to 5 = "Very afraid"; α = .75). We combined these fears to a single average COVID-related fear score which we used in further analyses due to their high inter-correlations (See Table1). Note that in all analyses, we pre-defined our alpha level to .05 (two-sided).
Results
First, we present descriptive information regarding the main study’s variables and their dispersion. In we describe correlations between the specific fears that comprised our averaged fear score and how they relate to pre-pandemic tonic SCL (in microsiemens), and the number of NS-SCRs. As can be seen, higher scores for all three fears were positively related to a higher number of NS-SCRs. Tonic SCL was positively related only to fear of unknown sickness. See for means and SEs as well as Pearson’s correlation coefficients for the main study’s variables. Household sizes ranged from one to ten. See and for a scatter plot of the data regarding COVID-19 fears and tonic SCL, and number of NS-SCRs (respectively) in our sample.
Figure 1. Individuals’ COVID-19 related fears as a function of their pre-pandemic Tonic SCL scores. A scatter plot of pre-pandemic Tonic SCL in microsiemens and COVID-related fears with a linear regression line and its corresponding 95% confidence interval. On the margins we display density plots of each of the plotted variables.
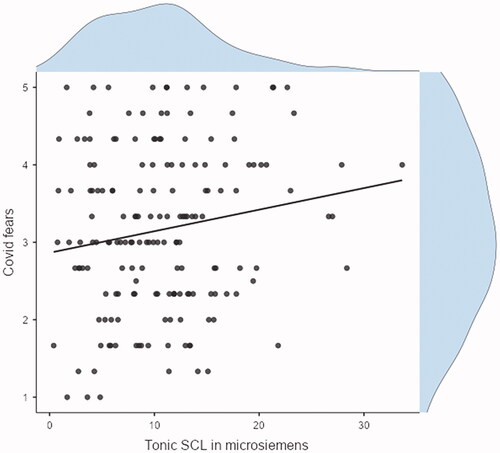
Figure 2. Individuals’ COVID-19 related fears as a function of their pre-pandemic NS-SCRs score. A scatter plot of pre-pandemic NS-SCRs and COVID-related fears with a linear regression line and its corresponding 95% confidence interval. On the margins we display density plots of each of the plotted variables.
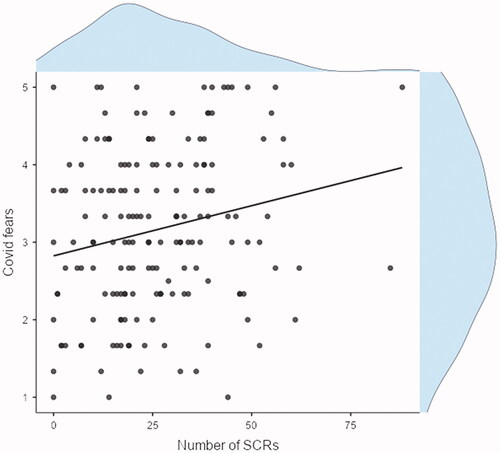
Table 1. Correlation matrix for the three specific fears comprising our COVID-19 fear score and pre-pandemic tonic SCL and number of SCRs.
Table 2. Means and SD’s of the main variables and correlations between them.
To test our hypotheses that pre-pandemic tonic SCL and pre-pandemic number of NS-SCRs predict COVID-19 related fears, and that this relation is moderated by the number of people in the household with the participant during the lockdown, we used hierarchical regression analyses.
We first examined number of NS-SCRs as a predictor, and in a separate model, we tested tonic SCL as a predictor. In both models, we introduced our covariates: gender, age, reduction in financial state, and time passed since baseline measurement (in days). These socio-demographic measures were chosen as covariates for the following reasons: We controlled for gender since there is robust evidence that fears and anxiety are related to gender (Feingold, Citation1994) and because we had an unbalanced number of men and women in our sample. We controlled for age, as it is plausible that age and number of people in the household are dependent, and we wanted to make sure that our results were due to the number of people in the household rather than age. As for the reduction in financial state, we wanted to make sure that we captured fears of the COVID and concern for others, rather than indirect impacts of financial concerns. Finally, the number of days elapsed since BL measurement was used to control for potential effects of the different lab studies participants originally took part in – which is embedded into the varying time elapsing from the first physiological measurement to the COVID survey.
