1. Introduction
Every year in France, 18500 patients suffer from patellar instability. 17% of these are recurrences. Patellar instability is caused by excessive lateralization of the tibial tuberosity (TT) measured by a distance between femoral trochlear groove and the tibial tuberosity (> 17 mm +/– 4), dysplasia of the femoral trochlea, patella height anomaly (alta) and a rupture of the medial patellofemoral ligament (MPFL). In case of excessive lateralization, surgical management may be considered. It consists of medializing the anterior tibial tuberosity (TTA) to bring the patella to a stable position on the femoral trochlea. Recently, clinical observations based on MRI, have suggested that the inclination of the TT was also an aggravating factor in patellar instability. The purpose of our study was to quantify the effect of this new factor in patellar instability and to observe the effect of its correction on patellar dislocation. This surgical strategy has not yet been described in the literature, only the risk factors have been analyzed, by Chassaing.
2. Methods
Six knees were taken from fresh unpreserved corpses. The average sample age was 72.4 years +/- 6.8, with 4 women and 2 men: there were 4 left and 2 right knees. Samples with osteo-ligamentous pathology of the knee were excluded. The samples were prepared taking the distal ¾ of the femur and the proximal ¾ of the tibia as well as the patellar ligament, patella, femoral quadriceps tendon (keeping only the tendon of the rectus femoris and the vastus lateralis muscles). This part of the quadriceps tendon allowed us to apply the mechanical stress via locking loop Krackow suture with mersuture 3.
The samples were positioned in a TINUS OLSEN 10KN traction machine by means of a mechanical assembly that allowed the angle of mechanical loading to be adjusted (between the traction cable and the axis of the femoral diaphysis). This angle of torque is not physiological but was necessary to recreate the phenomenon of patellar dislocation. The load angle was determined by means of pulling, in order to have a tensile force producing patellar dislocation of between 60 and 90 N.
This arbitrary value was chosen in such a way as not to be destructive, for assembly, during mechanical loading. The traction angle was between 25° and 45° in the frontal plane and 0° in the sagittal plane. The knee was positioned with a 25° flexion and locked with a femoro-tibial pin.
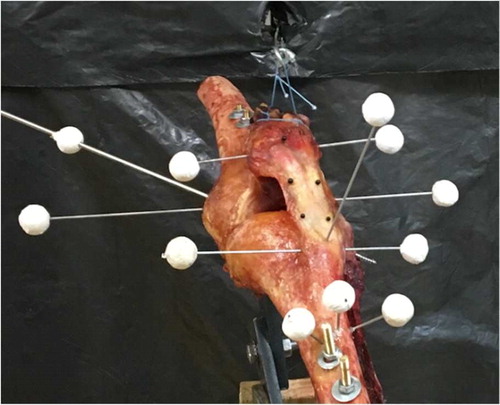
With the aid of a stereovision system, marker trihedrons were positioned on the assembly () using pins (∅ 2 mm) to enable measurement of the 3 D movements occurring during the translation and rotation of the femur, tibia, patella and TT. These trihedrons made it possible to identify the anatomical planes and more particularly the posterior bi-condylar plane, which was our reference for this study. During our tests we ensured that the tibial and femoral landmarks were immobile.
Figure 1. Experimental set-up to achieve traction on the tendon of the femoral quadriceps and markers to follow 3 D movements.
The loading (axial displacement of the retained fraction of the quadricipital tendon) for all tests was 10 mm/min. We performed 3 tests on each sample to ensure the reproducibility of patellar dislocation. The acquisition of force and images for the calculation of 3 D movements were performed at 1 Hz.
We performed an internal 30° de-rotation osteotomy of the TT that did not involve medialization of the TT. This latter was imperative to demonstrate that only the inclination of the TT was an aggravating factor in patellar dislocation. The fixation was carried out using two resorbable screws. The same test protocol performed on the native sample was repeated on the same sample after the osteotomy.
3. Results and discussion
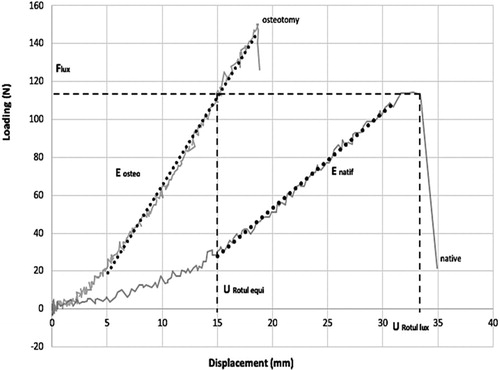
We measured the medialization of the TT to ensure that it was less than 2 mm (double thickness of the saw blade), thus validating the test. The marker tracking analysis determined the lateral displacement of the patella (U), the patellar tilt with respect to the posterior bi-condylar plane (α) as a function of the tensile force exerted on the retained fraction of the quadriceps tendon (F) ( and ).
Table 1. Average values of parameters (mm, N and degrees).
From the behaviour curves obtained, we calculated the following parameters: patellar displacement at the time of dislocation in the native subjects (Urotul lux), force at the time of dislocation (Flux), patellar displacement equivalent to this force Flux after osteotomy (Urotul equi). Also, we calculated the patellar tilt with respect to the posterior bi-condylar plane at the time of dislocation in native subjects (αrotul lux), and the equivalent tilt after osteotomy (αrotul equi). Finally, the initial tilt in natives (α0 natif) and after osteotomy (α0 osteo) was noted.
We subsequently determined the slope of the curve in the native subjects (Enative) and after osteotomy (Eosteo), thus reflecting the rigidity of the patellar system. We compared the data before and after the osteotomy using a Wilcoxon matched series test.
Statistical analysis showed a 4-fold increase in patellar system rigidity after medial de-rotation osteotomy (Enatif vs Eosteo; p = 0.03125) and a lateral displacement of the patella divided by 3 for an identical load after osteotomy (Urotul lux vs Urotul equi; p = 0.03125). We also showed a patellar tilt compared to the bicondylar plane reduced by a factor of 7 after osteotomy (αrotul lux vs αrotul equi; p = 0.03125). In addition, without mechanical stress, the osteotomy has the effect of parallelizing the transverse axis of the patella with the posterior bicondyle plane (α0lux vs α0equi; p = 0.03125). Morphologically, the patella is re-positioned on the femoral trochlea, in order to avoid recurrence of patellar instability.
4. Conclusions
In this study, we demonstrated that the torsion of the anterior tibial tuberosity is a factor in patellar instability. Surgical management by a new osteotomy of internal rotation, whose torsion’s angle would be measured by MRI and scanner, seems to be indicated for patients with recurrent patellar dislocations. A clinical study should validate the surgical technique on a cohort of patients.
References
- Chassaing V, Zeitoun JM, Camara M, Blin JL, Marque S, Chancelier MD. 2017. Tibial tubercle torsion, a new factor of patella instability. Orthop Traumatol: Surg Res. 103:11731178.
- Goutallier D, Bernageau J, Lecudonnec B. 1978. Mesure de l’écart tubérosité tibiale antérieure - gorge de la trochlée (T.A.-G.T.). Technique. Résultats. Intérêt. Revue de Chirurgie Orthopedique et Reparatrice de L’Appareil Moteur. 64(5):423–428.