?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.1. Introduction
The Fractional Flow Reserve (FFR) is a clinical index of functional severity validated for isolated stenoses. FFR may be viewed as the ratio of achievable blood flow in a stenotic artery to the theoretic healthy flow in the same artery. FFR values < 0.75 lead to an insufficient blood irrigation of the myocardium, whereas FFR values > 0.80 are considered to be safe. A significant stenosis in the left main (LM) coronary artery is a dangerous configuration, commonly accompanied by downstream lesions in the daughter arteries and collateral flows. Collateral circulation is an alternative flow increasing total myocardial flow in obstructive coronary disease (Seiler et al. Citation2013). In these complex configurations, the individual apparent FFR, ( is the measured FFR in the presence of downstream stenoses) of the LM coronary is not representative of the actual severity of the LM lesion. To address this issue, several reduced order (0 D) models have been developed to predict the true hemodynamic FFR (FFRTrue) of the LM stenosis in multiple stenoses configuration. This FFRTrue is the FFR of the the LM lesion if the downstream lesions were removed and is the true indicator of the severity of LM lesion. According to our knowledge, the proposed model is the first one to consider simultaneously: 1) LM stenoses with up to two downstream lesions, 2) the fractal geometry (as defined by Finet et al. Citation2010) of vascular trees, and 3) the influence of collateral circulation. The final goal of this model is to assist interventional cardiologists during decision making for revascularization for complex configurations.
2. Methods
2.1. Reduced order model
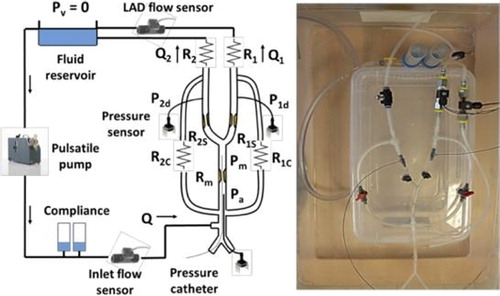
Assuming that the Poiseuille law is valid for the flow in coronaries (Huo and Kassab Citation2009; Kweon et al. Citation2016; Yamamoto et al. Citation2016), an equivalent electrical circuit can be used. In this study, the two collateral flows supplying the Left anterior descending coronary artery (LAD) and Left circumflex coronary artery (LCx) were considered to come from the right coronary artery. illustrates the proposed coronary flow model of the LM bifurcation. A general equation, based on this circuit, was derived to predict the FFRTrue of the LM stenosis (cf. Coppel et al. Citation2019):
(1)
(1)
Figure 1. Electrical analogy of an LM bifurcation supplying the myocardial resistances R1 and R2 with one LM stenosis (Rm), two downstream lesions (R1S and R2S) and two collateral (R1C and R2C).
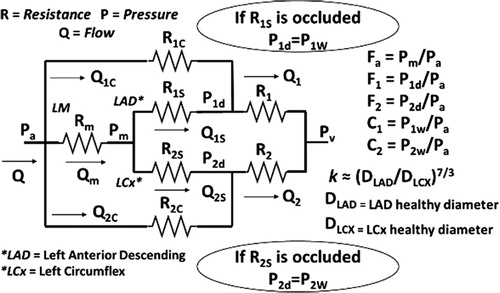
Where FA, F1 and F2 represent the FFRApp of the LM lesion, the composite FFR of LM plus LAD lesions and the composite FFR of LM plus LCx lesions, respectively, C1 and C2 represent the collateral flow indexes (i.e. measured during momentary arterial occlusion) for the LAD and LCx, respectively, and ‘k’ represents the flow ratio between healthy LAD and LCx branches (i.e. without stenoses), obtained with the flow scaling law (Huo and Kassab Citation2009), P1w and P2w are the wedge pressures during the occlusion of the LAD and LCX respectively.
