Abstract
Systematically review existing evidence to (1) identify the association between self-report stress and cortisol levels measured during pregnancy; and, (2) assess their association with adverse infant outcomes to determine which is the better predictor. A systematic review was conducted in accordance with PRISMA guidelines. Search terms focused on pregnancy, psychological stress and cortisol. Nine electronic databases were searched, in addition to reference lists of relevant papers. Eligibility criteria consisted of studies that included measurement of self-reported psychological stress, cortisol and assessed their associations with any infant-related outcome. Further limits included studies published in English or Spanish with human female participants. A meta-regression was not feasible due to differences in study samples, measurement tools employed, types of cortisol assessed and outcomes reported. A narrative synthesis was provided. 28 studies were eligible for inclusion. Convergent validity between self-report measures and cortisol was reported by three studies (range r = 0.12–0.41). Higher levels of self-report stress were significantly associated with intrauterine growth restriction (fetal biparietal diameter, low fetal head circumference, abdominal circumference), low gestational age at birth, low anthropometric measures (birth length, head circumference, length of the neonate), poor infant neurodevelopment (cognitive development) and potentially pathogenic gut microbiota (Clostridiaceae Clostridium, Haemophilus) in six studies. Higher cortisol levels were significantly associated with intrauterine growth restriction (fetal biparietal diameter, low fetal head circumference, abdominal circumference), low gestational age at birth, low infant birth weight, poor infant neurodevelopment (attention scores on the Network Neurobehavioral Scale) and low levels of potentially protective gut microbiota (Lactobacillus, Slackia and Actinobaculum) in 13 studies. Of the studies that assessed which type of measure was a better predictor of infant outcomes (n = 6), there was agreement that cortisol levels were statistically better at predicting adverse outcomes than self-reported stress. Self-report stress measures appear to be modest predictors of adverse infant outcomes in comparison to cortisol. A number of methodological limitations need to be addressed in future studies to help understand the relationship between cortisol and self-reported stress and how they are related to adverse infant outcomes.
Introduction
Stress is considered a leading determinant of health and disease (Orta et al., Citation2019). In the context of pregnancy, high levels of maternal stress can have negative effects and may be related to a number of adverse outcomes in the short term, such as prematurity and low infant birthweight (Babenko et al., Citation2015; Cannella et al., Citation2013; Yehuda et al., Citation2005), as well as the long-term, such as reduced childhood intelligence (LeWinn et al., Citation2009), neuroinflamation (Roshan-Milani et al., Citation2021) and a higher gain in body fat in children (Entringer et al., Citation2015; Hohwü et al., Citation2015).
Prenatal maternal stress is commonly assessed using psychological self-report measures or physiological measures (Musana et al., Citation2020). For the latter, cortisol is a frequently used biomarker to assess levels of maternal stress during pregnancy (Kirschbaum et al., Citation2009) with the analysis of the mother’s saliva, urine, blood serum, amniotic fluid or hair samples. Cortisol is a glucocorticoid hormone released through stimulation of the Hypothalamic–Pituitary–Adrenal (HPA) axis in response to stressors. It is necessary for an adequate functioning of the organism and regulates a wide range of processes, such as immunity, inflammatory responses and metabolism. It is, therefore, involved in adjustment to environmental challenges (Marieb & Hoehn, Citation2007). Cortisol helps coping with stress through the coordination of brain and body functions (Lazarus & Folkman, Citation1984). This process involves a temporary increase of cortisol secretion, which consequently boosts energy availability by incrementing muscle strength, memory, glucose and lipid metabolism, and pain threshold (Marieb & Hoehn, Citation2007). The difficulty occurs when levels of cortisol remain elevated over time. Theoretical suppositions suggest that consistently elevated levels of cortisol have an adverse impact on the infant. Various forms of prenatal stress (e.g. natural disasters, communities at war, interpersonal violence) have an impact on the placenta and its ability to metabolize cortisol (Glover et al., Citation2018; Rakers et al., Citation2017). The placenta contains an enzyme named 11-b-hydroxysteroid dehydrogenase type II (11 b-HSD2) which is a natural inhibitor by metabolizing cortisol to an inactive form cortisone (Glover, Citation2014; Glover et al., Citation2018). The activity of the 11 b-HSD2 is impaired in pregnant women exposed to high levels of prenatal stress, allowing more cortisol to pass from mother to fetus (Galbally et al., Citation2021). Added to this, cortisol levels will naturally increase over the course of pregnancy and, therefore, the function of the HPA will be affected by pregnancy (Duthie & Reynolds, Citation2013; Obel et al., Citation2005).
In relation to psychological stress measurement during pregnancy, self-report tools used to measure psychological stress are increasingly being used in research (Alderdice et al., Citation2012; Nast et al., Citation2013). Prenatal psychological stress, measured through self-report generic measures or pregnancy-specific measures, has been linked to a number of adverse infant outcomes including stillbirth, preterm birth, altered immune offspring response, fetal growth restriction and low birth weight (Coussons-Read et al., Citation2012; Ding et al., Citation2014; Lewis et al., Citation2016). Measuring psychological stress during pregnancy faces four major challenges: first, the fact that stress is a multidimensional concept (Nater, Citation2018; Preis et al., Citation2020) classified into physiological stress and psychological stress (emotional stress, cognitive stress, perceptual stress and psychosocial stress) (Lu et al., Citation2021); second, retrospective measures of stress may be biased by current stress levels (Epel et al., Citation2018); third, high levels of interindividual variation in perception of stress (the autonomic homeostatic process is involved in stress awareness (Crum et al., Citation2020; Kanbara & Fukunaga, Citation2016); fourth, that self-report generic questionnaires commonly used to assess stress might not be appropriate for use during pregnancy (Nast et al., Citation2013). Pregnancy-specific stress specifically relates to worries and concerns about the health of the fetus, relationships, diet, body weight, appearance, labor, and delivery (Yali & Lobel, Citation1999). These measures are considered to be more sensitive than generic stress measures in predicting fetal behavior, infant development and infant emotional regulation (DiPietro et al., Citation2002, Citation2006), and have been linked to preterm birth and neurodevelopmental delay (Huizink et al., Citation2003; Kramer et al., Citation2009).
While there is evidence of the association between prenatal maternal stress and infant outcomes, it is unclear whether psychological stress, using self-report measures, or physiological stress, through assessment of cortisol levels, is a better predictor of adverse infant outcomes. In this review, stress was defined as a state of homeostasis that has been challenged and consequently activates the HPA axis (Lu et al., Citation2021). This current review aims to (1) identify the association between cortisol levels and self-report measurement tools for stress and (2) determine which type of measure is the better predictor of infant outcomes, in studies where both measures were included.
Methods
A systematic review was conducted in accordance with PRISMA guidelines (Moher et al., Citation2009) to identify studies assessing associations between measures of cortisol levels during pregnancy, measures of self-report stress and infant outcomes.
Search strategy
A systematic search strategy was developed. Search terms focused on pregnancy, psychological stress, cortisol and a range of infant-related outcomes, including preterm birth, low birth weight and infant development. MeSH headings were used for search terms in addition to a number of free text terms, where needed. The electronic databases included in the search were MEDLINE, PsychInfo, CINAHL, EMBASE, Web of Science, Scopus, LILACS, LatinIndex and Redalyc. Filters were put in place to limit the search to articles that were published in English or Spanish, as these are the languages spoken by the authors, and contained human participants, to filter out research related to animal models of stress. Date of publication was not considered as a restriction in the search. The search was carried out in August 2021.
The retrieved records were independently screened by two reviewers (R.C.G and F.L.) according to the following inclusion criteria: (1) studies reporting the use of self-report measurement tools of general stress, pregnancy-specific stress or anxiety during pregnancy; (2) studies reporting biological measurements of cortisol during pregnancy; (3) studies reporting infant outcomes; (4) quantitative approach to the study design and empirical analysis. Each of these criterions had to be satisfied for inclusion in the review. Due to the fact that stress is often a poorly defined term in the literature, self-report measures of anxiety were also deemed relevant for inclusion. Studies were excluded if they only reported one method of measuring stress i.e. either self-report measures or cortisol levels. Records’ titles and abstracts were initially screened, followed by an assessment of the full text of papers that were deemed to be potentially eligible for inclusion. Two reviewers (R.C.G. and F.L.) verified the eligibility of each record and extracted data from the included studies through the use of a data extraction form designed specifically for the purpose of this review. Discrepancies at this stage were discussed by the first and second author and agreement reached.
Data extraction of study characteristics and findings was completed prior to determining any patterns in the literature. Once all data were extracted, a summary of findings of each study were tabulated and described in terms of a narrative synthesis of evidence. Methodological implications observed by included studies were reviewed relating to the different measures of stress used throughout pregnancy, including the rationale for using self-report measures and cortisol and the authors’ recommendations regarding the use of these measures.
To rate the quality of the included studies, the Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies (National Institute of Health, Citation2014) was used. The checklist consists of 14 items assessing the research question, sample size justification, independent and dependent variables’ definitions, potential confounding factors and offers a guidance for classifying the quality of each study as good, fair or poor. The use of this checklist reduces threats to internal and external validity and assists reviewers and researchers in assessing the quality of the reported study (National Institute of Health, Citation2014).
We planned to pool relevant data from studies to perform meta-regression analyses and assess the strength of associations between the stress measures and outcomes reported by pooling the mean change in an outcome given a 1 unit shift in stress. However, this was not feasible, as there was a high level of heterogeneity across the studies in the stress measures used and outcomes recorded, the timing of assessments and/or differences in the studies’ samples. Subsequently, a narrative review was presented. In addressing the primary aim of evaluate the association between self-report stress measures and cortisol levels during pregnancy, we extracted and synthesized data from studies that reported the correlation coefficient. While there are limitations in the correlation coefficient as a test for association between a dependent and independent variable, it is useful as an indicator for association between two independent variables that represent alternative approaches to measuring a concept, such as stress.
In addressing the secondary aim of this review, we firstly synthesized the evidence for each type of stress measure as a predictor for infant outcomes (intrauterine growth, infant birth weight, gestational age at birth, infants’ neurodevelopment) presented in the included studies. This included a synthesis of the patterns of findings by trimester of pregnancy, and a review of evidence related to fetal/infant sex as a moderator in the association between stress and infant outcomes. Following this, we set out to identify which type of measure was a better predictor of infant outcomes, represented by a statistically greater weight of one variable relative to another in predicting the outcome (Cohen et al., Citation2003). To achieve this, we extracted and synthesized data from included studies if they reported one of two statistical techniques. Firstly, if the study reported standardized (beta) coefficients representing the mean change in an infant outcome given a one standard deviation shift for both types of measures of stress. This would enable a direct comparison of the alternative measures of stress, assessing the degree to which an infant outcome responds to a change in each; thus, indicating which was the better predictor. Secondly, if the study reported a change in R-squared after each stress measure was added to the regression model. Any change in the R-squared would represent an improvement in the goodness of fit attributable to the last variable added, while accounting for all other independent variables. Thus, the better predictor would be the stress measure that produced the largest increase in R-squared when added to the model.