The model’s first step included the the control variables and and the number of NS-SCRs (see , Step 1). This block was significantly related to COVID-19 fears (R2 = .14, p < .001), and the number of NS-SCRs was a significant predictor. In the second block, we introduced the interaction effect between pre-pandemic NS-SCRs and the number of people in the household (see , Step 2). As expected, the interaction term was a significant predictor in the modelFootnote1.
Table 3. Hierarchical regression analysis predicting COVID-19 related fears with NS-SCRs as a predictor.
In the second model, we included tonic SCL inmicrosiemens s a predictor (See ). The model’s first step included the control variables and the two main predicting variables: pre-pandemic tonic SCL in microsiemens and the number of people in the household with the participant during the first lockdown (Step 1). This block was significantly related to COVID-19 fears (R2 = .11, p < .001). In the second block, we introduced the interaction effect between pre-pandemic tonic SCL and the number of people in the household. Contrary to our hypothesis, the interaction term was not a significant predictor in our model.
To understand the interaction effect between number of NS-SCRs and household size, we performed a simple slope moderation analysis (See and below for simple slope estimates), which revealed that individuals with an average or high number of people in their household during lockdown had a strong positive relationship between baseline NS-SCRs and COVID-19 fears, whereas those with a small number of people in their household, did not have a relationship between NS-SCRs and fears.
Figure 3. Effects of pre-pandemic number of NS-SCRs on COVID-related fears among individuals who inhabited with a low, average, and high number of people in their household during the lockdown. A simple slope plot depicting the relationship between standardized pre-pandemic number of NS-SCRs and COVID fears in three subgroups in the sample – those reporting a low (-1SD; two people), an average (four people), and a high (+1SD; six people) number of people in their household during the lockdown.
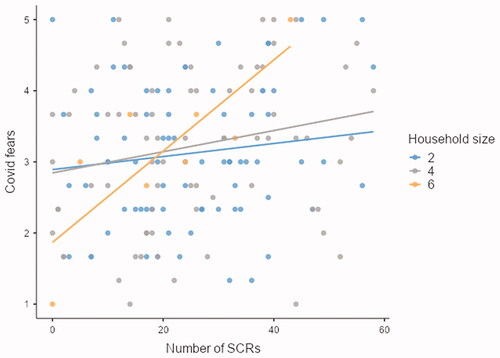
Table 4. Moderation analysis of the interaction between number of NS-SCRs and household size on covid-19 fears.
Table 5. Hierarchical regression analysis predicting COVID-19 related fears with tonic SCL, in microsiemens, as a predictor.
Discussion
In this paper, we set out to examine the associations between pre-pandemic EDA, a measure of baseline sympathetic arousal, and COVID-related fears. This is one of only a few studies to include physiological measurements taken before the pandemic as prospective predictors of peri-pandemic psychological distress. Our results reveal a positive association between EDA levels and several types of COVID-fears: unknowingly carrying the virus, infecting others with the virus, and family members’ contraction. Importantly, this EDA-fears association was moderated by the number of individuals who resided with the respondent during COVID-19, with the association failing to reach significance for those with a low number of people in the household. Finally, COVID-related fears were also associated with being female, as well as with a decrease in one’s financial status during the pandemic.