Moreover, an in vitro model mimicking the fractal geometry of LM bifurcation trees with variable collateral flows (Cf. ) was developed to experimentally study the effect of various parameter on the FFR and compare these values with predicted
FFR (). Different collateral flow developments and random downstream lesion severities was used to validate the performance of the proposed model on a moderate LM stenosis about 80% of diameter reduction. The proposed model was compared to Yamamoto’s one (Yamamoto et al. Citation2016) which covers the same lesion configuration but without collateral flow, and to Kweon’s one (Kweon et al. Citation2016) which considers just one downstream lesion and a constant collateral flow index (i.e. CFI = 0.25).
3. Results and discussion
Using 50 experiments, 25 for one downstream lesion and 25 for two downstream lesions, the error
of the proposed model was compared to the ones of previous approaches ().
Figure 3. Histograms of mean absolute FFR differentials for a 80% LM stenosis A) with one downstream lesion, B) with two downstream lesions.
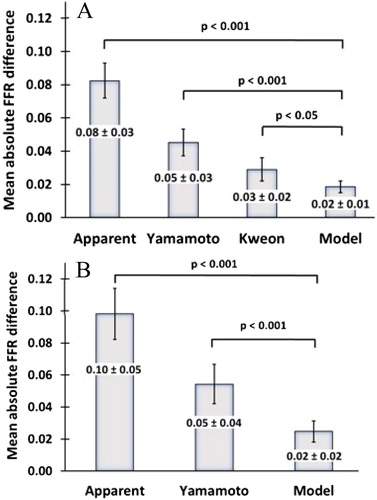
The accuracy obtained with the proposed model was significantly higher (p-value < 0.001) by a factor of two when compared to the second-best approach. As illustrated on , the proposed model significantly improved the accuracy of the predicted FFR value for one or two downstream stenoses. The proposed theoretical equation, developed and compared with in vitro results, successfully predicted the true FFR of the LM atherosclerotic lesion with one or two downstream stenoses and two distinct collateral circulations supplying the LAD and LCx branches.
Moreover, and in vitro measurements (Coppel et al, Citation2019) highlight the significant effect of the development of collateral circulation on the true FFR.
4. Conclusions
Collateral development may be a new prognostic factor to predict accurately the true severity of an LM stenosis with downstream lesions, and a key element to improve our understanding of how collaterals modulate the apparent severity of atherosclerotic lesions. The proposed model provides interesting information to assist interventional cardiologists during decision making for revascularization.
Additional information
Funding
References
- Coppel R, Lagache M, Finet G, Rioufol G, Gómez A, Dérimay F, Malvé M, Yazdani SK, Pettigrew RI, Ohayon J. 2019. Influence of collaterals on true FFR prediction for a left main stenosis with concomitant lesions: an in vitro study. Ann Biomed Eng. 47(6):1409–1421.
- Finet G, Huo Y, Rioufol G, Ohayon J, Guerin P, Kassab GS. 2010. Structure-function relation in the coronary artery tree: from fluid dynamics to arterial bifurcations. EuroInter. 6:10–15.
- Huo Y, Kassab GS. 2009. A scaling law of vascular volume. Biophys J. 96(2):347–353.
- Kweon J, Kim YH, Yang DH, Lee JG, Roh JH, Mintz GS, Lee SW, Park SW. 2016. In vivo validation of mathematically derived fractional flow reserve for assessing haemodynamics of coronary tandem lesions. EuroInter. 12:1375–1384.
- Seiler C, Stoller M, Pitt B, Meier P. 2013. The human coronary collateral circulation: Dev. and clinical importance. Eur Heart J. 34(34):2674–2682.
- Yamamoto E, Saito N, Matsuo H, Kawase Y, Watanabe S, Bao B, Watanabe H, Higami H, Nakatsuma K, Kimura T. 2016. Prediction of the true fractional flow reserve of left main coronary artery stenosis with concomitant downstream stenoses: in vitro and in vivo experiments. EuroInter. 11:1249–1256.