1. Introduction
The face expression is animated by the movements of the muscles, which can be altered during pathology. Assessment of facial muscle deficits is subjective (palpation), dependent operator, and is currently estimated with clinical scales (Kanerva et al. Citation2006). Thus, the quantification of the facial muscle functional properties is a key point for the clinician to adapt and evaluate treatments (surgical, injection or reeducation) for patients with facial paralysis. Magnetic resonance elastography (MRE) has been developed to measure the in vivo elastic properties of healthy (Chakouch et al. Citation2016) and pathological (Bensamoun et al. Citation2015) muscles. The objective of this study is to develop a new imaging protocol to evaluate the functional properties of the zygomaticus major (ZM) muscle using MRE technique.
2. Methods
2.1. Magnetic resonance elastography (MRE)
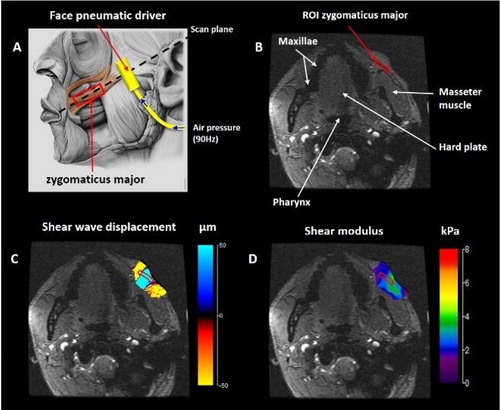
MRE was conducted with a 1.5 T Signa HDx MR machine (General Electric, Milwaukee, WI, USA) on three healthy participants in a supine position. To characterize the ZM muscle, in a relax state, a pneumatic driver was placed below the zygomatic bone in the direction of the corner of the mouth (). This driver has a rectangular mouthpiece (1.5 cm × 2.5 cm) and is surrounded with a pad. To ensure good transducer contact, a pad was added to the top of the driver that induced no movement when the head coil (32 channels) was added. Periodic variations in air pressure were induced inside the tube at 90 Hz resulting in the propagation of acoustic waves within the facial muscles. The MRE pulse sequence included a motion-encoding gradient, that oscillated in the Z direction, was used to image the displacement of the shear waves.
Figure 1. MRE protocol developed for the ZM muscle. A: Localization of the scan plane through the ZM and the face pneumatic driver. B: Anatomical axial T1 image with the ZM surrounded by red region of interest (ROI). C: Phase image showing the shear wave displacement. D: Cartography of the shear modulus.
2.2. Anatomical and phase images
MRI acquisition of the ZM is a challenge due to its thin morphology and long structure. In the present study, anatomical axial T1-weighted images () of the ZM were evaluated using a specific MRI protocol developed by the Radiology Department at CHU Amiens in collaboration with maxillofacial surgeons.
Then, an oblique scout was placed in the ZM to track the propagation of the shear waves. The wave displacement phase images were recorded with a 256 × 256 acquisition matrix, two opposite polarities of the motion-encoding gradient (with a 2.2 G/cm maximum amplitude limit) in the Z direction, a flip angle of 25°, a 18 cm field of view, a 1.5 mm slice thickness and 4 offsets were recorded. The scan time was 45 seconds with a TR/TE of 55.5/19.1 ms.
2.3. Phase image processing and data analyses
The recorded phase images underwent post processing by applying a mask that removed the noise located in the background of the image. A directional filter oriented along the direction of the wave propagation and a Butterworth spatial filter were applied to simultaneously remove interfering waves, longitudinal waves, and noise (Manduca et al. Citation2003).
Assuming that the ZM muscle was linearly elastic, isotropic, homogeneous and incompressible, the shear modulus (μ), representing the local elasticity, was calculated using the following equation: μ = ρ (f. λ)2 where ρ is the muscle density and was assumed to be close to that of water (i.e. 1000 kg/m3), f is the frequency and λ is the wavelength.
3. Results and discussion
shows a clear propagation of the shear wave within the cheek tissues (ZM, fat, etc …). The shear modulus (µ) value, measured from a ROI placed around the ZM, was 2.45 ± 0.32 kPa. However, the displacement of the waves was not only within the individual ZM muscle, leading difficult the interpretation of the elastic properties of this muscle.
Thus, the imaging protocol should be further improved to generate shear wave only within this thin muscle. Indeed, clinicians need to quantify the functional behavior of ZM before and after treatment and to test the effectiveness of therapies.
A solution could be to adjust the power and the design of the pneumatic drivers for such tiny muscles. Another improvement could be to develop acupuncture needle pneumatic drivers, such as those used for invasive muscle electromyography, to generate shear waves via longitudinal vibrations of the needle within the ZM. This type of driver has been applied to livers of mice using 3T MRI to assess fibrosis (Yin et al. Citation2017). However, the application of such needle driver to the human face seems impossible (invasive and uncomfortable) to incorporate into patient care.
In addition to clinical application, the present MRE protocol could provide the real in vivo functional properties of the ZM muscle which could be implemented in numerical models of facial expression (Esteve-Altava et al. Citation2015; Ang-Xiao et al. Citation2017).
4. Conclusions
The originality has been to develop a new MRE protocol for thin muscles (<3mm) and it remains technological challenges. The present study is the first to demonstrate the utility of MR elastography in the regular care of facial palsy patients and paves the way for other applications.
Acknowledgements
We thank the Mayo Clinic (Dr Ehman, elastography department) for its technical support.
Additional information
Funding
References
- Ang-Xiao F, Dakpé S, Dao TT, Pouletaut P, Rachik M, Ho Ba Tho MC. 2017. MRI-based finite element modeling of facial mimics: a case study on the paired zygomaticus major muscles. Comp Method Biomech Biomed Eng. 20 (9):919–928.
- Bensamoun SF, Charleux F, Debernard L, Themar-Noel C, Voit T. 2015. Elastic properties of skeletal muscle and subcutaneous tissues in duchenne muscular dystrophy by Magnetic Resonance Elastography (MRE): a feasibility study. IRBM. 36 (1):4–9.
- Chakouch MK, Pouletaut P, Charleux F, Bensamoun SF. 2016. Viscoelastic shear properties of in vivo thigh muscles measured by MR elastography. J Magn Reson Imaging. 43(6):1423–1433.
- Esteve-Altava B, Diogo R, Smith C, Boughner JC, Rasskin-Gutman D. 2015. Anatomical networks reveal the musculoskeletal modularity of the human head. Sci Rep. 5 (1):8298.
- Kanerva M, Poussa T, Pitkäranta A. 2006. Sunnybrook and house-brackmann facial grading systems: intrarater repeatability and interrater agreement. Otolaryngol Head Neck Surg. 135 (6):865–871.
- Manduca A, Lake DS, Kruse SA, Ehman RL. 2003. Spatio-temporal directional filtering for improved inversion of MR elastography images. MIA. 7 (4):465–473.
- Yin M, Glaser K J, Manduca A, Mounajjed T, Malhi H, Simonetto D A, Wang R, Yang L, Mao S A, Glorioso J M, et al. 2017. Distinguishing between hepatic inflammation and fibrosis with MR elastography. Radiology. 284(3):694–612.