Results
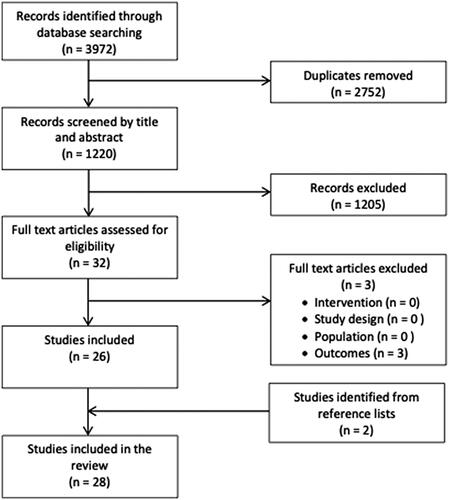
A total of 28 empirical research studies were identified as eligible for inclusion. presents the PRISMA flow diagram detailing the identification of records, screening and eligibility process. The studies were published between 1997 and 2021, inclusive, and were all conducted in high income countries, including Australia, Belgium, Ecuador, the United States, Canada, United Kingdom, Finland, the Netherlands, Sweden, Spain and Germany. Participants recruited for these studies were mainly low risk pregnant women with singleton pregnancies; although, vulnerable groups, such as pregnant women reporting depression or adolescent mothers, were reported by five of the included studies (Bolten et al., Citation2011; Doyle et al., Citation2015; Field et al., Citation2006; Pluess et al., Citation2010; Ponirakis et al., Citation1998).
Figure 1. Flow diagram for selection of studies.
summarizes the characteristics of included studies, with details on stress measures used (both self-report and cortisol), study setting, sample, timing of assessment in pregnancy, outcomes assessed, results and a quality assessment for each study.
Table 1. Summary of included studies (n = 28).
A range of psychological measures were used to assess prenatal stress. Thus, 13 studies used the Perceived Stress Scale (PSS) (Baibazarova et al., Citation2013; Bolten et al., Citation2011; Buitelaar et al., Citation2003; Caparros-Gonzalez et al., Citation2020; Davis & Sandman, Citation2010, Citation2012; Hoffman et al., Citation2016; Huizink et al., Citation2003; Jahnke et al., Citation2021a, Citation2021b; Kivlighan et al., Citation2008; Kramer et al., Citation2009; Romero-Gonzalez et al., Citation2021; Smew et al., Citation2018). Eight studies included the Pregnancy Related Anxieties Questionnaire-Revised (PRAQ-R) (Aatsinki et al., Citation2020; Baibazarova et al., Citation2013; Buitelaar et al., Citation2003; De Weerth et al., Citation2013; Goedhart et al., Citation2010; Hompes et al., Citation2012; Huizink et al., Citation2003; Kramer et al., Citation2009). Eleven studies included the State-Trait Anxiety Inventory (STAI) in their protocols (Baibazarova et al., Citation2013; Bergman et al., Citation2010; Davis & Sandman, Citation2010, Citation2012; De Weerth et al., Citation2013; Diego et al., Citation2006; Field et al., Citation2006; Goedhart et al., Citation2010; Hoffman et al., Citation2016; Kivlighan et al., Citation2008; Ponirakis et al., Citation1998). Three studies used a pregnancy-specific measure to assess stress, the Prenatal Distress Questionnaire (PDQ) (Bolten et al., Citation2011; Caparros-Gonzalez et al., Citation2020; Romero-Gonzalez et al., Citation2021). Psychological measurement was assessed at a range of time points. In this respect, the studies in this review reported the following: (1) a single measurement at the first trimester using the PRAQ and the STAI (Goedhart et al., Citation2010), and at the third trimester using the PRAQ (Goedhart et al., Citation2010), the STAI (De Weerth et al., Citation2013) or the PSS (Jahnke et al., Citation2021a, Citation2021b); (2) serial measurement using the PSS, the PRAQ, the STAI or the PDQ (Aatsinki et al., Citation2020; Baibazarova et al., Citation2013; Bolten et al., Citation2011; Buitelaar et al., Citation2003; Caparros-Gonzalez et al., Citation2020; Davis & Sandman, Citation2010, Citation2012; Hoffman et al., Citation2016; Hompes et al., Citation2012; Huizink et al., Citation2003; Ponirakis et al., Citation1998; Smew et al., Citation2018).
In respect to cortisol levels, amniotic cortisol level (acute stress measure) was assessed in two studies during the second trimester at 18 weeks of pregnancy (Baibazarova et al., Citation2013; Bergman et al., Citation2010). Blood cortisol level (acute stress measure) was assessed in three studies during the first or second trimester (Baibazarova et al., Citation2013; Bergman et al., Citation2010; Goedhart et al., Citation2010). Salivary cortisol (acute stress measure) was evaluated in 11 studies throughout pregnancy (Bolten et al., Citation2011; Buitelaar et al., Citation2003; Davis & Sandman, Citation2010, Citation2012; De Weerth et al., Citation2013; Doyle et al., Citation2015; Hompes et al., Citation2012; Huizink et al., Citation2003; Kivlighan et al., Citation2008; Ponirakis et al., Citation1998; Smew et al., Citation2018). Urinary cortisol (acute stress measure) was included in two studies during the second trimester (Diego et al., Citation2006; Field et al., Citation2006). Hair cortisol levels (retrospective stress measure) was assessed in seven studies (Aatsinki et al., Citation2020; Caparros-Gonzalez et al., Citation2020; Conradt et al., Citation2020; Galbally et al., Citation2019; Gao et al., Citation2021; Kramer et al., Citation2009; Romero-Gonzalez et al., Citation2021).
Justification for measuring stress using self-report measurement tools, as well as biological measures was given by eight of the included studies (Baibazarova et al., Citation2013; Bergman et al., Citation2010; Bolten et al., Citation2011; Buitelaar et al., Citation2003; Davis & Sandman, Citation2012; Goedhart et al., Citation2010; Hompes et al., Citation2012; Ponirakis et al., Citation1998). Justifications were based on (i) the unclear association between self-report measures, cortisol levels during pregnancy and adverse outcomes; (ii) it was unlikely that cortisol levels were the unique mechanism involved in adverse outcomes; and/or (iii) measuring both self-report and biological measures would better capture levels of prenatal maternal stress.
Association between self-report stress measures and cortisol levels during pregnancy
Seventeen studies reported tests of association between self-report stress measures and cortisol levels during pregnancy (Baibazarova et al., Citation2013; Bergman et al., Citation2010; Bolten et al., Citation2011; Conradt et al., Citation2020; Davis & Sandman, Citation2010, Citation2012; De Weerth et al., Citation2013; Diego et al., Citation2006; Doyle et al., Citation2015; Galbally et al., Citation2019; Gilles et al., Citation2018; Goedhart et al., Citation2010; Hoffman et al., Citation2016; Kivlighan et al., Citation2008; Kramer et al., Citation2009; Ramiro-Cortijo et al., Citation2021; Smew et al., Citation2018). Five studies found a significant association between high maternal prenatal stress, assessed using the Perceived Stress Scale (PSS) (r = 0.28), the State Trait Anxiety Inventory-Trait (STAI-T) (r = 0.26–0.41), the Daily Hassles Scale (r = 0.28), the UCLA Life Stress Interview (LSI) (β = 0.002), the Early Life Stress (ELS) (r = 0.123) with high cortisol levels, using hair, salivary and urinary cortisol, respectively (Conradt et al., Citation2020, Diego et al., Citation2006; Gilles et al., Citation2018; Hoffman et al., Citation2016; Kivlighan et al., Citation2008). These results were derived from studies using relatively small samples, ranging from 41 to 405 pregnant women, and only one study rated as fair quality (Diego et al., Citation2006). A single study reported an inverse association between salivary cortisol and the PSS scores (r = −0.31) (Smew et al., Citation2018). Eleven studies found no significant associations between self-report stress measures and cortisol levels during pregnancy (p > 0.05) (Baibazarova et al., Citation2013; Bergman et al., Citation2010; Bolten et al., Citation2011; Davis & Sandman, Citation2010, Citation2012; Doyle et al., Citation2015; Field et al., Citation2006; Galbally et al., Citation2019; Goedhart et al., Citation2010; Kramer et al., Citation2009; Ramiro-Cortijo et al., Citation2021).
Predictors of intrauterine fetal growth
Seven studies evaluated the correlation between self-report stress, cortisol levels and intrauterine fetal growth (Caparros-Gonzalez et al., Citation2020; Diego et al., Citation2006; Field et al., Citation2006; Gilles et al., Citation2018; Goedhart et al., Citation2010; Hompes et al., Citation2012; Ramiro-Cortijo et al., Citation2021). Intrauterine fetal growth was measured by medical ultrasonography. Regarding self-report stress, four studies found no significant associations with intrauterine fetal growth (Field et al., Citation2006; Goedhart et al., Citation2010; Hompes et al., Citation2012; Ramiro-Cortijo et al., Citation2021). Goedhart and colleagues conducted a large, good quality, prospective study (Goedhart et al., Citation2010), which lends weight to the reliability of their findings. One study found a significant association between high self-report stress scores, assessed using the STAI-T and Daily Hassles Scale, and a low intrauterine fetal growth (Diego et al., Citation2006). In this study, high STAI-T scores were significantly related to low fetal biparietal diameter (r = −0.21; p < 0.001), low fetal head circumference (r = −0.23; p < 0.05) and low abdominal circumference (r = −0.21; p < 0.05). High maternal daily hassles scores were associated with low fetal biparietal diameter (r = −0.29; p < 0.01). However, this study (Diego et al., Citation2006) was rated as fair quality due to the cross-sectional study design, conducted with a small sample of pregnant women (n = 41) with an absence of a power calculation to justify the sample size. An additional study found significant associations between high self-report stress scores, assessed using the ELS, and reduced anthropometric measures (birth length, head circumference) (r = −0.13, r = −0.18, respectively) (Gilles et al., Citation2018).
On study found a significant positive association between psychological stress during pregnancy (PDQ) and length of the neonate (β = 0.69, p < 0.05) (low stress group 50.59 cm versus high stress group 51.46 cm) and head circumference (β = 0.54, p < 0.05) (Caparros-Gonzalez et al., Citation2020).
In respect to cortisol levels, three studies, rated as good quality, found no significant associations (Goedhart et al., Citation2010; Hompes et al., Citation2012; Ramiro-Cortijo et al., Citation2021); while two studies, one of which was rated as fair quality, reported a significant relation between high urinary cortisol levels with low intrauterine fetal growth (smaller head circumference, biparietal diameter, abdominal circumference and fetal weight) (Diego et al., Citation2006; Field et al., Citation2006) and between high salivary cortisol levels and low head circumference at birth (r = −0.11). An additional study reported a positive association between hair cortisol levels and neonatal length Caparros-Gonzalez et al., Citation2020). According to these results, high cortisol levels (urinary and salivary) appeared to be a better predictor of restricted fetal growth than self-report measures; however, the evidence is limited and should be interpreted with caution.
