?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.1. Introduction
Tibial plateau fractures represent 1.2% of all fractures (Court-Brown and Caesar Citation2006). Due to their number and their difficulties of care, they represent a real public health issue.
This study is about tibial plateau depression fractures: Schatzker type III (Kfuri & Schatzker Citation2018; Schatzker et al. 1979). The impact of the femoral condyle in the tibial plateau generates a depression, a spherical, multi-fragmented cavity. Surgical management is the current gold standard for this type of tibial plateau fracture (Honkonen Citation1994). It is based on reduction via a chasse graft or a creed spatula; a graft and then an osteosynthesis by plate and/or screws. This invasive approach exposes to a significant risk of infectious complications, pseudarthrosis, and stiffness (Kugelman et al. Citation2017; Li et al. Citation2018; Gaunder et al. Citation2019). It requires several days of hospitalization.
With a good understanding of the fracture mechanism (Kennedy and Bailey Citation1968), it is legitimate to believe that reduction via harvesting tamp is not the optimal management. The fracture created by a cylindrical surface represented by the femoral condyle must be reduced by a larger surface that follows the entire depression and not a single portion.
Recently, Tuberplasty (Vendeuvre et al. Citation2013) has been developed as a novel method using minimally invasive techniques to treat tibial plateau fracture. The surgeons use the inflation of a balloon to reduce the fracture. The surgical balloon seems to meet the criteria for a perfect reduction in the joint surface.
The aim of this study was to demonstrate that the swelling of a surgical balloon on a cortico-spongy structure allows a three-dimensional anatomical reduction of joint fragments in the context of a tibial plateau fracture by Schatzker III depression.
2. Methods
2.1. Specimen preparations
The analysis concerns a tibia-fibula specimen derived from a cadaveric subject. The specimen was sawn at the diaphysis at the distal third and cast in the resin (rigid polyurethane) in order to ensure fix boundary conditions during mechanical tests. A Schatzker III depression fracture was performed using the Tinius Olsen 10 kN setup () (Vendeuvre et al. Citation2018).
2.2. Measurement method
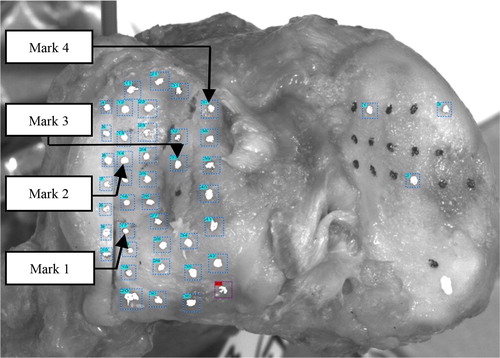
Displacement field was measured stereoscopic optical method (3 D mark tracking) (Germaneau et al. Citation2010). A set of points was placed on the surface of the tibia to follow the surface displacement of the various fractured fragments. ()
2.3. Balloon inflation
The surgical balloon (Kyphon Expender II Kit) was introduced, with X-Ray supervision, under the fracture. The surgical balloon was inflated gradually of 0.5 cm3 between each step. The surface reduction was captured with the stereoscopic system. Procedure was done when the fracture was reduced from the surgeon-view. A CT scan was performed at the end to check the result.
3. Results and discussion
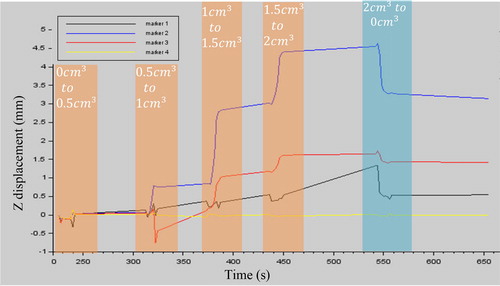
The three displacement components of each mark were analysed. We found that the maximum Z displacement on the tibial plateau is 4.48 mm. It corresponds to a balloon inflation; the fracture was reduced.
shows the Z displacement of four marks during balloon inflation and deflation. Three of them were in different fragments; the fourth was placed on a unbraked part. The balloon imposes a movement on all the fragments of the depressed part.
Figure 3. Z displacement (mm) of 4 markers () during inflations and deflation. The orange areas correspond to balloon inflation phases; the blue area corresponds to balloon deflation.
This experiment with stereoscopic measurement of the displacement during reduction allows us to analyse the mechanical behaviour of the tibial plateau fragments according to inflation. The main limitations are the use of cadaveric bone and the isolation of the bone. Soft tissue impact is not represented. This methodology should be used with the bone tamp method. This would allow comparisons between the two methods.
4. Conclusions
Tibial plateau depression fractures are completely reduced by the multi-directional expansion of the balloon. The surface analysis carried out, allows us to conclude that reduction with a surgical balloon provides a real advantage for the management of Schatzker III-type fractures of the tibial plateau. The balloon is a reliable alternative in the management of tibial plateau fractures. It allows a perfect reduction of the fracture site and avoids the complications associated with an invasive approach.
References
- Court-Brown CM, Caesar B. 2006. Epidemiology of adult fractures: a review. Injury. 37(8):691–697.
- Gaunder CL, Zhao Z, Henderson C, McKinney BR, Stahel PF, Zelle BA. 2019. Wound complications after open reduction and internal fixation of tibial plateau fractures in the elderly: a multicentre study. Int Orthopae (Sicot)). 43(2):461–465.
- Germaneau A, Doumalin P, Dupré JC, Brèque C, Brémand F, D’Houtaud S, Rigoard P. 2010. Experimental analysis of mechanical response of stabilized occipitocervical junction by 3D mark tracking technique. EPJ Web Conf. 6:21004.
- Honkonen SE. 1994. Indications for surgical treatment of tibial condyle fractures. Clin Orthop. 199–205.
- Kennedy J. C, Bailey WH. 1968. Studies of the mechanism and a classification. J Bone Jt Surg. 50(8):1522–1534.
- Kfuri M, Schatzker J. 2018. Revisiting the Schatzker classification of tibial plateau fractures. Injury. 49(12):2252–2263.
- Kugelman D, Qatu A, Haglin J, Leucht P, Konda S, Egol K. 2017. Complications and unplanned outcomes following operative treatment of tibial plateau fractures. Injury. 48(10):2221–2229.
- Li J, Zhu Y, Liu B, Dong T, Chen W, Zhang Y. 2018. Incidence and risk factors for surgical site infection following open reduction and internal fixation of adult tibial plateau fractures. Int Orthopae (Sicot)). 42(6):1397–1403.
- Vendeuvre T, Babusiaux D, Brèque C, Khiami F, Steiger V, Merienne J-F, Scepi M, Gayet LE. 2013. Tuberoplasty: minimally invasive osteosynthesis technique for tibial plateau fractures. Orthop Traumatol Surg Res. 99(4):S267–S272.
- Vendeuvre T, Grunberg M, Germaneau A, Maloubier F, Faure J-P, Gayet L-E, Rigoard P, Brèque C. 2018. Contribution of minimally invasive bone augmentation to primary stabilization of the osteosynthesis of Schatzker type II tibial plateau fractures: balloon vs bone tamp. Clin Biomech. 59:27–33.