?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.1. Introduction
Tibial plateau fracture represents 1.2% of all fractures and 4749 surgeries has been identified in 2017 in France (www.scansantz.fr. . . . . . . . . . ). Tuberoplasty (Vendeuvre et al. Citation2013) has been developed as a novel treatment method for two of the six types of tibial plateau fracture using minimally invasive techniques. This allowed the surgeons to reduce the fracture with the inflation of a surgical balloon usually used in Kyphoplasty —vertebrae compression fracture reduction—. Then, the surgeons stabilize the reduced fracture with PMMA cement injection and screws.
In this work, a numerical approach with a personalized finite element (FE) analysis based on peroperative —during the course of a surgery— images is proposed to evaluate the screw’s mechanical behaviour. It aims to help surgeons to manage the post-operative treatment as stele and reloading.
These goals include the estimation of (a) the risk of implant failures, (b) the risk of fracture instability from stress analysis around the fractured area, in accordance with the interactions with surgical materials —PMMA and screw— and stress shielding for bone healing (Giannoudis et al. Citation2007).
2. Methods
The study comprised a 40-year-old male patient (84 kg, 1.82 m tall) with a tibial plateau fracture from road accident. The fractures classified Schatzker type-II (Kfuri & Schatzker Citation2018) corresponded to the splitting and the depression of the lateral tibial plateau.
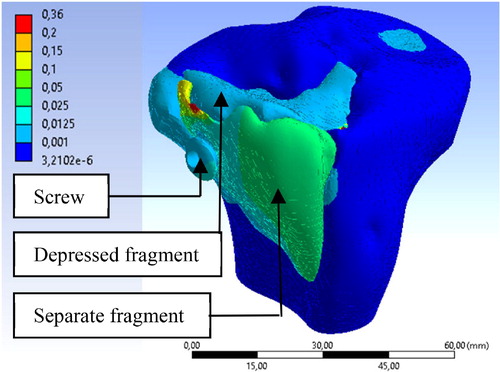
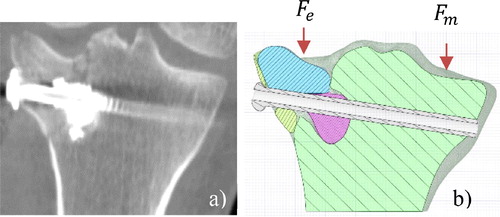
We segmented the model geometry from 3 D images acquired from a per-operative O-arm CT-Scan with a semi-automatic method based on a fast growing algorithm, with 3 D Slicer software (Fedorov et al. Citation2012). The model geometry was composed of two fragments, unbroken tibia, cement and screw (). The bone material properties were assigned according to local Hounsfield units using Bonemat software. The relation used between Hounsfield unit and elastic material behavior was based on the work of (Rho et al. Citation1995) for the proximal tibia:
Figure 1. a) Coronal CT Scan view of the tibia after stabilization. b) Schematic representation of the geometry, red arrows indicate the load.
The screw and cement material proprieties were: titanium alloy and PMMA
respectively. (Belaid et al. Citation2018).
A perfect bonding condition was considered between the screw-bone and cement-bone interfaces assuming ideal fixations. A frictionless behavior was assigned to the bone-bone contacts. These conditions correspond to the postoperative fracture after a short period of bone healing.
The applied load was chosen to simulate a single leg stance during gait, which corresponds to a joint contact force equal to three times the body weight. The load was shared between external ( and medial
plateau by 45% and 55% respectively (Zhao et al. Citation2007).
3. Results and discussion
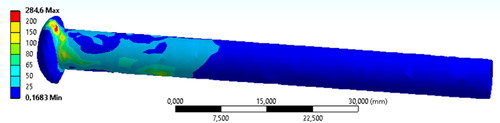
We found that the maximum Van Mises stress on the screw was 284.6 MPa, it corresponds to 30.60% of the titanium alloy yield strength. The maximum Van Mises stress in the PMMA cement was 10.83 MPa. According to this, the simulation ensures a good mechanical behaviour of the surgical material ().
The maximum Van Mises stress in the tibia was 160.82 MPa.
The average displacement Z of the depressed fragment was mm with a maximum and minimum of
mm and
mm respectively. The maximum displacement was
mm located on the separate fragment ().
The main limitations of our work are non-integration of soft tissues behaviour and the contact assumptions. First, soft tissues should influence the displacement of the separate fragment. Secondly, the PMMA should have a good interconnexion and bonded conditions should be verified. However, the screw may act only as a beam into the structure. Bonded screw-bone contact may be an over evaluated contact behaviour. Frictionless behaviour for bone-bone contact maximise the displacement but lower contact pressures. In next work, we should evaluate the cohesion among bone-cement; screw-cement; screw-bone and bone-bone contacts. The frictionless assumption should be change to a frictional behaviour with a correct friction coefficient for a stress analysis in the bone geometries.
As bone healing process is better under constraint, early full weight bearing is desirable for clinicians (Giannoudis et al. Citation2007). And, for old patients, it prevents the dangers of bed rest. This work could help surgeons to evaluate their postoperative treatment after Tuberoplasty. Actually, the patient has to wait 3 months before full weight bearing.
4. Conclusions
For the first time, surgeons performed peroperative navigation system for minimally invasive tibial plateau fracture reduction. This allowed the surgeons to use only one screw for the fracture stabilization. The present work based on the images acquired during the surgery evaluated the post-operative mechanical behaviour of the stabilization solution. Based on stress analysis, we found that the choice of a 6.5 mm diameter screw was appropriate for this clinical case. The clinical practitioners can appreciate the data —mechanical resistance and the deformation for the maximal load during gait— to determine the personalized post-operative treatment —as stele and reloading—.
Acknowledgements
The authors would like to thank ANSYS SAS France
References
- Belaid D, Vendeuvre T, Bouchoucha A, Brémand F, Brèque C, Rigoard P, Germaneau A. 2018. Utility of cement injection to stabilize split-depression tibial plateau fracture by minimally invasive methods: a finite element analysis. Clin Biomech. 56:27–35.
- Fedorov A, Beichel R, Kalpathy-Cramer J, Finet J, Fillion-Robin J-C, Pujol S, Bauer C, Jennings D, Fennessy F, Sonka M, et al. 2012. 3D Slicer as an image computing platform for the quantitative imaging network. Magn Reson Imaging. 30(9):1323–1341.
- Giannoudis PV, Einhorn TA, Marsh D. 2007. Fracture healing: the diamond concept. Injury. 38:S3–S6.
- Kfuri M, Schatzker J. 2018. Revisiting the Schatzker classification of tibial plateau fractures. Injury. 49(12):2252–2263.
- Rho JY, Hobatho MC, Ashman RB. 1995. Relations of mechanical properties to density and CT numbers in human bone. Med Eng Phys. 17(5):347–355.
- Vendeuvre T, Babusiaux D, Brèque C, Khiami F, Steiger V, Merienne J-F, Scepi M, Gayet LE. 2013. Tuberoplasty: minimally invasive osteosynthesis technique for tibial plateau fractures. Orthop Traumatol Surg Res. 99(4):S267–S272.
- Zhao D, Banks S A, Mitchell K H, D'Lima D D, Colwell C W, Fregly B J. 2007. Correlation between the knee adduction torque and medial contact force for a variety of gait patterns. J Orthop Res. 25(6):789–797.