Predictors of infant birth weight
Thirteen studies assessed associations between prenatal maternal stress, cortisol levels and infant birth weight (Baibazarova et al., Citation2013; Bolten et al., Citation2011; Buitelaar et al., Citation2003; Diego et al., Citation2006; Doyle et al., Citation2015; Field et al., Citation2006; Gilles et al., Citation2018; Goedhart et al., Citation2010; Hompes et al., Citation2012; Huizink et al., Citation2003; Kivlighan et al., Citation2008; Ponirakis et al., Citation1998; Smew et al., Citation2018). Eleven of these 13 studies were rated as good quality (Baibazarova et al., Citation2013; Bolten et al., Citation2011; Buitelaar et al., Citation2003; Doyle et al., Citation2015; Field et al., Citation2006; Gilles et al., Citation2018; Goedhart et al., Citation2010; Hompes et al., Citation2012; Huizink et al., Citation2003; Kivlighan et al., Citation2008; Smew et al., Citation2018). In relation to self-report stress measurement tools, eleven studies found no significant associations with infant birth weight (p > 0.05). A single study found a significant association between psychological stress, assessed using the ELS in a sample of 405 pregnant women, and infant birth weight (r = −0.18) (Gilles et al., Citation2018).
Regarding cortisol levels to predict infant birth weight, only eight of these 13 studies reported significant associations between maternal cortisol levels during pregnancy and infant birth weight (Baibazarova et al., Citation2013; Bolten et al., Citation2011; Diego et al., Citation2006; Field et al., Citation2006; Gilles et al., Citation2018; Goedhart et al., Citation2010; Hompes et al., Citation2012; Kivlighan et al., Citation2008). The remaining five studies found no association (Buitelaar et al., Citation2003; Doyle et al., Citation2015; Huizink et al., Citation2003; Ponirakis et al., Citation1998; Smew et al., Citation2018).
Predictors of gestational age at birth
Twelve studies assessed relations between self-report maternal stress, cortisol levels and gestational age at birth (Baibazarova et al., Citation2013; Bolten et al., Citation2011; Buitelaar et al., Citation2003; Davis & Sandman, Citation2012; Doyle et al., Citation2015; Field et al., Citation2006; Goedhart et al., Citation2010; Hoffman et al., Citation2016; Huizink et al., Citation2003; Kivlighan et al., Citation2008; Kramer et al., Citation2009; Ramiro-Cortijo et al., Citation2021), which were all rated as good quality. In respect to self-report stress measures, ten studies found no significant association with gestational age at birth (p > 0.05) (Baibazarova et al., Citation2013; Bolten et al., 2003; Buitelaar et al., Citation2003; Davis & Sandman, Citation2012; Doyle et al., Citation2015; Field et al., Citation2006; Goedhart et al., Citation2010; Huizink et al., Citation2003; Kivlighan et al., Citation2008; Ramiro-Cortijo et al., Citation2021). Only two studies reported a significant association between a self-report stress measures, assessed using the PSS and the PRAQ-R before 28 weeks of gestation, and gestational age at birth (Hoffman et al., Citation2016; Kramer et al., Citation2009). Higher self-report maternal stress was positively correlated with earlier gestational age at delivery (r = 20.30, p < 0.05) (Hoffman et al., Citation2016) and the risk of spontaneous preterm birth (OR = 1.7, 95% CI = 1.2–2.3) (Kramer et al., Citation2009).
The same two studies were also the only studies to report an association between cortisol levels during pregnancy and gestational age at birth, assessed through hair cortisol levels (Hoffman et al., Citation2016; Kramer et al., Citation2009). However, the direction of this association is unclear. Hoffman et al. (Citation2016) reported higher hair cortisol levels at 22 weeks of gestation were related to low gestational age at birth (r = 20.25, p < 0.05), while Kramer et al. (Citation2009) identified higher hair cortisol levels at delivery, reflecting stress levels during the last trimester, to be associated with higher gestational age at birth (p < 0.05). Although both studies (Hoffman et al., Citation2016; Kramer et al., Citation2009) were rated as good quality, the large sample assessed in Kramer et al.’s prospective study may support higher cortisol levels during the third trimester of pregnancy to be associated with a greater gestational age. These findings should take into consideration the possibility that the other studies may not have enough power to detect an effect size of the same size. As a conclusion, it is not clear that certain levels of stress during the third trimester of pregnancy may always lead to a shorter gestational age (Hoffman et al., Citation2016; Kramer et al., Citation2009).
Predictors of infants’ neurodevelopment
Five studies in this review, rated as good quality, assessed self-report stress measures and cortisol levels with infant neurodevelopment at 2.3 days, and at 3, 6, 8, 12 and 17 months (Bergman et al., Citation2010; Buitelaar et al., Citation2003; Davis & Sandman, Citation2010; Gao et al., Citation2021; Huizink et al., Citation2003). Infants’ neurodevelopment was assessed by using the Bayley Scales of Infant and Toddler Development (BSID) in four studies (Bergman et al., Citation2010; Buitelaar et al., Citation2003; Davis & Sandman, Citation2010; Huizink et al., Citation2003), while one study reported using the Neonatal Intensive Care Unit (NICU) Network Neurobehavioral Scale (NNNS) (Gao et al., Citation2021).
In relation to self-report prenatal stress measures all five studies reported significant associations (Bergman et al., Citation2010; Buitelaar et al., Citation2003; Davis & Sandman, Citation2010; Gao et al., Citation2021; Huizink et al., Citation2003). High maternal prenatal stress assessed using the State Trait Anxiety Inventory-State (STAI-S), Pregnancy Anxiety Questionnaire-Revised (PRAQ-R), PSS, the Pregnancy-Specific Anxiety (PSA), and the Everyday Stress Index (ESI) before the third trimester, were associated with low motor and cognitive scores on the BSID (Bergman et al., Citation2010; Buitelaar et al., Citation2003; Davis & Sandman, Citation2010; Huizink et al., Citation2003) and low attention score on the NICU NNNS (Gao et al., Citation2021).
In respect to cortisol levels to predict infants’ neurodevelopment, four studies (Bergman et al., Citation2010; Buitelaar et al., Citation2003; Davis & Sandman, Citation2010; Huizink et al., Citation2003) found significant associations. High amniotic and salivary cortisol levels during the first and second trimester were significantly related to low BSID scores in three studies (Bergman et al., Citation2010; Buitelaar et al., Citation2003; Huizink et al., Citation2003). One study found a significant association between high hair cortisol levels in the third trimester and low attention scores on the Network Neurobehavioral Scale only in female neonates (NICU NNNS) (β = −.30, p < 0.05) (Gao et al., Citation2021). One study, conducted by Davis and Sandman (Citation2010), reported high salivary cortisol levels at the third trimester of pregnancy predicted accelerated BSID scores (Mental Development Index) (t = 1.9, p < 0.05). The findings for self-reported stress and cortisol were consistent across studies.
Predictors of infant’s gut microbiota
Two studies in this review, rated as good quality, assessed self-report stress measures and cortisol levels with gut microbiota (Aatsinki et al., Citation2020; Jahnke et al., Citation2021a). In relation to self-report prenatal stress measures, the two studies reported significant associations between high prenatal stress and some potentially pathogenic infant’s gut microbiota (Aatsinki et al., Citation2020; Jahnke et al., Citation2021b). More specifically, higher scores on the PSS during the third trimester was associated with a higher presence of Clostridiaceae Clostridium at 2 months of age (Jahnke et al., Citation2021a). Higher PRAQ-R2 scores were associated with higher presence of Camplylobacter, Serratia, and Haemophilus at 2.5 months of age (FDR < 0.01) (Aatsinki et al., Citation2020).
In respect to cortisol, higher levels of hair cortisol levels during the second trimester was related with a lower presence of Lactobacillus, Slackia and Actinobaculum (phylum Actinobacteria), Paraprevotella and Butyricimonas (phylum Bacteroidetes), Citrobacter (phylum Proteobacteria), Ruminococcus, Phascolarctobacter, Anaerotruncus and Enterococcus (FDR < 0.01, absolute log2 Fold Change > 1) (Aatsinki et al., Citation2020). Besides, higher salivary cortisol levels at the third trimester was associated with a higher presence of potentially pathogenic germs (Enterobacteriaceae, Streptococcaceae, Veillonella) (p < 0.05) and a lower presence of potentially protective germs (Bifidobacterium, Lachnospiraceae) (p < 0.05) (Jahnke et al., Citation2021a).
These findings reflect the adverse consequences high levels of maternal stress during pregnancy may have on the development of potentially pathogenic germs (Aatsinki et al., Citation2020; Jahnke et al., Citation2021b).
Patterns of findings by trimester of pregnancy
During the first trimester of pregnancy, high self-report stress measures scores were associated with low gestational age at birth (Hoffman et al., Citation2016) and a low neurodevelopment (Davis & Sandman, Citation2010; Huizink et al., Citation2003), while high maternal cortisol levels were related to a low infant neurodevelopment (Davis & Sandman, Citation2010; Goedhart et al., Citation2010).
During the second trimester, higher scores on self-report stress measures were associated with a higher risk of prematurity (Kramer et al., Citation2009), low biparietal diameter and low head circumference (Diego et al., Citation2006) and low infant neurodevelopment (Buitelaar et al., Citation2003; Huizink et al., Citation2003). Higher cortisol levels through the second trimester were related to low birthweight (Bolten et al., Citation2011; Hompes et al., Citation2012), low biparietal diameter and low head circumference (Diego et al., Citation2006; Field et al., Citation2006), low gestational age at birth (Hoffman et al., Citation2016) and low infant neurodevelopment (Bergman et al., Citation2010; Davis & Sandman, Citation2010).
In the third trimester, high levels of self-report stress were linked to low levels of infant neurodevelopment (Buitelaar et al., Citation2003). Elevated cortisol levels during the third trimester were associated with low birthweight (Bolten et al., Citation2011; Kivlighan et al., Citation2008) and low infant neurodevelopment (Buitelaar et al., Citation2003; Huizink et al., Citation2003). One study found that high levels of cortisol during the third trimester were related to high infant neurodevelopment in the form of improved mental development (Davis & Sandman, Citation2010).
To sum up, high levels of stress (psychological or cortisol levels) during the first and second trimester were associated with low gestational age (Hoffman et al., Citation2016; Kramer et al., Citation2009), low birth weight (Bolten et al., Citation2011; Hompes et al., Citation2012), low biparietal diameter and low head circumference (Diego et al., Citation2006; Field et al., Citation2006), and low infant neurodevelopment (Davis & Sandman, Citation2010; Goedhart et al., Citation2010).
