1. Introduction
Mandibular ramus sagittal osteotomy is a common surgical intervention in orthognathic and maxillofacial surgery, which consists in creating a directed fracture along the alveolar inferior nerve canal. It allows the surgeon to separate the mandible into two parts, an internal part carrying the denture, and an external part carrying the temporo-mandibular joint. Performed on both sides, it allows one to locate the dentulate part of the mandible to correct maxillae and mandibular dysmorphia. One common complication is the wrong cleavage of the mandible, called “bad split”, which provokes a highly unstable fracture and jeopardizes the whole intervention. This intervention requires some experience but is frequently practiced in daily routine, which is why young surgeons should be able to train themselves on relevant anatomic models. However, in anatomic courses, young and fully dentulate specimen, with trophic bone, are difficult to obtain. Finally, with 3D printing, not only could one obtain “standard patient models”, but also pathological ones, that could lead to further applications. On the road to a biomechanically referring reliable 3D printed mandible model, the first step - the subject of the study described here - is to characterize the relevant biomechanical properties regarding ramus sagittal osteotomy using cadaveric samples.
2. Methods
2.1. Surgical technique
The ramus sagittal osteotomy comprehends 3 steps: the corticotomy, performed using a Lindeman burr through the cortical surface to access the medullar bone, the split preparation, performed using an osteotome and a mallet with special care brought to create a passage externally to the alveolar mandibular nerve, and the final cleavage, which consists in a directed fracture trough the unreachable cortical lingual bone ().
2.2. Sampling
We sampled 5 fully or partially dentulate human anatomic full mandibles and split them in two, the right side was used for the hardness tests and the left side was used for the traction-to-fracture test within an unfinished ramus sagittal osteotomy.
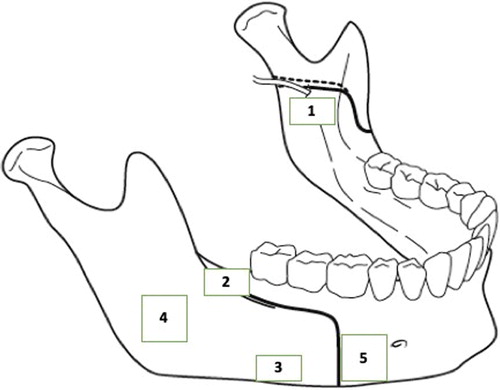
Each right side was sampled in 5 parts underlying the osteotomy course, and each sample was listed as following (see ):
1: lingual cortical bone sample
2: vestibular diagonal ramus cortical bone sample
3: vestibular horizontal corpus cortical bone sample
4: full ramus piercing sandwich, with vestibular cortical, medullar and lingual cortical bone sample 5: full corpus piercing sandwich, with vestibular cortical, medullar and lingual cortical bone sample.
2.3. Hardness tests
All samples were hot press-mounted in a standard resin with a 3 min heating time and a 2.5 min cooling time, at a 250-bar pressure and then automatically polished under water using a polishing disk (80 grains) until plain surface was obtained. Each sample was tested with a hardness testing automatic Fischer↓ machine calibrated with a pyramidal Vickers tip, using 6 × 6 matrices in order to keep more than 30 relevant values in HV. Each hardness measure was performed for a 2000 mN load, with an increase and decrease time of 20 seconds, and a 5 seconds peak time. Each result was compared using the Z-statistical test or the Student t test when less than 30 values-per-sample were kept out.
2.4. Traction-to-fracture test
All left sides were osteotomized according to Epker's technique, but not cleaved in two. The cleavage was performed at a 2 mm.min−1 rate until fracture, on an automatic Instron® electro-mechanical testing machine, with specific home-made grips mounted on two sub-periosteal elevators introduced inside the uncleaved osteotomy.
Each half-left mandible was then cleaved with measurement of the necessary force (N) depending on the displacement (l) of the two grips.
3. Results and discussion
We sampled and submitted 3 mandibles to hardness tests, and 5 mandibles to traction to fracture tests.
3.1. Hardness results
The results detailed in are concordant with the bony state of the specimens, as the measured hardness decreases as the specimen number increase. As a matter of fact, specimen 1 was fully dentulate with a trophic bone, specimen 2 had a worsened oral state with slightly atrophic bone, and specimen 3 had a very atrophic basilar mandibular bone.
Table 1. Hardness results in HV, mean (SD).
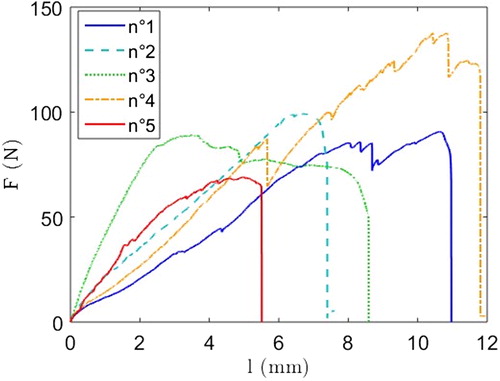
3.2. Traction to fracture results
The curves are reported in . The load increase is quite linear until rupture. The final load drop is characteristic of a brittle fracture, while small decreases during loading can be associated with cracks initiations. No “bad splits” were observed with our protocol.
3.3. Discussion
Most studies on the biomechanical properties of the mandibular bone concern the dentulate part of the mandible. Lettry et al. (Citation2003) performed a 3-pts bending tests in various parts of the dentulate mandible to obtain an average Young's modulus and demonstrated that the mandibular bone is anisotropic. Odin et al. (Citation2010) have performed an inverse finite element analysis to obtain such results, but without care brought to the medullar bone. Eijden et al. (Citation2006) studied the condylar bone with the same protocol than Lettry et al. (Citation2003) and obtained lower Young's modulus than for the dentulate part of the mandible, but with a rather important variation (600MPA to 3 GPa).The results presented here suggest that hardness could be a proper indicator of bone trophicity. Those results will enlighten the fact that mandibular bone especially ramus has variable biomechanical properties that depend on the sample location. Another interesting result is the absence of “bad splits” suggesting that the correct course of the directed fracture is favored by small velocity cleavage.
4. Conclusions
This testing protocol will allow us to define the relevant underlying biomechanical properties regarding ramus sagittal osteotomy, in order to produce a reliable 3D printed model for surgical simulation. Our tests applied to their respective 3D printed replies will allow us to determine which protocol best matches the biomechanical properties at work during the osteotomy.
Acknowledgements
This original study was performed with the financial help of “La Fondation des Gueules Cassées” and le “Fond d'études pour la recherche et le corps médical”. Anatomic specimens experiments were supported by l'Ecole de chirurgie de l'APHP.
References
- Eijden T-M, van der Helm P-N, van Ruijven L-J, Mulder L. 2006. Structural and mechanical properties of mandibular condylar bone. J Dent Res. 85(1):33–33.
- Lettry S, Seedhom B-B, Berry E, Cuppone M. 2003. Quality assessment of the cortical bone of the human mandible. Bone. 32(1):35–44.
- Odin G, Savoldelli C, Bouchard P-O, Tillier Y. 2010. Determination of Young's modulus of mandibular bone using inverse analysis. Med Eng Phys. 32 (6):630–637.