1. Introduction
The left ventricle hemodynamics is complex and is influenced by the anatomy of the mitral valve. Subsequent changes of intraventricular flow patterns, particularly vortex formations, are in relation with the type of the mitral valve prosthesis (Gharib et al. Citation2006). In this study, we reproduced in vitro the intraventricular hemodynamics downstream a native anatomical-shaped mitral valve (LifeLike BioTissue Inc., Ontario, Canada). Flow velocity fields were obtained with the Echo Particle Image Velocimetry (Echo-PIV) method, which is a clinical tool analog to optical particle image velocimetry (PIV) principle used to detect flow velocity field.
2. Methods
2.1. Double activation simulator
The double-activation simulator mimics the left human heart from the pulmonary valve to the systemic capillaries, going through the left atrium (LA), the left ventricle (LV) and the aorta (AO) (Tanné et al. Citation2010). The left atrium and ventricle were anatomical shape silicone molding parts. They were both immersed into separate and closed boxes filled, and activated by two Vivitro super pumps (VivitroLabs, Victoria, BC, Canada). Pulmonary venous return was done by a gear pump. The fluid circulating was a water and glycerol solution (40% of glycerol, 60% of water) with a dynamic viscosity of 3.8 ± 0.2 cP. LV, LA and AO pressures were measured using 3 pressure catheters (Millar MPR 500 [Millar Sensor System Solution, Houston, Tex]). The diastolic and systolic flow volumes were measured using an electromagnetic flowmeter (Probe 95 [Carolina Medical, East Bend, NC]) positioned between LA and LV, 5 mm upstream of the mitral valve. The effective orifice area (EOA) was calculated by dividing the diastolic flow volume measured with the flowmeter by the time velocity integral of the mitral flow.
2.2. The mitral valve
An anatomically shaped mitral valve made of hydrogel was designed and manufactured specially for this study with Lifelike Biotissue company (Lifelike BioTissue Inc., Ontario, Canada). This valve had six chordae and presented tactile and mechanical properties of a real tissue. Chordae were attached on the lateral wall of the left ventricle with a system to adjust their tension by applying calibrated strain on the chordae.
2.3. Experimental conditions
Eight different hemodynamic conditions were tested by varying the mean aortic pressures (40 and 100 mmHg), mitral flow volumes (3, 4.5 and 5.5 L/min), heart rate (45 and 70 bpm) and mitral flow profile (E wave/A wave; E/A = 0.5, E/A = 1 and E/A = 1.5).
2.4. Images acquisitions
Echographic B-mode images were acquired with a General Electric Vivid E9 using a transesophageal probe (6Tc-RS TEE probe, 5.0 MHz). It was placed in front of the mitral valve in the LV box at a distance of 1 cm from the apex and 8 cm from the mitral valve. Microbubbles of a contrast agent Sonovue (Bracco International) were introduced into the circulating fluid. Their concentration remained stable during the experiment by infusing 2 ml/min.
2.5. Echo-PIV data
Echographic raw data were extracted from the hierarchical data file (HDF5) format using the clinical workstation EchoPAC (GE Healthcare). The speckles tracking and the vector flow mapping modality were computed using a PIV algorithm (Perrot and Garcia Citation2018).
3. Results and discussion
The qualitative analysis of Echo-PIV data allowed to visualize velocity fields in the left ventricle during a cardiac cycle. shows velocity fields at the peak of the filling wave, at the beginning of systole and at late systole. The flow passed through the mitral valve and reached the septum, then moved along the septum toward the apex. The formation and the development of a vortex facilitated the ejection of the flow through the aortic valve.
Figure 1. Qualitative representation of velocity fields in case of normal hemodynamics conditions (mean aortic pressure: 100 mmHg, heart rate: 70bpm, mitral flow: 5.5 L/min and E/A ratio: 1.5).
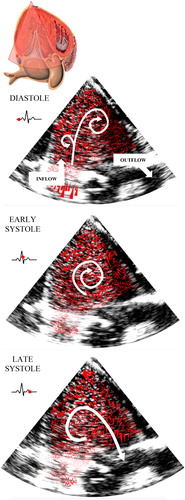
First, during diastole, the mitral jet developed two vortices on each side of the ring mitral valve then reached the apex. During diastasis, the flow formed a stable vortex in the mid-apical part of the left ventricle. Then, the circulation was reinforced by the second filling jet induced by the atrial contraction. Once the left ventricle contracted, the flow was directed to the aortic valve.
All of these comments are similar to observations made during the in-vivo analysis of left ventricular hemodynamics on healthy hearts (Cimino et al. Citation2012).
The vortex formation time defined by Gharib et al. was calculated at T = 5.3, which is within the optimal range of 3.3 <T < 5.5, a predictor of a healthy left ventricle.
4. Conclusions
In this study, we reproduced in-vitro the hemodynamics of the left ventricle in a normal heart with a new model of anatomically native mitral valve. Thus, this experiment opens new perspectives for the study of left intraventricular hemodynamics in cases of mitral insufficiency. A more general study will aim to achieve a mitral regurgitation by inducing a pathology to the left ventricle (ventricular remodeling) or directly on the valve (elongation or tension on a chordae). Afterwards, the pathological mitral valve will be repaired with the “Kalios” mitral ring (Tozzi et al. Citation2017) which can be adapted to the pathology by adjusting its geometry.
References
- Cimino S, Pedrizzetti G, Tonti G, Canali E, Petronilli V, De Luca L, Iacoboni C, Agati L. 2012. In vivo analysis of intraventricular fluid dynamics in healthy hearts. Eur J MechB/Fluids. 35:40–46.
- Gharib M, Rambod E, Kheradvar A, Sahn DJ, Dabiri JO. 2006. Optimal vortex formation as an index of cardiac health. Proc Natl Acad Sci USA. 103(16):6305–6308.
- Perrot V, Garcia D. 2018. Back to basics in ultrasound velocimetry: tracking speckles by using a standard piv algorithm. In: 2018 IEEE International Ultrasonics Symposium (IUS). p. 206–212.
- Tanné D, Bertrand E, Kadem L, Pibarot P, Rieu R. 2010. Assessment of left heart and pulmonary circulation flow dynamics by a new pulsed mock circulatory system. Exp Fluids. 48(5):837–850.
- Tozzi P, Hayoz D, Antona C, Fiore GB, Siniscalchi G, Ferrari E, Baeriswyl G, Vismara R. 2017. Mastering mitral leaflets coaptation after valve repair with adjustable mitral annuloplasty ring: proof of concept in mock loop study. ASAIO J. 63(2):168–173.