During the third trimester, high levels of psychological stress was associated with low levels of infant neurodevelopment (Buitelaar et al., Citation2003). In the third trimester, high cortisol levels were associated with low birthweight (Bolten et al., Citation2011; Kivlighan et al., Citation2008). Controversial findings were reported in respect to high cortisol levels during the third trimester. While two studies reported an inverse association between cortisol levels during the third trimester and infant neurodevelopment (Buitelaar et al., Citation2003; Huizink et al., Citation2003), one study suggested that high levels of cortisol levels during the third trimester may have beneficial consequences on infant mental development (Davis & Sandman, Citation2010).
Prenatal stress and infant’s sex
The moderating role of infant/fetal sex on the association of psychological stress and cortisol levels on infant development was examined in seven studies Four of these studies reported no evidence of a moderating role (De Weerth et al., Citation2013; Diego et al., Citation2006; Huizink et al., Citation2003; Ramiro-Cortijo et al., Citation2021), while three studies found that female fetal sex was a mediating factor in the association between stress and infant development when compared to male fetal sex (Bolten et al., Citation2011; Doyle et al., Citation2015; Jahnke et al., Citation2021b). Pregnant women who were experiencing stress were more likely to have an infant of lower birth weight if the infant was female (Bolten et al., Citation2011). Similarly, if women were experiencing stress, the female fetus had a less accelerated fetal heart rate compared to the male fetus (Doyle et al., Citation2015), and a lower placental 11β-hydroxysteroid dehydrogenase type 2 functioning (Jahnke et al., Citation2021b). The latter of which acts as a buffer for cortisol levels reaching the fetus.
Evidence of the better predictor of infant outcomes
Two studies reported standardized coefficients for both cortisol and self-reported stress within their regression model assessing the relationship between stress and infant outcomes (Doyle et al., Citation2015; Galbally et al., Citation2019). Doyle et al. (Citation2015) centered all predictor variables by subtracting their overall means, with their regression model providing evidence that salivary cortisol was a better predictor of the rate of developmental change in fetal heart rate than ecological momentary assessment of negative mood (β = 0.22, p ≤ 0.001 versus β= −0.03, p ≤ 0.001). Galbally et al. (Citation2019) conducted a cross-lag panel model to assess direct associations between maternal hair cortisol and state anxiety, measured in the third trimester, and infant cortisol levels at 12 months. The only statistically significant predictor of infant cortisol (measured as salivary cortisol response) was state anxiety (STAI) with a beta coefficient of −0.19 (SE = 0.07), compared to a beta coefficient of −0.13 (SE = 0.07) for hair cortisol. While all other associations were not significant, hair cortisol produced greater standardized coefficients than sate anxiety, indicating perhaps a trend of greater weight than state anxiety in explaining changes to infant cortisol reactivity.
A further study (Bergman et al., Citation2010) indicated that on assessing the association between stress and infant cognitive development, the standardized coefficient for amniotic fluid cortisol was unchanged when self-reported prenatal stress was included in the regression model. This suggested that cortisol was a better predictor of cognitive development, as the effect of prenatal stress on cognitive development was mediated by cortisol levels. Similarly, Diego et al. (Citation2006) also reported that the effect of a latent variable representing maternal distress on fetal weight was mediated by urinary cortisol levels, as the inclusion of the latter in the model reduced the coefficient with a non-significant association (β= −0.08, p ≤ 0.05 without cortisol versus β= −0.04, p ≤ 0.05 with cortisol). Hoffman et al. (Citation2016) reported that gestational age at delivery was more strongly associated with hair cortisol than perceived stress (PSS). While their analysis did not present standardized coefficients for perceived stress, they conducted a mediation analysis to assess the difference in coefficients and found that the association between perceived stress and gestational age at birth was no longer significant after the inclusion of cortisol (Δβ= −0.05, bootstrapped SE = 0.02, p = 0.04).
Three studies reported the changes in R-squared values as each measure of stress was added to their regression models (Bolten et al., Citation2011; Davis & Sandman, Citation2010; Ramiro-Cortijo et al., Citation2021). Bolten et al. (Citation2011) reported that the change in R-squared, when cortisol levels (early and late pregnancy) were added as predictors for infant birth weight, was greater than when self-reported stress (PDQ and PSS) was added (ΔR2 = 0.198, p ≤ 0.001 versus ΔR2 = 0.022, p = ≥0.05, respectively). This finding was also identified when assessing an association with infant body length at birth (ΔR2 = 0.090, p ≤ 0.05 versus ΔR2 = 0.014, p = ≥ 0.05). Thus, providing evidence of cortisol being, statistically, a better predictor of infant outcomes than self-reported prenatal stress. This greater goodness of fit was not observed by Bolten et al. (Citation2011) for infant head circumference at birth in terms of statistical significance. However, the change in R-squared value was greater with the addition of cortisol then with self-reported prenatal stress (ΔR2 = 0.055 versus ΔR2 = 0.052). Davis and Sandman (Citation2010) reported that both measures of stress (cortisol and pregnancy-specific anxiety) accounted for 12% in the variance of infant cognitive development scores on the MDI. However, the change in R-squared was greater when cortisol was added to the model than for pregnancy-specific anxiety (ΔR2 = 0.07, p ≤ 0.01 versus ΔR2 = 0.05, p ≤ 0.05), suggesting cortisol as a better predictor. Ramiro-Cortijo et al. (Citation2021) used stepwise procedures within logistic regression models to determine associations of blood cortisol levels and self-reported anxiety (HADS) in the first trimester with fetal complications (presence or not of alterations in the physiologic systems reported by echography, fetal growth restriction or preterm birth). The change in R-squared was the same (ΔR2 = 0.05, p ≤ 0.05) following sequential inclusion of both independent variables in the model.
One further study, while not reporting the change in R-squared values, did report the R-squared value for each predictor variable from principal components analyses, thus providing information on the proportion of variance in the infant outcome explained by each predictor (Hompes et al., Citation2012). For birth weight, salivary cortisol levels at mid-pregnancy represented a greater proportion of variance than anxiety, measured using HADS (R2=0.116, p ≤ 0.05 versus R2=0.011, p ≥ 0.05). Similar findings were observed for BMI at birth (R2=0.068, p ≤ 0.05 versus R2=0.001, p ≥ 0.05), and ponderal index at birth (R2=0.027, p ≤ 0.05 versus R2=0.012, p ≥ 0.05), albeit while the R-squared value was greater for salivary cortisol than for anxiety, neither proportion was statistically significant. Hompes et al. (Citation2012) concluded that cortisol, measured mid-pregnancy, may be a better predictor of infant birth weight and BMI than self-reported anxiety. However, findings from their multivariate models for stress measures taken at late pregnancy were not statistically significant with the exception of head circumference, presenting a greater R-squared value for salivary cortisol than for anxiety (R2=0.092, p ≤ 0.05 versus R2=0.000, p ≤ 0.05).
Discussion
The aim of this review was to identify studies that assessed associations between psychological stress and cortisol levels, with infant outcomes, and synthesize evidence in terms of (i) the association between maternal cortisol levels and self-reported psychological stress; and, (ii) the better predictor of infant outcomes. In summary, the majority of included studies reported no association between self-report stress measures and cortisol levels. High cortisol levels and, to a lesser extent, high self-reported stress scores were associated with adverse infant outcomes (intrauterine fetal growth, low infant birth weight, low gestational age at birth, low infant neurodevelopment and high levels of potentially pathogenic gut microbiota). These identified associations between cortisol, self-report stress and infant outcomes remained significant after adjustments for confounders were made, such as maternal age, pre-gestational body mass index, level of education, marital status or infant gender. However, where evidence was available, cortisol levels were considered a more consistent and better predictor, statistically, of adverse infant outcomes than self-reported stress.
While limited evidence of association between self-report stress and cortisol levels was identified in this review, it is possible that this finding reflects the different underlying mechanisms. However, it is difficult to interpret findings due to variations in the measures used for cortisol and self-report stress, along with the methodological flaws and bias inherent in the studies. Maternal psychological stress can activate a number of biomarkers that include cytokines, tryptophan, catecholamines, reactive oxygen species, and cortisol, which may be behind the lack of association reported between self-report psychological stress measures and cortisol levels (Rakers et al., Citation2017). Prospective studies would benefit from including both measures of self-report psychological stress and cortisol (Caparros-Gonzalez et al., Citation2018). Assessing maternal stress levels during pregnancy with self-report stress measures and cortisol may enhance the comprehension of the mechanisms involved in prematurity, low birth weight infants’ neurodevelopment and infants’ gut microbiota. Stress has several dimensions and has been classified into psychological and physiological stress (Lu et al., Citation2021). It has been reported that psychological stress can impact fetal health by activating a number of biomarkers, including cortisol (Rakers et al., Citation2017). In this review, cortisol appeared to be a better predictor than self-report stress measures of infant outcomes. Although previous studies have recommended including both measures (psychological and cortisol) (Glover, Citation2014; Lobel & Dunkel Schetter, Citation2016; Rakers et al., Citation2017), the present study found cortisol is the best predictor of infant’s outcomes. The present review has identified the statistical significance of cortisol over self-reported stress, not clinical significance. Considering other factors associated with measuring cortisol (higher cost, length of time and more invasive (Wosu et al., Citation2013), including cortisol and self-report stress measures may help studying potential associations between maternal stress and infants’ outcomes.
Associations between self-report stress, cortisol levels and intrauterine fetal growth were studied in seven studies in the present review, with one study reporting an association between higher self-report stress and low fetal head growth (Diego et al., Citation2006). A recent review reported significant associations between maternal stress and reduced fetal head growth, while other fetal growth measures showed inconclusive findings (Lewis et al., Citation2016). Fetuses exposed to high levels of maternal stress while in the womb receive low volume blood flow (Levine et al., Citation2016), which may have detrimental consequences on fetus’s growth. While cortisol metabolism during pregnancy is beneficial to fetal maturation, exposure to intense levels of cortisol can have detrimental infant effects (Hannerfors et al., Citation2015; Hellgren et al., Citation2016). A study in this review reported a positive association between maternal stress and head circumference (Caparros-Gonzalez et al., Citation2020). This finding was related to women pregnant through assisted reproductive techniques. This study agrees with previous studies reporting that high levels of stress during pregnancy or high-risk pregnant women can have infants showing a better development (Caparros-Gonzalez et al., Citation2019; Romero-Gonzalez et al., Citation2020).
Although associations between high self-report stress and low infant birthweight have been previously reported (Cannella et al., Citation2013; Ding et al., Citation2014), no association was found between self-report stress measures and infant birth weight in the majority of studies included in this review. Only a single study reported an inverse association between psychological stress and infant birth weight (Gilles et al., Citation2018). This finding is in line with a study on the adverse effects of higher prenatal stress due to a natural disaster on low infant birth weight (Dancause et al., Citation2011). This review identified that high cortisol levels were associated with low infant birth weight. These findings support previous studies reporting an inverse association between maternal cortisol levels during pregnancy with infant birthweight (Goedhart et al., Citation2010; Stewart et al., Citation2015). These results suggest that observing higher maternal cortisol levels in the prenatal period could be a risk factor for having an infant of lower than average weight at birth. Maternal cortisol levels may be a more sensitive measure than self-report tools for identifying women at risk of having a low birth weight infant.
