1. Introduction
Cerebral palsy (CP) is the result of a lesion that has occurred in the brain. Signs of this condition appear in the early years of life. Clinically, this term refers to permanent neuro-motor disorders, affecting the movement development and posture which cause activity limitations. The diagnosis of this condition is difficult to establish and its classification is sometimes questionable due to the many possible clinical conditions. Nevertheless, irrespective of the disease’s severity, both medical and non-medical methods of care are based on a variety of therapeutic methods. The main objectives currently accepted are the maintenance and development of the individual’s general function in order to limit the expansion of the disability (Novak et al. Citation2013). Physical activity (PA) is a parameter that needs increased developing and encouraged in the care for young PC patients (Damiano Citation2006). Indeed, it has been established that these children have a daily PA level below the international threshold recommended by the WHO for 5-17 year olds (4-7). The purpose of this study is to identify the influence of adapted dynamic cycling upon the motor function of children with CP and to quantify the effects of PA.
2. Methods
Participants recruited were patients at the Eclore centre, a paediatric rehabilitation centre of the “Centre Hospitalier de l’Ardenne” (CHA) Vivalia in Libramont (Belgium). Seven children (8.5 ± 2.58 years old) with different motor levels (I to IV on GMFCS - E&R) were enrolled in this longitudinal and prospective clinical.
All participants were informed on the aim and objectives of the study and their parents agreed the participation through a written consent. This study was approved by mutual agreement by the medical ethics committees of the “Centre Hospitalier Universitaire” Dinant-Godinne and the “CHA-Vivalia” of Libramont. Ten individual dynamic cycling sessions were proposed during 5 weeks. The evaluated settings were gross motor function measure (GMFM-88), locomotor performances with the Abiloco-Kids test, locomotor endurance with the 6 minute walking test (6MWT) or the assisted 6 minute cycling test (A6MCT), and the enjoyment level towards the activity. Inclusion criteria applied were: established diagnosis of BMI or related motor disorder caused by a brain injury that appeared no later than 2 chronological years after birth, between 4 and 13 years old, ability to understand and respond to simple verbal commands, and in progress rehabilitation care. For the selected exclusion criteria, the researchers took several parameters into account such as: Medical conditions that contraindicate PA and/or are likely to be aggravated by PA practice.
The activity was carried out individually at 2 sessions per week for 5 consecutive weeks. The sessions were scheduled according to each child’s school and weekly therapy schedules. The days of practice could therefore vary from one week to the next. An adapted bike was assigned to each participant for the duration of the experiment, whether it was a personal bike or one lent by the centre. A total of six bicycles were used ().
Protective helmets were worn at each session. The statistical analysis was performed using XL-Stat 2019 software on EXCEL. The data normality tests were performed according to the Shapiro-Wilk scheme. Depending on the results of these tests, the comparison tests utilized were either the Wilcoxon signed rank test or the Student t for matched data. The threshold of the results’ significance (p-value) has been set at p < 0.05.
3. Results and discussion
No significant difference was found between pre- and post-scores concerning mean gross motor function and locomotor endurance. Only a significant improvement of locomotor performances (p = 0.006) of lying and reversal motor capacities (p = 0.005) were observed. The mean level of enjoyment measured during the experiment was at 4.58 (± 0.55) on a maximum level of 5. There was no significant effect of the proposed cycling activity on the participants’ overall motor function, contrary to the results found in the literature. In 2007, Williams and Pountney (2007) found a positive and significant change in standing, walking, running and jumping (GMFM-D and E) motor skills in 11 non-ambulatory CP children aged 11 to 15 years. Following 18 sessions of strength training on a static bicycle.
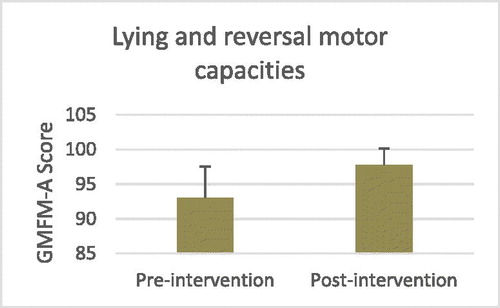
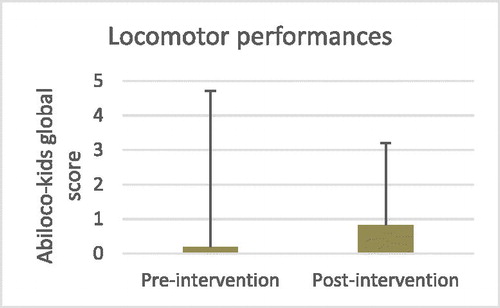
Fowler et al. reached similar conclusions in 2010 by offering 360 sessions of static bike training at 58 mobile CP children ages 7 to 18 years. However, no significant differences were found compared to the control group in this study. Researchers of this study noted a significant improvement following the cycling sessions in participants’ motor skills in the items in the lying and reversal test (GMFM-A) (). No studies identified have used the GMFM-88 in its entirety to assess the impact of cycling on participants’ motor function. It would then be interesting to verify through further studies whether this finding is confirmed. An improvement in the participants’ locomotor endurance was observed following the cycling activity, but this was not significant. Fowler et al. (Citation2010) demonstrated that cycling has a positive effect on the locomotor endurance of children with CP by observing a significant improvement in this parameter following training on a static bicycle. A significant improvement in the locomotor performance of participants in their daily lives was reported by their parents following the activity, via the Abiloco-Kids (). This would mean that the proposed cycling activity had a direct impact on the evolution of this parameter. In 2007, Verschuren et al. (Citation2007) reported that parents of youth with CP who had participated in a physical training program noticed progress in their child’s motor skills and independence.
4. Conclusions
The proposed dynamic cycling activity did not have a significant influence on the motor function of the participants. Contrarily, a significant improvement of their locomotor performance in everyday life was demonstrated at the end of the intervention. The activity also proved to be very popular with children. The adapted dynamic bicycle is therefore a possible and attractive physical activity for children with CP of different motor levels, but further studies are needed to clarify the effects of this physical activity on their motor skills.
References
- Damiano D. 2006. Activity, activity, activity: rethinking our physical therapy approach to cerebral palsy. Phys Ther. 86(11):1534–1540.
- Fowler E G, for the Physical Therapy Clinical Research Network (PTClinResNet), Knutson LM, DeMuth SK, Siebert KL, Simms VD, Sugi MH, Souza RB, Karim R, Azen SP. 2010. Pediatric endurance and limb strengthening (PEDALS) for children with cerebral palsy using stationary cycling: a randomized controlled trial. Phys Ther. 90(3):367–381.
- Novak I, Mcintyre S, Morgan C, Campbell L, Dark L, Morton N, Goldsmith S. 2013. A systematic review of interventions for children with cerebral palsy: state of the evidence. Dev Med Child Neurol. 55(10):885–910.
- Verschuren O, Ketelaar M, Gorter JW, Helders PJM, Uiterwaal CSPM, Takken T. 2007. Exercise training program in children and adolescents with cerebral palsy: a randomized controlled trial. Arch Pediatr Adolesc Med. 161(11):1075–1081.
- Williams H, Pountney T. 2007. Effects of a static bicycling programme on the functional ability of young people with cerebral palsy who are non-ambulant. Dev Med Child Neurol. 49(7):522–527.