The current study contributes to a very limited, almost non-existent, literature presenting prospective examinations of pre-pandemic physiological predictors of peri-pandemic distress. Our finding that EDA baseline levels are associated with COVID fears is in line with numerous studies showing skin conductance to be a potent predictor of psychological distress in the face of trauma and crisis (Orr et al., Citation2012). Alterations in EDA, a well-known indication of physiological arousal, have been consistently associated with PTSD, such that differences in skin conductance were found between individuals with and without the disorder (Michopoulos et al., Citation2015; Pole, Citation2007). The fact that, in our study, EDA was measured 2-3 years prior to the pandemic adds another layer of complexity, as it shows the distal effects of one’s physiological makeup on one’s emotional reactions during a later crisis. Drawing from literature on EDA lability (Crider, Citation2008; Dawson et al., Citation2016) and from a diathesis-stress perspective to psychological disorders (McKeever & Huff, Citation2003), one may claim that some aspects of individuals’ physiological baseline serve as a basis for their future mental reactions under extreme circumstances (i.e. a global health pandemic). Perhaps even more importantly, our study moves beyond the simple association between baseline EDA and COVID fears, showing that this process in fact varies between individuals depending on contextual, environmental factors, which are of particular importance in these COVID days (Singh, Citation2020). Specifically, the number of people in one’s household during the pandemic moderated the association between EDA and COVID fears. Thus, for individuals who are prone to higher sympathetic lability, being in lockdown with a relatively large number of people may trigger specific fears of contagion and illness.
Interestingly, the two measures of EDA in our study did not yield the exact same pattern of results. In our models, the number of NS-SCRs was a significant predictor, whereas tonic SCL was not. Perhaps NS-SCRs are more reflective of EDA lability, which is many times assessed as increased numbers of nonspecific responses during rest (Crider, Citation2008; Dawson et al., Citation2016). Lability is also reflected by an enhanced latency for the diminishing of skin conductance responses (Crider, Citation2008; Dawson et al., Citation2016) – which should influence tonic SCL as well, and yet other trait-level factors (Crider, Citation1993; Citation2008; Crider et al., Citation2004) that are represented in tonic SCL may have come into play, and potentially explain why this measure did not come out as significant. It should be noted that these “hidden trait variables”, such as genetic factors (Crider et al., Citation2004), may also drive the association between EDA and COVD-related fears. A fuller understanding of these factors is called for in future studies.
While some studies have shown that the size of one’s household during COVID-19 is less important than the identity of those in the household (Okabe-Miyamoto et al., Citation2021), our findings indicate otherwise. It may be proposed that elevated baseline EDA reflects a basic tendency for emotional reactivity, which may subsequently lead to more stress and worry in the face of adversity. When staying at home with a large number of people, those who tend to be more physiologically and emotionally reactive may feel that they now have more people to worry about. A larger household size entails a wider variety of individuals, each may have different health status, emotional state, and vulnerabilities. Thus, this factor may play an important role in determining COVID-related mental health outcomes. Overall, these findings can be considered as a manifestation of an integrative bio-psycho-social model of COVID-19 vulnerably, which has been called for by many scholars during the past year (Wainwright & Low, Citation2020). These findings should also be viewed considering prominent biopsychological theories. According to the literature on EDA lability as a trait-like factor (Crider, Citation2008), the current results indicate that increased vigilance, emotional reactivity, or arousal at baseline is predictive of fears, worries or distress that individuals in our sample were experiencing during lockdown amidst the unfolding of the pandemic. An over-reactivity of the SNS at baseline potentially indicates a proneness or vulnerability to increased fears and worries. The Polyvagal Theory, referred to previously (Porges, Citation2011), emphasizes the complex interactions between social context and ANS activity, which yield unique responses to threat in different individuals. We believe our findings are in line with this notion, which may be particularly relevant in these days of a global pandemic. Future studies should further elaborate on the dynamics of activation of the SNS as well the parasympathetic nervous system, to reach a more comprehensive understanding of these complex processes.
Our finding that women reported greater levels of worry compared to men, is in line with numerous studies, indicating that women report higher levels of stress, anxiety and post-traumatic symptoms (Horesh et al., Citation2015). This was also found in other COVID-19 studies (Horesh et al., Citation2020). There are multiple explanations for these for gender differences (Pineles et al., Citation2017), related to biological, cognitive, and behavioral processes (McLean & Anderson, Citation2009). One explanation that may be particularly relevant to the current pandemic is that women were often found to show an increased tendency for ‘monitoring’ (i.e. looking out for signs of/information about the stressor), which may account for increased threat perception and subsequent distress (Muris & De Jong, Citation1993). Other explanations, such as stronger fear conditioning among women (Inslicht et al., Citation2013), may also be relevant for COVID-19.