Regarding the contradictory findings on the association between cortisol levels in the first and third trimester and gestational age at birth, previous studies support these findings. Sandman et al. (Citation2006) and Stewart et al. (Citation2015) reported an association between high cortisol levels in the first trimester and a shorter duration of gestation or preterm birth. Regular cortisol levels during pregnancy increase from the first to the third trimester, and have been observed to be higher at the end of pregnancy (Kane et al., Citation2014). While having high cortisol levels during the first trimester may have an impact on gestational age, it is expected that women in their third trimester will have higher cortisol levels, which has been associated with healthy infants (Bolten et al., Citation2011; Glover, Citation2014). Overall, the results suggest that the association between self-report maternal stress, cortisol levels and gestational age remains unclear and neither self-report stress nor cortisol levels are sensitive in identifying women at risk of preterm birth.
This review identified that high levels of self-report stress and cortisol during the first and second trimester predicted low infant neurodevelopment. This finding is consistent with previous reviews, where pregnancy-specific stress was identified as a predictor of infant neurodevelopment (Alderdice et al., Citation2012; Nast et al., Citation2013). In this respect, the present review agrees with a previous study on natural disaster-related prenatal maternal stress reporting that pregnant women exposed to an ice storm during the first or second trimester predicted a delayed brain development (Dancause et al., Citation2011). In addition, changes in the HPA axis during pregnancy, producing higher levels of cortisol, have been associated with low intelligence and low neurodevelopment in infants (Glover, Citation2014; LeWinn et al., Citation2009). Maternal cortisol levels have been associated with infant brain development through magnetic resonance imaging (MRI). Besides, psychological stress was associated with decreased functional connectivity between the amygdala and medial prefrontal cortex (mPFC) which plays a key role on the infants’ stress response (Humphreys et al., Citation2020). A recent review analyzing brain imaging reported that maternal stress is associated with modifications in the functional and microstructural connections linking limbic and frontotemporal networks among infants (Lautarescu et al., Citation2020). For example, it has been found cortical thinning and an enlarged amygdala associated with exposure to high levels of maternal stress.
Although high levels of stress during pregnancy can have adverse consequences on infant development, it has been suggested that certain levels of stress during pregnancy may be beneficial in accelerating motor and cognitive development (DiPietro et al., Citation2006). These findings are in line with a recent study reporting high cortisol levels during the third trimester were associated with a higher cognitive and gross motor infant neurodevelopment at 6 months of age (Caparros-Gonzalez et al., Citation2019). However, additional studies reported higher levels of cortisol as a predictor of low infant mental development during the first year of life (Bergman et al., Citation2010; Davis & Sandman, Citation2010) and low infant cognitive development (Glover, Citation2014). A study included in this review support that higher levels of maternal psychological stress predicted a low neurodevelopment only in female neonates (Gao et al., Citation2021). The findings from this review support the association between prenatal cortisol levels and an impaired neurodevelopment among the offspring. Previous studies assessing prenatal maternal stress due to a natural disaster (e.g. 1998 Quebec ice storm) reported that high levels of prenatal stress were associated with a delayed infant neurodevelopment (Cao et al., Citation2014) and poorer temperamental status among infants (Laplante et al., Citation2016).
Natural disasters have been described as natural quasi-experimental events that can provide an unique insight on the impact prenatal stress can have on the infants’ development (Helgertz & Bengtsson, Citation2019; Nomura et al., Citation2021). A recent meta-analytic study on the effects natural disasters may have on the infants’ health reported that maternal exposure to an ice storm, a flood or an earthquake is associated with a low cognitive, motor and behavioral development in the offspring (Lafortune et al., Citation2021).
Consideration of timing of assessment and method of measuring stress is essential when assessing levels of stress across the trimesters of pregnancy (D’Anna-Hernandez et al., Citation2011; Sandman et al., Citation2016). The validity of hair cortisol levels as a biological measure of chronic stress has previously been reported and offers beneficial aspects compared to acute cortisol measures (Wosu et al., Citation2013). Using chronic cortisol measures, such as those provided through hair samples, would reduce the impact of invasive measurements and improve the timeframes assessed (Wosu et al., Citation2013). Acute cortisol levels from blood, saliva, and urine limit the information obtained and may be influenced by situational features (Wosu et al., Citation2013).
In respect to gut microbiota, there is a growing body of evidence reporting associations between maternal stress and gut flora in offspring (Rakers et al., Citation2017; Zhang et al., Citation2021). Gut microbiota, through the bidirectional communication the gut-brain axis (GBA) represent between the enteric and the central nervous system, has a key role on the development of psychiatric disorders (e.g. Autism, Anxiety) (Carabotti et al., Citation2015). Our findings in this review highlight the negative impact prenatal stress has on infants’ gut microbiota (Aatsinki et al., Citation2020; Jahnke et al., Citation2021a). Thus, higher levels of prenatal stress were associated with low levels of Lactobacillus (Aatsinki et al., Citation2020). Lactobacillus is a beneficial bacterium for humans and can be considered a potential probiotic with benefits for the infants’ health (Sun et al., Citation2021). Moreover, in this review high levels of maternal prenatal stress were associated with high levels of Streptococcaceae and Enterobacteriaceae (Jahnke et al., Citation2021a). Streptococcaceae is a microorganism that have been associated with prematurity, premature rupture of membranes and upper respiratory tract infection and pneumonia in neonates (Ying et al., Citation2019). Enterobacteriaceae has been associated with neonatal sepsis and is usually resistant to antibiotics (Smith et al., Citation2020). A higher understanding of the mechanism of communication of the gut-brain axis may contribute to understand the long-term effects maternal stress can have on infants (Simmons et al., Citation2021).
Prenatal stress can impact infants differently depending on whether it is a male or a female infant. In this review, it was reported that certain levels of psychological maternal stress were associated with having a male infant (Gao et al., Citation2021), while higher cortisol levels were found to be associated with having a girl (Romero-Gonzalez et al., Citation2020). In this regard, a previous review reported that low sex ratio at birth (SRB) (having more females) is associated with higher levels of stress during or before pregnancy (James & Grech, Citation2017). Maternal exposure to a natural disaster was also associated with a low sex ratio at birth (Torche & Kleinhaus, Citation2012). Although male infants showed higher birthweight (Bolten et al., Citation2011; Gilles et al., 2009 ; Hompes et al., Citation2012), female infants appeared to have a better neurodevelopment than males (Bergman et al., Citation2010). This finding is in line with a previous study reporting a higher impact of prenatal stress on male infants, including higher rates of dyslexia and autism (Bale, Citation2016). Nevertheless, a study in this review found that female premature infants exposed to high levels of stress while still in the womb obtained low scores in the NICU Network Neurobehavioral Scale (Gao et al., Citation2021).
The majority of studies in this review lack of a sex-specific perspective on the impact of prenatal stress. There is evidence that maternal stress impacts differently to male and female neonates (Kortesluoma et al., Citation2021), including sex-specific associations with brain connectivity through fMRI (Graham et al., Citation2019). Future studies addressing maternal stress should include fetal sex and analyze the way prenatal stress impact infants’ outcomes from a sex-specific point of view.
Findings from this review indicate that cortisol is a better predictor of adverse infant outcomes than self-reported psychological stress. While this finding implies that future research in this area would be justified in measuring cortisol alone, there is an important reservation to this implication: the evidence implied cortisol was statistically the better predictor, not whether it was clinically the better predictor. With the use of standardized coefficients, it is not possible to determine clinical significance. As well as considering clinical significance in future observational research, further consideration should be given to whether targeting high cortisol levels is achievable during pregnancy; likewise with high self-reported stress levels. Even with a clinical and statistical understanding of the effect of high stress levels during pregnancy on adverse infant outcomes, researchers need to assess the feasibility of producing a meaningful change in stress levels. In recommending the use of self-report and biological measures for prenatal maternal stress, Bergman et al. (Citation2010) noted that cortisol alone would not be a reliable predictor of adverse outcomes. This is supported by the lack of association observed between the two types of measures, with Baibazarova et al. (Citation2013) recommending their continued measurement in further research in order to gain a better understanding of the maternal stress experience.
In terms of limitations, this review included studies that reported the use of both a self-report measure and a measure of cortisol. It is possible that these studies were not representative of the larger literature that has only examined either a self-report measure or a measure of cortisol. However, our findings are commensurate with previous reviews on associations between self-reported stress and infant outcomes (Korja et al., Citation2017) and associations between cortisol levels and infant outcomes (Cherak et al., Citation2018). In addition, many of the included studies used self-report measures of stress that have been previously reported to have low validity as measures of stress in pregnancy, including the STAI, NEO and the EMA, which may have influenced associations identified, or lack thereof, between self-reported stress and adverse infant outcomes.
In order to deal with the apparently lack of association between cortisol levels and self-report stress measures during pregnancy, future research assessing stress levels during pregnancy and its potential association should include both types of measures (cortisol and self-report measures) (Rakers et al., Citation2017).
Conclusion
Cortisol levels appear to be a better predictor of adverse infant outcomes than self-report stress measures. High cortisol levels in the first and second trimester appear to be detrimental to infant outcomes. However, inconsistent findings suggest further evidence is needed to support the psychoneuroendocrinological pathway of stress in pregnancy and alleviate its impact on infant outcomes.
Future studies on stress levels during pregnancy should have a longitudinal design to better understand the role of both physiological and psychological measures on certain trimesters of pregnancy. Moreover, it is crucial to include a sex-specific perspective when studying the role of stress during pregnancy on infant’s outcome (Kortesluoma et al., Citation2021).
Informed consent
This study is a systematic review. For this reason, no informed consent was needed and/or required.
Ethical approval
This study is a systematic review. For this reason, no ethical approval was needed and/or required.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
Notes on contributors
Rafael A. Caparros-Gonzalez
Rafael A. Caparros-Gonzalez studies the impact perinatal stress has on maternal and infant outcomes through biomarkers and self-report measures. His research focus on the fetal programming hypothesis, infant neurodevelopment and maternal post-traumatic stress disorder. He currently holds a position as assistant professor at University of Granada (Spain).
Fiona Lynn
Fiona Lynn’s works at the Department of Nursing and Midwifery at Queen’s University Belfast. Her research focus on increasing maternal and child health, particularly interested in identifying and evaluating families during the antenatal period through to the early stages of childhood. Dr. Fiona Lynn has experience of economic evaluations and intervention-based studies (randomized controlled trials, cluster RCTs, pilot trials and feasibility studies).
Fiona Alderdice
Fiona Alderdice is the Senior Social Scientist at the National Perinatal Epidemiology Unit (NPEU, University of Oxford, UK) and Professor in Perinatal Health and Wellbeing at Queen’s University Belfast. Her research interests in maternal and child health date back to 1992 when she first worked at the NPEU as a research fellow. She is a Fellow of the Higher Education Academy and a Cochrane reviewer.
