1. Introduction
Thoracolumbar (TL) fractures occur in 7% of blunt trauma and have a high impact on the patient’s quality of life and healthcare costs (Schouten et al. 2015). In case of instability, spinal alignment disruption and vertebral canal stenosis surgery is indicated. Short posterior fixation is the most commonly used treatment (Hu et al. Citation2019). In comparison to the conventional open approach, the less invasive percutaneous approach results in less blood loss and earlier post-operative recovery. However, fracture reduction is less effective in percutaneous compared to open procedures (Sun et al. Citation2017) and therefore is not always advised (Jiang et al. Citation2012).
A novel polyaxial screw (OAK system, Safe Orthopaedics, France) is developed that functions like a monoaxial screw to realign the spine after fixation to the rod. Forceful reduction is possible since the OAK screw after fixation always reduces to an angle of 90° with the rod. Since the screw is polyaxial before final fixation to the rod the operation is simplified. Possibly making this a fast and more effective percutaneous treatment for TL fractures. In this experimental cadaveric study, fracture reduction and construct stiffness is compared between the novel OAK screw and a polyaxial screw (Sterispine PS, Safe Orthopaedics, France) in two cadaver samples as a proof of concept.
2. Methods
2.1. Specimen preparation and experimental setups
Since the burst fracture is the most common TL fracture type, a validated burst fracture model by (Germaneau et al. Citation2017) was chosen. Since the L1 vertebra is most often affected in case of TL fractures, T11-L3 segments of 2 subjects (samples 1 and 2) were selected.
In sample 1 the L1 vertebra was weakened by making small holes in the anterior wall ensuring fracture formation at this level without impact on fracture characteristics. In sample 2 the anterior wall was weakened by performing an anterior wall osteotomy sacrificing the anterior longitudinal ligament (ALL) to obtain more kyphosis.
2.2. Loading setup and measurement method
A specific spinal loading simulator (Germaneau et al. Citation2017) was used for this study, where physiological loading on specimens is applied using pure moments. Three loading cycles of 5Nm were used in sagittal, frontal and transverse directions.
Both screw systems were compared in both samples. In sample 1 the tests were started with 5.5 mm diameter OAK screws and, a second round of testing was done with 6.5 mm diameter Sterispine screws. In sample 2 the Sterispine screws were tested first.
A stereoscopic mark tracking technique was employed to measure motion variation between each spinal level during loading (Germaneau et al. Citation2017).
3. Results and discussion
3.1. Fracture reduction
Observation and analysis of the images made by the optical method confirm a significant kyphotic deformity in both samples as shown in . Although the change in vertebral kyphosis (VK) and regional kyphosis (RK) was more outspoken in sample 2 (ΔVK= 17°, ΔRK= 20°) than sample 1 (ΔVK= 8°, ΔRK= 6°) final kyphotic deformity was similar in both samples.
Table 1. Vertebral kyphosis (VK) and regional kyphosis (RK) measured after reduction with two types of implants for specimens with (1) or without (2) the anterior longitudinal ligament (ALL).
A convincing difference in VK and RK reduction is seen by the OAK screw in both samples compared to a slight VK and RK reduction by the Sterispine screw. In both samples VK and RK reduction by the Sterispine screw was incomplete, reducing VK and RK for 37,5% and 33,3% respectively in sample 1 and 11,8% and 25% in sample 2. The OAK screw achieved successful VK and RK reduction in both samples, showing 125% VK reduction and 183% RK reduction in sample 1 and 94.1% VK reduction and 100% RK reduction in sample 2.
In this pilot, two different techniques for making a burst fracture were used. In sample 2 the ALL was cut as part of the osteotomy. This resulted in more anterior movement, possibly resulting in more extensive fracture reduction. Still these results strongly suggests that additional fracture reduction is possible with the OAK screw by forceful reduction compared to the Sterispine screw. Due to small sample size possible variation in fracture reduction due to screw switching could not be detected.
3.2. Construct stiffness analysis
Both samples were tested in the sagittal, frontal and transverse direction. Flexibility curves were computed for each level in all directions for both samples. shows the mean flexibility curve for flexion/extension (F/E) between level T12 and L2 (the fixated levels) of sample 1.
Figure 1. Angle variation (°) for level T12–L2 according to imposed pure moments in flexion/extension (Nm) for sample 1.
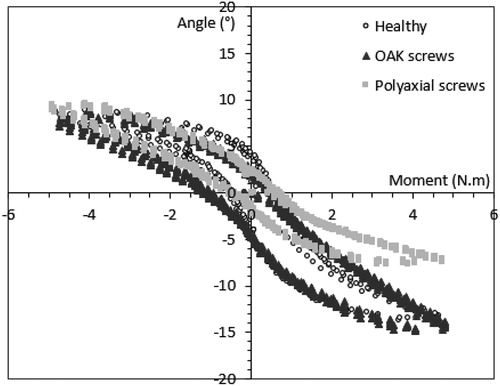
Due to small sample size, no definitive conclusions can be drawn from these preliminary results. The flexibility curve suggests that construct stiffness of the OAK screw is comparable to that of the Sterispine screw, but further testing is mandatory. Similar results were seen in both samples for all directions. Although the Sterispine screw seems to show less flexion. After analysing the images, it was seen that this was due to less fracture reduction and the inability of the sample to further go into kyphosis. Switching screws between testing did not seem to influence these results. No screw loosening was seen after switching the screws between testing.
4. Conclusions
This article presents the proof of concept for superior vertebral and regional kyphosis reduction of the novel OAK screw system compared to the Sterispine screw system in a pilot study with two cadaver samples.
Acknowledgements
The authors gratefully acknowledge Safe Orthopaedics for their financial support in order to make this research possible.
References
- Germaneau A, Vendeuvre T, Saget M, Doumalin P, Dupré JC, Brémand F, Hesser F, Brèque C, Maxy P, Roulaud M, et al. 2017. Development of an experimental model of burst fracture with damage characterization of the vertebral bodies under dynamic conditions. Clin Biomech (Bristol, Avon). 49:139–144.
- Hu Z-C, Li X-B, Feng Z-H, Wang J-Q, Gong L-F, Xuan J-W, Fu X, Jiang B-J, Wu L, Ni W-F. 2019. Modified pedicle screw placement at the fracture level for treatment of thoracolumbar burst fractures: a study protocol of a randomised controlled trial. BMJ Open. 9(1):e024110.
- Jiang XZ, Tian W, Liu B, Li Q, Zhang GL, Hu L, Li Z, He D. 2012. Comparison of a paraspinal approach with a percutaneous approach in the treatment of thoracolumbar burst fractures with posterior ligamentous complex injury: a prospective randomized controlled trial. J Int Med Res. 40(4):1343–1356.
- Sun X-Y, Zhang X-N, Hai Y. 2017. Percutaneous versus traditional and paraspinal posterior open approaches for treatment of thoracolumbar fractures without neurologic deficit: a meta-analysis. Eur Spine J. 26(5):1418–1431.
