1. Introduction
Thoracolumbar spine fractures are the most common injuries of the spine. They are mainly the result of a high-energy trauma. A surgical treatment is needed for most of the cases to restore bone stability, prevent neurological deterioration and provide pain relief. Generally, it consists in a posterior approach to reduce and stabilize the fracture by a synthesis with screws and rods. This synthesis can be combined with an injection of cement (kyphoplasty) after a balloon inflation providing a vertebral bone augmentation. The objective of this study is to quantify the interest of a filling when reducing the balloon vertebral fracture associated with a posterior stabilization assembly and to evaluate the different filling: bone (KO), cement (KS) or just internal reduction without filling (KV).
2. Methods
2.1. Specimen preparations
We used eighteen fresh frozen specimens of five vertebrae (T11-L3), providing from the laboratory of anatomy (ABS Lab) of Poitiers university. Mean age of specimens was 72.4 years (range of 55-87 years). The spine segments were dissected, and soft tissue scare fully removed to preserve bony parts and spinal ligaments in accord with the recommendations of (Wirtz et al. Citation2003). For each specimen, the upper half of cranial (T11) and the lower half of the caudal (L3) vertebra were fixed in rigid polyurethane resin to apply boundary conditions and loading. Specimens were distributed among three groups corresponding to each reduction solution.
2.2. Burst fracture and spine testing setup
A burst fracture was generated on L1 for each specimen from a dynamic loading (REF Germaneau CLB). All fractures were reduced and stabilized using titanium pedicle screws, and curved rods. For the Kyphoplasty procedure (KS) we used a 10 cc Poly Methyl MethAcrylate cement (PMMA). For KO group, cancellous bone coming from femoral heads were crushed and mixed with blood to increase viscosity and facilitate injection.
To study biomechanical behavior associated to each reduction techniques, we imposed physiological loadings on specimens. For that, a specific spinal loading simulator was used (Germaneau et al. Citation2017) to test flexibility by imposing pure moments according to one of the 3 physiological axes (Sagittal, bending and rotation) with cycles at 2.5 Nm and 3 cycles at 5 Nm.
We used a stereoscopic mark tracking technique to measure strain of vertebral body during loading (Germaneau et al. Citation2016) and angular motion between each level.
3. Results and discussion
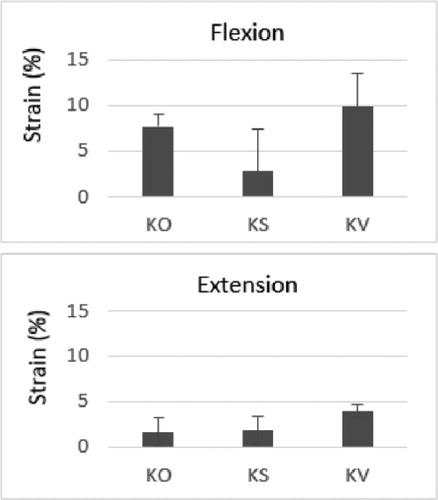
shows an example of strain values measured on vertebral body for flexion-extension movements for the three stabilisation techniques. For flexion loadings, we found a decrease of strain vertebral body in the fracture site for the PMMA (KS) group. We observed a significant difference with the absence of filling (p < 0.04) (Wilcoxon rank sum test). The comparison between KS filling and KO filling did not reveal any significant difference (p > 0.571). There was also no significant difference between KO and KV.
Figure 1. Strain on fractured vertebral body during Flexion-Extension loading according to stabilisation.
presents values of angle measurements before fracture and after stabilisation for flexionextension loadings and for each level of specimens from the KS group. We observed a decreasing of the mobility for adjacent disks of the fractured vertebra without a significant difference.
Figure 2. Evolution of angle mobility before fracture and after stabilisation by Kyphoplasty + cement (KS).
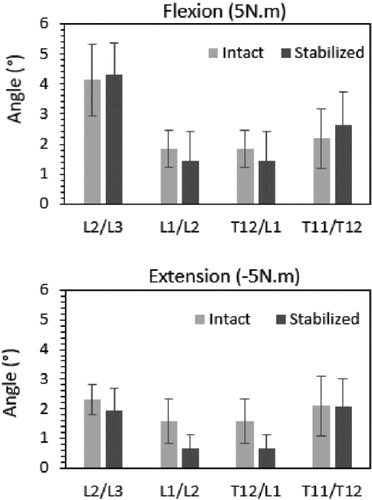
Similar observations and mobility evolutions have been observed for the two other groups. Comparison analysis did not reveal any significant difference between the groups.
The use of the balloon showed no increase displacement and even in some cases a complete reduction of the posterior wall related to ligamentotaxis, suggesting that it is a technique usable in a secure way even in case of important central canal compromise. We found also an important rate of screw loosening for elderly specimens (82,8vs 68; p < 0,04).
This is consistent with the result of Piazolla et al who find a PMMA cement or bone substitutes are not necessary for young people with additional posterior fixation.
4. Conclusions
The experiment highlighted frequent fixation problems when using short construct, especially in elderly specimens. Nevertheless, it appears that filling, whatever its nature, limits the loss of reduction in flexion extension mainly. This study shows that PMMA injection seems to be superior to bone injection and reduction only in mechanical analysis.
References
- Germaneau A, Vendeuvre T, Saget M, Doumalin P, Dupré JC, Brémand F, Hesser F, Couvertier M, Brèque C, Maxy P, et al. 2016. A novel approach for biomechanical spine analysis: Mechanical response of vertebral bone augmentation by kyphoplasty to stabilise thoracolumbar burst fractures. J Mech Behav Biomed Mater. 59:291–303.
- Germaneau A, Vendeuvre T, Saget M, Doumalin P, Dupré JC, Brémand F, Hesser F, Brèque C, Maxy P, Roulaud M, et al. 2017. Development of an experimental model of burst fracture with damage characterization of the vertebral bodies under dynamic conditions. Clin Biomech. 49:139–144.
- Piazzolla A, Solarino G, Bizzoca D, Parato C, Monteleone G, Dicuonzo F, Moretti B. 2018. The pedicle instrumentation and percutaneous elevation (Pi.Pe): a new cementless surgical technique in type A posttraumatic vertebral fractures. Eur Spine J. 27(S2):182–189.
- Wirtz DC, Pandorf T, Portheine F, Radermacher K, Schiffers N, Prescher A, Weichert D, Niethard FU. 2003. Concept and development of an orthotropic FE model of the proximal femur. J Biomech. 36(2):289–293.