Maria Isabel Peralta-Ramirez
M. Isabel Peralta- Ramirez is a full professor at the Department of Personality, Assessment and Psychological Treatment (University of Granada, Spain). Her research focus on physiological and psychological stress during pregnancy and patients with systemic lupus erythematosus.
References
- Aatsinki, A.-K., Keskitalo, A., Laitinen, V., Munukka, E., Uusitupa, H.-M., Lahti, L., Kortesluoma, S., Mustonen, P., Rodrigues, A. J., Coimbra, B., Huovinen, P., Karlsson, H., & Karlsson, L. (2020). Maternal prenatal psychological distress and hair cortisol levels associate with infant fecal microbiota composition at 2.5 months of age. Psychoneuroendocrinology, 119, 104754. https://doi.org/10.1016/j.psyneuen.2020.104754
- Alderdice, F., Lynn, F., & Lobel, M. (2012). A review and psychometric evaluation of pregnancy-specific stress measures. Journal of Psychosomatic Obstetrics and Gynaecology, 33(2), 62–77. https://doi.org/10.3109/0167482X.2012.673040
- Babenko, O., Kovalchuk, I., & Metz, G. A. (2015). Stress-induced perinatal and transgenerational epigenetic programming of brain development and mental health. Neuroscience and Biobehavioral Reviews, 48, 70–91. https://doi.org/10.1016/j.neubiorev.2014.11.013
- Baibazarova, E., van de Beek, C., Cohen-Kettenis, P. T., Buitelaar, J., Shelton, K. H., & van Goozen, S. H. (2013). Influence of prenatal maternal stress, maternal plasma cortisol and cortisol in the amniotic fluid on birth outcomes and child temperament at 3 months. Psychoneuroendocrinology, 38(6), 907–915. https://doi.org/10.1016/j.psyneuen.2012.09.015
- Bale, T. L. (2016). The placenta and neurodevelopment: Sex differences in prenatal vulnerability. Dialogues in Clinical Neuroscience, 18(4), 459–464. https://doi.org/10.31887/DCNS.2016.18.4/tbale
- Bergman, K., Sarkar, P., Glover, V., & O’Connor, T. G. (2010). Maternal prenatal cortisol and infant cognitive development: Moderation by infant-mother attachment. Biological Psychiatry, 67(11), 1026–1032. https://doi.org/10.1016/j.biopsych.2010.01.002
- Bolten, M. I., Wurmser, H., Buske-Kirschbaum, A., Papoušek, M., Pirke, K.-M., & Hellhammer, D. (2011). Cortisol levels in pregnancy as a psychobiological predictor for birth weight. Archives of Women’s Mental Health, 14(1), 33–41. https://doi.org/10.1007/s00737-010-0183-1
- Buitelaar, J. K., Huizink, A. C., Mulder, E. J., de Medina, P. G. R., & Visser, G. H. A. (2003). Prenatal stress and cognitive development and temperament in infants. Neurobiology of Aging, 24, S53–S60. https://doi.org/10.1016/S0197-4580(03)00050-2
- Cannella, D., Auerbach, M., & Lobel, M. (2013). Predicting birth outcomes: Together, mother and health care provider know best. Journal of Psychosomatic Research, 75(4), 299–304. https://doi.org/10.1016/j.jpsychores.2013.08.004
- Cao, X., Laplante, D. P., Brunet, A., Ciampi, A., & King, S. (2014). Prenatal maternal stress affects motor function in 5½‐year‐old children: Project Ice Storm. Developmental Psychobiology, 56(1), 117–125. https://doi.org/10.1002/dev.21085
- Caparros-Gonzalez, R. A., Garcia-Garcia, I., Mariñas-Lirola, J. C., & Peralta-Ramírez, M. I. (2018). GESTASTRES cohort study protocol on the effects of stress during pregnancy by measuring the cortisol in women’s and newborn’s hair. Revista Española de Salud Pública, 92, e201804027. PMID: 29658496
- Caparros-Gonzalez, R. A., Romero-Gonzalez, B., Quesada-Soto, J. M., Gonzalez-Perez, R., Marinas-Lirola, J. C., & Peralta-Ramírez, M. I. (2020). Maternal hair cortisol levels affect neonatal development among women conceiving with assisted reproductive technology. Journal of Reproductive and Infant Psychology, 37(5), 480–498. https://doi.org/10.1080/02646838.2019.1578949
- Caparros-Gonzalez, R. A., Romero-Gonzalez, B., Strivens-Vilchez, H., Gonzalez-Perez, R., Martinez-Augustin, O., & Peralta-Ramirez, M. I. (2017). Hair cortisol levels, psychological stress and psychopathological symptoms as predictors of postpartum depression. PLoS One, 12(8), e0182817. https://doi.org/10.1371/journal.pone.0182817
- Caparros-Gonzalez, R. A., Romero-Gonzalez, B., Gonzalez-Perez, R., Lucena-Prieto, L., Perez-Garcia, M., Cruz-Quintana, F., & Peralta-Ramirez, M. I. (2019). Maternal and neonatal hair cortisol levels are associated with infant neurodevelopment at six months of age. Journal of Clinical Medicine, 8(11), 2015. https://doi.org/10.3390/jcm8112015
- Carabotti, M., Scirocco, A., Maselli, M. A., & Severi, C. (2015). The gut-brain axis: Interactions between enteric microbiota, central and enteric nervous systems. Annals of Gastroenterology: quarterly Publication of the Hellenic Society of Gastroenterology, 28(2), 203. PMID: 25830558
- Cherak, S. J., Giesbrecht, G. F., Metcalfe, A., Ronksley, P. E., & Malebranche, M. E. (2018). The effect of gestational period on the association between maternal prenatal salivary cortisol and birth weight: A systematic review and meta-analysis. Psychoneuroendocrinology, 94, 49–62. https://doi.org/10.1016/j.psyneuen.2018.04.023
- Cohen, J., Cohen, P., West, S. G., & Aiken, L. S. (2003). Applied multiple regression/correlation analysis for the behavioral sciences (3rd ed.). Lawrence Erlbaum Associates Publishers.
- Conradt, E., Shakiba, N., Ostlund, B., Terrell, S., Kaliush, P., Shakib, J. H., & Crowell, S. E. (2020). Prenatal maternal hair cortisol concentrations are related to maternal prenatal emotion dysregulation but not neurodevelopmental or birth outcomes. Developmental Psychobiology, 62(6), 758–767. https://doi.org/10.1002/dev.21952
- Coussons-Read, M. E., Lobel, M., Carey, J. C., Kreither, M. O., D’Anna, K., Argys, L., Ross, R. G., Brandt, C., & Cole, S. (2012). The occurrence of preterm delivery is linked to pregnancy-specific distress and elevated inflammatory markers across gestation. Brain, Behavior, and Immunity, 26(4), 650–659. https://doi.org/10.1016/j.bbi.2012.02.009
- Crum, A. J., Jamieson, J. P., & Akinola, M. (2020). Optimizing stress: An integrated intervention for regulating stress responses. Emotion (Washington, D.C.), 20(1), 120–125. https://doi.org/10.1037/emo0000670
- Dancause, K. N., Laplante, D. P., Oremus, C., Fraser, S., Brunet, A., & King, S. (2011). Disaster-related prenatal maternal stress influences birth outcomes: Project Ice Storm. Early Human Development, 87(12), 813–820. https://doi.org/10.1016/j.earlhumdev.2011.06.007
- D’Anna-Hernandez, K. L., Ross, R. G., Natvig, C. L., & Laudenslager, M. L. (2011). Hair cortisol levels as a retrospective marker of hypothalamic-pituitary axis activity throughout pregnancy: Comparison to salivary cortisol. Physiology & Behavior, 104(2), 348–353. https://doi.org/10.1016/j.physbeh.2011.02.041
- Davis, E. P., & Sandman, C. A. (2010). The timing of prenatal exposure to maternal cortisol and psychosocial stress is associated with human infant cognitive development. Child Development, 81(1), 131–148. https://doi.org/10.1111/j.1467-8624.2009.01385.x
- Davis, E. P., & Sandman, C. A. (2012). Prenatal psychobiological predictors of anxiety risk in preadolescent children. Psychoneuroendocrinology, 37(8), 1224–1233. https://doi.org/10.1016/j.psyneuen.2011.12.016
- De Weerth, C., Buitelaar, J. K., & Beijers, R. (2013). Infant cortisol and behavioral habituation to weekly maternal separations: Links with maternal prenatal cortisol and psychosocial stress. Psychoneuroendocrinology, 38(12), 2863–2874. https://doi.org/10.1016/j.psyneuen.2013.07.014
- Diego, M. A., Jones, N. A., Field, T., Hernandez-Reif, M., Schanberg, S., Kuhn, C., & Gonzalez-Garcia, A. (2006). Maternal psychological distress, prenatal cortisol, and fetal weight. Psychosomatic Medicine, 68(5), 747–753. https://doi.org/10.1097/01.psy.0000238212.21598.7b
- Ding, X. X., Wu, Y. L., Xu, S. J., Zhu, R. P., Jia, X. M., Zhang, S. F., Huang, K., Zhu, P., Hao, J. H., & Tao, F. B. (2014). Maternal anxiety during pregnancy and adverse birth outcomes: A systematic review and meta-analysis of prospective cohort studies. Journal of Affective Disorders, 159, 103–110. https://doi.org/10.1016/j.jad.2014.02.027
- DiPietro, J. A., Hilton, S. C., Hawkins, M., Costigan, K. A., & Pressman, E. K. (2002). Maternal stress and affect influence fetal neurobehavioral development. Developmental Psychology, 38(5), 659–668. https://doi.org/10.1037/0012-1649.38.5.659
- DiPietro, J. A., Novak, M. F., Costigan, K. A., Atella, L. D., & Reusing, S. P. (2006). Maternal psychological distress during pregnancy in relation to child development at age two. Child Development, 77(3), 573–587. https://doi.org/10.1111/j.1467-8624.2006.00891.x
- Doyle, C., Werner, E., Feng, T., Lee, S., Altemus, M., Isler, J. R., & Monk, C. (2015). Pregnancy distress gets under fetal skin: Maternal ambulatory assessment & sex differences in prenatal development. Developmental Psychobiology, 57(5), 607–625. https://doi.org/10.1002/dev.21317
- Duthie, L., & Reynolds, R. M. (2013). Changes in the maternal hypothalamic-pituitary-adrenal axis in pregnancy and postpartum: Influences on maternal and fetal outcomes. Neuroendocrinology, 98(2), 106–115. https://doi.org/10.1159/000354702
- Entringer, S., Buss, C., Andersen, J., Chicz-DeMet, A., & Wadhwa, P. D. (2011). Ecological momentary assessment of maternal cortisol profiles over a multiple-day period predicts the length of human gestation. Psychosomatic Medicine, 73(6), 469–474. https://doi.org/10.1097/PSY.0b013e31821fbf9a
- Entringer, S., Buss, C., & Wadhwa, P. D. (2015). Maternal cortisol concentrations during pregnancy and infant adiposity. Psychoneuroendocrinology, 61, 13. https://doi.org/10.1016/j.psyneuen.2015.07.422
- Epel, E. S., Crosswell, A. D., Mayer, S. E., Prather, A. A., Slavich, G. M., Puterman, E., & Mendes, W. B. (2018). More than a feeling: A unified view of stress measurement for population science. Frontiers in Neuroendocrinology, 49, 146–169. https://doi.org/10.1016/j.yfrne.2018.03.001
- Field, T., Hernandez-Reif, M., Diego, M., Figueiredo, B., Schanberg, S., & Kuhn, C. (2006). Prenatal cortisol, prematurity and low birthweight. Infant Behavior and Development, 29(2), 268–275. https://doi.org/10.1016/j.infbeh.2005.12.010
- Galbally, M., van Rossum, E. F., Watson, S. J., de Kloet, E. R., & Lewis, A. J. (2019). Trans-generational stress regulation: Mother-infant cortisol and maternal mental health across the perinatal period. Psychoneuroendocrinology, 109, 104374. https://doi.org/10.1016/j.psyneuen.2019.104374
- Galbally, M., Watson, S. J., Lappas, M., de Kloet, E. R., van Rossum, E., Wyrwoll, C., Mark, P., & Lewis, A. J. (2021). Fetal programming pathway from maternal mental health to infant cortisol functioning: The role of placental 11β-HSD2 mRNA expression. Psychoneuroendocrinology, 127, 105197. https://doi.org/10.1016/j.psyneuen.2021.105197
- Gao, M. (M.), Ostlund, B., Brown, M. A., Kaliush, P. R., Terrell, S., Vlisides-Henry, R. D., Raby, K. L., Crowell, S. E., & Conradt, E. (2021). Prenatal maternal transdiagnostic, RDoC-informed predictors of newborn neurobehavior: Differences by sex. Development and Psychopathology, 33(5), 1512–1554. https://doi.org/10.1017/S0954579420002266
- Gilles, M., Otto, H., Wolf, I. A. C., Scharnholz, B., Peus, V., Schredl, M., Sütterlin, M. W., Witt, S. H., Rietschel, M., Laucht, M., & Deuschle, M. (2018). Maternal hypothalamus-pituitary-adrenal (HPA) system activity and stress during pregnancy: Effects on gestational age and infant’s anthropometric measures at birth. Psychoneuroendocrinology, 94, 152–161. https://doi.org/10.1016/j.psyneuen.2018.04.022
- Glover, V. (2014). Prenatal stress and its effects on the fetus and the child: Possible underlying biological mechanisms, perinatal programming of neurodevelopment. Springer Science + Business Media.