Finally, an association was also found between a major deterioration in one’s financial status during COVID-19 and one’s level of worry. The economic impact of the current pandemic has been massive (Estrada et al., Citation2021), with millions around the world losing their jobs, and entire industries finding themselves on the verge of collapse. It may come as no surprise that this economic struggle may have severe mental health implications (Mann et al., Citation2020). However, what our findings interestingly show is that financial difficulties are associated with health-related fears, thus moving beyond one’s livelihood and income. This finding may be looked upon from the framework of Hobfoll’s Conservation of Resources Theory (Hobfoll, Citation1989), and its emphasis on a “spiral of losses” – a process that depicts how one resource loss (e.g. financial or emotional) may then be related to further losses, and thus subsequently be related to reduced mental health.
Our study has several limitations, including a reliance on self-report measures, which may be prone to memory or reporting biases. In addition, our EDA assessments were not all conducted at the same time, a fact that we attempted to rectify by controlling for time elapsed since the measurement. Furthermore, we did not include a general measure of psychopathology (e.g. anxiety, depression), but instead chose to rely only on three COVID-related worries. Also, while the worries measured here are indeed relevant to the pandemic and its social context, there are many more COVID worries which were not assessed (e.g. financial worries) and that should be examined in future studies vis-à-vis household size and EDA. Finally, the relatively homogeneous nature of the sample with regards to age and their academic background, makes it challenging to generalize the results to other populations, which should be a goal for future research.
These limitations notwithstanding, this study represents a novel attempt to combine pre-pandemic physiological data with peri-pandemic psychological reports. This type of research has been very scarce so far, in the face of the pandemic. Our findings have theoretical importance, as they clearly show how physiological and socio-demographic factors interact to explain the wide heterogeneity of psychological responses to COVID-19. Clinically, these findings show the importance of identifying at-risk populations (e.g. those who are a-priori more aroused; those who have limited financial resources) for whom mental health interventions may be offered. These findings also emphasize the immense importance of social context when treating the individual patient. One’s physical and emotional environment often plays a major role in one’s mental health and coping, particularly during times of crisis (Maercker & Horn, Citation2013). Finally, the integration of physiological, social, and psychological measures is crucial for better assessment and diagnosis in mental health settings – a multimodal process that may be particularly relevant for a health pandemic that carries massive effects on both body and mind.
Supplemental Material
Download Zip (29.4 KB)Disclosure statement
There is no conflict of interest to disclose.
Additional information
Funding
Notes
1 An additional analysis revealed that the interaction effect was significant also without control variables, β = .16, p = .038. A bootstrap analysis with 5,000 repetitions indicated that the effect is significant at 95% CI [b = 0.006, 0.107]. See Table S1 in the supplementary digital results file.
References
- Abrams, E. M., & Szefler, S. J. (2020). COVID-19 and the impact of social determinants of health. The Lancet Respiratory Medicine, 8(7), 659–661. https://doi.org/10.1016/S2213-2600(20)30234-4
- Ahorsu, D. K., Lin, C. Y., Imani, V., Saffari, M., Griffiths, M. D., & Pakpour, A. H. (2020). The fear of COVID-19 scale: development and initial validation. International Journal of Mental Health Addiction, 1–9. https://doi.org/10.1007/s11469-020-00270-8
- Benner, S. M., Grim, J., Approach, A. A. R., Bleiberg, E., Damasio, A. R., & Resilience, U. S. (2014). The polyvagal theory: neurophysiological foundations of emotions, attachment, communication, and self-regulation (Norton Series on Interpersonal Neurobiology), vol. 31. WW Norton & Company.
