1. Introduction
The foot is a complex polyarticular system that requires, for advanced biomechanical modeling, to take into account structural anatomy in a comprehensive way. When neuropathy affects the sensory nerves responsible for protecting the foot of sustaining high pressures, there is a risk of pressure ulcers. This risk can be increased when bony structures exhibit pathological shapes. Mechanobiology describes a process of fast ulcer formation when soft tissues undergo strains larger than 50% (Oomens et al. Citation2015). Reducing the load in overpressure areas is the recommended treatment to prevent risk. When unloading is not effective, a surgical procedure may be necessary. This study investigates the influence of sole stiffness on the risk of ulceration in a patient with type 2 neuroarthropathy with a history of pressure ulcers. We also propose a procedure to optimize surgery if the conservative treatment is deficient.
2. Methods
2.1. Generic biomechanical finite element foot model
Our group has developed a complete foot model combining finite element (FE) and rigid multibody modeling using the Artisynth framework (Perrier et al. Citation2015). The FE mesh has 142,060 elements (mainly hexahedrons) and 66,362 nodes. Three soft tissue layers with Neo Hookean materials (Young moduli, Poisson Ratio) were created to represent a 1 mm skin layer (200 kPa, 0.485), fat (30 kPa, 0.49) and muscle (60 kPa, 0.495) tissues. A fourth layer represents the heel fat pad (100 kPa, 0.4998). The model includes ligaments, plantar aponeurosis and simulates the contacts between bony structures ().
2.2. Patient specific strain risk analysis
Starting from the generic foot model, we designed a simplified patient-specific model presenting the same features only without contacts between bones. The considered patient is suffering from a type 2 neuroarthropathy and has a 7 years history of plantar ulcer recurrences despite an adapted orthosis. In a first simulation, real pressures, measured under the patient’s foot, were applied on the sole. In a second simulation the model was positioned on a virtual pressure platform bearing half of the patient’s weight. An analysis of the strains within the finite element mesh was performed. Contiguous elements with the strain values above the ulceration threshold were extracted as “strain clusters.” Finally, the volume of these clusters was monitored and displayed in order to anatomically locate the deformation sites as well as the volume of affected tissues.
2.3. Influence of insole stiffness on internal strain levels
In order to determine the impact of the stiffness of insoles material on strain clusters, we simulated various EVA with Young’s moduli ranging from 2000 KPa to 100 KPa, and a Poisson coefficient of 0.495.
We analyzed the volumes of 2 types of strain clusters: (1) with strains greater than 50%, and (2) with strains between 20% and 50%.
3. Results and discussion
3.1. Plantar pressure comparison model
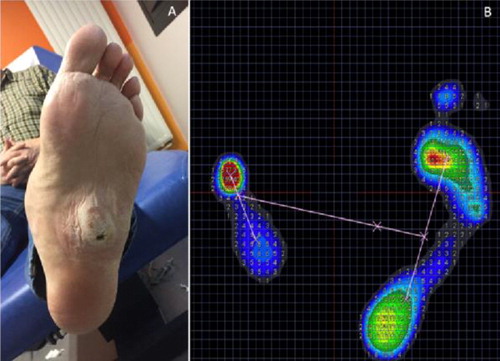
Plantar pressures as recorded by a calibrated baropodometric platform (Zebris FDM-SX, Germany) show a pressure distribution comparable to the one exhibited by the simulated foot loading on the virtual platform.
We advocate that assessing plantar pressure magnitudes and spatial distribution is a reliable way to validate the loading of complex foot models.
3.2. Patient-specific strain risk analysis
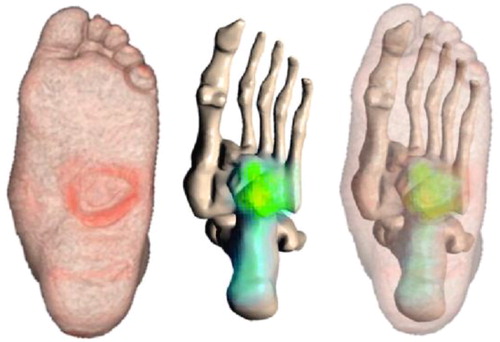
The three-dimensional superposition of simulated risk deformation data and CT-scan visualizations shows good agreement between the location of 50%-or-more strain clusters and the location of the ulcer area (). These results seem to indicate that the use of strain thresholds along with the extraction of strain clusters could be a new method for assessing the risk and location of possible ulceration. If a simulated surgical gesture reduces the strain clusters’ volumes along with deformation values, it can be expected that such a gesture would reduce wound recurrence.
3.2. Influence of insole stiffness on internal strain levels
Strain clusters’ volume analysis shows that for this patient, stiffness changes have a small influence on the risk for deep tissue injury. Indeed, cluster volumes with strains between 20% and 50%, as well as those above 50% decrease only slightly despite a significant decrease of the insole’s Young’s modulus. Pressure ulcer risk seems therefore to be still present despite softer insoles. This result might explain why this patient had systematic wound recurrence despite the use of various foot orthoses adapted in shape and material. For this patient, the therapeutic solution finally chosen was to reduce tissue compression by surgically cutting the cuboid bone.
4. Conclusions
Patient-specific biomechanical FE foot modeling coupled with a rigid multi-body skeleton shows promising results in terms of correlation between internal strain clusters and tissue locations at a higher risk of deep tissue injury. Parametric analysis of interface materials (such as an insole) can provide insight on the effect of an orthosis on pressure ulcer risk. As concerns the clinical case presented here, this method explained the failure of orthotic treatments, and helped to set-up a surgical treatment aiming at a subcutaneous bone clipping (). At this moment, this method cannot be used in a clinical routine due to the complexity of biomechanical model design. However, the conclusions drawn from the FE analysis presented here provide fresh insight on otherwise inexplicable pressure ulcer recurrences in a neuropathic subject.
References
- Bucki M, Luboz V, Perrier A, Champion E, Diot B, Vuillerme N, Payan Y. 2016. Clinical workflow for personalized foot pressure ulcer prevention. Med Eng Phys. 38(9).
- Oomens CW, Bader DL, Loerakker S, Baaijens F. 2015. Pressure induced deep tissue injury explained. Ann Biomed Eng. 43(2):297–305.
- Perrier A, Luboz V, Bucki M, Vuillerme N, Payan Y. 2015. Conception and evaluation of a 3D musculoskeletal finite element foot model. Comput Methods Biomech Biomed Engin. 18( Suppl 1):2024–2025.