- Glover, V., O’Donnell, K. J., O’Connor, T. G., & Fisher, J. (2018). Prenatal maternal stress, fetal programming, and mechanisms underlying later psychopathology-a global perspective. Development and Psychopathology, 30(3), 843–854. https://doi.org/10.1017/S095457941800038X
- Goedhart, G., Vrijkotte, T. G. M., Roseboom, T. J., Van der Wal, M. F., Cuijpers, P., & Bonsel, G. J. (2010). Maternal cortisol and offspring birthweight: Results from a large prospective cohort study. Psychoneuroendocrinology, 35(5), 644–652. https://doi.org/10.1016/j.psyneuen.2009.10.003
- Graham, A. M., Rasmussen, J. M., Entringer, S., Ben Ward, E., Rudolph, M. D., Gilmore, J. H., Styner, M., Wadhwa, P. D., Fair, D. A., & Buss, C. (2019). Maternal cortisol concentrations during pregnancy and sex-specific associations with neonatal amygdala connectivity and emerging internalizing behaviors. Biological Psychiatry, 85(2), 172–181. https://doi.org/10.1016/j.biopsych.2018.06.023
- Hannerfors, A. K., Hellgren, C., Schijven, D., Iliadis, S. I., Comasco, E., Skalkidou, A., Olivier, J. D. A., & Sundström-Poromaa, I. (2015). Treatment with serotonin reuptake inhibitors during pregnancy is associated with elevated corticotropin-releasing hormone levels. Psychoneuroendocrinology, 58, 104–113. https://doi.org/10.1016/j.psyneuen.2015.04.009
- Helgertz, J., & Bengtsson, T. (2019). The long-lasting influenza: The impact of fetal stress during the 1918 influenza pandemic on socioeconomic attainment and health in Sweden, 1968–2012. Demography, 56(4), 1389–1425. https://doi.org/10.1007/s13524-019-
- Hellgren, C., Edvinsson, Å., Olivier, J. D., Fornes, R., Stener-Victorin, E., Ubhayasekera, S. J., Skalkidou, A., Bergquist, J., & Sundström-Poromaa, I. (2016). Tandem mass spectrometry determined maternal cortisone to cortisol ratio and psychiatric morbidity during pregnancy − interaction with birth weight. Psychoneuroendocrinology, 69, 142–149. https://doi.org/10.1016/j.psyneuen.2016.04.006
- Hoffman, M. C., Mazzoni, S. E., Wagner, B. D., Laudenslager, M. L., & Ross, R. G. (2016). Measures of maternal stress and mood in relation to preterm birth. Obstetrics & Gynecology, 127(3), 545–552. https://doi.org/10.1097/AOG.0000000000001287
- Hohwü, L., Henriksen, T. B., Grønborg, T. K., Hedegaard, M., Sørensen, T. I. A., & Obel, C. (2015). Maternal salivary cortisol levels during pregnancy are positively associated with overweight children. Psychoneuroendocrinology, 52, 143–152. https://doi.org/10.1016/j.psyneuen.2014.11.006
- Hompes, T., Vrieze, E., Fieuws, S., Simons, A., Jaspers, L., Van Bussel, J., Schops, G., Gellens, E., Van Bree, R., Verhaeghe, J., Spitz, B., Demyttenaere, K., Allegaert, K., Van den Bergh, B., & Claes, S. (2012). The influence of maternal cortisol and emotional state during pregnancy on fetal intrauterine growth. Pediatric Research, 72(3), 305–315. https://doi.org/10.1038/pr.2012.70
- Huizink, A. C., Robles de Medina, P. G., Mulder, E. J. H., Visser, G. H. A., & Buitelaar, J. K. (2003). Stress during pregnancy is associated with developmental outcome in infancy. Journal of Child Psychology and Psychiatry, 44(6), 810–818. https://doi.org/10.1111/1469-7610.00166
- Humphreys, K. L., Camacho, M. C., Roth, M. C., & Estes, E. C. (2020). Prenatal stress exposure and multimodal assessment of amygdala-medial prefrontal cortex connectivity in infants. Developmental Cognitive Neuroscience, 46, 100877. https://doi.org/10.1016/j.dcn.2020.100877
- Jahnke, J. R., Roach, J., Azcarate-Peril, M. A., & Thompson, A. L. (2021a). Maternal precarity and HPA axis functioning shape infant gut microbiota and HPA axis development in humans. PLoS One, 16(5), e0251782. https://doi.org/10.1371/journal.pone.0251782
- Jahnke, J. R., Terán, E., Murgueitio, F., Cabrera, H., & Thompson, A. L. (2021b). Maternal stress, placental 11β-hydroxysteroid dehydrogenase type 2, and infant HPA axis development in humans: Psychosocial and physiological pathways. Placenta, 104, 179–187. https://doi.org/10.1016/j.placenta.2020.12.008
- James, W. H., & Grech, V. (2017). A review of the established and suspected causes of variations in human sex ratio at birth. Early Human Development, 109, 50–56. https://doi.org/10.1016/j.earlhumdev.2017.03.002
- Kanbara, K., & Fukunaga, M. (2016). Links among emotional awareness, somatic awareness and autonomic homeostatic processing. BioPsychoSocial Medicine, 10(1), 11–16. https://doi.org/10.1186/s13030-016-0059-3
- Kane, H. S., Dunkel Schetter, C., Glynn, L. M., Hobel, C. J., & Sandman, C. A. (2014). Pregnancy anxiety and prenatal cortisol trajectories. Biological Psychology, 100, 13–19. https://doi.org/10.1016/j.biopsycho.2014.04.003
- Kirschbaum, C., Tietze, A., Skoluda, N., & Dettenborn, L. (2009). Hair as a retrospective calendar of cortisol production—increased cortisol incorporation into hair in the third trimester of pregnancy. Psychoneuroendocrinology, 34(1), 32–37. https://doi.org/10.1016/j.psyneuen.2008.08.024
- Kivlighan, K. T., DiPietro, J. A., Costigan, K. A., & Laudenslager, M. L. (2008). Diurnal rhythm of cortisol during late pregnancy: Associations with maternal psychological well-being and fetal growth. Psychoneuroendocrinology, 33(9), 1225–1235. https://doi.org/10.1016/j.psyneuen.2008.06.008
- Korja, R., Nolvi, S., Grant, K. A., & McMahon, C. (2017). The relations between maternal prenatal anxiety or stress and child’s early negative reactivity or self-regulation: A systematic review. Child Psychiatry and Human Development, 48(6), 851–869. https://doi.org/10.1007/s10578-017-0709-0
- Kortesluoma, S., Korhonen, L., Pelto, J., Hyttinen, S., Laine, O., Karlsson, L., & Karlsson, H. (2021). Sex differences in the associations between maternal prenatal distress and infant cortisol reactivity and recovery. Psychoneuroendocrinology, 124, 105064. https://doi.org/10.1016/j.psyneuen.2020.105064
- Kramer, M. S., Lydon, J., Séguin, L., Goulet, L., Kahn, S. R., McNamara, H., Genest, J., Dassa, C., Chen, M. F., Sharma, S., Meaney, M. J., Thomson, S., Van Uum, S., Koren, G., Dahhou, M., Lamoureux, J., & Platt, R. W. (2009). Stress pathways to spontaneous preterm birth: The role of stressors, psychological distress, and stress hormones. Am J Epidemiol, 169(11), 1319–1326. https://doi.org/10.1093/aje/kwp061
- Lafortune, S., Laplante, D. P., Elgbeili, G., Li, X., Lebel, S., Dagenais, C., & King, S. (2021). Effect of natural disaster-related prenatal maternal stress on child development and health: a meta-analytic review. International Journal of Environmental Research and Public Health, 18(16), 8332. https://doi.org/10.3390/ijerph18168332
- Laplante, D. P., Brunet, A., & King, S. (2016). The effects of maternal stress and illness during pregnancy on infant temperament: Project Ice Storm. Pediatric Research, 79(1–1), 107–113. https://doi.org/10.1038/pr.2015.177
- Lautarescu, A., Craig, M. C., & Glover, V. (2020). Prenatal stress: Effects on fetal and child brain development. International Review of Neurobiology, 150, 17–40. https://doi.org/10.1016/bs.irn.2019.11.002
- Lazarus, R. S., & Folkman, S. (1984). Stress, appraisal and coping. Springer Publishing Company.