- Berger, E., & Reupert, A. (2020). The COVID-19 pandemic in Australia: lessons Learnt. Psychology Trauma, 12(5):494–496. https://doi.org/10.1037/tra0000722
- Blechert, J., Michael, T., Grossman, P., Lajtman, M., & Wilhelm, F. H. (2007). Autonomic and respiratory characteristics of posttraumatic stress disorder and panic disorder. Psychosomatic Medicine, 69(9), 935–943. https://doi.org/10.1097/PSY.0b013e31815a8f6b
- Boucsein, W. (2012). Electrodermal activity. Springer Science & Business Media.
- Brooks, S. K., Webster, R. K., Smith, L. E., Woodland, L., Wessely, S., Greenberg, N., & Rubin, G. J. (2020). The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet, 395(10227), 912–920. https://doi.org/10.1016/S0140-6736(20)30460-8
- Crider, A. (1993). Electrodermal response lability-stability: Individual difference correlates. Progress in Electrodermal Research. Springer. p. 173–186.
- Crider, A. (2008). Personality and electrodermal response lability: An interpretation. Applied Psychophysiology and Biofeedback, 33(3), 141–148. https://doi.org/10.1007/s10484-008-9057-y
- Crider, A., Kremen, W. S., Xian, H., Jacobson, K. C., Waterman, B., Eisen, S. A., Tsuang, M. T., & Lyons, M. J. (2004). Stability, consistency, and heritability of electrodermal response lability in middle-aged male twins . Psychophysiology, 41(4), 501–509. https://doi.org/10.1111/j.1469-8986.2004.00189.x
- Dawson, M. E., Schell, A. M., & Filion, D. L. (2016). The electrodermal system. In J. T. Cacioppo, L. G. Tassinary, & G. G. Berntson (Eds.), Handbook of Psychophysiology, 4th ed. Cambridge University Press, 217–243. https://doi.org/10.1017/9781107415782
- Dong, L., & Bouey, J. (2020). Public mental health crisis during COVID-19 Pandemic, China. Emerging Infectious Diseases, 26(7), 1616–1618. https://doi.org/10.3201/eid2607.200407
- Estrada, M. A. R., Koutronas, E., & Lee, M. (2021). Stagpression: The economic and financial impact of the covid-19 pandemic. Contemporary Economics, 15(1), 19–33. https://doi.org/10.5709/ce.1897-9254.433
- Feingold, A. (1994). Gender differences in personality: A meta-analysis. Psychological Bulletin, 116(3), 429–456. https://doi.org/10.1037/0033-2909.116.3.429
- Fitzpatrick, K. M., Drawve, G., & Harris, C. (2020). Facing new fears during the COVID-19 pandemic: The State of America's mental health. Journal of Anxiety Disorders, 75, 102291. https://doi.org/10.1016/j.janxdis.2020.102291
- Gatzke-Kopp, L., & Ram, N. (2018). Developmental dynamics of autonomic function in childhood. Psychophysiology, 55(11), e13218. https://doi.org/10.1111/psyp.13218
- Gertler, J., Novotny, S., Poppe, A., Chung, Y. S., Gross, J. J., Pearlson, G., & Stevens, M. C. (2020). Neural correlates of non-specific skin conductance responses during resting state fMRI. NeuroImage, 214, 116721. https://doi.org/10.1016/j.neuroimage.2020.116721
- Guo, Q., Zheng, Y., Shi, J., Wang, J., Li, G., Li, C., Fromson, J. A., Xu, Y., Liu, X., Xu, H., Zhang, T., Lu, Y., Chen, X., Hu, H., Tang, Y., Yang, S., Zhou, H., Wang, X., Chen, H., Wang, Z., & Yang, Z. (2020). Immediate psychological distress in quarantined patients with COVID-19 and its association with peripheral inflammation: A mixed-method study. Brain, Behavior, and Immunity, 88, 17–27. https://doi.org/10.1016/j.bbi.2020.05.038
- Heim, C., & Nemeroff, C. B. (2009). Neurobiology of posttraumatic stress disorder. CNS Spectrums, 14(1 Suppl 1), 13–24.