- Levine, T. A., Alderdice, F. A., Grunau, R. E., & McAuliffe, F. M. (2016). Prenatal stress and hemodynamics in pregnancy: A systematic review. Archives of Women’s Mental Health, 19(5), 721–739. https://doi.org/10.1007/s00737-016-0645-1
- LeWinn, K. Z., Stroud, L. R., Molnar, B. E., Ware, J. H., Koenen, K. C., & Buka, S. L. (2009). Elevated maternal cortisol levels during pregnancy are associated with reduced childhood IQ. International Journal of Epidemiology, 38(6), 1700–1710. https://doi.org/10.1093/ije/dyp200
- Lewis, A. J., Austin, E., & Galbally, M. (2016). Prenatal maternal mental health and fetal growth restriction: A systematic review. Journal of Developmental Origins of Health and Disease, 7(4), 416–428. https://doi.org/10.1017/S2040174416000076
- Lobel, M., & Dunkel Schetter, C. (2016). Pregnancy and prenatal stress. Academic Press.
- Lu, S., Wei, F., & Li, G. (2021). The evolution of the concept of stress and the framework of the stress system. Cell Stress, 5(6), 76–85. https://doi.org/10.15698/cst2021.06.250
- Marieb, E. N., & Hoehn, K. (2007). Human anatomy and physiology. Benjamin Cumming.
- Moher, D., Liberati, A., Tetzlaff, J., & Altman, D. G. (2009). Preferred Reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ (Clinical Research ed.), 339(jul21 1), b2535. https://doi.org/10.1136/bmj.b2535
- Musana, W., Cohen, R., Kuppermann, M., Gerona, R., Wanyoro, A., Aguilar, D., Santos, N., Temmerman, M., & Weiss, S. J. (2020). Association of differential symptoms of stress to hair cortisol and cortisone concentrations among pregnant women in Kenya. Stress (Amsterdam, Netherlands), 23(5), 556–566. https://doi.org/10.1080/10253890.2019.1696305
- Nast, I., Bolten, M., Meinlschmidt, G., & Hellhammer, D. H. (2013). How to measure prenatal stress? A systematic review of psychometric instruments to assess psychosocial stress during pregnancy. Paediatric and Perinatal Epidemiology, 27(4), 313–322. https://doi.org/10.1111/ppe.12051
- Nater, U. M. (2018). The multidimensionality of stress and its assessment. Brain, Behavior, and Immunity, 73, 159–160. https://doi.org/10.1016/j.bbi.2018.07.018
- National Institute of Health (2014). Quality assessment tool for observational cohort and cross-sectional studies. http://www.nhlbi.nih.gov/health-pro/guidelines/in-develop/cardiovascular-risk-reduction/tools/cohort
- Nomura, Y., Rompala, G., Pritchett, L., Aushev, V., Chen, J., & Hurd, Y. L. (2021). Natural disaster stress during pregnancy is linked to reprogramming of the placenta transcriptome in relation to anxiety and stress hormones in young offspring. Molecular Psychiatry, 26(11), 6511–6520. https://doi.org/10.1038/s41380-021-01123-z
- Obel, C., Hedegaard, M., Henriksen, T. B., Secher, N. J., Olsen, J., & Levine, S. (2005). Stress and salivary cortisol during pregnancy. Psychoneuroendocrinology, 30(7), 647–656. https://doi.org/10.1016/j.psyneuen.2004.11.006
- Orta, O. R., Tworoger, S. S., Terry, K. L., Coull, B. A., Gelaye, B., Kirschbaum, C., Sanchez, S. E., & Williams, M. A. (2019). Stress and hair cortisol concentrations from preconception to the third trimester. Stress (Amsterdam, Netherlands), 22(1), 60–69. https://doi.org/10.1080/10253890.2018.1504917
- Pluess, M., Bolten, M., Pirke, K. M., & Hellhammer, D. (2010). Maternal trait anxiety, emotional distress, and salivary cortisol in pregnancy. Biological Psychology, 83(3), 169–175. https://doi.org/10.1016/j.biopsycho.2009.12.005
- Ponirakis, A., Susman, E. J., & Stifter, C. A. (1998). Negative emotionality and cortisol during adolescent pregnancy and its effects on infant health and autonomic nervous system reactivity. Developmental Psychobiology, 33(2), 163–174. https://doi.org/10.1002/(SICI)1098-2302(199809)33:2<163::AID-DEV7>3.0.CO;2-H
- Preis, H., Mahaffey, B., & Lobel, M. (2020). Psychometric properties of the pandemic-related pregnancy stress scale (PREPS). Journal of Psychosomatic Obstetrics and Gynaecology, 41(3), 191–197. https://doi.org/10.1080/0167482X.2020.1801625
- Rakers, F., Ruprecht, S., Dreiling, M., Bergmeier, C., Witte, O. W., & Schwab, M. (2017). Transfer of maternal psychosocial stress to the fetus. Neuroscience & Biobehavioral Reviews, 117, 185–197. https://doi.org/10.1016/j.neubiorev.2017.02.019
- Ramiro-Cortijo, D., De la Calle, M., Benitez, V., Gila-Diaz, A., Moreno-Jiménez, B., Arribas, S. M., & Garrosa, E. (2021). Maternal psychological and biological factors associated to gestational complications. Journal of Personalized Medicine, 11(3), 183. https://doi.org/10.3390/jpm11030183
- Romero-Gonzalez, B., Puertas-Gonzalez, J. A., Gonzalez-Perez, R., Davila, M., & Peralta-Ramirez, M. I. (2021). Hair cortisol levels in pregnancy as a possible determinant of fetal sex: A longitudinal study. Journal of Developmental Origins of Health and Disease, 12(6), 902–906. https://doi.org/10.1017/S2040174420001300
- Romero-Gonzalez, B., Caparros-Gonzalez, R. A., Cruz-Martinez, M., Gonzalez-Perez, R., Gallego-Burgos, J. C., & Peralta-Ramirez, M. I. (2020). Neurodevelopment of high and low-risk pregnancy babies at 6 months of age. Midwifery, 89, 102791. https://doi.org/10.1016/j.midw.2020.102791
- Roshan-Milani, S., Seyyedabadi, B., Saboory, E., Parsamanesh, N., & Mehranfard, N. (2021). Prenatal stress and increased susceptibility to anxiety-like behaviors: role of neuroinflammation and balance between GABAergic and glutamatergic transmission. Stress (Amsterdam, Netherlands), 24(5), 415–481. https://doi.org/10.1080/10253890.2021.1942828
- Sandman, C. A., Glynn, L., Schetter, C. D., Wadhwa, P., Garite, T., Chicz-DeMet, A., & Hobel, C. (2006). Elevated maternal cortisol early in pregnancy predicts third trimester levels of placental corticotropin releasing hormone (CRH): Priming the placental clock. Peptides, 27(6), 1457–1463. https://doi.org/10.1016/j.peptides.2005.10.002
- Sandman, C. A., Glynn, L. M., & Davis, E. P. (2016). Neurobehavioral consequences of fetal exposure to gestational stress. In N. Reissland & S. B. Kisilevsky (Eds.). Fetal development: Research on brain and behavior, environmental influences, and emerging technologies. Springer International.
- Simmons, J. M., Winsky, L., Zehr, J. L., & Gordon, J. A. (2021). Priorities in stress research: A view from the US National Institute of Mental Health. Stress (Amsterdam, Netherlands), 24(2), 123–129. https://doi.org/10.1080/10253890.2020.1781084
- Smew, A. I., Hedman, A. M., Chiesa, F., Ullemar, V., Andolf, E., Pershagen, G., & Almqvist, C. (2018). Limited association between markers of stress during pregnancy and fetal growth in ‘Born into Life’, a new prospective birth cohort. Acta Paediatrica (Oslo, Norway : 1992), 107(6), 1003–1010. https://doi.org/10.1111/apa.14246
- Smith, A., Anandan, S., Veeraraghavan, B., & Thomas, N. (2020). Colonization of the preterm neonatal gut with carbapenem-resistant Enterobacteriaceae and its association with neonatal sepsis and maternal gut flora. Journal of Global Infectious Diseases, 12(2), 101–104. https://doi.org/10.4103/jgid.jgid_104_19
- Stewart, C. P., Oaks, B. M., Laugero, K. D., Ashorn, U., Harjunmaa, U., Kumwenda, C., Chaima, D., Maleta, K., Ashorn, P., & Dewey, K. G. (2015). Maternal cortisol and stress are associated with birth outcomes, but are not affected by lipid-based nutrient supplements during pregnancy: an analysis of data from a randomized controlled trial in rural Malawi. BMC Pregnancy and Childbirth, 15, 346. https://doi.org/10.1186/s12884-015-0793-8
- Sun, M., Luo, J., Liu, H., Xi, Y., & Lin, Q. (2021). Can mixed strains of lactobacillus and bifidobacterium reduce eczema in infants under three years of age? A meta-analysis. Nutrients, 13(5), 1461. https://doi.org/10.3390/nu13051461
- Torche, F., & Kleinhaus, K. (2012). Prenatal stress, gestational age and secondary sex ratio: The sex-specific effects of exposure to a natural disaster in early pregnancy. Human Reproduction, 27(2), 558–567. https://doi.org/10.1093/humrep/der390
- Wosu, A. C., Valdimarsdóttir, U., Shields, A. E., Williams, D. R., & Williams, M. A. (2013). Correlates of cortisol in human hair: Implications for epidemiologic studies on health effects of chronic stress. Annals of Epidemiology, 23(12), 797–811.e792. https://doi.org/10.1016/j.annepidem.2013.09.006
- Yali, A. M., & Lobel, M. (1999). Coping and distress in pregnancy: An investigation of medically high risk women. Journal of Psychosomatic Obstetrics and Gynaecology, 20(1), 39–52. https://doi.org/10.3109/01674829909075575
- Yehuda, R., Engel, S. M., Brand, S. R., Seckl, J., Marcus, S. M., & Berkowitz, G. S. (2005). Transgenerational effects of posttraumatic stress disorder in babies of mothers exposed to the World Trade Center attacks during pregnancy. The Journal of Clinical Endocrinology and Metabolism, 90(7), 4115–4118. https://doi.org/10.1210/jc.2005-0550
- Ying, F., ChengFang, X., YanZhen, R., XiaoLan, D., & Ke, S. (2019). Clinical study on screening and pregnancy outcome of group B streptococcal infection in pregnant women in late pregnancy. Chinese Journal of Nosocomiology, 29(3), 440–447.
- Zhang, Z., Li, N., Chen, R., Lee, T., Gao, Y., Yuan, Z., Nie, Y., & Sun, T. (2021). Prenatal stress leads to deficits in brain development, mood related behaviors and gut microbiota in offspring. Neurobiology of Stress, 15, 100333. https://doi.org/10.1016/j.ynstr.2021.100333