- Hobfoll, S. E. (1989). Conservation of resources. A new attempt at conceptualizing stress. The American Psychologist, 44(3), 513–524. https://doi.org/10.1037//0003-066x.44.3.513
- Horesh, D., & Brown, A. D. (2020). Covid-19 response: Traumatic stress in the age of Covid-19: A call to close critical gaps and adapt to new realities. Psychological Trauma: Theory, Research, Practice and Policy, 12(4), 331–335. https://doi.org/10.1037/tra0000592
- Horesh, D., Kapel Lev-Ari, R., & Hasson-Ohayon, I. (2020). Risk factors for psychological distress during the COVID-19 pandemic in Israel: loneliness, age, gender, and health status play an important role. British Journal of Health Psychology, 25(4):925–933. https://doi.org/10.1111/bjhp.12455
- Horesh, D., Lowe, S. R., Galea, S., Uddin, M., & Koenen, K. C. (2015). Gender differences in the long-term associations between posttraumatic stress disorder and depression symptoms: Findings from the Detroit neighborhood health study. Depression and Anxiety, 32(1), 38–48. https://doi.org/10.1002/da.22267
- Inslicht, S. S., Metzler, T. J., Garcia, N. M., Pineles, S. L., Milad, M. R., Orr, S. P., Marmar, C. R., & Neylan, T. C. (2013). Sex differences in fear conditioning in posttraumatic stress disorder. Journal of Psychiatric Research, 47(1), 64–71. https://doi.org/10.1016/j.jpsychires.2012.08.027
- Kelsey, R. M. (1991). Electrodermal lability and myocardial reactivity to stress. Psychophysiology, 28(6), 619–631. https://doi.org/10.1111/j.1469-8986.1991.tb01005.x
- Kirsch, V., Wilhelm, F. H., & Goldbeck, L. (2011). Psychophysiological characteristics of PTSD in children and adolescents: a review of the literature. Journal of Traumatic Stress, 24(2), 146–154. https://doi.org/10.1002/jts.20620
- Leonardi, M., Lee, H., van der Veen, S., Maribo, T., Cuenot, M., Simon, L., Paltamaa, J., Maart, S., Tucker, C., Besstrashnova, Y., Shosmin, A., Cid, D., Almborg, A.-H., Anttila, H., Yamada, S., Frattura, L., Zavaroni, C., Zhuoying, Q., Martinuzzi, A., … de Camargo, O. K. (2020). Avoiding the banality of evil in times of COVID-19: thinking differently with a biopsychosocial perspective for future health and social policies development. SN Comprehensive Clinical Medicine, 2(10), 1758–1760. https://doi.org/10.1007/s42399-020-00486-8
- Maercker, A., & Hecker, T. (2016). Broadening perspectives on trauma and recovery: A socio-interpersonal view of PTSD. European Journal of Psychotraumatology, 7, 29303. https://doi.org/10.3402/ejpt.v7.29303
- Maercker, A., & Horn, A. B. (2013). A socio-interpersonal perspective on ptsd: The case for environments and interpersonal processes. Clinical Psychology & Psychotherapy, 20(6), 465–481. https://doi.org/10.1002/cpp.1805
- Mann, F. D., Krueger, R. F., & Vohs, K. D. (2020). Personal economic anxiety in response to COVID-19. Personality and Individual Differences, 167, 110233. https://doi.org/10.1016/j.paid.2020.110233
- McKeever, V. M., & Huff, M. E. (2003). A diathesis-stress model of posttraumatic stress disorder: Ecological, biological, and residual stress pathways. Review of General Psychology, 7(3), 237–250. https://doi.org/10.1037/1089-2680.7.3.237
- McLean, C. P., & Anderson, E. R. (2009). Brave men and timid women? A review of the gender differences in fear and anxiety. Clinical Psychology Review, 29(6), 496–505. https://doi.org/10.1016/j.cpr.2009.05.003
- Michopoulos, V., Norrholm, S. D., & Jovanovic, T. (2015). Diagnostic biomarkers for posttraumatic stress disorder: promising horizons from translational neuroscience research. Biological Psychiatry, 78(5), 344–353. https://doi.org/10.1016/j.biopsych.2015.01.005
- Muris, P., & De Jong, P. (1993). Monitoring and perception of threat. Personality and Individual Differences , 15(4), 467–470. https://doi.org/10.1016/0191-8869(93)90075-E
- Norful, A. A., Rosenfeld, A., Schroeder, K., Travers, J. L., & Aliyu, S. (2021). Primary drivers and psychological manifestations of stress in frontline healthcare workforce during the initial COVID-19 outbreak in the United States. General Hospital Psychiatry, 69, 20–26. https://doi.org/10.1016/j.genhosppsych.2021.01.001
- Okabe-Miyamoto, K., Folk, D., Lyubomirsky, S., & Dunn, E. W. (2021). Changes in social connection during COVID-19 social distancing: It's not (household) size that matters, it's who you're with. PLoS One, 16(1), e0245009. https://doi.org/10.1371/journal.pone.0245009
- Orgilés, M., Morales, A., Delvecchio, E., Mazzeschi, C., & Espada, J. P. (2020). Immediate psychological effects of COVID-19 quarantine in youth from Italy and Spain. Frontiers Psychology, 11:579038. https://doi.org/10.2139/ssrn.3588552
- Orr, S. P., Lasko, N. B., Macklin, M. L., Pineles, S. L., Chang, Y., & Pitman, R. K. (2012). Predicting post-trauma stress symptoms from pre-trauma psychophysiologic reactivity, personality traits and measures of psychopathology. Biology of Mood & Anxiety Disorders, (2012). 2 (2), 1–12. https://doi.org/10.1186/2045-5380-2-8
- Pineles, S. L., Arditte Hall, K. A., & Rasmusson, A. M. (2017). Gender and PTSD: different pathways to a similar phenotype. Current Opinion in Psychology, 14, 44–48. https://doi.org/10.1016/j.copsyc.2016.11.002
- Pole, N. (2007). The psychophysiology of posttraumatic stress disorder: a meta-analysis. Psychological Bulletin, 133(5), 725–746. https://doi.org/10.1037/0033-2909.133.5.725
- Porges, S. W. (2011). The polyvagal theory: neurophysiological foundations of emotions, attachment, communication, and self-regulation. 161–162.
- Roy, D., Tripathy, S., Kar, S. K., Sharma, N., Verma, S. K., & Kaushal, V. (2020). Study of knowledge, attitude, anxiety & perceived mental healthcare need in Indian population during COVID-19 pandemic. Asian Journal of Psychiatry, 51, 102083. https://doi.org/10.1016/j.ajp.2020.102083
- Schimmenti, A., Billieux, J., & Starcevic, V. (2020). The four horsemen of fear: An integrated model of understanding fear experiences during the COVID-19 pandemic. Clinical Neuropsychiatry, 17, 41–45.
- Singh, J. (2020). COVID-19 and its impact on society. Electronic Research Journal of Social Sciences & Humanities, 2, 168–172.
- Stam, R. (2007). PTSD and stress sensitisation: a tale of brain and body. Part 1: Human studies. Neuroscience and Biobehavioral Reviews, 31(4), 530–557. https://doi.org/10.1016/j.neubiorev.2006.11.010
- Suppawittaya, P., Yiemphat, P., & Yasri, P. (2020). Effects of social distancing, self-quarantine and self-isolation during the COVID-19 pandemic on people ’ s well -being, and how to cope with it. International Journal of Science and Healthcare Research, 5, 12–20.
- Wainwright, T. W., & Low, M. (2020). Why the biopsychosocial model needs to be the underpinning philosophy in rehabilitation pathways for patients recovering from COVID-19. Integrated Healthcare Journal, 2(1), e000043. https://doi.org/10.1136/ihj-2020-000043
- Zimmer, H. (2000). Frequency and mean amplitude of spontaneous electrodermal fluctuations are not interchangeable indicators of psychological processes. Experimental Psychology, 47(2), 129–12943. https://doi.org/10.1026//0949-3964.47.2.129
